Abstract
BACKGROUND
Woven EndoBridge (WEB; Sequent Medical) treatment is an innovative endovascular approach for treatment of wide-neck bifurcation aneurysms. Initial studies have shown high safety with good efficacy at short term confirmed by trials conducted in United States (WEB-Intrasaccular Therapy) and in Europe (WEB Clinical Assessment of Intrasaccular Aneurysm Therapy [WEBCAST], French Observatory, and WEBCAST-2).
OBJECTIVE
To report the 2-yr clinical and anatomical results of WEB treatment in the combined population of 3 European trials.
METHODS
In a French Observatory, 2-yr clinical and anatomical data were collected. In WEBCAST and WEBCAST-2, 2-yr follow-up was optional, and data were collected when follow-up was performed. Aneurysm occlusion was evaluated using a 3-grade scale: complete occlusion, neck remnant, and aneurysm remnant.
RESULTS
The population for safety was 138/168 patients (82.1%), including 89 females (64.5%), with mean age of 55.5 ± 10.2 yr. The population for efficacy was 121/169 aneurysms (71.6%). Aneurysm locations were middle cerebral artery in 65/121 aneurysms (53.7%), anterior-communicating artery in 25/121 (20.7%), basilar artery in 17/121 (14.0%), and internal carotid artery terminus in 14/121 (11.6%). No clinically relevant adverse events occurred between years 1 and 2. At 2 yr, complete occlusion was observed in 62/121 (51.2%) aneurysms, neck remnant in 36/121 (29.8%) aneurysms, and aneurysm remnant in 23/121 (19.0%) aneurysms. The global retreatment rate at 2 yr was 9.3%.
CONCLUSION
This analysis confirms the high safety profile of WEB treatment at 2 yr. Aneurysm occlusion is generally stable at 2 yr, and the retreatment rate between 1 yr and 2 yr is low (2.0%).
Keywords: Aneurysms, Endovascular treatment, Flow disruption, WEB device
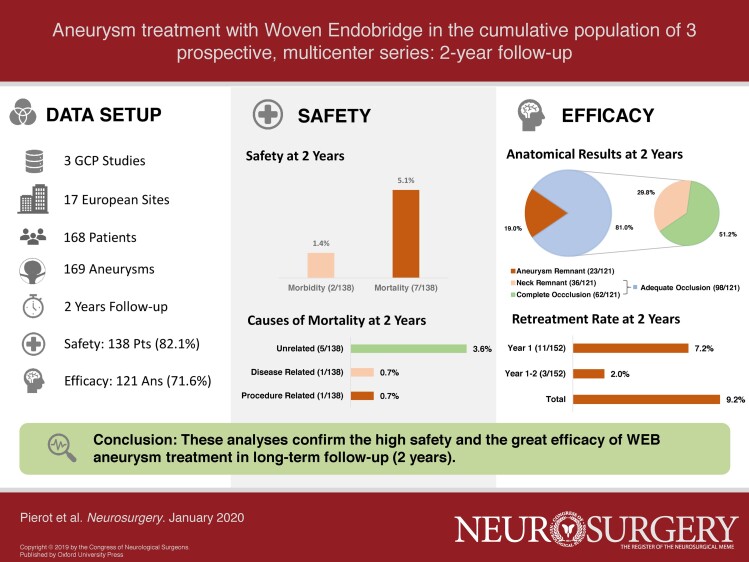
Graphical Abstract
Graphical Abstract.
ABBREVIATIONS
- ACom
anterior communicating artery
- BA
basilar artery
- CI
confidence interval
- CTA
computed tomography angiography
- DSA
digital subtraction angiography
- EVT
endovascular treatment
- GCP
Good Clinical Practice
- ICAt
internal carotid artery terminus
- MCA
middle cerebral artery
- MRA
magnetic resonance angiography
- WEB
Woven EndoBridge
- WEBCAST
Woven EndoBridge Clinical Assessment of Intrasaccular Aneurysm Therapy
- WEB DL
Woven EndoBridge dual layer
The complexity of treating some intracranial aneurysms with coiling and remodeling has led to the development of alternative techniques such as flow diversion and flow disruption.1,2 Flow disruption with Woven EndoBridge (WEB; Sequent Medical) has been evaluated in several single-center and multicenter prospective and retrospective studies, which have shown high safety and efficacy in the short term.3-7 Indeed, since the introduction of this device in Europe in 2010, several studies have been conducted, including 2 European trials (WEB Clinical Assessment of Intrasaccular Aneurysm Therapy [WEBCAST] and WEBCAST-2), 1 trial in the United States (WEB-Intrasaccular Therapy), and 1 French trial (French Observatory), confirming with rigorous methodology the safety and efficacy of this technique.8-13 However, only limited information is available regarding the safety and efficacy of this treatment more than 1 yr following the initial procedure.14 One-year follow-up results from the combined population of the 3 European studies (WEBCAST, WEBCAST-2, and the French Observatory) have recently been published.13 However, all 3 studies followed patients for longer periods of time: 2 yr (French Observatory) and 5 yr (WEBCAST and WEBCAST-2). Therefore, the present paper analyzes the clinical and anatomical results at 2 yr of WEB aneurysm treatment in the combined population of the WEBCAST, French Observatory, and WEBCAST-2 trials. For Clinical Trial Registration (http://www.clinicaltrials.gov), the French Observatory unique identifier is NCT01975233 and the WEBCAST and WEBCAST-2 unique identifier is NCT01778322.
METHODS
WEBCAST, WEBCAST-2, and French Observatory are single-arm, prospective, consecutive, multicenter European and French trials dedicated to evaluating WEB treatment for bifurcation aneurysms.
The 3 trials received national or institutional approval according to each country's regulations. In France, they were approved by Consultative Committee of Information Processing in Healthcare Research Program, Reims Institutional Review Board, and National Commission for Data Processing and Freedom. For all patients, written informed consent was obtained.
WEB Devices
The WEB is a self-expanding, retrievable, nitinol braided device, which is placed within the aneurysm sac and electrothermally detached. During the study time frame, the device existed in several iterations: initially WEB dual layer (WEB DL), followed by single layer in 2 shapes (barrel: WEB SL, and spherical: WEB SLS), followed by a version that enhancing visualization (WEB SL EV and WEB SLS EV) and made from composite wire strands (nitinol and platinum).
In tandem with device evolution, the microcatheters used for the placement of these devices were also evolving. After the initial use (for WEB DL) of Rebar-27 (Covidien, Irvine, California), Headway 27 (MicroVention, Tustin, California), or DAC 038 (Stryker, Fremont, California), specific microcatheters were developed for WEB treatment, including the VIA 33, VIA 27, VIA 21, and VIA 17 (MicroVention/Sequent Medical, Aliso Viejo, California).
Trial Design and Procedural Modalities
Trial design and procedural modalities have been described in previous publications, and all were conducted following Good Clinical Practice (GCP) guidelines.8-11,13 In the 3 studies, ruptured (Hunt and Hess I, II, or III) and unruptured aneurysms located in the basilar artery (BA) apex, middle cerebral artery (MCA) bifurcation, internal carotid artery terminus (ICAt), or anterior communicating artery complex (ACom) were included. In French Observatory, recanalized aneurysms were also included.
At each center, endovascular treatment (EVT) was defined as first-line treatment by a local multidisciplinary team including neurosurgeons and neuroradiologists. Based upon aneurysm characteristics, aneurysms treated with the WEB device were selected in each center by interventional neuroradiologists.
No specific recommendation was made for the perioperative antiplatelet therapy, and antiplatelet activity testing was not a protocol requirement. Selection of the device size was made using 2-dimensional and 3-dimensional digital subtraction angiography (DSA). In WEBCAST, aneurysms were treated with WEB DL, in French Observatory with both WEB DL and WEB SL/SLS, and in WEBCAST-2 with WEB SL/SLS EV. Depending on WEB device size, different microcatheters were used to catheterize the aneurysm (as noted above). No aneurysm was treated with VIA 17. In the French Observatory trial, use of ancillary devices (balloons, coils, and stents) was possible as part of the initial treatment strategy, whereas in WEBCAST and WEBCAST-2, they were used only as a rescue treatment.
Data Collection
The following data were collected for each patient:
Demographics: age and sex.
Aneurysm: rupture status, location, size, and neck size.
Procedure: date, device used (dual layer or single layer), perioperative antiplatelet medications, complications, and use of additional devices during the procedure.
Preoperative Hunt and Hess grade was collected in the case of ruptured aneurysms. Modified Rankin Scale score was gathered before treatment for unruptured and recanalized aneurysms. In addition to clinical follow-up at 30 d (±7 d), clinical and imaging follow-up was mandatory at 1 yr in the 3 studies, at 2 yr in French Observatory, and at 3 and 5 yr in WEBCAST and WEBCAST-2. In these last 2 studies, follow-up at 2 yr and 4 yr was optional, but recommended, and data collected when performed.
Data Analysis
In all 3 studies, independent monitoring of clinical data was performed. Clinical data and all adverse events were independently analyzed by a medical monitor (A.M.). Aneurysm location was independently evaluated on initial angiograms by an expert interventional neuroradiologist (J.V.B.). Aneurysm occlusion was evaluated using a 3-grade scale: complete occlusion, neck remnant, and aneurysm remnant. This evaluation was performed on postoperative DSA and on 1- and 2-yr vascular imaging. Based on Lubicz et al,7 opacification of the proximal recess of the WEB device was considered as complete occlusion. Evolution of aneurysm occlusion between 1 and 2 yr was also evaluated using a 3-grade scale: worse, stable, and improved. Worsening and improvement were defined as a grade change in the 3-grade occlusion scale.
Statistical Analysis
Continuous variables were reported as mean ± standard deviation (SD). Categorical data were described both numerically (categorical total) and as a percentage of the analyzed population. For the binomial data, the ratio of the true value and the analyzed population (x/n) was calculated, and CIs were calculated using the Clopper-Pearson method. The Fisher exact test calculated P-values. Analyses were conducted using SPSS statistical software (IBM, Armonk, New York).
RESULTS
Patient and Aneurysm Population
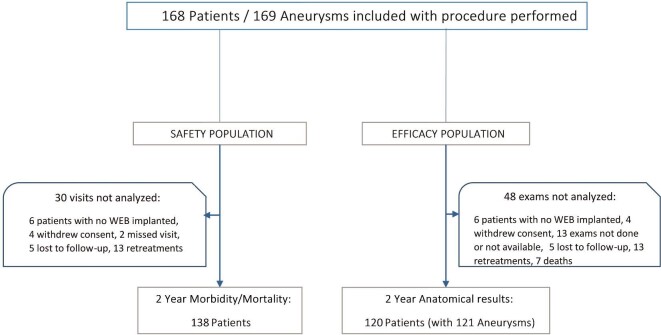
The recruitment periods for the European GCP studies were February 2011 to February 2014 for WEBCAST, November 2012 to January 2014 for French Observatory, and July 2014 to May 2015 for WEBCAST-2. The combined population of the 3 trials was 168 patients and 169 aneurysms.13 The 2-yr follow-up visits were performed between 17 and 39 mo (mean: 24.3 ± 2.5 mo) after the initial procedure. According to the study flow chart (Figure 1), study population for safety included 138/168 patients (82.1%), including 89 females (64.5%), with age range of 30 to 77 yr (mean: 55.5 ± 10.2 yr). Study population for efficacy (Figure 1) included 121/169 (71.6%) aneurysms. Aneurysm status was ruptured in 8/121 (6.6%) and unruptured (or recanalized) in 113/121 (93.4%). Aneurysm locations per core lab analysis were MCA in 65/121 aneurysms (53.7%), ACom in 25/121 (20.7%), BA in 17/121 (14.0%), and ICAt in 14/121 (11.6%). Aneurysm size ranged from 2.8 to 17.0 mm (mean: 7.4 ± 2.0 mm). Aneurysm neck size ranged from 2.4 to 11.0 mm (mean: 5.1 ± 1.4 mm), and the neck was wide (≥4 mm) in 102/121 (84.3%) aneurysms.
FIGURE 1.
Flowchart of the population included in the 3 studies for safety and efficacy at 2 yr.
Treatment was successfully performed in 163/169 aneurysms (96.4%). A WEB DL was implanted in 78/163 aneurysms (47.9%) and WEB SL/SLS in 85/163 aneurysms (52.1%).
Mortality and Morbidity at 2 Years
There were no delayed complications during the 1 to 2-yr period following the initial procedure, with no bleeding, rebleeding, or thromboembolic events observed. At 2 yr, 2/138 (1.4%) patients had morbidity related to the initial procedure (already reported at 1 yr): 1 thromboembolic event related to the WEB procedure and 1 thromboembolic event related to retreatment with a flow diverter. Five deaths were reported at 1 yr: 1 procedure-related (retroperitoneal hematoma), 1 disease-related (brainstem compression by a giant basilar aneurysm), 3 unrelated to aneurysm or procedure (cancer: 2, and cirrhosis: 1). Two deaths unrelated to the aneurysm or the procedure occurred between year 1 and 2 postprocedure (cancer: 1, and pneumonia: 1). Finally, at 2 yr, procedural mortality was 0.7%, mortality related to the disease 0.7%, and unrelated mortality 3.6%.
Anatomical Results at 2 Years
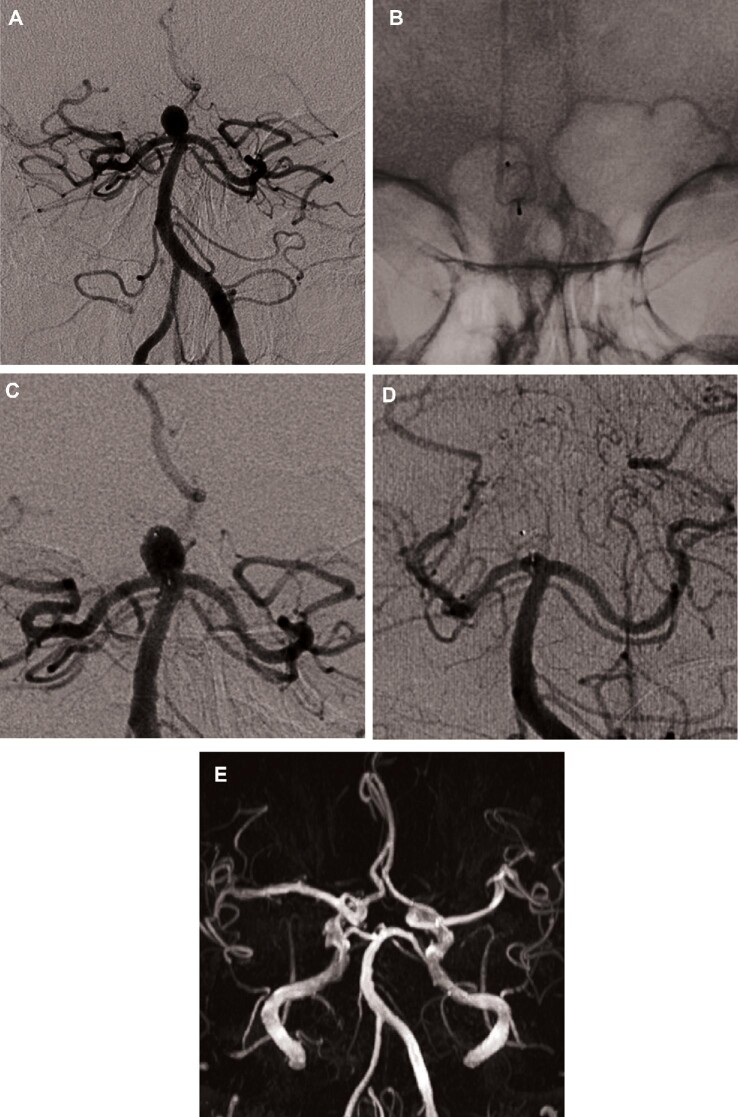
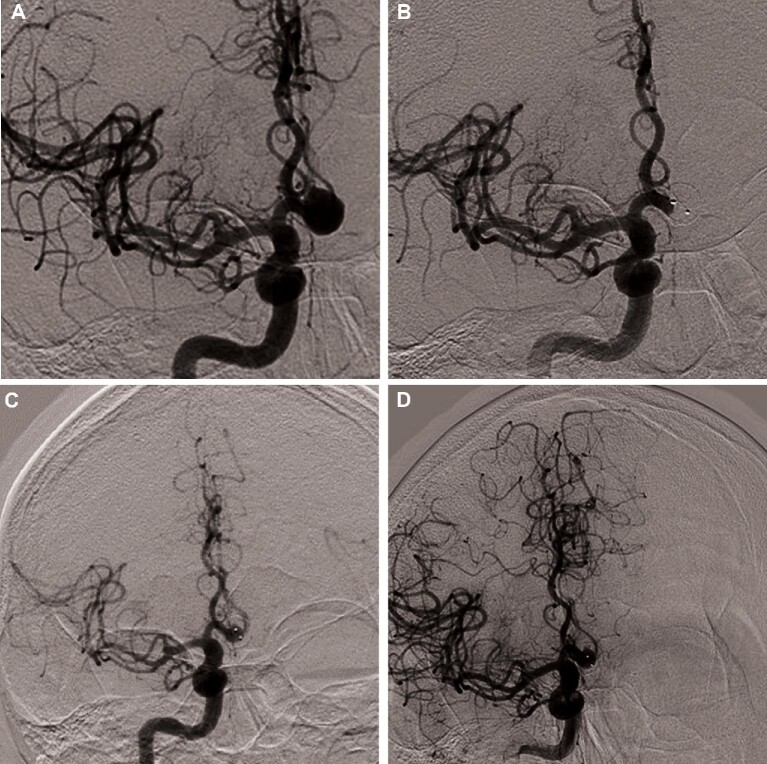
Vascular imaging techniques used included DSA in 51/121 (42.1%), aneurysms, magnetic resonance angiography (MRA) in 57/121 (47.1%) aneurysms, and computed tomography angiography (CTA) in 13/121 (10.7%) aneurysms. At 2 yr, complete occlusion was observed in 62/121 (51.2%) aneurysms (Figure 2), neck remnant in 36/121 (29.8%) (Figure 3), and aneurysm remnant in 23/121 (19.0%) (Figure 4). Adequate occlusion (complete occlusion or neck remnant) was observed in 98/121 (81.0%) aneurysms. Of note, no neck or aneurysm remnant was associated with bleeding/rebleeding during the follow-up period.
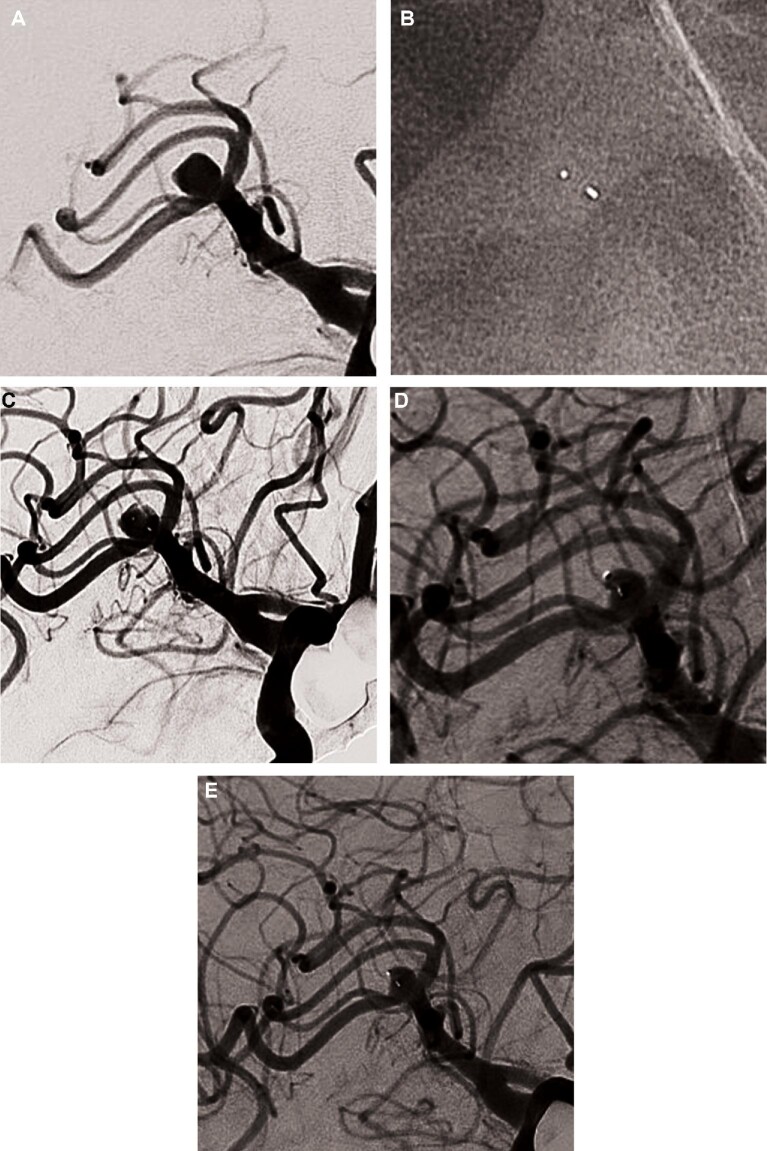
FIGURE 2.
Unruptured basilar tip aneurysm (mean transverse diameter: 6.3 mm; mean height: 6.7 mm; neck: 4.3 mm). A, DSA (frontal view) shows the aneurysm. B and C, Postoperative DSA (unsubstracted and subtracted view, respectively) show the detached WEB device (WEB SL 7 × 4 mm) and residual flow in the aneurysm and the device. D, One-year DSA shows complete aneurysm occlusion. E, Two-year MRA shows stable complete aneurysm occlusion.
FIGURE 3.
Unruptured ACom aneurysm (mean transverse diameter: 8.9 mm; mean height: 9.1 mm; neck: 5.1 mm). A, DSA (frontal view) shows the aneurysm. B, Postoperative DSA shows complete aneurysm occlusion after treatment with WEB SLS 10. C, One-year DSA shows a neck remnant. D, Two-year DSA shows that the neck remnant is stable.
FIGURE 4.
Unruptured MCA aneurysm (mean transverse diameter: 5.1 mm; mean height: 3.5 mm; neck: 5.4 mm). A, DSA, working view, shows the aneurysm. B and C, Postoperative DSA (unsubstracted and subtracted views, respectively) shows the detached WEB device (WEB SL 5 × 3 mm) and residual flow in the aneurysm and the device. D, One-year DS shows an aneurysm remnant. E, Two-year DSA shows a stable aneurysm remnant.
Evolution of aneurysm occlusion was not evaluated in 2 aneurysms because of lack of 1-yr follow-up. Compared with 1-yr aneurysm occlusion, occlusion at 2 yr was improved in 7/119 (5.9%) aneurysms (Figure 5), stable in 96/119 (80.7%), and worsened in 16/119 (13.4%) (Table 1). Worsening of aneurysm occlusion evolved from complete occlusion to neck remnant in 11 (9.2%) aneurysms, complete occlusion to aneurysm remnant in 1 (0.8%) aneurysm, and neck remnant to aneurysm remnant in 4 (3.4%) aneurysms.
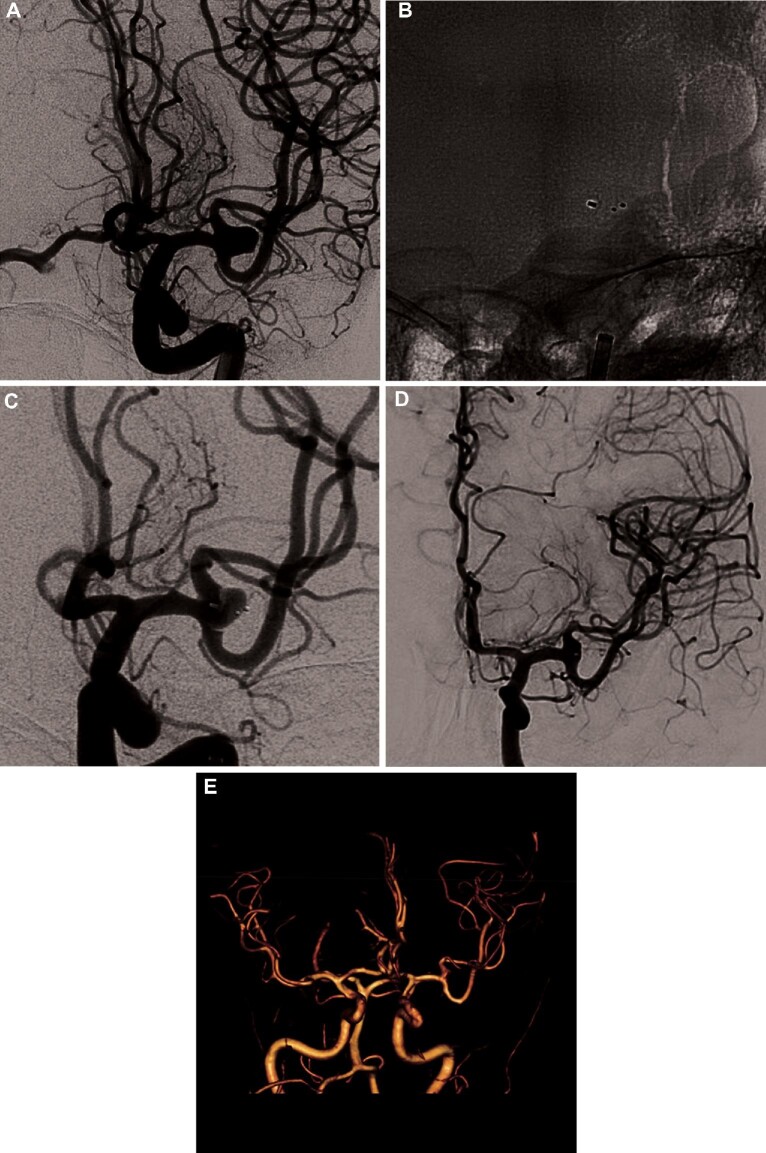
FIGURE 5.
Unruptured MCA aneurysm (mean transverse diameter: 5.8 mm; mean height: 4.8 mm; neck: 6.4 mm). A, DSA, working view, shows the aneurysm. B and C, Postoperative DSA (unsubstracted and subtracted view, respectively) show the detached WEB device (WEB DL 7 × 4 mm) and residual flow in the aneurysm and the device. D, One-year DS shows a neck remnant. E, Two-year DSA shows complete aneurysm occlusion.
TABLE 1.
Evolution of Aneurysm Occlusion Between 1 yr and 2 yr Follow-up
| 2 yr | |||
|---|---|---|---|
| 1 yr | Complete occlusion (n = 62) | Neck remnant (n = 35) | Aneurysm remnant (n = 22) |
| Complete occlusion (n = 67) | 55 (82.1%) | 11 (16.4%) | 1 (1.5%) |
| Neck remnant (n = 34) | 6 (17.6%) | 24 (70.6%) | 4 (11.8%) |
| Aneurysm remnant (n = 18) | 1 (5.6%) | 0 (0.0%) | 17 (94.4%) |
Anatomical Results at 2 Years in Aneurysms Treated With WEB DL and WEB SL/SLS
No significant difference was observed in anatomical results in aneurysms treated with WEB DL and WEB SL/SLS (Table 2).
TABLE 2.
Aneurysm Occlusion at 2 yr in Aneurysms Treated With WEB DL and WEB SL/SLS
| All (n = 121) | WEB DL (n = 63) | WEB SL/SLS (n = 58) | P value | |
|---|---|---|---|---|
| Complete occlusion | 62 (51.2%) | 32 (50.8%) | 30 (51.7%) | .815 |
| Neck remnant | 36 (29.8%) | 18 (28.6%) | 18 (31.0%) | |
| Aneurysm remnant | 23 (19.0%) | 13 (20.6%) | 10 (17.2%) |
Anatomical Results at 2 Years in Different Aneurysm Locations
No significant difference was observed in anatomical results in the different aneurysm locations (Table 3).
TABLE 3.
Aneurysm Occlusion at 2 Yr According to Aneurysm Location
| MCA* (n = 65) | ACom** (n = 25) | BA*** (n = 17) | ICAt**** (n = 14) | |
|---|---|---|---|---|
| Complete occlusion | 34 (52.3%) | 12 (48.0%) | 11 (64.7%) | 5 (35.7%) |
| Neck remnant | 18 (27.7%) | 9 (36.0%) | 5 (29.4%) | 4 (28.6%) |
| Aneurysm remnant | 13 (20.0%) | 4 (16.0%) | 1 (5.9%) | 5 (35.7%) |
P value = .511.
*Middle cerebral artery.
**Anterior communicating artery.
***Basilar artery.
****Internal carotid artery terminus.
Retreatment
The retreatment rate was evaluated in 152 aneurysms. Excluded from this analysis were 6 aneurysms untreated with WEB, 4 aneurysms of 4 patients who withdrew consent, and 7 aneurysms in patients lost to follow-up. A total of 11 (7.2%) aneurysms were retreated (or had a retreatment attempt) between the initial procedure and 1 yr, and 3 (2.0%) between 1 yr and 2 yr, leading to a retreatment rate of 14/152 (9.2%). The retreatment modalities between the initial procedure and 1 yr have previously been described.13 Retreatment between 1 yr and 2 yr was performed with stent and coils in 1 aneurysm, flow diverter in 1 aneurysm, and clipping in 1 aneurysm.
DISCUSSION
The combined population of the 3 WEB trials (WEBCAST, WEBCAST 2, and French Observatory) represents the largest series to date of aneurysm patients treated with the WEB device. Based on 2-yr follow-up data from a large percentage of patients initially included (71.6%), our findings indicate excellent treatment stability with a relatively low rate of retreatment.
Safety and Short-Term Efficacy of WEB Aneurysm Treatment
New EVT techniques are needed for the management of complex aneurysms, such as large and giant aneurysms, as well as wide-neck aneurysms. Indeed, EVT with coils (eventually associated with balloon assistance) of these complex aneurysms is often difficult or is associated with relatively high rates of recanalization. These new EVT techniques must be rigorously evaluated in order to determine their safety as well as efficacy, especially in relation to recanalization. Following several trials conducted in Europe and United States, WEB is an EVT device that has now been extensively studied since its introduction in clinical practice. All studies have shown very high safety, with no mortality and very low morbidity at 1 mo (0.7% in the United States trial and 3.0% in the 3 European trials).8-12 One-year follow-up also showed very good safety and efficacy at preventing bleeding/rebleeding, and anatomic results.13 No delayed neurological adverse events were observed between years 1 and 2. In contrast to what can be observed with intravascular flow diverters, no delayed aneurysm rupture or thromboembolic complications were observed between years 1 and 2.15-17
Mid- and Long-Term Follow-Up in Studies Evaluating Aneurysm EVT
Most large aneurysm studies (eg, analysis of treatment by endovascular approach of non ruptured aneurysms, clinical and anatomic results in the treatment of ruptured intracranial aneurysms, and hydrocoil endovascular aneurysm occlusion and packing study) do not have follow-up beyond 1 yr.18-20 International Subarachnoid Aneurysm Trial has very long-term clinical follow-up, but does not evaluate aneurysm occlusion.21 However, efficacy of an EVT technique must be evaluated not only in the short term, but also in mid and long term. In the 3 European WEB studies, mid- and long-term follow-up was carried out with follow-up at 2 yr in French Observatory and 3 and 5 yr in WEBCAST and WEBCAST-2 (in these 2 studies, follow-up at 2 yr was only recommended). Although not mandatory in WEBCAST and WEBCAST-2, a high percentage of the aneurysm population of the 3 trials had a 2-yr imaging follow-up (71.6%).
WEB Aneurysm Treatment: 2-Year Anatomical Follow-up
Interestingly, 2-yr anatomical results are quite similar to those at 1-yr, showing great stability of treatment. Complete aneurysm occlusion was observed in 51.2% (52.9% at 1 yr), neck remnant in 29.8% (26.2% at 1 yr), and aneurysm remnant in 19.0% (20.9% at 1 yr) leading to adequate occlusion in 81.0%. Worsening of aneurysm occlusion was reported between 1 and 2 yr follow-up in 13.4%; in the majority of cases (9.2%) the aneurysm evolved from complete occlusion to neck remnant. Similar good results were previously reported in a small, retrospective European series.14 Indeed, the percentages of complete and adequate occlusion can be regarded as relatively low, but the 3 European GCP studies were conducted since the introduction of the WEB device in the clinical field (see recruitment periods above), so during the learning curve of the participating physicians. At the beginning of the experience, it was also not known that it was necessary to oversize the device in width to improve the stability of the treatment. Moreover, 47.9% of aneurysms included in the studies were treated with the first generation of the WEB device (WEB DL), which was more difficult to navigate and properly place in the aneurysm sac. Future WEB studies will probably report better anatomical results.
Compared Efficacy of WEB DL and WEB SL/SLS
The WEB device design has significantly changed since its introduction in clinical practice in Europe in 2010. One major evolution was from WEB DL to single-layer device (WEB SL and WEB SLS). The advantages of single-layer devices were numerous, including improved navigability and superior softness and conformability of the device. Notwithstanding these changes, it was important to determine if single-layer device efficacy was equal to that of dual-layer devices. Whereas WEBCAST included patients treated with WEB DL devices, WEBCAST-2 included patients treated with WEB SL or SLS devices, and French Observatory treated patients with both device types; it was therefore possible to analyze aneurysm occlusion according to device type used (Table 1). Results confirm a similar percentage of complete occlusion with both types of devices (WEB DL: 50.8%; WEB SL/SLS: 51.7%) as well as of adequate occlusion (WEB DL: 79.4%; WEB SL/SLS: 82.7%). Analysis according to aneurysm location also did not show significant difference (Table 2), even with tendency to have a higher percentage of aneurysm remnant in ICAt aneurysms (35.7%) and a lower percentage in BA aneurysms (5.9%) compared with MCA and ACom aneurysms (20.0% and 16.0%, respectively).
Comparison of WEB Treatment With Other Aneurysm Treatments
Given that most multicenter series with an independent core lab evaluation do not have follow-up beyond 1 yr (as noted above), comparing the present anatomical results with those of alternate EVT techniques is challenging. Additionally, the present series is dedicated to wide-neck bifurcation aneurysms and is not comparable to coiling series that include all types of aneurysms, including narrow-neck and sidewall. Moreover, our study is also not comparable to flow diverter series that usually include a high proportion of large and giant aneurysms that are not indications for the WEB device. A comparison is feasible with the MAPS (Matrix and Platinum Science) Trial—even though it only has a 1-yr follow-up—but includes a subgroup analysis for wide-neck aneurysms.22 In wide-neck aneurysms treated exclusively with coils, aneurysm occlusion at 1-yr was complete in 27.1%, neck remnant in 30.5%, and aneurysm remnant in 42.4%; in contrast, aneurysms treated with coils and stent, aneurysm occlusion at 1 yr was complete in 45.7%, neck remnant in 17.1%, and aneurysm remnant in 37.1%. These results are clearly inferior when compared to WEB (aneurysm remnant: 19.0%) results obtained in the present series.
Comparison with clipping is relatively difficult, because, in most surgical series, postoperative aneurysm occlusion is not evaluated as reported in Kotowski et al23 meta-analysis (aneurysm occlusion was not evaluated in 82.2% of all collected aneurysms). In all collected cases, no long-term aneurysm occlusion evaluation was available.
Retreatment Rate
At 2 yr, the global rate of retreatment from initial procedure was 9.2% of aneurysms, with the majority of retreatment completed prior to 1 yr. Several treatment modalities were used, including stent-assisted coiling, flow diversion, and clipping, as reported in previous series.24,25 Rates of retreatment are difficult to compare from one series to another given variable indications for retreatment.26 However, the rate of retreatment in wide-neck aneurysms is 13.7% in aneurysms treated with coils and 14.1% in aneurysms treated by stent-assisted coiling in the MAPS trial.22
Limitations
This study has several limitations. First, it is not a randomized study, and comparison with other techniques is difficult. However, the study does provide the largest series of patients with aneurysms treated with WEB to date, demonstrating the device's good safety and efficacy (at midterm follow-up). Second, imaging modalities used for the 2-yr follow-up were heterogeneous and included DSA, MRA, and CTA. Additionally, MRA has been shown to have some limitations in the evaluation of aneurysm occlusion in case of WEB treatment.27 However, we have to acknowledge that patients are often reluctant to undergo DSA. Moreover, we have to acknowledge that what is difficult to depict with MRA is contrast in the device that has probably not the same clinical impact than aneurysm or neck remnant. Third, potential change of WEB device shape as reported by Cognard et al28 was not evaluated, thus making it impossible to evaluate its potential influence on anatomical results. Indeed, the analysis conducted in a recent series showed that there is no relation between WEB shape modification and anatomical results.29 Fourth, follow-up was not obtained in all patients/aneurysms. Safety was effectively evaluated in 82.1% of patients when efficacy was evaluated in 71.6% of aneurysms.
Generalizability
This analysis is the first to report 2-yr anatomical results in a population of patients with aneurysms treated with WEB and collected in GCP studies. Additional series are necessary to further analyzed long-term efficacy of WEB aneurysm treatment taking into account the most recent technical developments (see Methods).
CONCLUSION
This analysis of the combined population of 3 European WEB trials (WEBCAST, French Observatory, and WEBCAST-2) confirms the high safety of this treatment with no additional morbidity between years 1 and 2. In addition, the study confirms high efficacy of the treatment at long-term follow-up with anatomical results similar to those at 1-yr and low retreatment rate between years 1 and 2.
Longer follow-up (3 and 5 yr) will be provided in WEBCAST and WEBCAST-2.
Disclosures
WEBCAST, WEBCAST-2, and French Observatory were funded by Sequent. Dr Pierot is a consultant for Balt, MicroVention, Neuravi, Penumbra, and Phenox. Dr Moret is a consultant for Medtronic, MicroVention, Stryker, and Balt. Dr Barreau is a consultant for MicroVention and Stryker. Dr Szikora is a consultant for Codman, Medtronic, Sequent, and Stryker. Dr Costalat is a consultant for MicroVention and Balt and received educational grants from Medtronic and Stryker. Dr Fiehler has received fees as a consultant or lecturer from Acandis, Bayer, Boehringer-Ingelheim, Codman, Covidien, MicroVention, Penumbra, Philips, Sequent, Siemens, and Stryker; his institution received funding from MicroVention, Medtronic, BMBF, BMWi, DFG, and the EU. Dr Klisch is a consultant for MicroVention/Sequent. Dr Weber is a consultant for MicroVention, Phenox, and Medtronic. Dr Liebig is a consultant for Medtronic, Mentice, Microvention, and Route 92. Dr Molyneux is a consultant for MicroVention/Sequent and Cerus Endovascular. Dr Byrne is a consultant and shareholder for Oxford Endovascular Ltd; his institution received funding from MicroVention. Dr Spelle is a consultant for Stryker, MicroVention, Medtronic, and Balt.
Notes
This work, the 2-year follow-up results of the 3 European WEB GCP studies, was previously presented as an oral presentation at the 46th Congress of the French Society of Neuroradiology on March 27-29, 2019, in Paris, France, and as an oral presentation at the 11th Society of NeuroInterventional Surgery on July 22-25, 2019, in Miami, Florida.
Contributor Information
Laurent Pierot, Department of Neuroradiology, Hôpital Maison-Blanche, Université Reims-Champagne-Ardenne, Reims, France.
Jacques Moret, Department of Neuroradiology, Hôpital Bicêtre, Assistance Publique-Hôpitaux de Paris, Paris, France.
Xavier Barreau, Department of Neuroradiology, CHU Bordeaux, Bordeaux, France.
Istvan Szikora, Department of Neuroradiology, National Institute of Clinical Neurosciences, Budapest, Hungary.
Denis Herbreteau, Department of Neuroradiology, CHU Tours, Tours, France.
Francis Turjman, Department of Neuroradiology, CHU Lyon, Lyon, France.
Markus Holtmannspötter, Department of Neuroradiology, Rigshospitalet, Copenhagen, Denmark.
Anne-Christine Januel, Department of Neuroradiology, CHU Toulouse, Toulouse, France.
Vincent Costalat, Department of Neuroradiology, CHU Montpellier, Montpellier, France.
Jens Fiehler, Department of Neuroradiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany.
Joachim Klisch, Department of Neuroradiology, Helios General Hospital, Erfurt, Germany.
Jean-Yves Gauvrit, Department of Neuroradiology, CHU Rennes, Rennes, France.
Werner Weber, Department of Neuroradiology, Universitätsklinikum Knappschaftskrankenhaus Bochum GmbH, Bochum, Germany.
Hubert Desal, Department of Neuroradiology, CHU Nantes, Nantes, France.
Stéphane Velasco, Department of Neuroradiology, CHU Poitiers, Poitiers, France.
Thomas Liebig, Institut of Neuroradiology, Ludwig-Maximilian University Hospital, Munich, Germany.
Luc Stockx, Department of Neuroradiology, ZOL (Ziekenhuis Oost-Limburg) Genk, Genk, Belgium.
Joachim Berkefeld, Department of Neuroradiology, Institut für Neuroradiologie, Klinikum der Johann Wolfgang Goethe-Universitaet, Frankfurt, Germany.
Andrew Molyneux, Department of Neuroradiology, Nuffield Department of Surgical Sciences, Oxford University, Oxford, United Kingdom.
James V Byrne, Department of Neuroradiology, Nuffield Department of Surgical Sciences, Oxford University, Oxford, United Kingdom.
Laurent Spelle, Department of Neuroradiology, Hôpital Bicêtre, Assistance Publique-Hôpitaux de Paris, Paris, France.
Neurosurgery Speaks! Audio abstracts available for this article at www.neurosurgery-online.com.
COMMENT
Innovation is key in endovascular neurosurgery. In many instances, endovascular treatment of intracranial aneurysms is limited by the available technology; however, those instances are decreasing given the continued development of embolic devices in this field. This current study illustrates this concept well. Presently, the authors analyze the 2-year results of 3 European trials evaluating the WEB (Woven EndoBridge) device in treating intracranial aneurysms. The results suggest good efficacy (81% complete occlusion or neck remnant) with acceptable 2-year retreatment rates (9.3%). There were no instances of long-term procedure-related morbidity or mortality. Perhaps most importantly, there was no cases of hemorrhage after treatment with WEB.
Introduction of the WEB device has facilitated treatment of a subset of intracranial aneurysms (ie, giant, wide-neck, or bifurcation aneurysms) for which there was previously no straightforward treatment option. Given the wide diversity of aneurysm size and morphology, a wide armamentarium of endovascular treatment modalities is necessary. The results of this report suggest that WEB remains a valid endovascular option for treatment of select intracranial aneurysms, with long-term results comparable to other endovascular techniques.
Kurt Yaeger
J Mocco
New York, New York
Neurosurgery Speaks (Audio Abstracts)
Listen to audio translations of this paper's abstract into select languages by choosing from one of the selections below.
REFERENCES
- 1.Pierot L, Wakhloo AK. Endovascular treatment of intracranial aneurysms. Stroke. 2013;44(7):2046-2054. [DOI] [PubMed] [Google Scholar]
- 2.Pierot L, Biondi A. Endovascular techniques for the management of wide-neck intracranial bifurcation aneurysms: a critical review of the literature. J Neuroradiol. 2016;43(3):167-175. [DOI] [PubMed] [Google Scholar]
- 3.Pierot L, Liebig T, Sychra Vet al.. Intrasaccular flow disruption: a new endovascular approach for the treatment of intracranial aneurysms. Results of a preliminary clinical evaluation in a multicenter series. AJNR Am J Neuroradiol. 2012;33(7):1232-1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pierot L, Klisch J, Cognard Cet al.. Endovascular WEB flow disruption in middle cerebral artery aneurysms. Neurosurgery. 2013;73(1):27-35. [DOI] [PubMed] [Google Scholar]
- 5.Papagiannaki C, Spelle L, Januel ACet al.. Flow disruption with WEB device: report of a prospective, multicenter series of 83 patients with 85 aneurysms. AJNR Am J Neuroradiol. 2014;35(11):2006-2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mine B, Pierot L, Lubicz B. Intrasaccular flow-diversion for treatment of intracranial aneurysms: the Woven EndoBridge. Expert Rev Med Devices. 2014;11(3):315-325. [DOI] [PubMed] [Google Scholar]
- 7.Lubicz B, Klisch J, Gauvrit JYet al.. WEB-DL endovascular treatment of wide-neck bifurcation aneurysms: short- and midterm results in a european study. AJNR Am J Neuroradiol. 2014;35(3):432-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pierot L, Moret J, Turjman Fet al.. WEB treatment of intracranial aneurysms: feasibility, complications, and 1-month safety results with the WEB DL and WEB SL/SLS in the French Observatory. AJNR Am J Neuroradiol. 2015;36(5):922-927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pierot L, Costalat V, Moret Jet al.. Safety and efficacy of aneurysm treatment with WEB: results of the WEBCAST study. J NeuroIntervent Surg. 2016;124(5):1250-1256. [DOI] [PubMed] [Google Scholar]
- 10.Pierot L, Moret J, Turjman Fet al.. WEB treatment of intracranial aneurysms: clinical and anatomic results in the French Observatory. AJNR Am J Neuroradiol. 2016;37(4):655-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pierot L, Gubucz I, Buhk JHet al.. Safety and efficacy of aneurysm treatment with the WEB: results of the WEBCAST 2 study. AJNR Am J Neuroradiol. 2017;38(6):1151-1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fiorella D, Molyneux A, Coon Aet al.. Demographic, procedural and 30-day safety results from the WEB intra-saccular therapy study (WEB-IT). J NeuroIntervent Surg. 2017;9(12):1191-1196. [DOI] [PubMed] [Google Scholar]
- 13.Pierot L, Moret J, Barreau Xet al.. Safety and efficacy of aneurysm treatment with WEB in the cumulative population of three prospective, multicenter series. J NeuroIntervent Surg. 2018;10(6):553-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pierot L, Klisch J, Liebig Tet al.. WEB-DL endovascular treatment of wide-neck bifurcation aneurysms: long-term results in a European series. AJNR Am J Neuroradiol. 2015;36(12):2314-2319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Macdonald IR, Shankar JJS. Delayed parent artery occlusions following use of silk flow diverters for treatment of intracranial aneurysms. J Neurointerv Surg. 2018;11(7):690-693. [DOI] [PubMed] [Google Scholar]
- 16.Klisch J, Turk A, Turner R, Woo HH, Fiorella D. Very late thrombosis of flow-diverting constructs after the treatment of large fusiform posterior circulation aneurysms. AJNR Am J Neuroradiol. 2011;32(4):627-632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guedon A, Clarençon F, Di Maria Fet al.. Very late ischemic complications in flow-diverter stents: a retrospective analysis of a single-center series. J NeuroIntervent Surg. 2016;125(4):929-935. [DOI] [PubMed] [Google Scholar]
- 18.Cognard C, Pierot L, Anxionnat R, Ricolfi F. Clarity Study group. Results of embolization used as the first treatment choice in a consecutive nonselected population of ruptured aneurysms: clinical results of the Clarity GDC study. Neurosurgery. 2011;69(4):837-842. [DOI] [PubMed] [Google Scholar]
- 19.Pierot L, Spelle L, Vitry F. for the ATENA investigators. Immediate clinical outcome of patients harboring unruptured intracranial aneurysms treated by endovascular approach. Stroke. 2008;39(9):2497-2504. [DOI] [PubMed] [Google Scholar]
- 20.White PM, Lewis SC, Gholkar Aet al.. Hydrogel-coated coils versus bare platinum coils for the endovascular treatment of intracranial aneurysms (HELPS): a randomised controlled trial. Lancet North Am Ed. 2011;377(9778):1655-1662. [DOI] [PubMed] [Google Scholar]
- 21.Molyneux A, Kerr RSC, Birks J. for the ISAT investigators. Risk of recurrent subarachnoid haemorrhage, death, or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): long-term follow-up. Lancet Neurol. 2009;8(5):427-433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hetts SW, Turk A, English JDet al.. Stent-assisted coiling versus coiling alone in unruptured intracranial aneurysms in the matrix and platinum science trial: safety, efficacy, and mid-term outcomes. Am J Neuroradiol. 2014;35(4):698-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kotowski M, Naggara O, Darsaut TEet al.. Safety and occlusion rates of surgical treatment of unruptured intracranial aneurysms: a systematic review and meta-analysis of the literature from 1990 to 2011. J Neurol Neurosurg Psychiatry. 2013;84(1):42-48. [DOI] [PubMed] [Google Scholar]
- 24.Kabbasch C, Goertz L, Siebert Eet al.. Treatment strategies for recurrent and residual aneurysms after Woven Endobridge implantation. J NeuroIntervent Surg. 2019;11(4):390-395. [DOI] [PubMed] [Google Scholar]
- 25.Pierot L, Bannery C, Batchinsky-Parrou V, Kleiber JC, Soize S, Litré F. Clipping of recanalized intracerebral aneurysms initially treated by WEB device. J NeuroIntervent Surg. published online: 2019(doi:10.1136/neurintsurg-2019-014903). [DOI] [PubMed] [Google Scholar]
- 26.Turk AS, Johnston SC, Hetts Set al.. Geographic differences in endovascular treatment and retreatment of cerebral aneurysms. AJNR Am J Neuroradiol. 2016;37(11):2055-2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Timsit C, Soize S, Benaissa A, Portefaix C, Gauvrit JY, Pierot L. Contrast-enhanced and time-of-flight mra at 3t compared with DSA for the follow-up of intracranial aneurysms treated with the WEB device. AJNR Am J Neuroradiol. 2016;37(9):1684-1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cognard C, Januel AC. Remnants and recurrences after the use of the WEB intrasaccular device in large-neck bifurcation aneurysms. Neurosurgery. 2015;76(5):522-530. [DOI] [PubMed] [Google Scholar]
- 29.Herbreteau D, Bibi R, Narata APet al.. Are anatomic results influenced by WEB shape modification? Analysis in a prospective, single-center series of 39 patients with aneurysms treated with the WEB. AJNR Am J Neuroradiol. 2016;37(12):2280-2286. [DOI] [PMC free article] [PubMed] [Google Scholar]