Abstract
Purpose
The COVID-19 pandemic and related lockdown measures drastically changed health care and emergency services utilization. This study evaluated trends in emergency department (ED) access for seizure-related reasons in the first 8 weeks of lockdown in Italy.
Methods
All ED accesses of children (<14 years of age) at two university hospitals, in Turin and Rome, Italy, between January 6, 2020 and April 21, 2020, were examined and compared with the corresponding periods of 2019.
Results
During the COVID-19 lockdown period (February 23-April 21, 2020), there was a 72 % decrease in all pediatric ED accesses over the corresponding 2019 period (n = 3,395 vs n = 12,128), with a 38 % decrease in seizure-related accesses (n = 41 vs n = 66). The observed decrease of seizure-related ED accesses was not accompanied by significant changes in age, sex, type of seizure, or hospitalization rate after the ED visit.
Conclusion
The COVID-19 lockdown was accompanied by a sudden decrease in seizure-related hospital emergency visits. School closure, social distancing, reduced risk of infection, and increased parental supervision are some of the factors that might have contributed to the finding.
Keywords: Covid-19, Children, Seizure, Epilepsy, Emergency, Child neurology
1. Introduction
The coronavirus disease (COVID-19) pandemic abruptly changed life worldwide with profound implications for healthcare delivery [1]. Italy was the first European country to be struck by COVID-19. On February 23, 2020, in an effort to contain the contagion, schools were closed, followed by all non-essential businesses and services, so that the entire Italian population was put on a strict lockdown [2,3]. The impact on health care services was dramatic, with rapid redirection of resources to the management of COVID-19 patients, postponement of all non-urgent care, suspension of routine outpatient services, and significant decrease in hospital utilization for conditions other than COVID-19 [4,5]. However, access to hospital emergency departments (ED) for severe medical conditions such as seizures would not be expected to change.
We here report on a significant decrease in ED accesses for pediatric seizure-related reasons at two pediatric hospitals in Turin and Rome, Italy, during the first 8 weeks of the COVID-19 related lockdown.
2. Methods
All ED accesses by children under 14 years of age at two university hospitals in Italy (Regina Margherita Pediatric Hospital in Turin and Policlinico Umberto I University Hospital in Rome) between January 6 and April 19, 2020, and the corresponding period in 2019 (January 7 – April 21) were examined. The combined catchment area of the two hospitals is about 3 million people. All visits requiring a child neurologist consult were identified and manually reviewed for seizure-related conditions [6]. Seizure-related ED accesses were sub-grouped into five categories: status epilepticus, febrile seizure (including febrile status epilepticus), seizure in patient without a diagnosis of epilepsy, recurrence of seizure in patients with diagnosis of epilepsy, and paroxysmal movements [7]. Patients with known psychogenic non-epileptic seizures (PNES) were excluded (only 1 case of PNES was present in the first period of 2020). Hospital inpatient admission subsequent to ED access was recorded as an index of clinical relevance and severity.
Based on the date of February 24, when the COVID-19 lockdown began, the two periods (January 6 - April 19, 2020 and January 7 - April 21, 2019) were divided into two intervals each: “pre-COVID-19” (i.e., until February 23, 2020 or February 24, 2019) and “post-COVID-19” afterwards. For both 2019 and 2020, the period of observation was of 15 weeks (thus explaining why the period ends on April 19 in 2020 and on April 21 in 2019). The study was approved by the institutional ethics committee. The data were anonymously recorded and analyzed.
2.1. Statistical analysis
Weekly ED access counts were modeled using a Poisson regression model. A COVID-19-related covariate assumed the value of 0 until February 23 and the value of 1 thereafter in order to evaluate the impact of the COVID-19 lockdown. The same model, with an offset equivalent to the logarithm of all ED accesses per week, was used to evaluate the trend in seizure-related ED accesses adjusting by total ED accesses. Non-parametric statistics (chi-square test, with Williams’s correction when appropriate, and Mann-Whitney U test) were used to test for differences in demographics and clinical variables between the observed time-intervals. Alpha was set at two-tailed 0.05.
3. Results
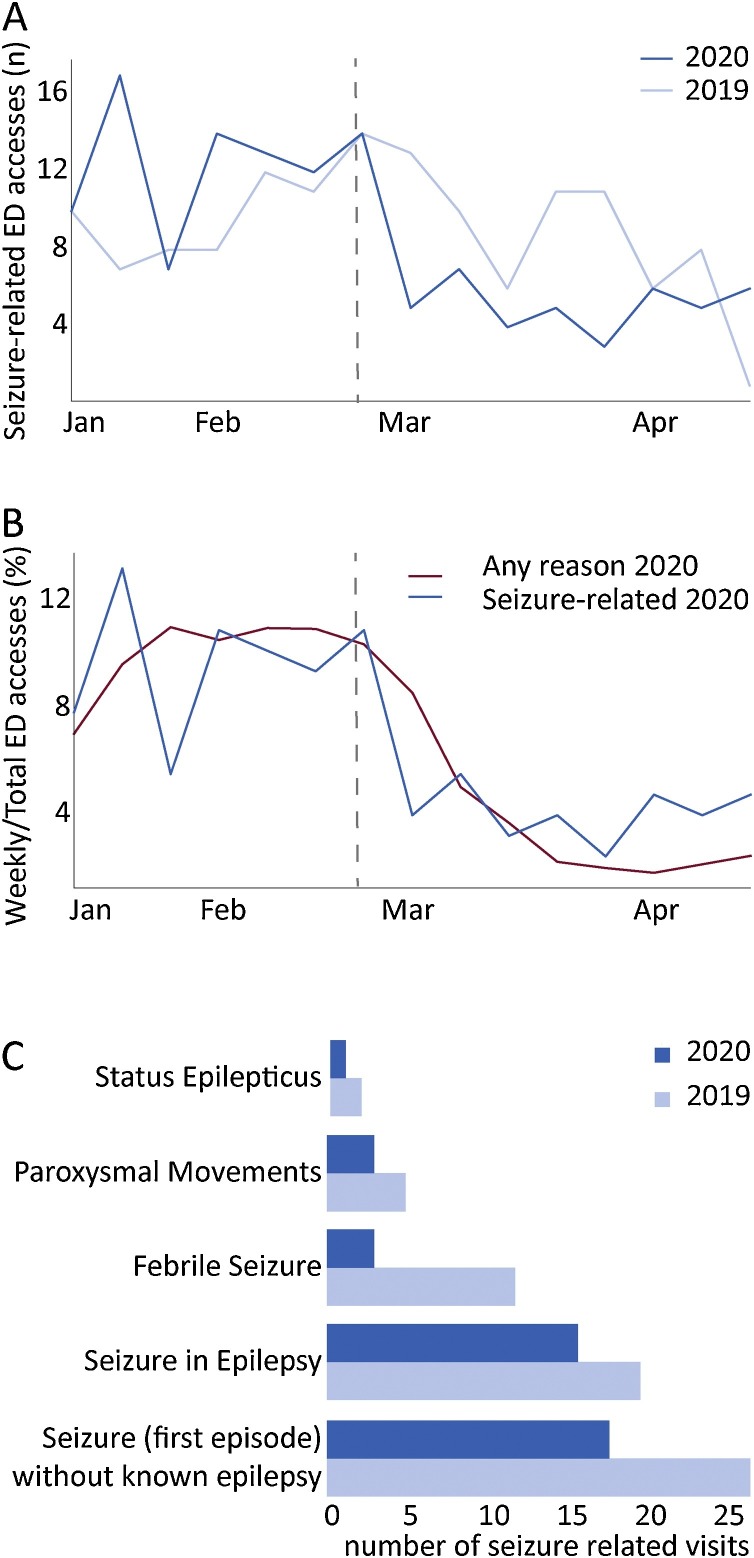
Total pediatric ED accesses for any reason were n = 14,239 between January 6 and April 19, 2020, and n = 23,016 during the corresponding period in 2019. Among these, seizure-related ED accesses were n = 128 in 2020 vs. n = 136 in 2019. Mean age was 5.77 ± 4.31 years in 2020 (SD: 4.31; median: 4.94, IQR: 2.01–9.05) and 6.38 ± 4.26 years (median: 6.53, IQR: 2.38–9.89) in 2019. Males were 55 % in 2020 and 45 % in 2019. Weekly seizure-related ED visits decreased after February 23, 2020 over the previous weeks in 2020 and compared with the corresponding period of 2019 (Fig. 1 A). Specifically, in the Poisson regression model, the COVID-19 lockdown factor was associated with a 59 % decrease in seizure-related accesses compared to the corresponding period of 2019 (41 visits in the second interval in 2020 vs 66 in 2019, p < 0.001, Table 1 ).
Fig. 1.
A: Weekly number of seizure-related visits in the observed periods of 2019 and 2020. B: Weekly percentage distribution of seizure-related visits and ED pediatric accesses (weekly seizure-related visits over total seizure related visits of the entire period, blue; weekly ED pediatric accesses over ED pediatric accesses of the entire period, red) in observed period in 2020. C: Percentage distribution of type of seizure event during the COVID-19 period in (2nd interval 2020). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
Table 1.
Impact of COVID-19 lockdown on ED visits for seizure-related events.
| Outcome - number of n visits per week |
||
|---|---|---|
| Comparison | IRR | 95 % CI |
| 2nd interval 2020 vs 1st interval 2020 | 0.41 | 0.28 - 0.59 |
| 2nd interval 2020 vs 2nd interval 2019 | 0.41 | 0.28 - 0.58 |
| 2nd interval 2020 vs 1st interval 2020 (adjusted by ED total) | 1.51 | 1.03–2.17 |
| 2nd interval 2020 vs 2nd interval 2019 (adjusted by ED total) | 1.53 | 1.05–2.19 |
IRR: incidence rate ratio.
Total pediatric ED accesses were n = 3,395 (2,326 in Turin and 1,069 in Rome) in the COVID-19 period, a 3.6-fold decline over the corresponding period of 2019 (n = 12,128, 7630 in Turin and 4,498 in Rome). Seizure-related ED accesses accounted for a larger proportion of all ED pediatric accesses during the COVID-19 period (xx%) as compared to the corresponding period of 2019 (xy%). In the Poisson regression model, the COVID-19 lockdown factor was associated with an incidence rate ratio (IRR) 0.41 (95 % CI 0.28 – 0.59) compared to the 2019 period (Table 1, Fig. 1B).
The distribution of seizure type did not show statistically significant changes in the COVID-19 lockdown (Fig. 1C), χ2 = 2.78 (df = 4), p = 0.60. In particular, 39 % of all seizure-related accesses were for seizures in patients already diagnosed with epilepsy (vs 30 % in the corresponding period of 2019), 44 % for seizures in patients without a diagnosis of epilepsy (vs 41 % in 2019), 7% for febrile seizures (vs. 18 % in 2019), 7% for paroxysmal events (vs. 7% in 2019), and 2 % for status epilepticus (vs. 3 % in 2019).
The rate of hospitalization following the ED visit did not significantly change during the COVID-19 lockdown (49 % vs 50 % in 2019). No sex or age differences were found between 2020 and 2019 accesses.
4. Discussion
We observed a 38 % decrease in ED accesses for seizure-related reasons during the COVID-19 lockdown period compared with the corresponding 2019 time-period. This decrease was less marked than the 72 % decline in all ED pediatric accesses, a difference that underscores the clinical relevance of seizures as medical emergency. In fact, the proportion of total ED accesses due to seizures increased by 51 % over 2019 (Table 1). Hospitalization rate following the ED visit, a possible index of clinical severity, did not significantly change, suggesting that there was not a self-selection based on advanced care needs.
A general reduction in ED use can be expected at a time of pandemic and in part ascribed to avoidance of hospital settings for fear of contagion. Under these circumstances, inappropriate use of ED services for non-urgent care is likely to decrease. Concern has been raised, however, that the COVID-19 crisis might have resulted in the opposite problem of ED underuse, with hospital avoidance even in cases of serious medical problems [4,5]. In fact, one would not expect a reduction of urgent care for conditions such as newly onset seizures. Thus, the observed decrease appears puzzling and not fully explained by known contextual variables.
A seasonality in seizure-related events is expected, being linked to the seasonality of common infections such as influenza [8]. Thus, incidence of febrile seizures is higher [9,10]. However, the observed decrease in ED accesses for seizure-related reasons during the COVID-19 lockdown greatly exceeds the seasonally expected reduction, and is also evident when it is compared with the corresponding 2019 time-period. The reduction in ED seizure-related accesses could be in part explained by a possible decrease in infections since the COVID-19 lockdown greatly curtailed social contacts by closing schools, prohibiting group activities and imposing social distancing.
More difficult to explain is the dramatic reduction in ED accesses for seizures not apparently linked to infections. Did the incidence of seizures in fact decline during the COVID-19 lockdown through still unknown mechanisms? A few hypotheses can be formulated about possible mechanisms of seizure reduction in patients with epilepsy. As the lockdown resulted in closure of most work activities, the time parents spent at home with their children increased and this could have resulted in better supervision and medication compliance [11]. Also, school closure could have reduced sleep deprivation, a risk factor for seizures.
Alternatively, did the incidence remain unchanged but children with seizures were not brought to hospital EDs and instead managed at home or in other settings? School closure might have increased home management of seizures by parents. That seizures were managed in other non-hospital medical settings seems to be unlikely. During the lockdown access to medical offices and outpatient clinics was greatly reduced. Outpatient offices appear in any case to be unwieldy settings for managing seizures. The possibility that more patients were treated at other, smaller and lower-volume hospitals may be considered. However, access to these local hospitals, which typically serve both adults and children, would have entailed a higher COVID-19 exposure risk than tertiary-care pediatric facilities. In fact, some of these smaller hospitals became COVID-19 wards during the pandemic acute phase. For these reasons, it seems unlikely that parents preferred small hospitals for their children with acute seizures.
Telemedicine has been increasingly used for a variety of clinical issues, but seems an unlikely means for managing status epilepticus or newly onset seizures. At our hospitals, we did not notice a higher volume of phone or online contacts for neurologic emergencies. In a few cases, telemedicine helped to instruct parents on the value of ED assessment as seizure-related risks outweighed COVID-19 exposure risk.
Thus the question remains why so many children with seizures seem to have suddenly disappeared. Trying to answer this question may shed light on still unknown risk and protective factors for developing seizures and possibly help identify alternative ways of managing these emergencies.
Ethical publication statement
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Declaration of Competing Interest
In last 2 years, BV was a paid consultant for Medice Pharmaceuticals, Lundbeck Pharmaceuticals, Alkermes Co., and lawfirms Goodwin & Procter, Haynes & Boone. None of the other authors have any conflict of interest to disclose.
References
- 1.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . 2020. Coronavirus disease 2019. Situation report – 114. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200513-covid-19-sitrep-114.pdf?sfvrsn=17ebbbe_4. Accessed 8 September 2020. [Google Scholar]
- 3.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4(5):e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Filippo O., D’Ascenzo F., Angelini F., Angelini F., Bocchino P.P., Conrotto F., et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383(1):88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fisher R.S., Acevedo C., Arzimanoglou A., Bogacz A., Cross J.H., Elger C.E. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55(4):475–482. doi: 10.1111/epi.12550. [DOI] [PubMed] [Google Scholar]
- 7.Lüders H., Vaca G.F., Akamatsu N., Amina S., Arzimanoglou A., Baumgartner C., et al. Classification of paroxysmal events and the four-dimensional epilepsy classification system. Epileptic Disord. 2019;21(1):1–29. doi: 10.1684/epd.2019.1033. [DOI] [PubMed] [Google Scholar]
- 8.Schrijver T.V., Brand P.L., Bekhof J. Seasonal variation of diseases in children: a 6-year prospective cohort study in a general hospital. Eur J Pediatr. 2016;175(4):457–464. doi: 10.1007/s00431-015-2653-y. [DOI] [PubMed] [Google Scholar]
- 9.Mikkonen K., Uhari M., Pokka T., Rantala H. Diurnal and seasonal occurrence of febrile seizures. Pediatr Neurol. 2015;52(4):424–427. doi: 10.1016/j.pediatrneurol.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Manfredini R., Vergine G., Boari B., Faggioli R., Borgna-Pignatti C. Circadian and seasonal variation of first febrile seizures. J Pediatr. 2004;145:838–839. doi: 10.1016/j.jpeds.2004.06.079. [DOI] [PubMed] [Google Scholar]
- 11.Yang C., Hao Z., Yu D., Xu Q., Zhang L. The prevalence rates of medication adherence and factors influencing adherence to antiepileptic drugs in children with epilepsy: a systematic review and meta analysis. Epilepsy Res. 2018;142:88–99. doi: 10.1016/j.eplepsyres.2018.03.018. [DOI] [PubMed] [Google Scholar]