Abstract
Context:
Conventional medical curricula have created an impenetrable wall between the preclinical and clinical years of training, thus submerging relevance of basic sciences in clinical setup. Recently, the Medical Council of India has introduced a number of changes and updates in the medical education, including “early clinical exposure” (ECE) in newly proposed competency-based medical education. ECE does not replace the basic and clinical sciences but enriches and contextualizes that learning, therefore motivating the students to develop a better insight into medical profession.
Aims:
(1) To develop a protocol for the introduction of ECE in undergraduate medical training, (2) to validate and to deliver it to the 1st year MBBS students and assess their perceptions.
Settings and Design:
It was a prospective, nonrandomized, interventional study.
Subjects and Methods:
After taking permission from the institutional research committee and institutional ethical committee, a protocol for the introduction of ECE in Biochemistry was developed. The feedback questionnaire for the students and the faculty and retro-preself-efficacy questionnaire for the students were designed and validated. The ECE protocol was delivered to 143 1st-year MBBS students, and perceptions of concerned were collected and analyzed.
Statistical Analysis Used:
Collected data were analyzed in terms of percentages, medians, and satisfaction index and were represented in graphs.
Results:
Students reported that the ECE session was an enjoyable, satisfactory, and effective learning tool, with the improvement in knowledge, retention, attention, and motivation. Students also reported that this method of teaching–learning should be implemented in other topics as well as in other subjects of the first professional course.
Conclusions:
ECE protocol was perceived as very satisfactory by the students, and it helped in improvement of knowledge and to understand the relevance of preclinical subject in clinical setup.
Keywords: Biochemistry, early clinical exposure, MBBS first professional, perceptions
Introduction
Biochemistry is considered a dry, complex, but ever-evolving subject, where students are made to understand various biochemical reactions, enzymes, pathways, and regulations, without elucidating any correlation with its clinical context. This combined with “container–dispenser” type of teacher-centered didactic lectures makes it very difficult for students to retain what is necessary and how to apply these concepts effectively in practice. Hence, most of the students become less attentive in classrooms, cannot understand the relevance of biochemistry in clinical practice, and cannot perform to the best of their abilities. Due to lack of adequate exposure, intense competition, and the traditional curriculum, where the students are engaged in long hours of classroom and laboratory teaching with no exposure to the clinical setup,[1] there has been an urgent call for curricular reforms, with emphasis toward vertical and horizontal integration and competency-based training.[2]
Recently, the Medical Council of India (MCI) has developed the competency-based curriculum with the aim to produce medical graduates of global standards through curricular reforms. Proposed curricular changes begin early in the form of a foundation course; early clinical exposure (ECE); and properly designed integrated teaching and programs to develop the correct attitude and communication skills.[3]
ECE focuses on the introduction of clinically relevant material in the class or observation of patient handing and doctor– patient communication in actual outpatient department setting at the very 1st year. It helps to improve learning in all the three domains – cognitive, psychomotor, and affective of a medical student, which are needed to transform our undergraduates to physicians of first contact of community. Several studies have been undertaken to explore the impact of ECE among the medical students, which indicate it an effective technique to supplement the traditional theoretical teaching. ECE improves the performance of fresh medical entrants in basic science,[4] helps to relieve stress pertaining to patient handling, develops clinical reasoning, and produces good learning outcomes.[5,6,7] Although some authors have reported constraint of being more time- and effort-consuming,[4] the inclusion of this teaching–learning (T-L) method for few clinical conditions to supplement the effect of conventional teaching will largely improve the outcome, with benefit to students, economy, and society.
Subjects and Methods
It was a prospective, nonrandomized, interventional study carried out in Adesh Institute of Medical Sciences and Research, Bathinda, after taking the institutional research committee and institutional ethics committee permissions. A protocol on ECE for diabetes was prepared through departmental discussion and under the guidance of faculty, CMC, Ludhiana. The prepared protocol was peer-expert validated after providing them with validation criteria. Faculty of department of biochemistry was sensitized about the ECE. Feedback questionnaire for student participants and faculty facilitators and retro-preself-efficacy questionnaire for students were designed and validated by peer and experts.
First professional MBBS students were informed and sensitized about ECE, and those consenting were enrolled for the study. A total of 143 students participated in the study. ECE session targeting diabetes through laboratory reports, video clips, pictures, and case scenarios was delivered to the first professional MBBS students in batches of 70–75. The perceptions of the first professional MBBS student participants' about ECE on diabetes were taken through feedback questionnaire. The perceptions of involved faculty were also taken through feedback questionnaire. Retro-preself-efficacy questionnaire from students was collected, and data were analyzed using medians, percentages, and satisfaction index (SI). A flowchart of Methodology is detailed in Figure 1.
Figure 1.
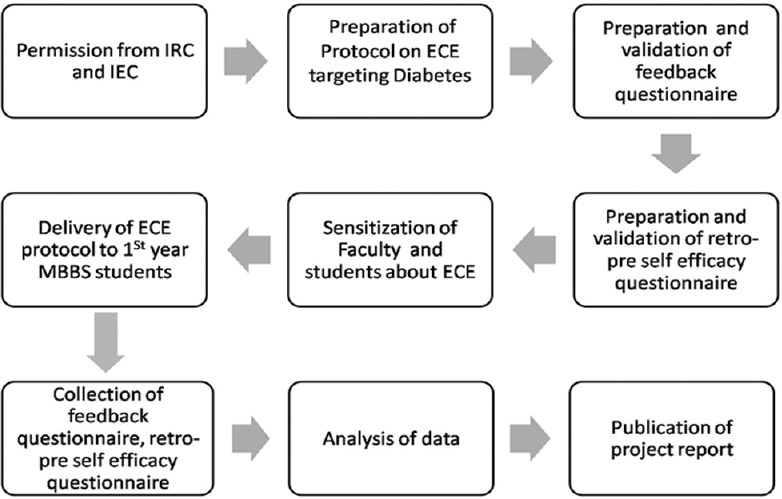
Flowchart of methodology
First-year student's feedback
The questionnaire for taking perceptions of students had three types of questions: (A) questions with five-point Likert scale to assess the perception of students about the session of ECE; (B) open-ended questions to assess two good things about the ECE session in totality; (C) open-ended question to suggest any change to improve ECE session.
To assess the perceived self-efficacy, the retro-preself-efficacy questionnaire had questions with seven-point Likert scale to check their efficacy about diabetes before and after the session of ECE. The questionnaire comprised of questions that were meant to assess the fortitude of students in diabetes before and after the session. For comparison purpose, median values were used.
Faculty feedback
Informal feedback from the faculty was collected at the end of each day session and was mainly for logistics and administrative purpose. The formal feedback was taken from the faculty in the form of a questionnaire with three type of questions: (A) questions with five-point Likert scale to assess the perception about the session of ECE; (B) open-ended questions to assess two good things about the ECE session in totality; (C) open-ended question to suggest any change to improve ECE session.
Results
A total of 143 students of MBBS first professional of batch 2017–2018, five faculty members from department of biochemistry, and three core committee members participated in the program. The protocol included brief introduction of diabetes, its types and differentiating features, biochemical and clinical features, diagnostic tests performed, management, and its correlated complications. The students were also exposed to various case scenarios of diabetes and actual blood reports of diabetic patients and were asked to deduce the provisional diagnosis. In the end, the students' and the faculties' perceptions of the effectiveness of the program were sought by a validated questionnaire. Similarly, gained efficacy of the students about diabetes before and after the ECE session was evaluated by retro-preself-efficacy questionnaire.
In the students' feedback questionnaire, 72% of the students strongly agreed that ECE is an enjoyable method of learning compared to conventional lecture (SI = 94.40), while 59% of the students strongly agreed that ECE is a satisfactory method of learning (SI = 79.92). 60%–65% of the students strongly agreed that ECE has made the topic of diabetes more interesting (SI = 91.32) and helped in improving the knowledge of diabetes (SI = 92.72). 50%–55% of the students strongly agreed that ECE has helped to increase attention in the class (SI = 88.95), better retention of the subject (SI = 89.37), motivated to learn the applied aspects of biochemistry (SI = 89.65), helped in correlating applied aspects of biochemistry in first professional (SI = 91.04) and therefore helped to understand the importance of biochemistry in clinical setup (SI = 89.51). Students also strongly agreed that ECE should be used as a method of T-L along with regular lectures in biochemistry in MBBS curriculum (SI = 94.26) as well as in other basic subjects in MBBS curriculum (SI = 93.56) [Figures 2 and 3].
Figure 2.
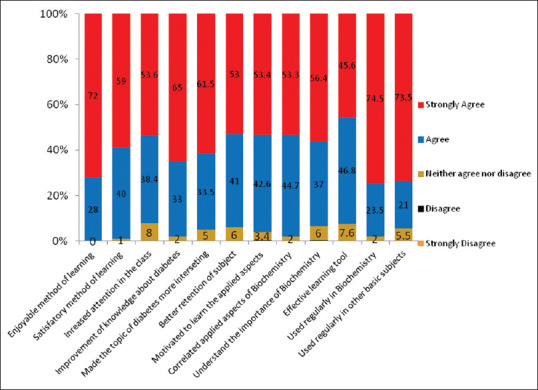
Perceptions of students about early clinical exposure session on five-point Likert scale
Figure 3.
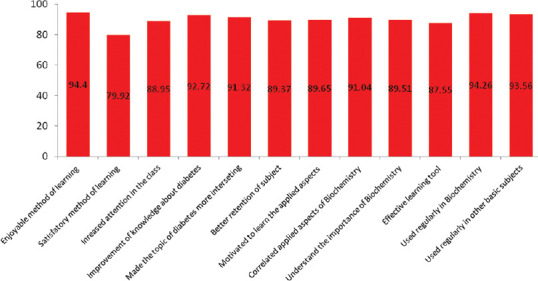
Satisfaction index of students on the early clinical exposure session on seven-point Likert scale
The main themes identified to open ended question “Enlist any two good things about feedback session” in the student feedback questionnaire were “improvement in knowledge,” “application of knowledge in clinical setup,” “student centric,” “effective learning tool,” “enhanced motivation,” and “enjoyable learning” [Figure 4].
Figure 4.
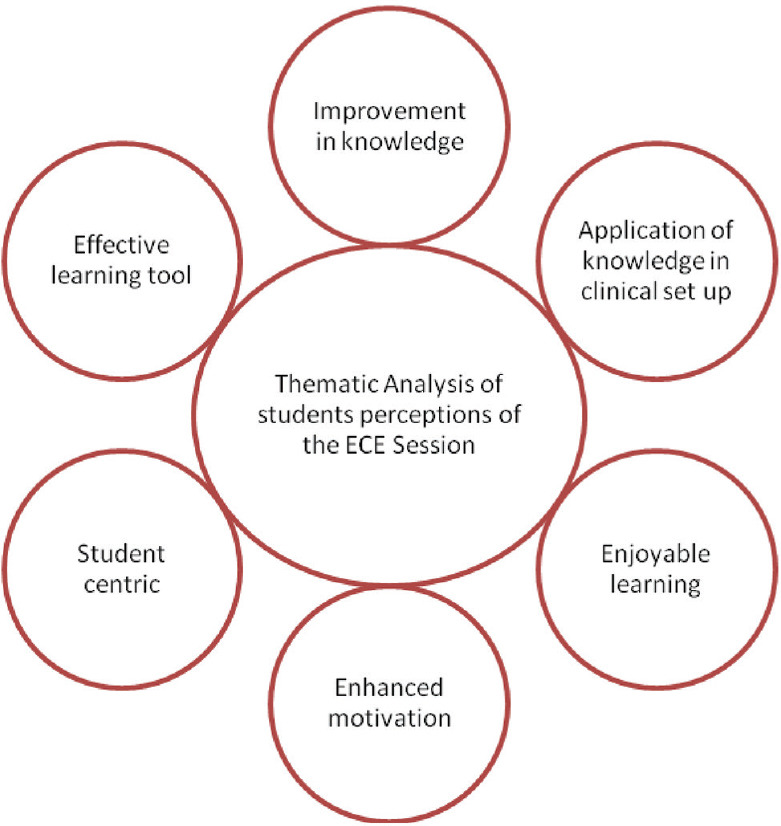
Thematic analysis of students' perceptions about early clinical exposure session
In the faculty's feedback questionnaire, 100% of the faculties strongly agreed that learning objectives were well explained and clear (SI = 100). 77.8% of the faculty strongly agreed that academic content for ECE session on diabetes was stimulating for the students (SI = 95.5), and therefore helped in better understanding of the topic diabetes (SI = 97.77). Faculty also opined that ECE has led to increase in attention of students compared to conventional lecture (SI = 86.66), response of the students was enthusiastic (SI = 93.33), and hence, they will be motivated to study biochemistry (SI = 88.88). The faculties disagreed that the session of ECE was time-consuming (SI = 48.88) or it adds on extra burden in routine schedule (SI = 35.55) with median value of 2, while they agreed that ECE should be included and implemented in routine curriculum in the future (SI = 93.33) [Figure 5].
Figure 5.
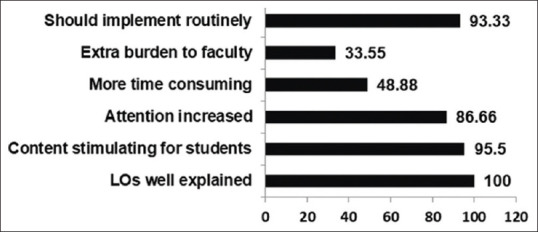
Satisfaction index of faculty about the early clinical exposure session
In student's retrospective pre–postself-efficacy questionnaire, students perceived an increase in median self-efficacy about basic understanding of diabetes, retention of topic taught, motivation to read, and confidence to attempt diabetes from 3 to 6. The median for self-efficacy for interpreting laboratory reports and skills in establishing correlation of biochemistry in various clinical case scenarios was also increased from 2 to 6 [Figure 6].
Figure 6.
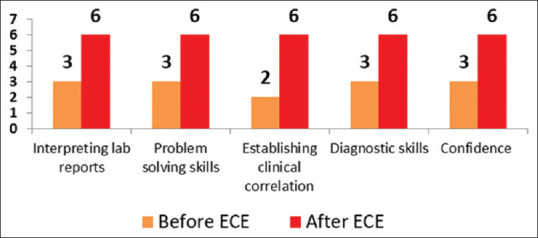
Improvement in median value of perceived efficacy on seven-point retro-preself-efficacy questionnaire for students after early clinical exposure
Discussion
Didactic lecture is teacher-centered, unidirectional, less interactive, and sometimes boring. By this mode of teaching, students get large amount of information only through passive transmission of knowledge and are not engaged in learning process. Moreover, the students are unable to understand the relevance of basic subjects in clinical settings, thus finding preclinical years tough, dreary, and ineffectual. This conventional mode of T-L creates a wide gap between the preclinical and clinical years. Therefore, in a need-based approach, the MCI, the regulatory body of medical education in India, has implemented competency-based medical education curriculum, which necessitates the need for clinical teaching from very 1st year onward. It has said that the clinical teaching should start with a foundation course focusing on communication, basic clinical skills, and professionalism, and ECE is one of the reforms to improve quality of medical education.
ECE calls for a shift in philosophy from “pedagogy” to “andragogy.” It is a teaching and learning methodology which fosters exposure of medical students to patients, clinics, or patient's relevant materials as early as the 1st year of medical college, in a social or clinical context that enhances learning of health, illness, or disease.[8] ECE allows higher order of thinking, covering higher levels of cognitive domain – application, analysis, synthesis, and evaluation.[9] This kind of learning may enable student to interpret clinical findings on the basis of basic concept of first professional subjects such as clinical or applied biochemistry. Hence, students can correlate the previous knowledge with the patient's history and laboratory reports, can learn actively about the disease, and can understand the importance of basic sciences in clinical setup. Students' confidence gets boosted, and so, they are motivated for self-directed learning, resulting in enhanced ability of problem-solving.
With this approach in mind, we carried the session of ECE-targeting diabetes with the help of video clips, laboratory reports, and case scenarios. Majority of students and the faculty found ECE a useful, enjoyable, satisfactory, and effective method of learning compared to conventional lectures. Students stated increased attention in the class, improvement in knowledge about the topic, motivation to read, and better retention, and these findings are in accordance with the study of Rawekar et al.,[10] which reported students giving a good feedback about ECE. In the present study, students also reported that ECE has helped them in correlating the applied aspects of biochemistry in clinical setup and it should be used as a method of T-L along with regular lectures in biochemistry as well as other basic subjects in first professional MBBS curriculum, a finding consistent with a study done by Kumar et al.[11] The perceptions about the understanding and retention of topic, motivation to read biochemistry, correlating it with clinical setup, diagnostic problem-solving skills, and confidence were improved from below average and average to very good. Correlating applied biochemistry by ECE will enable students to understand the relevance of underlying scientific knowledge and principles of clinical medicine. Self-directed learning and understanding by this method will help them to recall the knowledge and practical application of information and lead to the formation of a better clinician, thus benefiting the self, people, and society.
Conclusions
Students must be made aware of the clinical and diagnostic relevance of biochemistry. In this study, a validated protocol on ECE-targeting diabetes was delivered first time in our institution. Curriculum innovation in the form of ECE was perceived as a good intervention, efforts in designing and implementing such session were applauded, and relevance of biochemistry in clinical setup was well perceived by the students.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The present study was conducted under curriculum innovation education project for Advance Course in Medical Education under the flagship of CMC, MCI Nodal Centre, Ludhiana. I acknowledge the guidance and help provided by Dr. Dinesh Badyal, Convener, MCI Nodal Centre, and other faculty members of CMC, Ludhiana, for conceptualizing this study and subsequent motivation. I express a deep sense of gratitude to my batchmates of ACME 2018A for their continuous support and encouragement. I express my heartfelt thanks to faculty members of biochemistry department in delivering the module. I also thank my first professional students for their participation in the study.
References
- 1.Govindarajanan S, Vasanthb G, Kumarc PA, Priyadarshinib C, Radhakrishnand SS, Kanagaraje V, et al. Impact of a comprehensive early clinical exposure program for preclinical year medical students. Health Prof Edu. 2018;4:133–8. [doi.org/10.1016/j.hpe. 2017.06.002] [Google Scholar]
- 2.Irby DM, Cooke M, O'Brien BC. Calls for reform of medical education by the Carnegie foundation for the advancement of teaching: 1910 and 2010. Acad Med. 2010;85:220–7. doi: 10.1097/ACM.0b013e3181c88449. [DOI] [PubMed] [Google Scholar]
- 3.Mandal A, Ghosh A, Sengupta G, Bera T, Das N, Mukherjee S. Factors affecting the performance of undergraduate medical students: A perspective. Indian J Community Med. 2012;37:126–9. doi: 10.4103/0970-0218.96104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Das P, Biswas S, Singh R, Mukherjee S, Ghoshal S, Pramanik D. Effectiveness of early clinical exposure in learning respiratory physiology among the newly entrant MBBS students. J Adv Med Educ Prof. 2017;5:6–10. [PMC free article] [PubMed] [Google Scholar]
- 5.Sathishkumar S, Thomas N, Tharion E, Neelakantan N, Vyas R. Attitude of medical students towards early clinical exposure in learning endocrine physiology. BMC Med Educ. 2007;7:30. doi: 10.1186/1472-6920-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spencer J, Blackmore D, Heard S, McCrorie P, McHaffie D, Scherpbier A, et al. Patient-oriented learning: A review of the role of the patient in the education of medical students. Med Educ. 2000;34:851–7. doi: 10.1046/j.1365-2923.2000.00779.x. [DOI] [PubMed] [Google Scholar]
- 7.Dhonde S, Jagtap P, Belwalkar G, Nagane N, Bhandare V. Early clinical exposure: A tool to learn biochemistry: A small group study. Natl J Integr Res Med. 2015;6:76–80. [Google Scholar]
- 8.Verma M. Early clinical exposure: New paradigm in medical and dental education. Contemp Clin Dent. 2016;7:287–8. doi: 10.4103/0976-237X.188536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chari S, Gupta M, Gade S. The Early Clinical Exposure Experience Motivates First Year MBBS Students: A Study. Int J Edu Sci. 2015;8:403–5. [Google Scholar]
- 10.Rawekar A, Jagzape A, Srivastava T, Gotarkar S. Skill learning through early clinical exposure: An experience of Indian Medical School. J Clin Diagn Res JCDR. 2016;10:JC01–4. doi: 10.7860/JCDR/2016/17101.7022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar SS, Thomas N, Tharion E, Neelakantan N, Vyas R. Attitude of medical students towards early clinical exposure in learning endocrine physiology. BMC Med Edu. 2007;7:30. doi: 10.1186/1472-6920-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]


