Abstract
Aim
The COVID-19 pandemic may influence the willingness of bystanders to engage in resuscitation for out-of-hospital cardiac arrest. We sought to determine if and how the pandemic has changed willingness to intervene, and the impact of personal protective equipment (PPE).
Methods
We distributed a 12-item survey to the general public through social media channels from June 4 to 23, 2020. We used 100-point scales to inquire about participants’ willingness to perform interventions on “strangers or unfamiliar persons” and “family members or familiar persons”, and compared mean willingness during time periods prior to and during the COVID-19 pandemic using paired t-tests.
Results
Survey participants (n = 1360) were from 26 countries; the median age was 38 years (IQR 24–50) and 45% were female. Compared to prior to the pandemic, there were significant decreases in willingness to check for breathing or a pulse (mean difference −10.7% [95%CI −11.8, −9.6] for stranger/unfamiliar persons, −1.2% [95%CI −1.6, −0.8] for family/familiar persons), perform chest compressions (−14.3% [95%CI −15.6, −13.0], −1.6% [95%CI −2.1, −1.1]), provide rescue breaths (−19.5% [95%CI −20.9, −18.1], −5.5% [95%CI −6.4, −4.6]), and apply an automated external defibrillator (−4.8% [95%CI −5.7, −4.0], −0.9% [95%CI −1.3, −0.5]) during the COVID-19 pandemic. Willingness to intervene increased significantly if PPE was available (+8.3% [95%CI 7.2, 9.5] for stranger/unfamiliar, and +1.4% [95%CI 0.8, 1.9] for family/familiar persons).
Conclusion
Willingness to perform bystander resuscitation during the pandemic decreased, however this was ameliorated if simple PPE were available.
Keywords: Cardio pulmonary resuscitation, Bystander CPR, Personal protective equipment
Introduction
Out-of-hospital cardiac arrest (OHCA) outcomes are dependent on rapid interventions, with bystander cardiopulmonary resuscitation (CPR) significantly improving survival and long-term functional status.1 During the COVID-19 pandemic data from Paris demonstrated decreased bystander CPR rates and lower overall survival,2 yet investigators in Seattle and New York noted unchanged rates of bystander CPR.3, 4 We sought to survey the public to determine if and how COVID-19 has changed willingness to perform bystander CPR. Further, we investigated the impact of personal protective equipment (PPE) on willingness to intervene.
Methods
Survey tool development and administration
The University of British Columbia ethics board approved this study. Using standard survey development practises,5, 6 we created a survey using Qualtrics (Qualtrics 2019, Provo, Utah). We piloted the survey with 20 non-medically trained individuals and two community resuscitation organizations to assess for clarity and face and content validity. We used pilot results and iterative discussions among the investigator group to finalize the 12-question survey (Appendix A).
We distributed the survey to the general public via Twitter, Facebook, and Instagram from June 4 to 23, 2020 from the accounts of Providence Health Care Research Institute, the Hearts of BC Foundation, and our personal accounts. Participants had to be >18 years of age and understand English to be eligible. We did not provide incentives. Prior to participating in the survey, respondents read a 1-page description of the study, risks and benefits of participating, estimated duration, contact information, voluntary nature of participation, and consent process. Participants were asked if they consented to participation prior to being given access to the survey. We used reCAPTCHA (Google Inc., Mountainview, California) to identify respondents unlikely to be human (score of >0.5).7, 8 Based on a two-sided paired sample t-test, the study would require at least 200 participants to achieve a power of 80% and a level of significance of 5%, for detecting a mean change in willingness of 5, assuming the standard deviation of the changes to be 25. We planned to continue the survey for approximately three weeks, however would continue longer if we did not achieve 200 participants.
Statistical analysis and definitions
We used multiple-choice questions and 100-point scales to investigate participants’ willingness to perform resuscitative interventions on “strangers or unfamiliar persons” (hereinafter “stranger”) and “family members or familiar persons” (hereinafter “family”) prior to and during the COVID-19 pandemic. Although most previous surveys of bystander willingness to perform CPR have asked binary questions of “are you willing to intervene” we asked respondents to grade their willingness on a scale, a technique that has been previously described and validated.9 We believe that many factors (related to the bystander and the emergency situation) contribute to a bystander's decision to intervene in an emergency, many of which are unknown until a person is in the situation. Thus, we believed that asking respondents how likely they believed they would be to intervene would provide more granular data than asking a binary question. We calculated proportions using the number of respondents with non-missing data. We compared respondent willingness prior to and during the COVID-19 pandemic using paired t-tests and calculated mean differences with 95% confidence intervals. Since the pandemic reached different communities at different times, we did not indicate a specific start date for the pandemic period. We examined subgroups of: (1) healthcare worker (HCW); (2) female vs. male; (3) per capita COVID-19 incidence in the participant's country or state/province (if in North America), grouped as 0–50, 50–200, or >200 cases per 100,000 people (as of June 23).10, 11, 12, 13 We compared the mean difference between subgroups using two-sample t-tests for unadjusted analysis and analysis of covariance (ANCOVA) which adjusted for baseline willingness.
We studied the effect of victim age on changes in willingness to intervene by inquiring if respondents were less, the same, or more likely to intervene for a either a child or elderly victim (reference was adult) both prior to and during the COVID-19 pandemic (significance tested with Bowker's test). We did not specify age cut-offs, as we believed that the respondents’ impressions superseded a specific value. We classified changes in age-based willingness as: increased, decreased, or remaining the same.
Results
Respondent characteristics
Of 1501 respondents who initiated the survey, we excluded 141 (115 provided no answers, 3 ≤18 years old, and 23 likely non-human) leaving 1360 study participants from 26 countries (Table 1). Median age was 38 years (IQR 24–50), 686 (55.1%) identified as female, and 600 (47%) as HCWs. The majority believed handwashing (99.0%), social distancing (97.3%), and mask-wearing (89.6%) decreases COVID-19 spread; 34.5%, 95.6%, and 87.4% believed COVID-19 spreads from victim-to-rescuer via skin contact, mouth contact, or airborne, respectively (Suppl. Table 1).
Table 1.
Respondent characteristics.
| Den. | n (%) or median (IQR) | |
|---|---|---|
| Age (median, IQR) | 1263 | 38 (24 – 50) |
| Female sex, n (%) | 1245 | 686 (55.1) |
| Location of residence, n (%) | 1253 | |
| Africa | 5 (0.4) | |
| Asia | 60 (4.8) | |
| Australia or New Zealand | 8 (0.6) | |
| Canadaa | 925 (73.8) | |
| Central or South America | 3 (0.2) | |
| Europe | 87 (6.9) | |
| United Statesb | 165 (13.2) | |
| Location of residence, cases per 100,000 | 1253 | |
| 0–50, n (%) | 90 (7.2) | |
| 50–200, n (%) | 841 (67.1) | |
| >200, n (%) | 322 (25.7) | |
| Highest level of education, n (%) | 1264 | |
| High school diploma | 266 (21.0) | |
| Bachelor's degree | 314 (24.8) | |
| Master's degree, professional degree, or higher | 586 (46.4) | |
| None of the above | 98 (7.8) | |
| CPR training, n (%) | 1264 | |
| None | 221 (17.5) | |
| CPR course | 359 (28.4) | |
| Healthcare worker | 600 (47.5) | |
| Healthcare worker in training | 84 (6.6) |
Den., denominator (number of responses with non-missing data); HCW, healthcare worker; N, number.
Representing 9 provinces and 1 territory.
Representing 32 states.
Main results
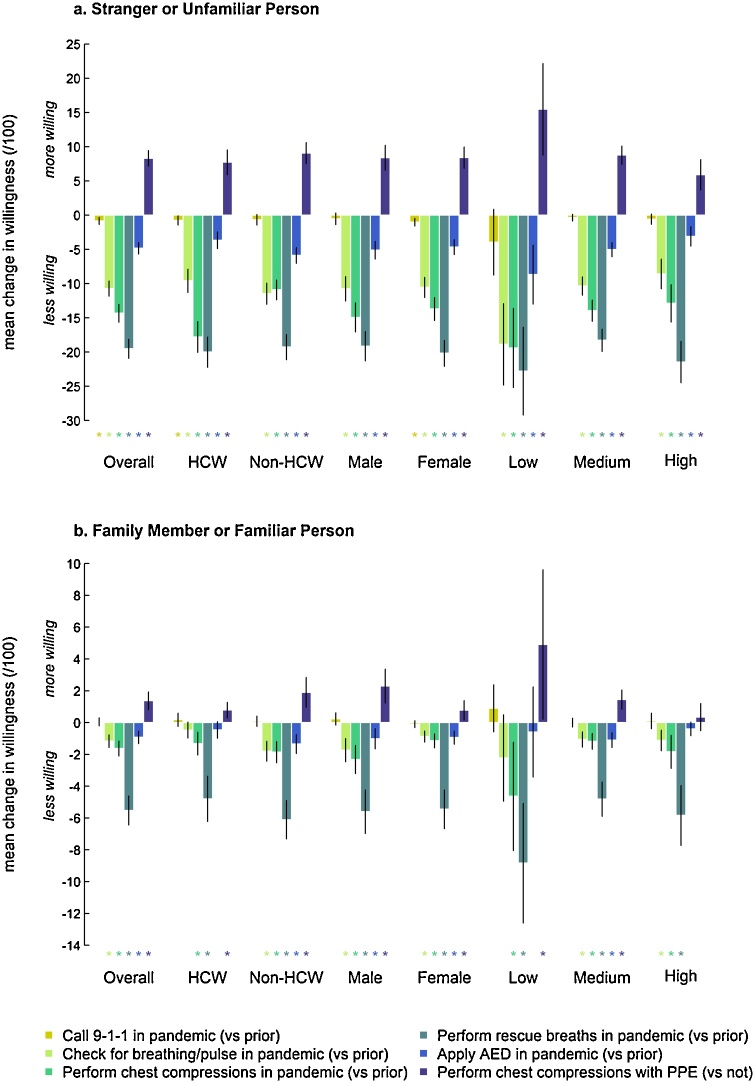
During the pandemic, respondents were less willing to check for breathing or a pulse (mean change −10.7% [95%CI −11.8, −9.6%] for stranger, −1.2% [95%CI −1.6, −0.8%] for family); perform chest compressions (stranger −14.3% [95%CI −15.6, −13.0%], family −1.6% [95%CI −2.1, −1.1%]); provide rescue breaths (stranger −19.5% [95%CI −20.9, −18.1%], family −5.5% [95%CI −6.4, −4.6%]); and apply an automated external defibrillator (stranger −4.8% [95%CI −5.7, −4.0%], family −0.9% [95%CI −1.3, −0.5%] There was a decrease in willingness to call 9-1-1 for a stranger (−0.8% [95%CI −1.4, −0.3%]) (Fig. 1 and Suppl. Table 2).
Fig. 1.
Change in bystander willingness to intervene in out-of-hospital cardiac arrests during the COVID-19 pandemic, for (1a) strangers or unfamiliar persons and (1b) family or familiar persons, overall and among subgroups. Subgroups include: (1) healthcare and non-healthcare workers; (2) female and male; (3) per capita COVID-19 incidence in the country or province/state (if in North America) of the participant (grouped as “Low” [0–50], “Medium” (50–200], or “High” [>200 cases per 100,000 people10]; the right endpoints are included in the group). Each bar represents the mean change in willingness (with 95% confidence intervals), calculated with paired t-tests, to perform the specified intervention. * Denotes a p value <0.05. HCW, healthcare worker; PPE, personal protective equipment (including a face-mask for the rescuer and the victim, and gloves for the rescuer); AED, automated external defibrillator.
These results were consistent across subgroups, with the following exceptions: (i) HCWs had no change in willingness to check for breathing or pulse for family, or to apply an AED for family; (ii) non-HCWs had no change in willingness to call 9-1-1 for a stranger; (iii) men had no willingness change to call 9-1-1 for strangers; (iv) none of the COVID-19 incidence subgroups demonstrated changes in willingness to call 9-1-1 for a stranger; the <50 cases per 100,000 subgroup had no change in willingness to check for breathing or a pulse for family, or apply an AED for family; and the >200 cases per 100,000 subgroup had no changes in willingness to apply an AED for family.
When comparing changes in willingness between subgroups, non-HCWs had a larger decrease in willingness to check for breathing or a pulse and apply an AED for family members, and HCWs had a larger decrease in willingness to perform chest compressions for strangers (Suppl. Table 3). Male (vs. female) respondents demonstrated a larger decrease in willingness to check for breathing or a pulse, and perform chest compressions for family members (Suppl. Table 3). Higher COVID-19 regional incidence did not appear correlated with greater decreases in willingness to perform chest compressions (Fig. 1).
The availability of PPE significantly increased willingness to perform chest compressions during the pandemic (stranger +8.3% [95%CI 7.2, 9.5%]; family +1.4% [95%CI 0.8, 1.9%]) (Suppl. Table 2). This was consistent across subgroups. If the OHCA occurred in a stranger, 39%, 56%, and 57% of respondents were more willing to perform chest compressions if they had gloves, a facemask, or a victim mouth-covering, respectively; 64% were more willing to provide rescue breaths if a plastic face barrier was available.
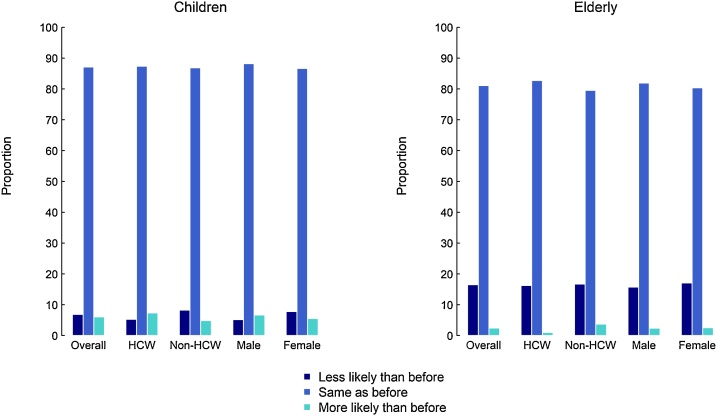
Overall and within all subgroups, victim age had a significant impact on change in willingness to perform CPR (Fig. 2 and Suppl. Table 4). Overall, 5.8% of respondents had increased, and 7.0% decreased willingness, to assist pediatric victims during the pandemic, in comparison to prior to the pandemic; for elderly victims, 2.5% were more willing to assist and 16.7% less.
Fig. 2.
Changes in bystander willingness to intervene for children or elderly victims of OHCA during the COVID-19 Pandemic (reference for both adult victims) HCW, health care worker.
Discussion
We surveyed 1360 international participants regarding willingness to perform bystander interventions during and prior to the COVID-19 pandemic. Overall, respondents were less willing to intervene in OHCA during the COVID-19 pandemic, especially for unfamiliar persons. However, willingness significantly increased with the availability of simple PPE, which may inform public health efforts.
We examined subgroups classified by HCW status, gender, and location of residence. When comparing HCWs and non-HCWs most results were similar, demonstrating decreased willingness to perform chest compressions and rescue breaths on familiar and unfamiliar cardiac arrest victims alike. In fact, the decrease in willingness of HCWs to perform chest compressions for strangers was significantly greater than for non-HCWs. Whereas non-HCWs showed less willingness during the pandemic to check for breathing or apply an AED in all individuals, for HCWs this decrease in willingness was only for strangers. Taken together, HCWs appeared to have greater decreases in enthusiasm to attempt resuscitation for unfamiliar victims. Many HCWs have undergone training in new COVID-related protocols, with standard best practises altered,14 often to prioritize occupational safety.15, 16, 17 This may have translated into a hesitancy to administer bystander resuscitation for unfamiliar patients. These results, primarily from North America, are inconsistent with survey results from Russia, in which respondents of a lay CPR training program appeared to have unchanged or increased willingness to intervene during the COVID pandemic.18
Decreases in willingness to provide bystander care did not appear correlated with higher regional COVID-19 incidence; in fact, regions with the lowest COVID-19 incidence tended to have the largest decreases in willingness. However, low-incidence regions also had the lowest pre-pandemic willingness to perform chest compressions on strangers, suggesting systematic regional differences in bystander CPR enthusiasm. It is unclear why male respondents demonstrated larger decreases in willingness to intervene for family members or familiar persons however may reflect differences in relationships and risk tolerance with next of kin. One study examining bystander willingness to perform CPR prior to the COVID-19 pandemic demonstrated that men were more likely to intervene,9 however another study detected no differences between sexes.19
Victim age had a significant impact on changes in willingness to intervene. Changes occurred in both directions, especially for pediatric cases, perhaps due to variable respondent impressions of potential victim COVID-19 infection. In contrast, our data indicate a net decreased willingness of individuals to respond in geriatric OHCA. While uncertain, this may be due to a balance between potential benefit to the victim (i.e. the elderly may have poor OHCA outcomes) and risk to the rescuer
Respondents demonstrated larger decreases in willingness to perform rescue breaths and chest compressions and a smaller decrease in willingness to call 9-1-1 or apply an AED, likely related to perceived risks of disease transmission. Importantly, PPE availability mitigated decreases: the mean 14% decrease in performing chest compressions was attenuated by 8% if PPE was available. These data may assist public health efforts to increase PPE availability both public and private settings.
A cohort of 537 OHCA in King County, WA, diagnosed COVID-19 in 3.7% patients declared dead at EMS arrival and 6.5% of EMS-treated OHCA from February 26 to April 5.3 The authors postulated that since COVID-19 was diagnosed in <10% OHCA, even a potential 10% risk of transmission to bystanders doing hands-only CPR without PPE would lead to a 1% chance of bystander infection; however, bystander CPR saves more than 300 additional lives for every 10,000 OHCA patients.20
Previous studies have examined the willingness of individuals to perform bystander CPR prior the COVID-19 pandemic. Cartledge and colleagues examined data from a national cross-sectional survey in Australia (n = 1076), and reported that only 49% of respondents would perform CPR on a stranger.21 Top identified barriers to willingness included: not being trained in CPR, not feeling confident, and fear. Urban et al. surveyed adult patients and visitors from a suburban ED in New York and reported that 78% were willing to perform hands-only CPR on strangers.19 Barbic et al. reported that 62% of individuals were willing to perform chest compressions, which increased to 77% if 9-1-1 dispatch was instructing the bystander.22 Another Canadian survey found that a greater proportion of respondents were willing to provide chest compression-only CPR, compared to traditional CPR, for all victims (61.5% v. 39.7%), when the victim was a stranger (55.1% v. 38.8%), or when the victim was an “unkempt” individual (47.9% v. 28.5%).23
Most previous studies have asked the question of whether bystanders are willing or not willing to perform interventions. However, as a bystander may be unsure if she or he would actually intervene we choose instead to but ask participants of how likely they would be willing to intervene. Chew and colleagues used this same approach, asking participants how willing they would be to intervene in a cardiac arrest, using a 10-point scale. They reported a median willingness of 7 (IQR 5–9) to perform chest compression-only CPR, compared to 5 (IQR 5–8) for chest compression-plus-ventilation CPR.9
Limitations
This survey was undertaken early in the pandemic and re-surveying could lead to different results. Recall bias is a limitation; specifically, fears of participants to COVID-19 that were present while completing the survey may have influenced their perceptions of their willingness to perform CPR prior to the COVID-19 pandemic. The survey was English only; we did not measure attitudes of non-English speakers. We recruited participants via social media and this almost certainly over-represented certain groups, particularly younger, HCW-employed, and post-secondary educated individuals. We cannot comment on the attitudes of non-responders. Although respondents represented six continents, the majority were from Canada. Social desirability biases may have impacted answers.
Conclusions
We found a significant decrease in willingness to perform bystander CPR during the COVID-19 pandemic. Importantly, respondents reported a substantial increase in willingness to intervene if simple PPE are available.
Authors’ contribution
SC and JB conceived the study idea. BG applied for ethics. SC, BG, and JB designed the protocol with input from all authors. All authors contributed to the survey tool development, and SS, AC, NB, NS, and JB played the lead role in distributing the survey. DG performed the statistical analyses. BG drafted the manuscript. All authors contributed to interpretation of data, manuscript revision and final approval.
Conflict of interest
BG has received speaking honoria from Stryker Corp.
Footnotes
Supplementary material related to this article can be found, in the online version, at http://dx.doi.org/10.1016/j.resplu.2020.100034.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Hasselqvist-Ax I., Riva G., Herlitz J. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 2.Marijon E., Karam N., Jost D. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sayre M.R., Barnard L.M., Counts C.R. Prevalence of COVID-19 in out-of-hospital cardiac arrest: implications for bystander CPR. Circulation. 2020:1–7. doi: 10.1161/CIRCULATIONAHA.120.048951. [DOI] [PubMed] [Google Scholar]
- 4.Lai P.H., Lancet E.A., Weiden M.D. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York city. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burns K.E.A., Kho M.E. How to assess a survey report: a guide for readers and peer reviewers. CMAJ. 2015;187:E198–E205. doi: 10.1503/cmaj.1405.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burns K.E.A., Bscpharm M.D., Pt M.E.K., Meade M.O., Mdcm N.K.J.A., Sinuff T. Review: a guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179:245–252. doi: 10.1503/cmaj.080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Google . 2020. reCAPTCHA v3. (Accessed 9 August 2020, at https://developers.google.com/recaptcha/docs/v3) [Google Scholar]
- 8.von Ahn L., Maurer B., McMillen C., Abraham D., Blum M. reCAPTCHA: human-based character recognition via Web security measures. Science. 2008;321:1465–1468. doi: 10.1126/science.1160.379. [DOI] [PubMed] [Google Scholar]
- 9.Chew K.S., Ahmad Razali S., Wong S.S.L. The influence of past experiences on future willingness to perform bystander cardiopulmonary resuscitation. Int J Emerg Med. 2019;12:40. doi: 10.1186/s12245-019-0256-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Our World in Data . 2020. Total confirmed COVID-19 cases per million people, June 23, 2020. (Accessed 23 June 2020, at https://ourworldindata.org/grapher/new-covid-cases-per-million) [Google Scholar]
- 11.Johns Hopkins University. COVID-19 data repository by the center for systems science and engineering. (Accessed 20 June 2020, at https://github.com/CSSEGISandData/COVID-19).
- 12.Statistics Canada . 2020. Statistics Canada. Table 17-10-0009-01 population estimates, quarterly. (Accessed 20 June 2020) [DOI] [Google Scholar]
- 13.United States Census Bureau . 2019. National population totals and components of change. (Accessed 20 June 2020, at https://www.census.gov/data) [Google Scholar]
- 14.Nolan J.P., Monsieurs K.G., Bossaert L. European Resuscitation Council COVID-19 guidelines executive summary. Resuscitation. 2020;153:45–55. doi: 10.1016/j.resuscitation.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cook T.M., El-Boghdadly K., McGuire B., McNarry A.F., Patel A., Higgs A. Consensus guidelines for managing the airway in patients with COVID-19: guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetist. Anaesthesia. 2020;75:785–799. doi: 10.1111/anae.1505.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Savary D., Morin F., Fadel M., Metton P., Richard J.C., Descatha A. Considering the challenge of the Covid-19 pandemic, is there a need to adapt the guidelines for basic life support resuscitation? Resuscitation. 2020;152:50–51. doi: 10.1016/j.resuscitation.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kandori K., Narumiya H., Iizuka R. Extracorporeal cardiopulmonary resuscitation should not be performed on confirmed or suspected COVID-19 patients. Resuscitation. 2020;153:6–7. doi: 10.1016/j.resuscitation.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Birkun A. Distant learning of BLS amid the COVID-19 pandemic: influence of the outbreak on lay trainees’ willingness to attempt CPR, and the motivating effect of the training. Resuscitation. 2020;152:105–106. doi: 10.1016/j.resuscitation.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Urban J., Thode H., Stapleton E., Singer A.J. Current knowledge of and willingness to perform Hands-Only™ CPR in laypersons. Resuscitation. 2013;84:1574–1578. doi: 10.1016/j.resuscitation.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 20.Sasson C., Rogers M.A.M., Dahl J., Kellermann A.L. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.8895.76. [DOI] [PubMed] [Google Scholar]
- 21.Cartledge S., Saxton D., Finn J., Bray J.E. Australia's awareness of cardiac arrest and rates of CPR training: results from the Heart Foundation's HeartWatch survey. BMJ Open. 2020;10:e033722. doi: 10.1136/bmjopen-2019-0337.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barbic D., Duncan K., Trainor R. A survey of the public's ability to recognize and willingness to intervene in out-of-hospital cardiac arrest and opioid overdose. Acad Emerg Med. 2020 doi: 10.1111/acem.1391.6. [DOI] [PubMed] [Google Scholar]
- 23.Cheskes L., Morrison L.J., Beaton D., Parsons J., Dainty K.N. Are Canadians more willing to provide chest-compression-only cardiopulmonary resuscitation (CPR)? A nation-wide public survey. CJEM. 2016;18:253–263. doi: 10.1017/cem.2015.113. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.