Abstract
Background
Superior labrum anterior to posterior (SLAP) tears are a very common shoulder injury. The success rate of SLAP repair, particularly in the throwing athlete, has been variable in the literature.
Questions/Purposes
The purpose of this systematic review was to evaluate the reported post-operative outcomes of management techniques for failed SLAP repair.
Methods
The electronic databases MEDLINE, Embase, and PubMed were searched for relevant studies, and pertinent data was abstracted. Only studies reporting outcomes of management techniques for failed SLAP repairs were included.
Results
A total of 10 studies (levels III to IV) evaluating 176 patients were included in this systematic review. Most subjects were male (86.6%), with a mean age at surgery of 36.3 years (range, 17 to 67 years). The most commonly reported reason for failed SLAP repair was persistent post-operative mechanical symptoms after index SLAP repair. Common techniques used in the management of failed SLAP repair include biceps tenodesis and revision SLAP repair. Return to activity was significantly higher after biceps tenodesis than after arthroscopic revision SLAP repair. However, compared to primary SLAP repair, biceps tenodesis demonstrated no statistically significant differences in return to work rates. Complications reported in one case were resolved post-operatively, and there was no reported revision failure or reoperation after revision surgery.
Conclusion
The most common reason for failed SLAP repair is persistent post-operative mechanical symptoms. Revision surgery for failed SLAP repair has a high success rate. The rate of return to activity after biceps tenodesis was significantly higher than the rate after revision SLAP repair. Large high-quality randomized trials are required to provide definitive evidence to support the optimal treatment for failed SLAP repair.
Electronic supplementary material
The online version of this article (10.1007/s11420-019-09700-3) contains supplementary material, which is available to authorized users.
Keywords: shoulder, superior labrum anterior to posterior tears, SLAP, labrum, glenoid, athletes
Introduction
Superior labrum anterior to posterior (SLAP) tears are increasingly diagnosed, particularly in the throwing athlete [2]. “SLAP” tears were first described by Andrews et al. in 1985, but the term was later coined by Snyder et al. in 1990. “SLAP tear” describes the pathology of the superior labrum and the origin of the biceps tendon [1, 21]. SLAP tears are present in up to 26% of shoulder arthroscopy procedures, and arthroscopic SLAP repair has been a commonly performed treatment [8]. A recent statewide study in New York found a 464% increase in the number of SLAP repairs performed from 2002 to 2010—an increase approximately threefold greater than all other ambulatory shoulder procedures evaluated over the same period [13]. Additionally, there has been a significant increase in the age of patients being treated with arthroscopic SLAP repairs, despite evidence suggesting that SLAP repairs in patients over the age of 36 years is associated with higher rates of failure [13, 17].
A failed SLAP repair is defined as post-operative pain, stiffness, and/or consistent pre-operative symptoms (not associated with concomitant pathology) that do not resolve post-operatively or resolves post-operatively and returns at a later date [17, 25]. In general, mechanisms of failure for SLAP repair are categorized as failure to treat concomitant pathology, development of new pathology, technique-related failure, development of post-operative stiffness, or implant-related failure [23, 25]. Revision management techniques employed are dependent on the mechanism of failure of the SLAP repair. After a failed SLAP repair is established, and nonsurgical management techniques have been exhausted, surgical options include labral debridement, revision SLAP repair, biceps tenotomy, and/or biceps tenodesis [25].
It has been noted that outcomes after revision SLAP repair may be inferior to those of the primary operation. Park et al. in a retrospective study identified patients who had undergone revision arthroscopic type II SLAP repairs and found that revision surgery yielded worse results than index procedures, especially in overhead athletes [16]. De Giorgi et al. also conducted a retrospective study evaluating the outcomes of revision arthroscopic surgery for shoulder instability and identified a high overall failure rate after revision surgery [4].
The purpose of this systematic review was to evaluate and report causes of failed SLAP repairs, management strategies in revision cases, rates of revision failure, and post-operative outcomes of revision surgery for failed SLAP repair.
Methods
A systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [11]. A literature search was conducted using three electronic medical databases—PubMed, Embase, and MEDLINE—from their inception to the first week of September 2018, to identify all relevant studies related to the management of failed SLAP repairs. MeSH and Emtree terms were used in various combinations to increase search sensitivity. References of included studies were reviewed for additional relevant references that met the inclusion criteria (Appendix Table 3).
Table 3.
Search strategy
| MEDLINE: 665 | EMBASE: 861 | PUBMED: 9 |
|---|---|---|
| Search strategy: | Search strategy: | Search strategy: |
| 1. SLAP*.mp. | 1. SLAP*.mp. | (SLAP* OR superior labrum OR labrum OR superior labrum anterior to posterior) AND (manag* OR revis* OR Reoperation OR fail* OR Treatment Failure) AND pubstatusaheadofprint |
| 2. superior labrum.mp. | 2. superior labrum.mp. | |
| 3. labrum.mp. | 3. labrum.mp. | |
| 4. Superior labrum anterior to posterior.mp. | 4. Superior labrum anterior to posterior.mp. | |
| 5. manag*.mp. | 5. manag*.mp. | |
| 6. revis*.mp. | 6. revis*.mp. | |
| 7. Reoperation/ | 7. Reoperation/ | |
| 8. fail*.mp. | 8. fail*.mp. | |
| 9. TREATMENT FAILURE/ | 9. TREATMENT FAILURE/ | |
| 10. 1 or 2 or 3 or 4 | 10. 1 or 2 or 3 or 4 | |
| 11. 5 or 6 or 7 or 8 or 9 | 11. 5 or 6 or 7 or 8 or 9 | |
| 12. 10 and 11 | 12. 10 and 11 |
Studies were included if they (1) were level I to IV evidence published in English, (2) included patients of any age with a failed SLAP repair, (3) involved a surgical intervention for failed SLAP repair, and (4) reported post-intervention shoulder functional outcomes. Exclusion criteria included literature reviews, conference proceedings, expert opinions, case reports, technique guides, nonhuman studies, cadaver or biomechanical studies, clinical studies that did not include patients with failed SLAP repair, and studies where post-intervention shoulder functional outcomes were not reported.
A list of citations was compiled from the literature search and duplicates were removed. Systematic screening was performed in duplicate by two independent reviewers (I.M.N. and S.V.) from title to full-text screening stages. Discrepancies were resolved by consensus between the two reviewers. If they could not reach consensus, the input of a third, senior reviewer (N.H.) was sought to determine the study’s eligibility. Interrater agreement was calculated using Cohen’s kappa coefficient (κ) [10].
Data were extracted in duplicate by two independent reviewers (I.M.N. and S.V.) and recorded in a Microsoft Excel spreadsheet (version 2016; Microsoft, Redmond, WA, USA). Data on authors, year of publication, study design, level of evidence, sample size and characteristics, intervention for failed SLAP repair, time from index surgery to intervention, follow-up period, post-intervention complications, pre- and post-intervention shoulder functional outcomes, and rate of revision failure were extracted. The primary outcome was post-intervention shoulder functional outcome scores for the management technique of failed SLAP repair.
Study quality was appraised, using the Methodological Index for Non-randomized Studies (MINORS) tool [20], in duplicate by two independent reviewers, and discrepancies were resolved by consensus between the two reviewers.
A κ statistic was used to evaluate inter-reviewer agreement at all screening stages. Additionally, the intraclass correlation coefficient (ICC) was calculated to evaluate inter-reviewer agreement for the quality assessment using the MINORS criteria. Agreement was categorized a priori. Substantial agreement corresponded to a κ/ICC value of 0.61 or greater; moderate agreement to a value between 0.21 and 0.60; and slight agreement to a value of 0.20 or less [9]. Statistical Package for the Social Sciences (SPSS, version 23.0; IBM Corp., Armonk, NY, USA) was used to perform all statistical analyses.
Results
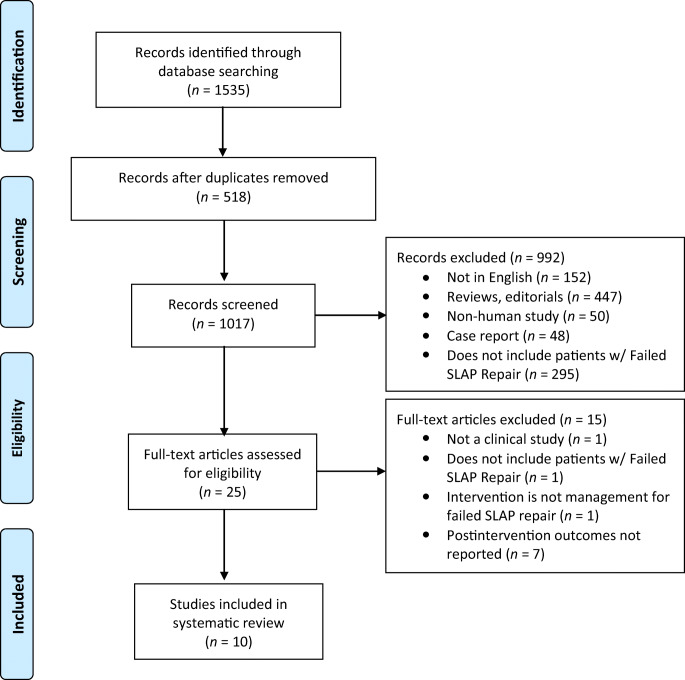
The search strategy initially identified 1535 titles for screening. After elimination of duplicates, 1017 titles and abstracts were screened. Following full-text review of 25 studies, ten met our inclusion criteria. There was moderate agreement between reviewers at the title- and abstract-screening stage (κ = 0.803; 95% CI, 0.683 to 0.922) and the full-text screening stage (κ = 0.746; 95% CI, 0.477 to 1.000) (Fig. 1).
Fig. 1.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) scheme of retrieved literature.
All ten included studies were published between 2006 and 2017, five (50%) in the past 5 years (2014 to 2018). Nine studies provided level-IV evidence, and one was a level-III study. A total of 176 patients with failed SLAP repair were included in the final analysis, with a mean age of 36.3 years (range, 17 to 67) [14, 16]. Of the nine studies reporting gender, 86.6% (305/352) were male.
Surgical management of the failed SLAP lesion included open biceps tenodesis (n = 60), arthroscopic biceps tenodesis (n = 52), arthroscopic revision SLAP repair (n = 28), labral debridement (n = 20), extensive glenohumeral joint debridement (n = 16), and arthroscopic knot removal (n = 11). The mean interval between index and revision surgeries was 13.1 months (range, 2 to 56 months) [9, 14], and average length of follow-up after revision was 36.3 months (range, 5 to 156 months) [6, 14].
The mean MINORS score for non-comparative studies was 10.2 ± 2.20 out of 16, and the MINORS score for the comparative study was 20 out of 24, indicating a fair quality of evidence (ICC = 0.889; 95% CI, 0.553 to 0.972) (Table 1).
Table 1.
Study characteristics of included studies, in order of publication date
| Study | Study design (level of evidence) | Number of patients with failed SLAP repair | Mean age of sample ± SD (range) (years) | Proportion of males (%) | Intervention procedure(s) reported | Time from index surgery and revision ± SD (months) | Length of follow-up (months) | MINORS scorea |
|---|---|---|---|---|---|---|---|---|
| Park et al. [14] (2017) | Case series (IV) | 11 | 24.6 ± 8.6 (17–43) | 10/11 (90.9%) | Arthroscopic knot removal (n = 11) | 21.2 ± 14.7 (8–56) | 48.0 ± 37.4 (24–156) | 12/16 |
| Sastre et al. [19] (2015) | Longitudinal & retrospective (IV) | 8 | 35.9b (19–55) | 18/22 (81.8%) b | Arthroscopic subpectoral biceps tenodesis (n = 8) | 21.6 (13–29) | – | 8/16 |
| Waterman et al. [24] (2015) | Cohort study (III) | 31 | 35.0 c ± 8.2 (20–56) | 184/192 (95.8%) c |
Arthroscopic SLAP repair (n = 6) Arthroscopic subpectoral biceps tenodesis (n = 25) |
– | – | 20/24 |
| Werner et al. [26] (2014) | Case series (IV) | 24, 17 included in final analysis | 39.2 ± 8.9 years | 14/24 (58.3%) |
Open subpectoral biceps tenodesis (n = 9) Arthroscopic suprapectoral biceps tenodesis (n = 15) Subacromial decompression (n = 7) Distal clavicle excision (n = 3) |
13.6 (5.7–26.0) | 24.2 | 10/16 |
| McCormick et al. [9] (2014) | Case series (IV) | 42 | 39.2 ± 6.1 | 35/42 (83.3%) |
Open subpectoral biceps tenodesis (n = 42) Subacromial debridement (n = 6) |
12.8 (9.0–22.0) | 42 (24–72) | 15/16 |
| Gupta et al. [6] (2013) | Case series (IV) | 9 | 40 (22–55) | 6/9 (66.7%) |
Open subpectoral biceps tenodesis (n = 9) Labral debridement (n = 9) Concomitant Acromioplasty (n = 2) Subacromial bursectomy (n = 1) |
– | 26 (5–49) | 11/16 |
| Stephenson et al. [22] (2012) | Case series (IV) | 6 | 34.3 (17–44) | 5/6 (83.3%) |
Arthroscopic rotator cuff repair (n = 6) Arthroscopic SLAP repair (n = 3) |
15.0 (10–22) | 58.3 (25–75) | 8/16 |
| Park et al. [16] (2011) | Case series (IV) | 12 | 32.6 (19–67) | 10/12 (83.3%) |
Arthroscopic SLAP repair (n = 12) Partial-thickness rotator cuff tear debridement (n = 7) Subacromial bursectomy (n = 2) Removal of prominent suture anchors (n = 1) Subacromial decompression (n = 4) Humeral head chondroplasty (n = 1) Distal clavicle excision (n = 1) |
13.0 ± 6.7 | 50.5 (8–81) | 11/16 |
| Katz et al. [7] (2009) | Case series (IV) | 34 | 42.7 (16–58) | 23/34 (67.6%) |
Conservative treatment (n = 34) Revision surgery - 21/34 Total shoulder arthroplasty (n = 1) SLAP repair (n = 1) Rotator cuff repair (n = 3) Biceps tenodesis (n = 4) Removal of loose or prominent hardware/suture (n = 8) Labral debridement (n = 11) Subacromial Depression (n = 15) Extensive glenohumeral joint debridement (n = 16) Manipulation (n = 1) Capsular release (n = 4) |
9 (2–24) | – | 8/16 |
| Sassmannshausen et al. [18] (2006) | Case series (IV) | 6 | 38 (28–50) | – | Arthroscopic SLAP repair with bioabsorbable suture anchor (n = 6) | 9.5 (8–12) | 14 (8–17) | 9/16 |
MINORS methodological index for non-randomized studies, SD standard deviation, SLAP superior labrum anterior to posterior
aThe global ideal MINORS score is 16 for non-comparative studies and 24 for comparative studies
bCharacteristic of entire 22 sample size, not just the 8 patients with failed SLAP repair
cCharacteristic of entire 192 sample size, not just the 31 patients with failed SLAP repair
The most common reason for SLAP failure was persistent post-operative mechanical symptoms after index SLAP repair that were not resolved after conservative treatment, reported in seven (70%) of the studies [6, 7, 9, 16, 19, 24, 26]. Another reason for SLAP failure was persistent post-operative pain due to hardware failure of index surgery: post-operative knot-induced pain reported in one (10%) of the studies [14] and broken/dislodged tacks reported in one (10%) study [18]. One study (10%) attributed failed SLAP repair to rotator cuff tear caused by portal placement during index surgery [22].
The revision management technique employed was determined by the reason for failed SLAP repair. For persistent post-operative mechanical symptoms after index surgery, revision techniques included open biceps tenodesis (n = 60), arthroscopic biceps tenodesis (n = 52), labral debridement (n = 20), and arthroscopic revision SLAP repair (n = 19). For the reason of post-operative pain due to hardware failure, revision techniques included arthroscopic knot removal (n = 11) and arthroscopic SLAP repair with bioabsorbable suture anchor (n = 6). Stephenson et al. determined rotator cuff tear in six patients to be caused by portal placement during index surgery and performed arthroscopic rotator cuff repair and arthroscopic SLAP repair in three patients, and arthroscopic rotator cuff repair only in the other three patients [22] (Table 2).
Table 2.
Reason for failed SLAP repair, reported symptoms, and revision intervention procedures of included studies, in order of publication date
| Study | Number of patients with failed SLAP repair | Reason for failed SLAP repair | Reported symptoms | Revision intervention procedure(s) |
|---|---|---|---|---|
| Park et al. [14] (2017) | 11 | Persistent post-operative knot-induced pain: 5 patients—misplaced knot on the articular side that caused glenoid erosion. 6 patients—knots were away from the glenoid but were causing knot irritation. |
Sharp pain (11/11–100%) Clicking (7/11–63.6%) Shoulder instability (1/11–9.1%) Tenderness on bicipital grove (4/11–36.4%) Positive Neer’s impingement sign (4/11–36.4%) Positive Hawkins’ impingement sign (2/11–18.2%) Positive speed’s test (6/11–54.5%) Positive O’Brien active compression test (5/11–45.5%) |
Arthroscopic knot removal (n = 11) |
| Sastre et al. [19] (2015) | 8 | Poor results with persistent pain over 1 year after the primary surgery with no response to specific rehabilitation treatment (Constant Scale score < 50 points) | – | Arthroscopic subpectoral biceps Tenodesis (n = 8) |
| Waterman et al. [24] (2015)a | 31 | Persistent post-operative pain related to primary repair of a type II SLAP lesion | – |
Arthroscopic SLAP repair (n = 6) Arthroscopic subpectoral biceps tenodesis (n = 25) |
| Werner et al. [26] (2014) | 24, 17 included in final analysis | When persistent post-operative symptoms were determined to be a result of a failed SLAP repair and conservative measures were exhausted, patients were offered surgical intervention | All patients reported pain as an initial symptom of failed SLAP repair. A traumatic aetiology of initial symptoms was reported in 15/24–62.5% of the cohort. |
Open subpectoral biceps tenodesis (n = 9) Arthroscopic suprapectoral biceps tenodesis (n = 15) Subacromial decompression (n = 7) Distal clavicle excision (n = 3) |
| McCormick et al. [9] (2014) | 42 | Failures of primary SLAP repair defined: inability to return to active duty within a minimum of 6 months from surgery, ASES score of less than 75 at 1-year follow-up from the primary procedure, or patient electing to undergo revision surgery because of dissatisfaction with the primary results |
Characteristics Pain (37/42–88.1%) Stiffness/loss of motion (40/42–95.2%) Surgical findings Loose repair sutures (40/42–95.2%) Synovitis of rotator interval (40/42–95.2%) Adhesions between biceps tendon and rotator cuff (33/42–78.6%) Extensive involvement of biceps tendon proper (SLAP type III or IV) (18/42–42.9%) Chondromalacia of humeral head (34/42–81.0%) Chondromalacia of superior glenoid (17/42–40.5%) |
Open subpectoral biceps tenodesis (n = 42) Subacromial debridement (n = 6) |
| Gupta et al. [6] (2013) | 9 | Persistent pain following arthroscopic type II SLAP repair and failed conservative treatment | – |
Open subpectoral biceps tenodesis (n = 9) Labral debridement (n = 9) Concomitant acromioplasty (n = 2) Subacromial bursectomy (n = 1) |
| Stephenson et al. [22] (2012) | 6 | Persistent symptoms and rotator cuff tear, which was judged to be caused as a complication of portal placement from index SLAP repair. |
Shoulder pain (6/6–100%) Mild scapular dyskinesia (5/6–83.3%) Pain with supraspinatus testing (6/6–100%) Pain with external rotation testing (4/6–66.7%) Positive Hawkins impingement sign (6/6–100%) Positive active compression test (4/6–66.7%) Positive Speed test (3/6–50%) Full-thickness rotator cuff tears (6/6–100%) |
Arthroscopic rotator cuff repair (n = 6) Arthroscopic SLAP repair (n = 3) |
| Park et al. [16] (2011) | 12 | The prior SLAP repair site was visualized and probed to assess for stability of the repair. Upon finding a type II SLAP lesion, the decision to perform revision SLAP repair was made. |
Persistent pain (8/12–66.7%) No patient reported instability |
Arthroscopic SLAP repair (n = 12) Partial-thickness rotator cuff tear debridement (n = 7) Subacromial bursectomy (n = 2) Removal of prominent suture anchors (n = 1) Subacromial decompression (n = 4) Humeral head chondroplasty (n = 1) Distal clavicle excision (n = 1) |
| Katz et al. [7] (2009) | 34 | Post-operative pain, stiffness, and/or mechanical symptoms developed after repair of a superior labral tear despite following a standard post-operative rehabilitation protocol. |
Pain (34/34–100%) Decreased range of motion (28/34–82.4%) |
Conservative treatment (n = 34) Revision surgery - 21/34 Total shoulder arthroplasty (n = 1) SLAP repair (n = 1) Rotator cuff repair (n = 3) Biceps tenodesis (n = 4) Removal of loose or prominent hardware/suture (n = 8) Labral debridement (n = 11) Subacromial depression (n = 15) Extensive glenohumeral joint debridement (n = 16) Manipulation (n = 1) Capsular release (n = 4) |
| Sassmannshausen et al. [18] (2006) | 6 | Persistent symptoms and MRI findings of broken/dislodged tacks: 4 patients—a single broken bioabsorbable PLLA tack was found. 2 patients—two PLLA tacks were found—one broken and one dislodged |
Persistent deep shoulder pain (6/6–100%) Mechanical symptoms (5/6–83.3%) Positive O’Brien’s test (6/6–100%) |
Arthroscopic SLAP repair with bioabsorbable suture anchor (n = 6) |
ASES American Shoulder and Elbow Surgeons, MRI magnetic resonance imaging, PLLA poly-L-lactic acid, SLAP superior labrum anterior to posterior
aStudy compared return to duty between post-arthroscopic SLAP repair and arthroscopic subpectoral biceps tenodesis
All studies reported improvements in functional outcomes after revision surgery for failed SLAP repair when comparing pre- and post-operative scores. Waterman et al. conducted the only comparative study, comparing arthroscopic SLAP repair (n = 6) and arthroscopic subpectoral biceps tenodesis (n = 25) for persistent post-operative pain related to index SLAP repair [24]. It was reported that the rate of return to military duty following biceps tenodesis (19/25, 76%) was significantly higher than after revision SLAP repair (1/6, 16.7%; p = 0.024) [24]. In addition, it was reported that compared to primary SLAP repair, revision of failed SLAP repair to a subpectoral biceps tenodesis demonstrated no statistically significant differences in rates of return to military duty (153/192, 79.7% vs. 19/25, 76%, respectively; p = 0.76) [24].
Park et al. performed arthroscopic knot removal for persistent post-operative knot-induced pain related to index SLAP repair and found the procedure to significantly improve range of motion of active forward flexion (155.5 ± 18.4 to 166.4 ± 7.4; p = 0.007) and internal rotation to the back (T11.8 ± 3.3 to T9.3 ± 2.0; p = 0.016) [14]. Arthroscopic knot removal also improved range of motion of external rotation at the side (54.5 ± 19.6 to 57.7 ± 17.5; p = 0.336) and abduction (123.6 ± 14.3 to 125.5 ± 16.9; p = 0.496), although the improvement was not statistically significant [14]. Furthermore, arthroscopic knot removal significantly improved visual analog scale (VAS) score for pain at rest (3.1 ± 1.6 to 0.6 ± 1.1; p = 0.011), VAS score at motion (5.6 ± 1.9 to 1.5 ± 1.8; p = 0.005), the Shoulder Rating Scale of the University of California at Los Angeles (UCLA) score (15.2 to 31.7; p = 0.003), and Constant scores (56.5 ± 10.2 to 89.8 ± 3.2; p = 0.003) [14].
McCormick et al. performed open subpectoral biceps tenodesis for patients who failed SLAP repair [9]. It was found that open subpectoral biceps tenodesis as a revision technique to failed index SLAP repair resulted in statistically significant improvements in range of motion of forward flexion (135° to 155°; p = 0.0001) and abduction (125° to 155°; p = 0.0001) [9]. Additionally, the revision procedure resulted in significantly higher post-operative shoulder functional scores, such as American Shoulder and Elbow Surgeons (ASES) (68 to 89; p = 0.0001), Single Assessment Numeric Evaluation (SANE) (64 to 84; p = 0.0001), and Western Ontario Shoulder Instability Index (WOSI) (65 to 81; p = 0.0001) scores. The rate of return to military duty and sports was 81% (34/42 patients) [9].
Gupta et al. performed open subpectoral biceps tenodesis and concomitant labral debridement on nine patients with persistent pain following arthroscopic type II index SLAP repair who failed conservative treatment [6]. It was found that the revision procedure resulted in significant improvements in VAS (4.11 ± 2.47 to 2.55 ± 2.60; p = 0.033), Simple Shoulder Test (SST) (5.40 ± 2.55 to 9.33 ± 2.87; p = 0.005), ASES (54.50 ± 19.48 to 77.96 ± 21.50; p = 0.002), SANE (42.50 ± 22.39 to 70.44 ± 27.65; p = 0.001), and Short Form 12-Questionnaire Health Survey (SF-12) Physical Composite Score (PCS) (35.47 ± 8.61 to 47.95 ± 7.66; p = 0.018) [6].
Katz et al. performed conservative treatment on 34 patients with persistent post-operative pain related to index SLAP repair, and various surgical interventions on 21 patients who failed conservative treatment [6]. It was found that the SST score significantly improved after either conservative or revision surgery (3.04 ± 2.18 to 8.73 ± 3.45; p < 0.0001), with 23 out of 34 patients (67.6%) being satisfied overall (10/34 satisfied after conservative treatment, 13/21 satisfied after revision surgery) [6] (Online Resource 1).
Five studies reported complications of revision surgery of failed SLAP repair [6, 9, 14, 16, 22]. Park et al., Gupta et al., Stephenson et al., and Park et al. reported no post-operative complications [6, 14, 16, 22]. McCormick et al. reported one case of transient musculocutaneous nerve neurapraxia, which resolved post-operatively and did not require further surgical intervention [9]. Overall complication rate was calculated to be 1.25% (1/80). There were no reported rates of revision failure or re-operations.
Discussion
A major finding of this systematic review was that all studies reported improved functional outcome scores following revision surgery for failed SLAP repair when comparing pre- and post-operative scores, with no reported revision failures. The most common reason for failure of SLAP repair was persistent post-operative mechanical symptoms that were not resolved after conservative treatment. Other commonly reported reasons for revision surgery after SLAP repair include technical errors in the index surgery and hardware failure.
Multiple reasons for SLAP failure have been identified in the literature. Post-operative pain and stiffness have been identified as the most common reason for revision of a SLAP repair; however, symptoms typically resolve with physical therapy and subacromial and/or glenohumeral injections. If there is suspicion of infection, diagnosis should be confirmed and treatment with antibiotics and possible revision surgery should be pursued. Other potential sources of pain include concomitant pathologies, such as biceps pathology, rotator cuff tear, acromioclavicular (AC) joint impingement, arthritis, instrumentation problems, and chondral injuries [25].
Other common causes for failed SLAP repair identified in the literature are misdiagnosis of SLAP lesion, inadequate healing, patient selection, poor surgical indications, or a subsequent injury caused by a straining activity (such as overhead throwing) [17, 25]. Technical factors, such as anchor placement, may contribute to SLAP failure to a lesser degree. Mechanisms for failed SLAP repair can be broadly categorized as (1) failure to treat concomitant pathology, (2) development of new pathology, (3) technique-related failure, (4) biologic failure, including failure to heal and development of post-operative stiffness, and (5) and implant-related failure. Our systematic review identified the causes for SLAP failure to be (1) persistent post-operative mechanical symptoms, (2) persistent post-operative hardware-induced symptoms from index surgery (knot-induced pain, broken/dislodged tacks), and (3) rotator cuff tear caused by incorrect portal placement during index surgery [25].
A number of papers in the literature evaluate risk factors for revision surgery after SLAP repair. Taylor et al. reviewed a large national database of 4751 patients who underwent SLAP repair and found 121 patients (2.55%) required revision surgery [23]. Risk factors for SLAP failure included age over 40 years, female sex, obesity, smoking, and diagnosis of biceps tendinitis or long head of the biceps tearing at or before the time of surgery [23]. Mollon et al. reported the incidence and risk factors for subsequent shoulder procedures after isolated SLAP repair [12]. In a larger database review of patients operated from 2003 to 2014, 2524 patients were identified. After 3 to 11 years of follow-up, 254 patients (10.1%) underwent repeat surgical intervention [12].
Park et al. investigated implant characteristics and risk for SLAP failure [15]. It was reported that subsequent surgery and failure after arthroscopic SLAP repair was significantly correlated with the use of absorbable poly-L/D-lactic acid (PLDLA) anchors, poly-96L/4D-lactic acid anchors (Mini-Revo; Linvatec, Largo, FL, USA), and poly-70L/30D-lactic acid anchors (Bio-Fastak and Bio-Suturetak; Arthrex, Naples, FL, USA). The rates of repeat surgery with PLDLA anchors from Linvatec and from Arthrex were 24% and 4%, respectively. After controlling for associated factors in a multivariate analysis, the use of absorbable anchors, in particular poly-96L/4D-lactic acid anchors, remained an independent factor associated with both repeat surgery and revision superior labrum repair [15].
Patient characteristics may also play a role in the failure of SLAP surgery. Cancienne et al. reported that the incidences of failed SLAP repair and post-operative infection were significantly higher in patients who used tobacco than in matched controls [3]. Additionally, Provencher et al. studied the factors associated with failure of primary SLAP repair and reported that patient age above 36 years was the only factor associated with a statistically significant increase in the incidence of failure [17].
Throwing athletes are also at increased risk of failure of SLAP repair. Fedoriw et al. examined return-to-play (RTP) and return-to-prior-performance (RPP) rates in professional baseball players after SLAP repair and found that the RTP rate for 27 pitchers who underwent surgical management was 48%, but RPP was 7% [5]. However, the RTP rate for 13 position players was 85%, and the RPP rate was 54%. The difference in rates between pitchers and position players can result from the extent of shoulder involvement required in their position.
It is important to evaluate the reason for SLAP repair when considering which surgical technique to use. No standard guidelines exist for management of failed SLAP repair; thus, the selection of a particular surgical technique is primarily based on the reason for SLAP failure, present pathologies, patient factors, and surgeon preference. A thorough workup for repair failure should be performed in patients before performing revision surgery. If a patient presents with post-operative symptoms following SLAP repair, a physical examination should be performed, and the physician should determine (1) the location, duration, and onset of pain, (2) whether symptoms are new or continued, (3) the presence of any new injuries, and (4) the range of motion in both shoulders. Post-operative stiffness is generally the most common cause of pain after SLAP repair and may resolve with non-surgical interventions. Physical therapy may be used for strengthening and increasing range of motion, and subacromial and/or glenohumeral injections can be used for diagnostic or therapeutic purposes. If there is suspicion of infection, appropriate laboratory tests should be obtained and treatment with antibiotics should be pursued. If non-surgical strategies fail, diagnostic imaging and diagnostic arthroscopy should be performed to identify the cause of pain and to determine which surgical procedure be performed, if it is required at all [17, 25].
This systematic review identified commonly used revision surgical techniques to include revision SLAP repair, biceps tenodesis, subacromial decompression, subacromial debridement, rotator cuff repair, and removal of loose or prominent hardware/sutures. According to Werner et al., biceps tenodesis is recommended as the surgical intervention in most patients with failed SLAP repair, particularly middle-aged patients and younger patients with pathology of the long head of the biceps tendon. Revision SLAP repair is recommended for younger patients (35 years or less) with no significant pathology of the long head of the biceps tendon, and biceps tenotomy is recommended for patients older than 65 years [25]. Patients should be counselled about the risks of cosmetic deformity, failure, and other complications associated with biceps tenotomy. However, the procedure for the management of a failed SLAP repair should always be tailored to the underlying reason for failure of the index procedure.
In this review, we found only one case of complication from among 80 patients (1/80, 1.25%), transient musculocutaneous nerve neurapraxia after open biceps tenodesis that resolved post-operatively and did not require further surgical intervention [9]. Additionally, no revision failures or re-operations were reported. This is a promising result; however, it is likely an underestimation due to selective reporting, limited follow-up time, and small sample size. Furthermore, there is a high level of heterogeneity across studies to draw certain conclusions.
The strengths of this systematic review include a comprehensive search strategy using multiple large medical databases, screening and data extraction conducted in duplicate with a high level of interrater agreement, and a mean MINORS score indicating fair quality of evidence of included studies. This systematic review is limited by the level of evidence of the included studies, as the studies were primarily case series. Additionally, most studies lacked a comparative group, precluding any formal meta-analysis. Furthermore, significant heterogeneity was present among included studies, particularly with respect to the reason for failed SLAP repair, the surgical revision intervention, and the measures utilized to report outcomes. Large high-quality randomized trials are required to definitively provide evidence to support the optimal treatment for failed SLAP repair.
In conclusion, the most common reason for failed SLAP repair was persistent post-operative mechanical symptoms after index procedure that were not resolved after conservative treatment. There are several interventions for failed SLAP repair that have demonstrated improved post-operative outcomes. Return to duty rates following revision to biceps tenodesis were significantly higher than those after revision SLAP repair; however, when compared to primary SLAP repair, biceps tenodesis demonstrated no statistically significant differences. According to our findings and those of other studies, biceps tenodesis is generally the recommended surgical technique for failed SLAP repair, especially in older patients and patients with a concomitant pathology of the long head of the biceps tendon. Younger patients may require revision SLAP repair. Due to significant heterogeneity and lack of comparative groups, further statistical analysis could not be conducted. Large high-quality randomized trials are required to provide definitive evidence to support the optimal treatment for failed SLAP repair.
Electronic supplementary material
(PDF 214 kb)
Appendix
Compliance with Ethical Standards
Conflict of Interest
Ibrahim M. Nadeem, BHSc Candidate, Seline Vancolen, BHSc Candidate, Nolan S. Horner, MD, Tim Leroux, MD, MSc, FRCSC, Bashar Alolabi, MD, MSc, FRCSC, and Moin Khan, MD, MSc, FRCSC, declare that they have no conflicts of interest.
Human/Animal Rights
N/A
Informed Consent
N/A
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
References
- 1.Andrews JR, Carson WG, Mcleod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13(5):337–341. doi: 10.1177/036354658501300508. [DOI] [PubMed] [Google Scholar]
- 2.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology, Part I: pathoanatomy and biomechanics. Arthrosc J Arthrosc Relat Surg. 2003;19(4):404–420. doi: 10.1053/JARS.2003.50128. [DOI] [PubMed] [Google Scholar]
- 3.Cancienne JM, Brockmeier SF, Werner BC. Tobacco use is associated with increased rates of infection and revision surgery after primary superior labrum anterior and posterior repair. J Shoulder Elb Surg. 2016;25(11):1764–1768. doi: 10.1016/j.jse.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 4.De Giorgi S, Garofalo R, Tafuri S, Cesari E, Delle Rose G, Castagna A. Can arthroscopic revision surgery for shoulder instability be a fair option? Muscles Ligaments Tendons J. 2014;4(2):226–231. doi: 10.11138/mltj/2014.4.2.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fedoriw WW, Ramkumar P, McCulloch PC, Lintner DM. Return to Play After Treatment of Superior Labral Tears in Professional Baseball Players. Am J Sports Med. 2014;42(5):1155–1160. doi: 10.1177/0363546514528096. [DOI] [PubMed] [Google Scholar]
- 6.Gupta AK, Bruce B, Klosterman E, McCormick F, Harris JD, Romeo AA. Subpectoral biceps tenodesis for failed type II SLAP repair. Orthop J Sport Med. 2013;1(4):e273–e728. doi: 10.1177/2325967113S00088. [DOI] [PubMed] [Google Scholar]
- 7.Katz LM, Hsu S, Miller SL, Richmond JC, Ketia E, Kohli N, et al. Poor outcomes after SLAP repair: descriptive analysis and prognosis. Arthroscopy. 2009;25(8):849–855. doi: 10.1016/j.arthro.2009.02.022. [DOI] [PubMed] [Google Scholar]
- 8.Kim TK, Queale WS, Cosgarea AJ, McFarland EG. Clinical features of the different types of SLAP lesions: an analysis of one hundred and thirty-nine cases. J Bone Jt Surg Am. 2003;85(1):66–71. doi: 10.2106/00004623-200301000-00011. [DOI] [PubMed] [Google Scholar]
- 9.McCormick F, Nwachukwu BU, Solomon D, et al. The efficacy of biceps tenodesis in the treatment of failed superior labral anterior posterior repairs. Am J Sports Med. 2014;42(4):820–825. doi: 10.1177/0363546513520122. [DOI] [PubMed] [Google Scholar]
- 10.McHugh ML. Interrater reliability: the kappa statistic. Biochem Medica. 2012;22(3):276–282. doi: 10.11613/BM.2012.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi:10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed]
- 12.Mollon B, Mahure SA, Ensor KL, Zuckerman JD, Kwon YW, Rokito AS. Subsequent shoulder surgery after isolated arthroscopic SLAP repair. Arthroscopy. 2016;32(10):1954–1962.e1. doi: 10.1016/j.arthro.2016.01.053. [DOI] [PubMed] [Google Scholar]
- 13.Onyekwelu I, Khatib O, Zuckerman JD, Rokito AS, Kwon YW. The rising incidence of arthroscopic superior labrum anterior and posterior (SLAP) repairs. J Shoulder Elb Surg. 2012;21(6):728–731. doi: 10.1016/j.jse.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Park JG, Cho NS, Kim JY, Song JH, Hong SJ, Rhee YG. Arthroscopic knot removal for failed superior labrum anterior-posterior repair secondary to knot-induced pain. Am J Sports Med. 2017;45(11):2563–2568. doi: 10.1177/0363546517713662. [DOI] [PubMed] [Google Scholar]
- 15.Park MJ, Hsu JE, Harper C, Sennett BJ, Huffman GR. Poly-L/D-lactic acid anchors are associated with reoperation and failure of SLAP repairs. Arthroscopy. 2011;27(10):1335–1340. doi: 10.1016/j.arthro.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 16.Park S, Glousman RE. Outcomes of revision arthroscopic type II superior labral anterior posterior repairs. Am J Sports Med. 2011;39(6):1290–1294. doi: 10.1177/0363546511398648. [DOI] [PubMed] [Google Scholar]
- 17.Provencher MT, McCormick F, Dewing C, McIntire S, Solomon D. A Prospective Analysis of 179 Type 2 Superior Labrum Anterior and Posterior Repairs. Am J Sports Med. 2013;41(4):880–886. doi: 10.1177/0363546513477363. [DOI] [PubMed] [Google Scholar]
- 18.Sassmannshausen G, Sukay M, Mair SD. Broken or dislodged poly-L-lactic acid bioabsorbable tacks in patients after SLAP lesion surgery. Arthroscopy. 2006;22(6):615–619. doi: 10.1016/j.arthro.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 19.Sastre S, Claret G, Peidro L, Lozano L, Caballero M. Slap lesions in middle-aged patients: biceps repair or tenodesis? What should we perform for long biceps tendon? J Orthop Trauma Rehabil. 2015;19(2):89–92. doi: 10.1016/j.jotr.2014.10.004. [DOI] [Google Scholar]
- 20.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 21.Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy. 1990;6(4):274–279. doi: 10.1016/0749-8063(90)90056-J. [DOI] [PubMed] [Google Scholar]
- 22.Stephenson DR, Hurt JH, Mair SD. Rotator cuff injury as a complication of portal placement for superior labrum anterior-posterior repair. J Shoulder Elb Surg. 2012;21(10):1316–1321. doi: 10.1016/j.jse.2011.08.054. [DOI] [PubMed] [Google Scholar]
- 23.Taylor SA, Degen RM, White AE, et al. Risk factors for revision surgery after superior labral anterior-posterior repair: a national perspective. Am J Sports Med. 2017;45(7):1640–1644. doi: 10.1177/0363546517691950. [DOI] [PubMed] [Google Scholar]
- 24.Waterman BR, Arroyo W, Heida K, Burks R, Pallis M. SLAP repairs with combined procedures have lower failure rate than isolated repairs in a military population. Orthop J Sport Med. 2015;3(8):232596711559915. doi: 10.1177/2325967115599154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Werner BC, Brockmeier SF, Miller MD. Etiology, diagnosis, and management of failed SLAP repair. J Am Acad Orthop Surg. 2014;22(9):554–565. doi: 10.5435/JAAOS-22-09-554. [DOI] [PubMed] [Google Scholar]
- 26.Werner BC, Pehlivan HC, Hart JM, Lyons ML, Gilmore CJ, Garrett CB, et al. Biceps tenodesis is a viable option for salvage of failed SLAP repair. J Shoulder Elb Surg. 2014;23(8):e179–e184. doi: 10.1016/j.jse.2013.11.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 214 kb)