Abstract
Background
Limited evidence informs whether pre-operative values of two-point discrimination (2PD) in patients with carpal tunnel syndrome predict response to surgery.
Questions/Purposes
The primary aim of this study was to determine the predictive value of pre-operative 2PD scores on outcomes following carpal tunnel release (CTR). In particular, we sought to evaluate whether a clinically relevant 2PD threshold exists that can predict symptomatic response after surgery.
Methods
Patients who underwent CTR between 2014 and 2018 were retrospectively reviewed. Static 2PD scores in each digit, as well as Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) and Levine-Katz scores, were collected from pre- and post-operative records. Pearson correlation coefficients assessed the relationship between pre-operative 2PD, early post-operative 2PD, and patient-reported outcome scores. Poor 2PD was defined as 2PD greater than 10 mm.
Results
Eighty-nine hands in 73 patients with a mean follow-up of 1.8 years were analyzed. Mean pre- and post-operative 2PD was 7.2 mm and 6.4 mm, respectively, in the most affected digit when measurable. Twenty patients had poor 2PD scores pre-operatively and 14 post-operatively. There was a positive correlation between pre- and early post-operative 2PD scores but no correlation between pre-operative 2PD score and final post-operative functional scores. Only 30% of patients with poor pre-operative 2PD scores demonstrated improvement, compared with 69% of patients with measurable 2PD.
Conclusion
We found that greater pre-operative 2PD scores predicted greater early post-operative 2PD scores but did not lead to worse functional outcome scores post-operatively. Patients with poor pre-operative 2PD scores were likely to demonstrate improvement in functional outcomes scores, while having less reliable improvement in 2PD after CTR. Patients with poor 2PD should be counseled that improvement of tactile perception is less predictable.
Electronic supplementary material
The online version of this article (10.1007/s11420-019-09694-y) contains supplementary material, which is available to authorized users.
Keywords: two-point discrimination, carpal tunnel syndrome, symptom severity, carpal tunnel release
Introduction
Carpal tunnel syndrome (CTS) is one of the most common diagnoses encountered by hand surgeons, with a prevalence of approximately 4% in the general population [4]. Several clinical tests are used to objectively measure nerve function in patients affected by CTS, including the static and moving two-point discrimination (2PD) tests and the Semmes-Weinstein monofilament test [11, 13]. Specifically, the Weber static 2PD test assesses sensation in the most distal aspect of the median nerve distribution to quantify the pathological loss of sensation caused by CTS [15]. Since 2PD testing correlates with digital innervation availability and capacity, some practitioners use this test as an objective measure of disease severity. The American Society for Surgery of the Hand (ASSH) divides 2PD values into the following categories: normal (less than 6 mm), fair (6 to 10 mm), and poor (11 to 15 mm), as well as protective, if only 1 point can be perceived beyond 15 mm, or anesthetic, if no point is perceived beyond 15 mm [1].
There are limitations of the 2PD test; it is time-consuming, requiring each digit to be tested, and it is not sensitive to sensory changes until conduction has ceased [11, 16]. Beyond the administration and interpretation of 2PD testing, the utility of 2PD scores in CTS has also been questioned. Multiple studies have reported that 2PD can be unaffected despite the presence of other clinical indicators in patients with CTS [3, 11, 12]. Phalen’s and Durkin’s tests are often cited as more diagnostically sensitive in patients with CTS, and it is known that 2PD scores correlate to age, though this might not be reflective of symptom severity [13]. For these reasons, many practitioners favor the use of these clinical examinations over objective tests that stratify disease severity, including 2PD and the Semmes-Weinstein monofilament test, particularly given that the strength of association between the static 2PD test and CTS symptom severity is unclear.
It remains unknown whether pre-operative 2PD scores predict CTS symptom severity and response to surgery. The primary aim of this study was to determine the predictive value of pre-operative 2PD scores on early post-operative symptom severity following carpal tunnel release (CTR). Secondary aims included correlation of pre-operative 2PD scores with post-operative recovery of 2PD. We hypothesized that a clinically relevant 2PD threshold exists that can predict symptomatic response after surgery.
Materials and Methods
All patients diagnosed with CTS based on CTS-6 score who underwent surgery by a single fellowship-trained surgeon between 2014 and 2018 were retrospectively reviewed. The CTS-6 score is a validated 6-item score that is highly responsive to changes in CTS symptoms [2]. Patients who failed conservative management using nighttime wrist immobilization were offered surgery based on patient preference and surgeon’s clinical indication. Pre- and post-operative Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) score (QDS), Levine-Katz symptom severity score (LKSSS) and Levine-Katz functional status score (LKFSS), and static 2PD values for the affected hand were recorded.
Patients were contacted by telephone at a minimum of 6 months after surgery to have the questionnaires repeated for final symptom severity follow-up. Patients were excluded from the study population if no pre- or post-operative 2PD scores were obtained. The primary outcome was post-operative improvement in the QDS. Secondary outcomes included improvement in the LKSSS, LKFSS, and post-operative 2PD scores of the most affected digit at final clinical follow-up.
Evaluation of static 2PD was performed in the affected hand using a caliper and was recorded as the smallest distance at which two points could be distinguished using standardized pressure sufficient to blanch skin. Starting at 5 mm, the calipers were placed over the volar aspect of the fingertip and progressively opened until the final threshold value was determined for all five fingers of the affected hand. Three or more correct responses at a given value were deemed a correct measurement of 2PD. All testing was performed by the surgeon (D.F.) or her physician assistant (E.H.). Values of greater than 10 mm were considered poor discrimination based on the ASSH criteria, and we did not distinguish between higher 2PD values beyond this point; those readings were classified as poor and excluded from means reported in the descriptive statistics. The most affected finger of the radial three digits was used to define pre-operative 2PD of the median nerve in the affected hand [9]. Improvement in post-operative 2PD score from baseline was defined as delta 2PD.
Surgical technique was consistent across all cases, through an open approach to the carpal tunnel through a 15-mm incision centered over the transverse carpal ligament (TCL). The release of the TCL proceeded from proximal to distal and was localized just radial to the hook of hamate. Complete release was confirmed with the use of dissecting scissors both proximally and distally. Wounds were closed with 5–0 nylon horizontal sutures, and patients were placed in a sterile, soft dressing and were seen at 2-week, 6-week, 6-month, and 12-month clinical visits. Patients who did not return to the clinic were called for post-operative follow-up.
Demographic data were reported as means for continuous data and percentages for categorical data. Continuous variables were evaluated with Student’s t test and categorical variables with the 2-tailed Fisher’s exact test. Pearson correlation coefficients assessed the relationship between pre-operative 2PD scores, post-operative 2PD scores, and patient-reported outcome scores. The one-way analysis of variance (ANOVA) test was used to analyze variance between patients with pre-operative 2PD scores of 10 mm or lower and more than 10 mm.
For determining the appropriate sample size, the QDS was used as the primary outcome. The standard deviation of DASH scores after CTR is approximately 20 points. Based on normative data, the inclusion of 29 patients in each group would provide 80% power and a two-sided alpha of 0.05 based on the Student’s t test. All data were analyzed with statistical significance defined as a p of 0.05.
Results
Eighty-nine hands in 73 patients (52 women, 21 men) with both pre- and early post-operative 2PD scores met the inclusion criteria and were analyzed in this study. Demographic and baseline characteristics reflected those typical of a population with CTS (Table 1). All patients were seen post-operatively for symptom severity follow-up and 2PD measurements at an average of 2 months (range, 2 weeks to 1 year). Phone follow-up to obtain patient-reported outcomes scores was performed at more than 6 months after surgery on 56 patients, with a mean follow-up of 1.8 years post-surgery (range, 7 months to 4.2 years).
Table 1.
Patient demographics and baseline characteristics CTS carpal tunnel syndrome
| Study population characteristics | |
|---|---|
| Age (years) | 68.0 ± 11.0 |
| Sex (M:F) | 21:52 |
| Laterality (R:L) | 51:38 |
| Mean CTS-6 score | 20.4 ± 5.9 |
| Mean in-person follow-up (weeks, range) | 7.6 (2–54) |
| Mean phone follow-up (weeks, range) | 95.1 (19–218) |
There was no correlation observed between the pre-operative 2PD score and long-term post-operative LKSSS, LKFSS, or QDS (Table 2). However, there was further improvement in LKFSS, LKSSS, and QDS at final follow-up compared with immediate post-operative scores. Patients who demonstrated improvement in 2PD scores (higher delta 2PD) in their most affected finger also trended toward greater improvement in LKSSS compared with those with no improvement or worsening in early 2PD scores post-operatively (1.1 vs. 0.56, p = 0.09), although these results were not statistically significant. Mean improvement in QDS was also greater in patients with higher delta 2PD scores compared with those with delta 2PD scores of zero or less (14.6 vs. 8.6, p = 0.35), but this also did not reach statistical significance.
Table 2.
Carpal tunnel symptom severity as measured by patient-rated outcomes and 2PD score at baseline, immediate post-operative, and at > 1-year follow-up
| Patient-reported outcome | Pre-operative | Immediate post-operative | Final follow-up | |||
|---|---|---|---|---|---|---|
| Score | N | Score | N | Score | N | |
| Mean LK score | ||||||
| SSS score | 2.74 ± 0.70 | 30 | 1.94 ± 0.66 | 28 | 1.17 ± 0.54 | 48 |
| FSS score | 2.25 ± 0.82 | 26 | 1.89 ± 0.71 | 24 | 1.17 ± 0.47 | 48 |
| Mean QuickDASH score | 39.11 ± 21.24 | 53 | 25.78 ± 16.88 | 71 | 6.70 ± 13.06 | 56 |
| Mean 2PD (mm) | ||||||
| 1st digit | 6.7 ± 1.2 | 65 | 6.1 ± 1.2 | 63 | ||
| 2nd digit | 6.6 ± 1.3 | 70 | 5.9 ± 1.1 | 65 | ||
| 3rd digit | 6.6 ± 1.2 | 67 | 6.0 ± 1.1 | 60 | ||
| 4th digit | 5.9 ± 1.3 | 87 | 5.8 ± 1.3 | 69 | ||
| 5th digit | 5.5 ± 1.2 | 86 | 5.8 ± 1.2 | 70 | ||
| Most affected radial digit, measurable | 7.2 ± 1.1 | 60 | 6.4 ± 1.2 | 59 | ||
LK, Levine-Katz; FSS, functional status score; SSS, symptom severity score
The mean pre- and early post-operative 2PD score was 7.2 mm (n = 60) and 6.4 mm (n = 59) in the most affected radial digit when measurable, respectively. Regression statistics were computed on the 86 patients with both pre- and post-operative 2PD scores. There was a positive correlation between pre- and early post-operative 2PD scores (r2 = 0.61, p < 0.001, Fig. 1). Additionally, a higher initial 2PD (up to 10 mm) was associated with greater improvement in 2PD (higher delta 2PD) post-operatively (r2 = 0.088, p = 0.006).
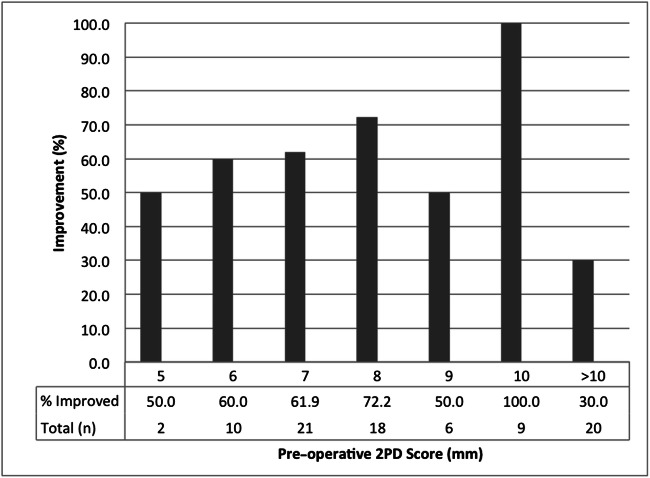
Fig. 1.
Percent of patients demonstrating improvement in 2PD score from pre- to post-operative based on pre-operative most affected digit 2PD score.
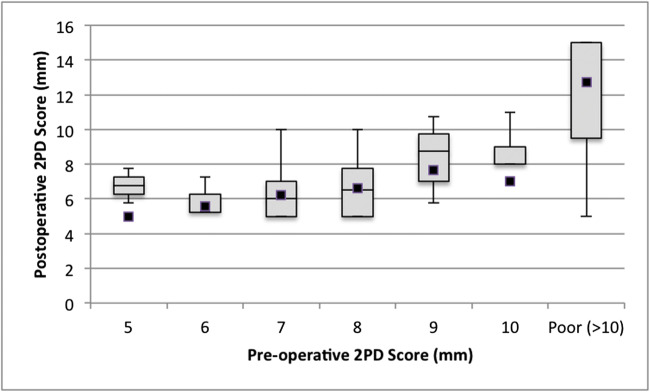
Twenty patients had poor static 2PD, greater than 10 mm, at baseline. Patients with higher than 10-mm pre-operative 2PD score were the least likely to demonstrate post-operative improvement in 2PD score from baseline, with only 30% (6/20) of patients demonstrating improvement (p = 0.03, Fig. 2). In contrast, 68.8% (44/64) of patients with measurable 2PD at baseline demonstrated improvement after surgery. Patients with pre-operative 2PD score of more than 10 mm also had the most variable improvement in early post-operative 2PD scores (Fig. 3) compared with patients with baseline 2PD of 10 mm or lower (F = 10.167, p = 0.002).
Fig. 2.
Variation in post-operative 2PD scores based on pre-operative 2PD score of most affected digit. The higher the pre-operative 2PD score, the more variable the recovery of 2PD post-operatively.
Fig. 3.
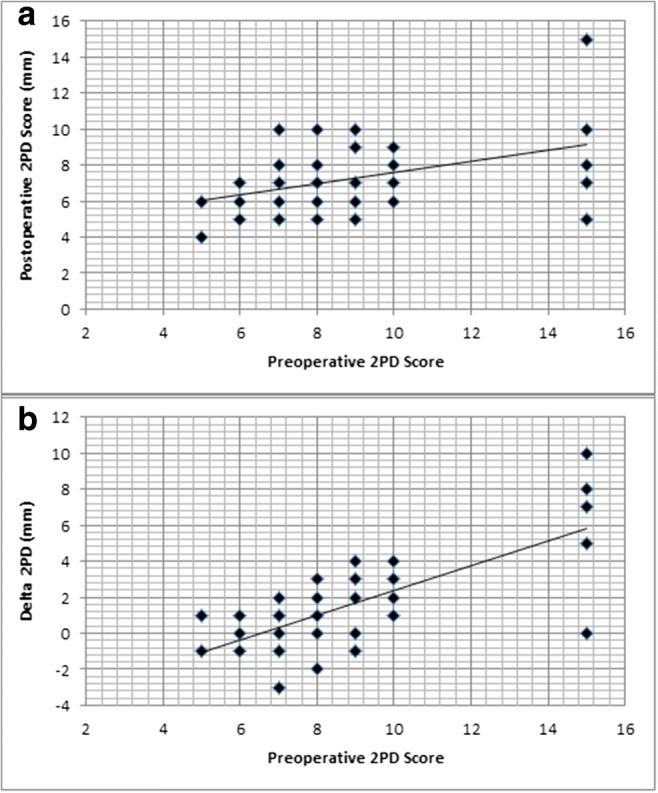
Linear regression comparing pre-operative 2PD score with post-operative 2PD score (Pearson correlation, 0.780; p < 0.001) demonstrates greater variability in post-operative 2PD scores in those with pre-operative scores > 10 mm (a); however, this population also demonstrates the greatest post-operative improvement with the greatest mean delta 2PD (Pearson correlation, 0.288; p = 0.006) (b)
Discussion
The results of our study demonstrate that pre-operative 2PD score was positively correlated with early post-operative 2PD score but that higher pre-operative 2PD scores did not lead to worse patient-reported outcomes scores at an average of 1.8 years post-operatively. Patients with pre-operative 2PD score of more than 10 mm were least likely to demonstrate improvement in 2PD scores at an early post-operative time point. However, improvement in 2PD score was not correlated with better long-term patient-reported outcomes scores following CTR.
Our study has several limitations. Data were collected retrospectively and as a result, post-operative evaluation of 2PD occurred at variable time points at an average of 2 months following CTR. As improvement in 2PD can take several months, no definitive conclusions regarding final 2PD can be made from these data. For example, some patients in all groups demonstrated interval increases in 2PD at early follow-up (Fig. 3a). We believe that this likely represents early inflammatory changes that might resolve at later follow-up. However, we believe that symptoms represent the more important outcome in this setting, and previous studies have attempted to identify when patients experience maximal improvement in symptoms post-CTR. Brown et al. found patients experienced maximal resolution of paresthesia within 3 weeks of CTR but that functional status improved more gradually [6]. While we do not know the time of maximum recovery of 2PD, we believe that post-operative follow-up at 2 months reflects a clinically relevant period for tracking patient physical examination and a clinically useful indicator to share with physicians. Another limitation of our study was our long-term (greater than 1 year) phone follow-up response rate of only 76.7% (56/73) with regard to patient-reported outcomes data, which may have introduced selection bias. However, this follow-up rate is in line with prior studies in the hand surgery literature [17]. We believe that this may have skewed our results toward worse patient-reported outcomes scores, since asymptomatic patients may have been less likely to respond to inquiries about surgery.
2PD testing is cost-effective and simple to perform in the surgeon’s office [10]. This clinical test became widely accepted after the development of a handheld testing device in the 1980s. Since that time, 2PD scores have been included in many studies as an objective measure of denervation and recovery after nerve repair and decompression [8, 14]. The test has a high interobserver agreement and correlates with normative values for innervation density [8, 12, 16].
It remains controversial whether a 2PD score correlates with symptom severity and function. Some studies have shown that innervation density as measured by 2PD is associated with function, and changes in 2PD score are apparent even in patients with mild CTS [7, 16]. However, other studies have shown no association between 2PD score and symptom severity [3]. A seminal study by Gelberman et al. demonstrated that the while the threshold tests (e.g., Semmes-Weinstein monofilament test) consistently demonstrated gradual decreases in nerve function, 2PD testing remained normal until almost all sensory conduction had ceased [11]. Furthermore, Elfar et al. identified that 2PD score only weakly correlates with electrodiagnostic study findings [9].
As a result, it is unclear whether 2PD scores can be used to predict surgical outcome [5]. Some surgeons counsel patients that when there is constant numbness in a finger (or clinically absent 2PD), there may be no or minimal improvement in this symptom after CTR. The results of our study suggest that 60% of patients with pre-operative 2PD score of over 10 mm did not demonstrate improvement following CTR. Of more clinical relevance, however, is the finding of our study that pre-operative 2PD score did not predict patient-reported outcomes in the post-operative period, although pre-operative 2PD score did correlate with post-operative 2PD score. In other words, more severe pre-operative 2PD scores predicted more severe post-operative 2PD scores, but post-operative 2PD scores did not necessarily correlate with subjective patient-reported outcomes scores.
In conclusion, we identified that patients with pre-operative 2PD of more than 10 mm have more variable and decreased ability to recover 2PD after CTR compared with those with measurements between 5 and 10 mm. We additionally identified that no absolute pre-operative 2PD threshold predicts patient-reported outcomes after CTR, considering that there were similar improvements in scores. This suggests that the examination could potentially be shortened to evaluate 2PD at a threshold at two clinically relevant thresholds: (1) normal sensation, with testing at 5 mm, and (2) decreased innervation, with testing at 10 mm. This information could be useful in pre-operative counseling on recovery of digital sensation, as well as consistency of patient-reported outcomes.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Acknowledgments
We would like to thank Elizabeth Herbert, PA, for her assistance in performing physical examination on study patients.
Compliance with Ethical Standards
Conflict of Interest
Charles M. Ekstein, MD, Danielle C. Marshall, BA, and Aaron Z. Chen, BA, declare that they have no conflicts of interest. Lauren E. Wessel, MD, reports grants from the American Foundation for Surgery of the Hand (AFSH) fast track award and the Hospital for Special Surgery (HSS) Surgeon-in-Chief award. Daniel A. Osei, MD, reports grants from the National Institutes of Health, the US Department of Defense, and the American Society for Surgery of the Hand (ASSH) Richard H. Gelberman scholar award. Duretti T. Fufa, MD, reports personal fees as a consultant to Medartis and grants from the ASFH fast track research award, the HSS Surgeon-in-Chief award, and the ASSH Richard H. Gelberman scholar award.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level III, Prognostic Study
References
- 1.American Society for Surgery of the Hand . The hand, examination and diagnosis. New York: Churchill Livingstone; 1990. [Google Scholar]
- 2.Atroshi I, Lyren PE, Ornstein E, Gummesson C. The six-item CTS Symptoms Scale and Palmar Pain Scale in carpal tunnel syndrome. J Hand Surg Am. 2011;36(5):788–794. [DOI] [PubMed]
- 3.Atroshi I, Axelsson G, Gummesson C, Johnsson R. Carpal tunnel syndrome with severe sensory deficit: endoscopic release in 18 cases. Acta Orthop Scand. 2000;71(5):484–487. doi: 10.1080/000164700317381180. [DOI] [PubMed] [Google Scholar]
- 4.Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosen I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;281(2):153–158. doi: 10.1001/jama.282.2.153. [DOI] [PubMed] [Google Scholar]
- 5.Bae JY, Kim JK, Yoon JO, Kim JH, Ho BC. Preoperative predictors of patient satisfaction after carpal tunnel release. Rev Chir Orthop Traumatol. 2018;104(6):613. doi: 10.1016/j.otsr.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 6.Brown R, Gelberman R, Seiler J, et al. Carpal tunnel release: a prospective randomized assessment of open and endoscopic methods. J Bone Jt Surg Am. 1993;75(9):1265–1275. doi: 10.2106/00004623-199309000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Dellon AL, Kallman CH. Evaluation of functional sensation in the hand. J Hand Surg Am. 1983;8(6):865–870. [DOI] [PubMed]
- 8.Djerbi I, Cesar M, Lenoir H, Coulet B, Lazerges C, Chammas M. Revision surgery for recurrent and persistent carpal tunnel syndrome : clinical results and factors affecting outcomes. Chir Main. 2015;34(6):312–317. doi: 10.1016/j.main.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Elfar JC, Yaseen Z, Stern PJ, Kiefhaber TR. Individual finger sensibility in carpal tunnel syndrome. J Hand Surg Am. 2010;35(11):1807–1812. [DOI] [PMC free article] [PubMed]
- 10.Eryilmaz M, Koçer A, Kocaman G, Dikici S. Two-point discrimination in diabetic patients. J Diabetes. 2013;5(4):442–448. doi: 10.1111/1753-0407.12055. [DOI] [PubMed] [Google Scholar]
- 11.Gelberman RH, Szabo RM, Williamson RV, Dimick MP. Sensibility testing in peripheral-nerve compression syndromes. J Bone Jt Surg Am. 1983;65-A(5):632–638. doi: 10.2106/00004623-198365050-00008. [DOI] [PubMed] [Google Scholar]
- 12.Gellis M, Pool R. Two-point discrimination distances in the normal hand and forearm: application to various methods of fingertip reconstruction. Plast Reconstr Surg. 1977;59(1):57–63. doi: 10.1097/00006534-197701000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Gerr E, Letz R. The sensitivity and specificity of tests for carpal tunnel syndrome vary with the comparison subjects. J Hand Surg Br. 1998;23B(2):151–155. [DOI] [PubMed]
- 14.Poppen NK, McCarroll HR, Doyle JR, Niebauer JJ. Recovery of sensibility after suture of digital nerves. J Hand Surg Am. 1979;4(3):212–226. [DOI] [PubMed]
- 15.Weber E. Ueber den tastsinn. Arch Anat Physiol Wissen Med Muller’s Arch. 1835;1:152–159. [Google Scholar]
- 16.Wolny T, Linek P. Reliability of two-point discrimination test in carpal tunnel syndrome patients. Physiother Theory Pract. 2019;35(4):348–354. doi: 10.1080/09593985.2018.1443358. [DOI] [PubMed] [Google Scholar]
- 17.Nota S, Strooker JA, Ring D. Differences in response rates between mail, e-mail, and telephone follow-up in hand surgery research. Hand. 2014;9(4):504–510. doi: 10.1007/s11552-014-9618-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)