Abstract
Context
Anterior cruciate ligament reconstruction (ACLR) and gait speed are risk factors for developing knee osteoarthritis (OA). Measuring minute-level cadence during free-living activities may aid in identifying individuals at elevated risk of developing slow habitual gait speed and, in the long term, OA.
Objective
To assess differences in peak 1-minute cadence and weekly time in different cadence intensities between individuals with and without ACLR.
Design
Cross-sectional study.
Setting
Short-term, free-living conditions.
Patients or Other Participants
A total of 57 participants with ACLR (34 women, 23 men; age = 20.9 ± 3.2 years, time since surgery = 28.7 ± 17.7 months) and 42 healthy control participants (22 women, 20 men; age = 20.7 ± 1.7 years).
Main Outcome Measure(s)
Each participant wore a physical activity monitor for 7 days. Data were collected at 30 Hz, processed in 60-second epochs, and included in the analyses if the activity monitor was worn for at least 10 hours per day over 4 days. Mean daily steps, peak 1-minute cadence, and weekly minutes spent at 60 to 79 (slow walking), 80 to 99 (medium walking), 100 to 119 (brisk walking), ≥100 (moderate- to vigorous-intensity ambulation), and ≥130 (vigorous-intensity ambulation) steps per minute were calculated. One-way analyses of covariance were conducted to determine differences between groups, controlling for height and activity-monitor wear time.
Results
Those with ACLR took fewer daily steps (8422 ± 2663 versus 10 033 ± 3046 steps; P = .005) and spent fewer weekly minutes in moderate- to vigorous-intensity cadence (175.8 ± 116.5 minutes versus 218.5 ± 137.1 minutes; P = .048) than participants without ACLR. We observed no differences in minutes spent at slow (ACLR = 77.4 ± 40.5 minutes versus control = 83.9 ± 34.3 minutes; P = .88), medium (ACLR = 71.6 ± 40.2 minutes versus control = 82.9 ± 46.8 minutes; P = .56), brisk (ACLR = 115.3 ± 70.3 minutes versus control = 138.3 ± 73.3 minutes; P = .18), or vigorous-intensity (ACLR = 24.3 ± 36.5 minutes versus control = 38.1 ± 60.9 minutes; P = .10) cadences per week.
Conclusions
Participants with ACLR walked approximately 40 fewer minutes per week in moderate- to vigorous-intensity cadence than participants without ACLR. Increasing the time spent at cadence ≥100 steps per minute and overall volume of physical activity may be useful as interventional targets to help reduce the risk of early development of OA after ACLR.
Keywords: step accumulation, walking gait, physical activity, knee, osteoarthritis
Key Points
Cadence can be assessed using commercially available or research-grade wearable accelerometers over the course of weeks or months for an accurate depiction of a patient's habitual gait pattern during activities of daily living.
Participants with primary unilateral anterior cruciate ligament reconstruction within the last 5 years took an average of 1611 fewer steps per day and spent 42.7 fewer minutes throughout the week in ambulatory activities of at least 100 steps per minute than did participants without anterior cruciate ligament reconstruction.
Less time spent at higher levels of cadence may indicate an elevated risk of knee osteoarthritis that can be feasibly assessed using wearable activity monitors.
Knee-joint osteoarthritis (OA) results in persistent knee pain, reduced quality of life, daily disability, and diminished participation in physical activity that is unlikely to improve as the disease progresses.1,2 More than 50% of individuals who experience an anterior cruciate ligament (ACL) injury and undergo ACL reconstruction (ACLR) will develop knee OA evident on radiographs within 2 decades of surgery.3 These findings are concerning because ACL injury is most likely to occur among physically active individuals between the ages of 13 and 25 years,4 meaning that half of these individuals may experience a permanent degenerative knee condition before 50 years of age.3 Developing and implementing clinically feasible tools that allow detection of the initiation or progression of knee OA among a high-risk population, such as young people with ACLR, is a critical step toward secondary prevention of this lifelong degenerative condition.
Minute-level cadence, or the number of steps an individual takes during a given minute during the day, has been implicated in the progression of slow gait speed among middle-aged individuals at high risk for knee OA and individuals with diagnosed knee OA later in the lifespan when measured under free-living conditions.5 The advantage of evaluating cadence as opposed to more traditional temporal gait variables, such as gait speed, that are assessed in a controlled environment (ie, laboratory or clinic setting) is that it can be measured using commercially available or research-grade wearable accelerometers over weeks or months.6 Such long-term monitoring allows for a more accurate depiction of a patient's habitual gait pattern during activities of daily living (ADLs) than in a clinic or laboratory setting. Whereas individuals with ACLR have demonstrated reduced moderate to vigorous physical activity in free-living conditions7 and persistent kinematic and kinetic alterations during walking gait in laboratory settings8 when compared with healthy peers, it remains unclear whether their temporal gait patterns under free-living conditions differ from those of individuals who have not experienced a traumatic knee injury. The ability to assess temporal gait characteristics in free-living conditions using wearable accelerometers represents a key advancement in researchers' ability to identify individuals who avoid walking at different cadence intensities during ADLs, which may be a target for intervention that extends outside of the direct observation afforded in the clinical environment.
Cadence has been used to help understand average gait speed, peak gait speed, and cadence characteristics under free-living conditions.9–11 This is important because slower average gait speed and cadence have been identified as risk factors for functional limitation, chronic disease morbidity, and premature mortality among older adults when assessed in the clinical environment.5,12 Researchers5 have hypothesized that reduced gait speed and physical activity engagement and, therefore, reduced cadence may result from biomechanical compensations adopted by patients to avoid pain and maximize functional capacity during ADLs despite underlying articular cartilage degeneration. Specifically, reductions in average daily step count13 and minutes per week in a moderate- to vigorous-intensity cadence (≥100 steps per minute) have been identified among individuals with and at elevated risk for knee-joint OA.5 However, investigators14 have also hypothesized that walking at slower speeds may reduce the magnitude and rate of knee-joint loading that occurs during ambulation, resulting in alterations in articular cartilage structure and metabolism in individuals with a history of ACLR. Although cadence is not a direct indicator of gait speed,15 it is clear that an individual's cadence and physical activity intensity and volume, which are associated with knee articular cartilage health,14 contribute to habitual gait speed. Therefore, cadence is a potential variable of interest for researchers and clinicians focused on preventing or slowing the progression of knee OA.
To our knowledge, free-living cadence has not been assessed in individuals with a history of ACLR despite their increased risk of knee OA. Understanding the effect of ACLR on habitual free-living cadence may provide insight into the mechanism underlying rapid progression of knee OA after ACLR. It may also enable the development of clinically feasible interventions using commercially available wearable technology to address reductions in daily ambulatory behavior both during and after structured rehabilitation. Therefore, the primary purpose of our study was to assess differences in mean daily steps and peak 1-minute cadence and minutes per week in moderate- to vigorous-intensity cadence (≥100 steps per minute) during ambulation. We hypothesized that individuals with a history of ACLR would demonstrate fewer average steps per day, smaller peak 1-minute cadence, and fewer minutes per week in moderate- to vigorous-intensity cadence than individuals without a history of ACLR. Our secondary purpose was to explore differences in weekly time spent in slow (60–79 steps per minute), medium (80–99 steps per minute), brisk (100–119 steps per minute), and vigorous-intensity (≥130 steps per minute) cadence between individuals with and without a history of ACLR. We proposed that these metrics would not differ between individuals with and those without a history of ACLR.
METHODS
Participants
Participants were recruited from the university campus and sports medicine clinics at Michigan State University and the University of Wisconsin–Madison via flyers, emails, and word of mouth. Volunteers were included in the study if they were between the ages of 18 and 40 years. They were assigned to the ACLR group if they reported a history of primary unilateral ACLR within 5 years of enrollment. We used these criteria for participant age and time since surgery to limit the likelihood that participants would be experiencing symptoms or functional limitations related to OA.3,16 Volunteers were excluded from the study if they reported a history of lower extremity injury in the 6 weeks before data collection, had any history of lower extremity surgery, or had any chronic medical condition that might have affected their ability to participate in physical activity. Weekly moderate-to-vigorous physical activity and daily step-count data from all healthy participants (n = 42) and most ACLR participants (n = 41) were included in a previous study7 that assessed differences in physical activity outcomes between individuals with and those without a history of ACLR.
All participants provided written informed consent, and this multisite, cross-sectional study was approved by the institutional review boards of Michigan State University and the University of Wisconsin–Madison.
Surveys
Participants completed the International Knee Documentation Committee (IKDC) Subjective Knee Evaluation form to rate their knee-related function and the Tegner Activity Scale (TAS) to rate their peak level of activity at the time of enrollment. The IKDC is a valid and reliable assessment of knee-related function scored on a 100-point scale, with 100 indicating optimal function.17 The TAS is a valid and reliable survey for individuals with a history of ACLR that consists of an 11-point Likert scale, with a score of 0 indicating participant is unable to complete any sport or recreational activity due to disability and a score of 10 indicating participant competes in professional or collegiate levels of sport on a regular basis.18
Cadence Data Collection and Data Processing
Participants were instructed to wear an ActiGraph wGT3X-BT or GT9X Link monitor (ActiGraph, LLC, Pensacola, FL) for 7 days during all waking hours except in water (ie, swimming activities). Researchers19 have reported good agreement between triaxial and uniaxial counts of the 2 monitors. Triaxial and uniaxial counts are also strongly correlated with step counts.20 These results have indicated that the monitors can be used interchangeably in research studies.19 Relevant data-collection and data-analysis methods are reported in Table 1 in compliance with the guidelines recommended by Montoye et al.21 Accelerometry data were processed in ActiLife (version 6.13; ActiGraph, LLC), and mean daily step count and the number of steps completed in every 60-second epoch22 on days with adequate wear time were reported. Wear-time validation was based on previously reported criteria23 and described in Table 1. For each validated day, nonwear time was removed according to previously established criteria,23 and all remaining data were exported to determine individual cadence outcomes. Peak 1-minute cadence was defined as the greatest number of steps per minute accumulated over the entire valid wear period. This metric is believed to reflect the best natural effort put forth by a participant during the wear period.12 The weekly time spent at different cadence intensities was calculated as the number of minutes with 60 to 79, 80 to 99, 100 to 119, ≥100, and ≥130 steps per minute during the valid wear period. Cadence intensities in laboratory settings were defined as slow walking (60–79 steps per minute), medium walking (80–99 steps per minute), brisk walking (100–119 steps per minute), moderate- to vigorous-intensity ambulation (≥100 steps per minute), and vigorous-intensity ambulation (≥130 steps per minute).
Table 1.
Accelerometer Data-Collection and -Analysis Methodsa
| Item |
Method |
| Model of accelerometer | ActiGraphb model wGT3X-BT and GT9X Link monitors |
| Data-collection sampling rate | 30 Hz7 |
| Data-analysis epoch length | 60 s20 |
| Placement of accelerometer | Anterior axillary line, right hip20 |
| No. of participants receiving accelerometer | 99 |
| Accelerometer distribution | In person |
| Data collection at each time point | 7 d |
| Criteria for defining nonwearing of accelerometer | Minimum length: 90 min Small window length: 30 min Spike tolerance: 2 min21 |
| Accelerometer data needed to be included in analysis | |
| No. of valid days | ≥4 (3 weekend days, 1 weekend)21 |
| No. of min/d | 600 min21 |
| Accelerometer-data physical activity outcome of interest and interpretation method | Steps per min |
Based on recommendations of accelerometry reporting methods.19
ActiGraph, LLC, Pensacola, FL.
Statistical Analysis
We calculated independent-samples t tests to compare characteristics between individuals with and those without a history of ACLR. The Fisher exact test and Mann-Whitney U test were performed to compare sex frequency distribution and TAS scores between groups. Researchers24 have reported that an individual's height influences cadence, especially at moderate to vigorous intensities; therefore, height was also entered as a covariate in subsequent analyses. Individual analysis-of-covariance tests, controlling for height24 and activity-monitor wear time, were used to compare cadence characteristics between groups. We evaluated and excluded participant age (see Supplemental Figure 1, available online at http://dx.doi.org/10.4085/1062-6050-425-19.S1) and time since surgery (see Supplemental Figure 2) as potential covariates due to their lack of relationship with average daily step count, peak 1-minute cadence, and weekly minutes in moderate- to vigorous-intensity cadence. Pooled partial η2 effect sizes were calculated to assess the magnitude of differences between groups for each outcome. Pooled partial η2 effect sizes were interpreted as small (0.01–0.05), medium (0.06–0.13), or large (≥0.14).25 The α level was set a priori at .05. All analyses were completed using SPSS (version 24.0; IBM Corp, Armonk, NY).
RESULTS
The ACLR and control groups did not differ on the basis of sex (P = .54), age (t97 = −0.351, P = .73), height (t97 = 1.206, P = .23), or mass (t97 = −0.156, P = .88; Table 2). The ACLR group demonstrated lower IKDC scores (t97 = 6.999, P < .001) and TAS scores (U = 823.0, P = .007) at study enrollment than did the control group (Table 2).
Table 2.
Participant Characteristics
| Characteristic |
Group |
P Value |
|
| Control |
Anterior Cruciate Ligament Reconstruction |
||
| Sex, male/female, No. | 20/22 | 23/34 | .54 |
| Mean ± SD or Median (Minimum–Maximum Outcome) |
|||
| Age, y | 20.7 ± 1.7 (18–25) | 20.9 ± 3.2 (18–32) | .73 |
| Height, m | 1.8 ± 0.1 (1.5–1.9) | 1.7 ± 0.1 (1.6–2.0) | .23 |
| Mass, kg | 72.9 ± 12.0 (49.9–103.0) | 73.3 ± 13.6 (52.0–109.0) | .88 |
| International Knee Documentation Committee score (0–100 scale) | 98.5 ± 3.1 (86.2–100.0) | 84.0 ± 13.1 (40.0–100.0) | <.001a |
| Tegner Activity Scale score (0–10 scale) | 7 (4–10) | 6 (2–10) | .007a |
| Activity monitor wear time, min | 5638.6 ± 1418.4 (2661–8737) | 5393.1 ± 1096.3 (3143–7772) | .33 |
| Time since surgery, mo | NA | 28.7 ± 17.7 (6–60) | NA |
Abbreviation: NA, not applicable.
Indicates between-groups difference (P < .05).
The ACLR group took fewer average daily steps than did the control group (F1,95 = 8.201, P = .005; Figure), but the groups did not differ on the basis of peak 1-minute cadence (F1,95 < 0.001, P > .99), which partially confirmed our primary hypothesis (Table 3). The ACLR group spent less weekly time at ≥100 steps per minute (Figure) than did the control group (F1,95 = 4.003, P = .048). The ACLR group did not differ from the control group on the basis of weekly time walking at 60 to 79 (F1,95 = 0.022, P = .88), 80 to 99 (F1,95 = 0.335, P = .56), 100 to 119 (F1,95 = 1.853, P = .18), or ≥130 (F1,95 = 2.848, P = .10) steps per minute, which confirmed our secondary hypothesis (Table 3).
Figure.
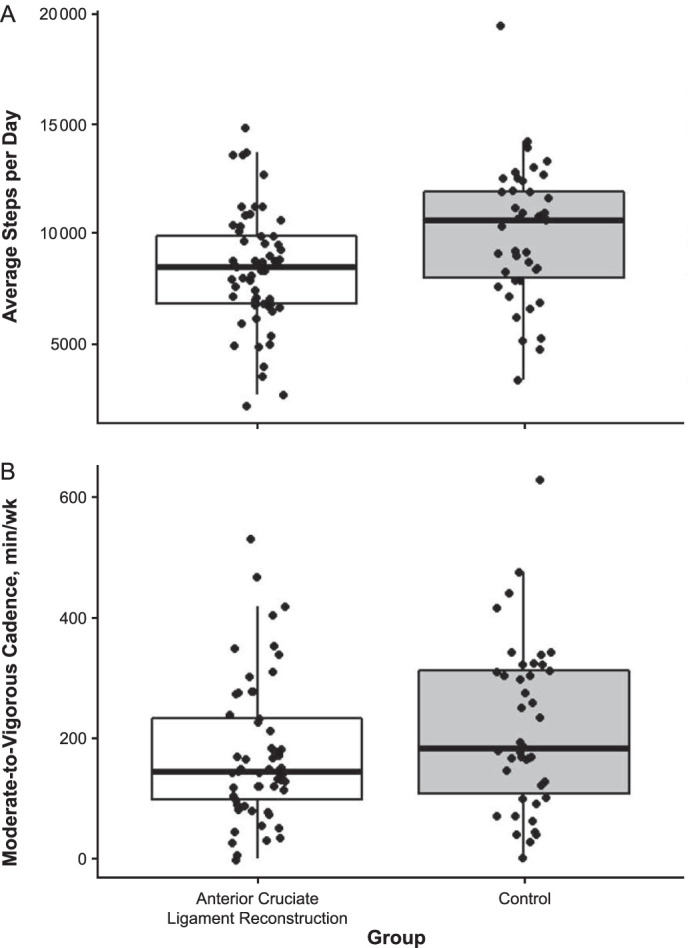
Average step count (steps per day) and time spent in moderate- to vigorous-intensity cadence (steps per minute) among individuals with and those without a history of anterior cruciate ligament reconstruction. The horizontal line indicates the median value, the box represents the interquartile range, and the dots represent individual outcomes.
Table 3.
Unadjusted Cadence (Steps per Minute) Outcome Differences Between Individuals With and Without a History of Anterior Cruciate Ligament Reconstruction
| Cadence Outcome |
Group, Mean ± SD |
P Value |
Partial η2 Effect Size |
|
| Control |
Anterior Cruciate Ligament Reconstruction |
|||
| No. of steps/d | 10 033 ± 3046 | 8422 ± 2663 | .005a | 0.079 |
| No. of steps/min | ||||
| Mean | 11.3 ± 3.4 | 10.0 ± 3.0 | .047a | 0.041 |
| Maximum | 151.2 ± 25.3 | 152.2 ± 23.4 | >.99 | 0.000 |
| Weekly time spent in cadence, min | ||||
| 60–79 steps/min | 83.9 ± 34.3 | 77.4 ± 40.5 | .88 | <0.001 |
| 80–99 steps/min | 82.9 ± 46.8 | 71.6 ± 40.2 | .56 | 0.004 |
| 100–119 steps/min | 138.3 ± 73.3 | 115.3 ± 70.3 | .18 | 0.019 |
| ≥100 steps/min | 218.5 ± 137.1 | 175.8 ± 116.5 | .048a | 0.040 |
| ≥130 steps/min | 38.1 ± 60.9 | 24.3 ± 36.5 | .10 | 0.029 |
Indicates between-groups difference (P < .05) when using height (cm) and wear time (min) as covariates.
DISCUSSION
We sought to determine whether individuals with ACLR displayed patterns of reduced free-living cadence when compared with individuals without a history of knee injury because less time spent in moderate- to vigorous-intensity ambulation is a risk factor for developing habitually slow gait speed, which has been linked to the development and progression of chronic disease.5 We opted to focus on free-living cadence because it can be assessed using cost-effective and clinically feasible tools,9 and effective interventions to enhance cadence during free-living activities can be developed using commercially available wearable and mobile technologies.6 Individuals in the ACLR group spent less time per week walking in a manner that enabled them to accumulate at least 100 steps per minute than did the individuals in the control group despite a lack of between-groups differences in peak 1-minute cadence rates. We chose the threshold of ≥100 steps per minute in accordance with past work9–11 to indicate the minimum threshold for moderate- to vigorous-intensity physical activity. Time spent at this intensity would contribute to meeting national physical activity guidelines.26 These findings are consistent with patterns previously observed among individuals with knee OA and may highlight a risk factor that can be feasibly assessed under free-living conditions early after ACLR.
Bell et al7 reported that individuals with ACLR participated in 65 fewer minutes or moderate to vigorous physical activity per week than control individuals matched for age, sex, and activity level. Those with ACLR were 2.36 times less likely to be categorized as physically active,27 based on the 2018 Physical Activity Guidelines Advisory Committee recommendation of at least 150 minutes of moderate- to vigorous-intensity activity per week to reduce the risks of chronic noncommunicable disease morbidity and all-cause mortality.26 Whereas not a direct measure of physical activity intensity among individuals with ACLR, daily step count is a clinically feasible measure that is strongly related to time engaged in moderate to vigorous physical activity in this population.7 In our study, the ACLR group took fewer steps per day than did the control group (8422 ± 2663 steps per day versus 10 033 ± 3046 steps per day), and the differences in step counts were similar to those described by Bell et al7 (8158 ± 2780 steps per day versus 9769 ± 2785 steps per day) and Baez et al28 (7754 ± 2399 steps per day versus 9199 ± 2385 steps per day) among similar populations. We are the first to identify that, in addition to diminished daily step counts, the ACLR group also displayed less average minute-level cadence at high step rates than the control group (Figure). Although different, the magnitude of difference between groups was medium for steps per day but small for time spent at a cadence ≥100 steps per minute. Given that both diminished participation in physical activity and slower walking speeds are risk factors for developing knee OA, regardless of ACLR status, our findings highlight a concerning pattern of reduced activity and lower average cadence in this population that is already at elevated risk for developing OA.
In addition to assessing traditional activity outcomes, such as average daily step count, we also evaluated the intensity of walking, which was defined as the time spent at different steps-per-minute intensities under free-living conditions. Consistently walking with a cadence pattern that corresponds to moderate- to vigorous-intensity ambulation (≥100 steps per minute) has been linked with numerous musculoskeletal and general health benefits; however, the focus of this research has generally been in older populations who are at elevated risk of noncommunicable disease-related morbidity.5,13 In our study of young individuals, the ACLR group also spent fewer minutes per week at ≥100 steps per minute than did the control group. These results are consistent with observations in older individuals at risk for noncommunicable chronic disease. For example, in 2 recent studies, individuals aged ≥50 years who had either been diagnosed as having knee OA or identified as having an elevated risk of knee OA were less likely to develop high-risk, slow gait speeds if they regularly took at least 6000 steps per day13 or replaced 5 to 20 minutes per day of slow walking with intentional walking at speeds ≥100 steps per minute.5 Participants with a history of ACLR in our study were, on average, less than 5 years postsurgery, indicating that changes in volume and time spent in moderate- to vigorous-intensity ambulation may begin to manifest as early as a few years after reconstructive surgery in young individuals, 20 years old on average. These differences suggest that individuals may engage in less volume or frequency of mechanical loading at the knee joint during weight-bearing activities after ACLR. Diminished mechanical loading, including slow gait speed, is a risk factor for poor knee-joint health after ACLR.14 Research in which the relationships between volume and intensity of mechanical knee-joint loading and knee-joint health are assessed is needed to help us understand modifiable risk factors and their association with developing knee OA after ACLR.
Cadence intensities of 100 steps per minute and 130 steps per minute have been associated with moderate-intensity (3 metabolic equivalents) and vigorous-intensity (6 metabolic equivalents) ambulation in laboratory settings, respectively.11,12 We observed that the ACLR group spent less time in moderate- to vigorous-intensity ambulation (Table 3) than the control group. Although ambulating at moderate to vigorous intensity has important health indications, it may be difficult for individuals to understand whether they are achieving these activity intensities without real-time or rapid postactivity sources of feedback. Consumer-grade technology paired with easy-to-use mobile applications can provide people with real-time feedback on steps taken per minute and minutes per day in which they achieve moderate- to vigorous-intensity walking, which may help them track and maintain healthy walking-intensity patterns during ADLs under free-living conditions. For example, prescribing the cadence intensity goal of 3000 steps in 30 minutes, which is based on 100 steps per minute, or providing individuals with music with a tempo of 100 to 105 beats per minute through a mobile application may help them to maintain moderate- to vigorous-intensity ambulation and increase the time spent in moderate to vigorous physical activity.29,30 The ability to integrate such approaches among young individuals with ACLR, who are more likely to have diminished step counts and time spent in ≥100 steps per minute, may provide a feasible strategy for early intervention. Interventions targeting these deficits may help promote healthy physical activity behaviors and mitigate the risk of knee OA-related morbidity.
Several limitations should be considered when evaluating the findings of our study. This study was cross-sectional in nature and featured a relatively heterogeneous sample of individuals with ACLR. Based on these limitations, it is unclear whether our participants exhibited reduced cadence before injury or surgery, which is a clear area for future investigation. Also, we did not consistently collect information about concomitant injuries or surgical procedures. Factors such as concomitant meniscectomies at the time of ACLR surgery have been reported to influence physiological outcomes after ACLR and should be explored by future authors. Our participants ranged in age from 18 to 32 years, which may have presented different limitations to physical activity due to their lifestyle. On the contrary, the most recent guidelines26 recommended the same physical activity for individuals between the ages of 18 to 64 years, indicating that healthy physical activity behaviors are achievable across the age range of participants in this study. In addition, cadence as an outcome measure is not without limitations. Dall et al15 clarified that cadence, although instructive about changes in gait characteristics under free-living conditions, should not be considered an analog for gait speed due to the indirect nature of cadence assessment via accelerometry data. However, it does describe an important activity-based behavior that has been associated with slow gait speeds in injured populations. It is also captured in free-living situations and not in laboratory settings. In subsequent investigations, researchers should consider the use of wearable technology that can provide concurrent assessment of gait speed and cadence in this population.
CONCLUSIONS
Walking is among the first functional tasks in the rehabilitation process after ACLR because of its importance for ADLs and the restoration of normal knee-joint loading in a population at elevated risk for knee OA. Those with a history of primary unilateral ACLR within the 5 years before the study appeared to spend less weekly time in ambulatory activities of at least 100 steps per minute than individuals without a history of ACLR. Although the optimal level of cadence for an individual with ACLR both during and after the rehabilitation process remains unclear, diminished time spent at higher cadence intensities may indicate an elevated risk of knee OA that can be feasibly assessed using wearable activity monitors.
Supplementary Material
REFERENCES
- 1.Han A, Gellhorn AC. Trajectories of quality of life and associated risk factors in patients with knee osteoarthritis: findings from the Osteoarthritis Initiative. Am J Phys Med Rehabil. 2018;97(9):620–627. doi: 10.1097/PHM.0000000000000926. [DOI] [PubMed] [Google Scholar]
- 2.Dunlop DD, Song J, Semanik PA, et al. Objective physical activity measurement in the Osteoarthritis Initiative: are guidelines being met? Arthritis Rheum. 2011;63(11):3372–3382. doi: 10.1002/art.30562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luc B, Gribble PA, Pietrosimone BG. Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train. 2014;49(6):806–819. doi: 10.4085/1062-6050-49.3.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. doi: 10.1177/0363546514542796. [DOI] [PubMed] [Google Scholar]
- 5.Fenton SAM, Neogi T, Dunlop D, et al. Does the intensity of daily walking matter for protecting against the development of a slow gait speed in people with or at high risk of knee osteoarthritis? An observational study. Osteoarthritis Cartilage. 2018;26(9):1181–1189. doi: 10.1016/j.joca.2018.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dobkin BH, Dorsch A. The promise of mHealth: daily activity monitoring and outcome assessments by wearable sensors. Neurorehabil Neural Repair. 2011;25(9):788–798. doi: 10.1177/1545968311425908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bell DR, Pfeiffer KA, Cadmus-Bertram LA, et al. Objectively measured physical activity in patients after anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(8):1893–1900. doi: 10.1177/0363546517698940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slater LV, Hart JM, Kelly AR, Kuenze CM. Progressive changes in walking kinematics and kinetics after anterior cruciate ligament injury and reconstruction: a review and meta-analysis. J Athl Train. 2017;52(9):847–860. doi: 10.4085/1062-6050-52.6.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ayabe M, Aoki J, Kumahara H, Tanaka H. Assessment of minute-by-minute stepping rate of physical activity under free-living conditions in female adults. Gait Posture. 2011;34(2):292–294. doi: 10.1016/j.gaitpost.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 10.Marshall MR, Montoye AHK, George AJ. Pregnancy walking cadence does not vary by trimester. Gait Posture. 2018;65:81–85. doi: 10.1016/j.gaitpost.2018.06.175. [DOI] [PubMed] [Google Scholar]
- 11.Tudor-Locke C, Aguiar EJ, Han H, et al. Walking cadence (steps/min) and intensity in 21–40 year olds: CADENCE-adults. Int J Behav Nutr Phys Act. 2019;16(1):8. doi: 10.1186/s12966-019-0769-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tudor-Locke C, Han H, Aguiar EJ, et al. How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review. Br J Sports Med. 2018;52(12):776–788. doi: 10.1136/bjsports-2017-097628x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.White DK, Tudor-Locke C, Zhang Y, et al. Daily walking and the risk of incident functional limitation in knee osteoarthritis: an observational study. Arthritis Care Res (Hoboken) 2014;66(9):1328–1336. doi: 10.1002/acr.22362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pfeiffer S, Harkey MS, Stanley LE, et al. Associations between slower walking speed and T1p magnetic resonance imaging of femoral cartilage following anterior cruciate ligament reconstruction. Arthritis Care Res (Hoboken) 2018;70(8):1132–1140. doi: 10.1002/acr.23477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dall PM, McCrorie PR, Granat MH, Stansfield BW. Step accumulation per minute epoch is not the same as cadence for free-living adults. Med Sci Sports Exerc. 2013;45(10):1995–2001. doi: 10.1249/MSS.0b013e3182955780. [DOI] [PubMed] [Google Scholar]
- 16.Bodkin SG, Werner BC, Slater LV, Hart JM. Post-traumatic osteoarthritis diagnosed within 5 years following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):790–796. doi: 10.1007/s00167-019-05461-y. [DOI] [PubMed] [Google Scholar]
- 17.Rossi MJ, Lubowitz JH, Guttmann D. Development and validation of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2002;30(1):152. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 18.Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–897. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 19.Montoye AHK, Nelson MB, Bock JM, et al. Raw and count data comparability of hip-worn ActiGraph GT3X+ and Link accelerometers. Med Sci Sports Exerc. 2018;50(5):1103–1112. doi: 10.1249/MSS.0000000000001534. [DOI] [PubMed] [Google Scholar]
- 20.Chomistek AK, Yuan C, Matthews CE, et al. Physical activity assessment with the ActiGraph GT3X and doubly labeled water. Med Sci Sports Exerc. 2017;49(9):1935–1944. doi: 10.1249/MSS.0000000000001299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Montoye AHK, Moore RW, Bowles HR, Korycinski R, Pfeiffer KA. Reporting accelerometer methods in physical activity intervention studies: a systematic review and recommendations for authors. Br J Sports Med. 2018;52(23):1507–1516. doi: 10.1136/bjsports-2015-095947. [DOI] [PubMed] [Google Scholar]
- 22.Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47(9):1821–1845. doi: 10.1007/s40279-017-0716-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43(2):357–364. doi: 10.1249/MSS.0b013e3181ed61a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rowe DA, Welk GJ, Heil DP, et al. Stride rate recommendations for moderate-intensity walking. Med Sci Sports Exerc. 2011;43(2):312–318. doi: 10.1249/MSS.0b013e3181e9d99a. [DOI] [PubMed] [Google Scholar]
- 25.Cohen J, Cohen P, West SG, Aiken LS. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences 3rd ed. Mahwah, NJ: Lawrence Erlbaum;; 2003. p. 703. [Google Scholar]
- 26.Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–2028. doi: 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuenze C, Lisee C, Pfeiffer KA, et al. Sex differences in physical activity engagement after ACL reconstruction. Phys Ther Sport. 2019;35:12–17. doi: 10.1016/j.ptsp.2018.10.016. [DOI] [PubMed] [Google Scholar]
- 28.Baez SE, Hoch MC, Hoch JM. Psychological factors are associated with return to pre-injury levels of sport and physical activity after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):495–501. doi: 10.1007/s00167-019-05696-9. [DOI] [PubMed] [Google Scholar]
- 29.Perry DC, Moore CC, Sands CJ, et al. Using music-based cadence entrainment to manipulate walking intensity. J Phys Act Health. 2019] doi: 10.1123/jpah.2019-0097. [published online September 10. [DOI] [PubMed]
- 30.Marshall SJ, Nicaise V, Ji M, et al. Using step cadence goals to increase moderate-to-vigorous-intensity physical activity. Med Sci Sports Exerc. 2013;45(3):592–602. doi: 10.1249/MSS.0b013e318277a586. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


