Abstract
Introduction:
Novel coronavirus disease 2019 (COVID 19) has usurped human peace and mobility. The confinement of the population and the rising epidemic has disrupted the routine care for non-COVID-19 patients. Telehealth is a growing field, and its application in palliative care is seen as a solution to serve the population in this difficult crisis.
Methodology:
A exploratory survey was designed to assess the changes in the hospital-based practice of palliative care in the COVID-19 pandemic and patient/caregiver's perception about the provision of telehealth services to palliative care patients of a tertiary care cancer hospital of eastern India.
Results:
There was a dramatic reduction in the outpatient clinic footfalls by 51% with teleconsultation. Although there was no change in the number of emergency visits, the inpatient admissions reduced by 44%. Nearly 82% of patient/caregivers gave a positive feedback about telemedicine care provided by the department and mentioned that the service provided them with support and connectedness. Almost 64% of the patients and caregivers reported that the service helped allay the fear and reassured them that there was a someone to support them. As high as 76% of the participants felt that they would prefer teleconsultation in future and were ready to pay for teleconsultations if charges were to be applied in the future.
Conclusion:
Telemedicine is an important tool and an essential service to care for palliative care patients in the community especially when the patient and health-care professionals are separated by a pandemic or natural disaster.
Keywords: Coronavirus disease 2019, palliative care, patient/caregiver's perspective, telemedicine
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic has and continues to pose an insurmountable challenge creating critical uncertainties in the delivery of health-care services across all segments. Cancer patients are at an increased risk of COVID-19 infection and carry a poorer prognosis than individuals without cancer owing to their systemic immunosuppressive state due to malignancy and anticancer treatments.[1] With the emergence of COVID-19 pandemic, an urgent necessity has propelled telemedicine as a critical essential service for cancer patients to help reduce the transmission of COVID-19 infection. Telemedicine is a proven modality to deliver palliative care to the most vulnerable population with serious illness and their families especially in the current pandemic situation necessitating social distancing and confinement as a protective mechanism for patient, families and health-care staff.[2]
In previous studies and scenarios involving palliative care patients, telemedicine has demonstrated to be a promising technology, reducing the need for urgent emergency room visits, providing improved continuity of care, reduced costs, and improved patient satisfaction in home-bound patients.[3] Telemedicine by providing access to remote areas has the power to overcome geographical barriers to provide health-care services in the present scenario of nationwide lockdown. The Government of India as an urgent response to the growing pandemic implemented rapid measures such as nationwide lockdown in a pretext to curb the situation. The confinement of population and the rising pandemic has led to the disruption of routine care of non-COVID-19 patients, demanding the rise of outreach measures to maintain continuity of health-care services. One such initiative implemented by the Government of India was the release of telemedicine guidelines prepared by the board of governors in partnership with the NITI Aayog on March 25, 2020. The purpose of these guidelines is to give practical advice to doctors so that all services and models of care used by doctors and health workers are encouraged to consider the use of telemedicine as a part of normal practice.[4]
However, there are always some practical challenges associated with telemedicine due to its virtual nature and lack of interpersonal interaction between doctor and patients. These challenges may also be further influenced by cultural, social, and regional factors. With this background, exploratory survey was designed to assess the changes in the hospital-based practice of palliative care in the COVID-19 pandemic and patient/caregiver's perception about the provision of telehealth services to palliative care patients of a tertiary care cancer hospital of eastern India.
METHODOLOGY
Teleconsultation service was started by the Department of Palliative care in 2014 with the intention of providing continuity of service to patients/caregivers attending the hospital for symptom control. Since January 2014, 10,856 teleconsultations have been provided to 7629 unique patients using a triage system [Figure 1]. This exploratory survey was conducted to assess the impact of our on-going telehealth services in challenging times faced during the current COVID pandemic.
Figure 1.
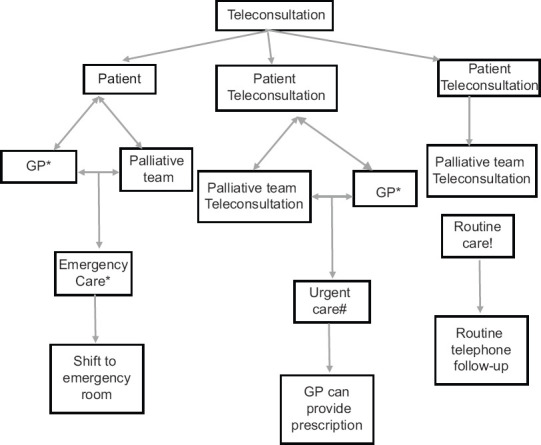
Triaging patients using teleconsultation. *Intractable pain or other symptoms such as breathlessness, bleeding etc., that endangers quality of life or increases the risk of death/status epilepticus, agitated delirium/risk of suicide. #Moderate symptoms/developed new symptoms warranting physical examination by physician/need a change of prescription such as benzodiazepines, antipsychotics or narcotics. !Mild symptoms/need dose titration of the existing prescription/on a scheduled follow-up
Fifty subjects were interviewed using a semi-structured interview guide to query diverse perspectives to inform acceptance and challenges of telemedicine services in the face of the COVID-19 pandemic crisis. Participants included advanced cancer patients registered with the Department of Palliative Care at Tata Medical Center and who consented to participate in the survey. The study participants were then selected from the master list of all patients with valid mobile numbers registered for outpatient department (OPD) consultation for the period January 1, 2020 – May 19, 2020.
Data were collected by a structured interview with both close-ended questions with binary answers (yes/no) or 3-point scales (very satisfied/satisfied/not satisfied).
Data collection and data quality
A predesigned and pretested structured questionnaire was used for telephonic data collection.
The data collection was done by a social worker under the active supervision of study investigators and subsequently, random review of the collected data as well as active observation of the interview process was done to ensure data correctness and quality.
Data analysis and review
The collected quantitative secondary data from review of electronic medical records as well as primary data collected through telephonic interview were cleaned and imported into standard excel sheets for ease of data analysis.
The aggregated data were analyzed using standard descriptive statistics and represented as frequencies and percentages.
RESULTS
Of the fifty subjects interviewed telephonically, 54% (n = 27) belonged to the age group of 18–60 years. 56% (n = 28) of the patients were males, while 44% (n = 22) were females [Table 1].
Table 1.
Patient demographics
| Patient characteristics | Number of patients (%) |
|---|---|
| Age (years) | |
| <18 | 1 (2) |
| 19-60 | 27 (54) |
| >60 | 22 (44) |
| Sex | |
| Male | 28 (56) |
| Female | 22 (44) |
The survey estimated an average footfall in the outpatient clinic during the COVID pandemic reduced by 51%. There was an average reduction of 55.22% in the number of inpatient admissions for symptom control and end-of-life care. However, the number of patients attending the hospital for emergency needs continued to be the same as during the non-COVID period [Table 2].
Table 2.
Footfall in outpatient departments/inpatient departments/emergency service
| Time period | Average outpatient per month | Average In-patient admissions per month | Average emergency room visits per month |
|---|---|---|---|
| Average patients during non-COVID period | 280 | 134 | 106 |
| Average patients per month during COVID period (from March 21 till date) | 142 | 60 | 104 |
COVID: Coronavirus disease 2019
Our survey was mainly conceptualized to gather patients and their primary care-givers experiences and perception regarding acceptance of telehealth services as a modality to meet their unmet health needs during the COVID pandemic. Majority of the participants, 64% (n = 32), scored their comfort levels as being “comfortable” using telehealth services offered. With regard to discussing their holistic health issues with the palliative care team, 54% (n = 27) rated the conversations “satisfying” [Table 3].
Table 3.
Participants perceptions and experiences
| Very satisfied, n (%) | Satisfied, n (%) | Dissatisfied, n (%) | |
|---|---|---|---|
| Conversation with palliative care team | 14 (28) | 27 (54) | 9 (18) |
| Time provided during consultation | 0 | 41 (82) | 9 (18) |
| Clarity of advice given | 0 | 41 (82) | 9 (18) |
| Courtesy and politeness | 21 (42) | 29 (58) | 0 |
| Helped reduce anxiety; a feeling that there is someone for support | 32 (64) | 18 (32) | 0 |
Eighty-two percent (n = 41) of the respondents were “satisfied” with regard to the time provided and clarity of advice given by the palliative care team. With reference to courtesy and politeness of the telehealth provider, 58% (n = 29) rated the experience as “satisfied.” Nearly 64% (n = 32) felt very satisfied with the advice provided and felt reassured of continued support by the team [Table 3].
Of the fifty participants interviewed, 76% (n = 38) expressed their willingness to pay for telehealth service if implemented in the future.
During the lockdown period, the patients/caregivers incurred higher cost towards travel to the hospital. 42.85% patients had to pay INR 500–1000 above the normal cost of travel during normal days and 28.57% patients spent INR 1000 above the normal cost.
DISCUSSION
The rising numbers in COVID-19 cases across the globe has disrupted the routine care of non-COVID-19 patients. The government has laid down formal guidelines for implementing telemedicine service[4] in order to restrict patients from seeking physical consultation. Therapies involving telemedicine are known to provide beneficial effects in patients with chronic pain.[5] A Cochrane systematic review of technological interventions for chronic pain in adults demonstrated a small-to-moderate reduction in pain, disability, and distress associated with symptoms in the tele-consultation groups as compared to patients who received standard care.[6,7] A study by Martorella et al. found no difference in the treatment effect between teleconsultation and face-to-face therapies.[7] There are conflicting evidences with regard to symptom reduction with teleconsultations. One randomized controlled trial comparing weekly teleconsultation with “case as usual” reported higher symptom burden in the teleconsultation group. Improving symptom burden in patients with advanced cancer can be complex. One more reason for reporting higher symptom burden could be attributed to higher awareness of symptoms, thus leading to worsening symptom experience or their symptoms may have been more precisely registered by the team.[8]
The teleconsultation reduced the OPD footfalls for our department dramatically by 51%. Contrary to our belief, implementation of restricted outpatient service did not impact the emergency visits although the inpatient admissions reduced by 55.22%. Many patients with poor general condition who presented for the first time to the hospital were referred to palliative care by the primary oncology team, which could justify the emergency numbers. Studies that have examined the use of telephone advice lines have reported a reduction in the number of inpatient admissions. Middleton-Green et al.[9] stated that 98.5% of calls resulted in patients remaining in their place of residence and only 13% patients expired in the hospital. Therein the challenges of lockdown and restricted physical consultations can be surmounted through a systematic approach using telemedicine where specialist palliative care team can liaise with general practitioners in the community [Figure 1]. It also supports the patient's choice of living at home for as long as possible, which is important for many patients.[10] Although, limited by physical examination, teleconsultation can improve the screening of patients in need of a clinical visit by way of triaging [Figure 1], prevents futile visits to the hospital and restricts only to necessary physical consultation or emergency service, reassures the patient/caregivers of continued support from the palliative care team, decreases the monetary burden on patients/caregivers as it saves the cost of travel, and reduces the waiting time of patients.[11]
It is essential to note here that the advice provided by the specialist team can bring a dramatic reduction in hospital admissions.[12,13] Although our data showed a reduction in the inpatient admission which was contradictory to the findings in a study by Lewis et al., the study failed to demonstrate any difference in hospital admissions, or emergency department visits which could be attributed to severity of the symptoms and the degree of medical and nursing support the patients have in the community.[14]
The telehealth service provided by our department was proactive where most calls were made during office hours by the team and <10% calls occurred out-of-office hours. Out-of-office hours calls were initiated by family members. Forty-one out of 50 (82%) of participants gave a positive feedback about telemedicine care and mentioned that the service provided them with support and connectedness. The politeness, the time given, and cordiality of the caller gave them a feeling that someone cared about their concerns. A study by Stern et al. showed similar results where the author claims that a proactive teleconsultation by the team can reassure the family and help reduce out of hours contact by patients whose condition is deteriorating.[15]
The cost of travel to the hospital more than doubled in this pandemic period. Most vehicle plying during this period belonged to private companies who hiked their charges exorbitantly. Patients who visited the palliative care team during this period had a scheduled appointment with the primary oncology team, had a scheduled chemotherapy, or needed a fresh prescription for opioids (caregivers travelled).
Although the mobile cellular subscription has increased in the recent years, only 34.45% of the Indian population has access to internet server.[16] Teleconsultations are impersonal as this reduces direct patient–doctor interaction, lacks physical examination which may result in incomplete diagnosis and is devoid of caring touch which palliative care patients would appreciate.[10] There could be concerns related to the quality of health information exchanged and confidentiality of information shared by the patient.
Thirty-eight out of the fifty (76%) participants were ready to pay for teleconsultations if charges were to be applied in future. It is important that charges levied be minimal especially for elderly population and people with lower income in order to encourage more people to avail the service.[17,18] Some studies suggested that minimal cost and cheaper options could be used for larger population to benefit as even bidirectional function via SMS could be impeded due to the charges levied.[18] Some participants felt the need for 24 h telephone support service in this lockdown period as they faced challenge in accessing general practitioner for out-of-hours support. They felt that such service would help allay the anxiety by providing guidance on a timely manner, thus constantly reassuring them of a continued support.[19,20] There are some limitations that need to be acknowledged. The number of study participants was small and the recruitment was from a single palliative care center. Therefore, further studies with larger sample size are required to confirm the effects of telemedical care.
CONCLUSION
Telemedicine is an emerging technology especially in the field of palliative medicine. Majority of the patients/caregivers in this study felt that telemedicine was advantageous as an alternative tool for physical consultation. The benefits included increased access to care, reduced discomfort, reduced travel time, and reduced risk of health-care-associated infections. Routine clinical practice is ridden with challenges but future studies will need to explore some of the main challenges such as influence of socioeconomic status, sound technology, funding, and health insurance to cover the cost of the service if high end technology were to be implemented and technical support and data security.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kamboj M, Sepkowitz KA. Nosocomial infections in patients with cancer. Lancet Oncol. 2009;10:589–97. doi: 10.1016/S1470-2045(09)70069-5. [DOI] [PubMed] [Google Scholar]
- 2.Calton B, Abedini N, Fratkin M. Telemedicine in the Time of Coronavirus [published online ahead of print, 2020 Mar 31] J Pain Symptom Manage. 2020 doi: 10.1016/j.jpainsymman.2020.03.019. S0885-3924(20)30170-6 doi:101016/jjpainsymman202003019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kidd L, Cayless S, Johnston B, Wengstrom Y. Telehealth in palliative care in the UK: A review of the evidence. J Telemed Telecare. 2010;16:394–402. doi: 10.1258/jtt.2010.091108. [DOI] [PubMed] [Google Scholar]
- 4. [Lst accessed 2020 Mar 25]. Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf .
- 5.Fisher E, Law E, Dudeney J, Eccleston C, Palermo TM. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2019;4:CD011118. doi: 10.1002/14651858.CD011118.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buhrman M, Gordh T, Andersson G. Internet interventions for chronic pain including headache: A systematic review. Internet Interv. 2016;4:17–34. doi: 10.1016/j.invent.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martorella G, Boitor M, Berube M, Fredericks S, Le May S, Gélinas C. Tailored web-based interventions for pain: Systematic review and meta-analysis. J Med Internet Res. 2017;19:e385. doi: 10.2196/jmir.8826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoek PD, Schers HJ, Bronkhorst EM, Vissers KC, Hasselaar JG. The effect of weekly specialist palliative care teleconsultations in patients with advanced cancer-A randomized clinical trial. BMC Med. 2017;15:119. doi: 10.1186/s12916-017-0866-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Middleton-Green L, Gadoud A, Norris B, Sargeant A, Nair S, Wilson L, et al. A friend in the corner': supporting people at home in the last year of life via telephone and video consultation-an evaluation. BMJ Support Palliat Care. 2019;9:e26. doi: 10.1136/bmjspcare-2015-001016. [DOI] [PubMed] [Google Scholar]
- 10.Sandsdalen T, Hov R, Høye S, Rystedt I, Wilde-Larsson B. Patients' preferences in palliative care: A systematic mixed studies review. Palliat Med. 2015;29:399–419. doi: 10.1177/0269216314557882. [DOI] [PubMed] [Google Scholar]
- 11.Coyle N, Khojainova N, Francavilla JM, Gonzales GR. Audio-visual communication and its use in palliative care. J Pain Symptom Manage. 2002;23:171–5. doi: 10.1016/s0885-3924(01)00402-x. [DOI] [PubMed] [Google Scholar]
- 12.Plummer S, Allan R. Analysis of a network-wide specialist palliative care out-of-hours advice and support line: A model for the future. Int J Palliat Nurs. 2011;17:494–9. doi: 10.12968/ijpn.2011.17.10.494. [DOI] [PubMed] [Google Scholar]
- 13.Purdy S, Lasseter G, Griffin T, Wye L. Impact of the Marie curie cancer care delivering choice programme in somerset and north somerset on place of death and hospital usage: A retrospective cohort study. BMJ Support Palliat Care. 2015;5:34–9. doi: 10.1136/bmjspcare-2013-000645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewis KE, Annandale JE, Warm DL, Rees SE, Hurlin C, Blyth H, Syed Y, Lewis L. Does home Telemonitoring after pulmonary rehabilitation reduce healthcare use in optimized COPD A pilot randomized trial COPD. J Chron Obstruct Pulmon Dis. 2010;7:44–50. doi: 10.3109/15412550903499555. [DOI] [PubMed] [Google Scholar]
- 15.Stern A, Valaitis R, Weir R, Jadad AR. Use of home telehealth in palliative cancer care: A case study. J Telemed Telecare. 2012;18:297–300. doi: 10.1258/jtt.2012.111201. [DOI] [PubMed] [Google Scholar]
- 16. [Last accessed on 2020 Jun 08]. Available from: https://data.worldbank.org/indicator/IT.NET.USER.ZS?locations=IN&most_recent_value_desc=true .
- 17.Akinfaderin-Agarau F, Chirtau M, Ekponimo S, Power S. Opportunities and limitations for using new media and mobile phones to expand access to sexual and reproductive health information and services for adolescent girls and young women in six Nigerian states. Afr J Reprod Health. 2012;16:219–30. [PubMed] [Google Scholar]
- 18.Rana Y, Haberer J, Huang H, Kambugu A, Mukasa B, Thirumurthy H, et al. Short message service (SMS)-based intervention to improve treatment adherence among HIV-positive youth in Uganda: Focus group findings. PLoS One. 2015;10:e0125187. doi: 10.1371/journal.pone.0125187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gorst SL, Armitage CJ, Brownsell S, Hawley MS. Home telehealth uptake and continued use among heart failure and chronic obstructive pulmonary disease patients: A systematic review. Ann Behav Med. 2014;48:323–36. doi: 10.1007/s12160-014-9607-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Young JD, Borgetti SA, Clapham PJ. Telehealth: Exploring the ethical issues. DePaul J Health Care L. 2018;19:1–15. [Google Scholar]


