Abstract
Background and Aims:
With the COVID-19 pandemic, lockdown, and fear from contagion, the advantages of telemedicine are clearly outweighing the setbacks by minimizing the need for individuals to visit health-care facilities. Our study aims to assess how palliative medicine physicians could follow up on cancer patients and barriers they faced, discuss their results, and evaluate their treatment response with the help of telemedicine.
Materials and Methods:
We conducted a prospective analysis of the smartphone-based telemedicine service at our palliative care (PC) unit from March 25, 2020, to May 13, 2020. We recorded the patient's reason for call, main barriers to a hospital visit, and the assistance given to them by the physician on call. Each caller was asked to measure his/her satisfaction with the service on a 4-point scale.
Results:
Out of 314 patients, 143 (45.54%) belonged to Delhi and 171 (54.46%) belonged to other states. 157 patients sought help for symptom management; 86 patients needed to restock their opioid medications. Seventy-one patients required information regarding their oncological treatments requiring consultation from other departments. Titration of oral opioids and medication prescription (n = 129), contact details of other PC units at their native state for opioid procurement (n = 55), and attachment to our community-based PC service (n = 22) were main modes of management. Fifty-six patients were very satisfied and 152 patients were satisfied with the service.
Conclusion:
Telemedicine is the future of health-care delivery systems. In PC, we deal with immunocompromised debilitated cancer patients and telemedicine is immensely helpful for us to provide holistic integrated care to these patients who are unable to visit hospitals regularly.
Keywords: COVID-19, palliative care, telemedicine
INTRODUCTION
Telemedicine is an old yet poorly adopted concept in oncology care.[1] In the era of novel coronavirus (COVID-19) pandemic, the telemedicine has regained the popularity.[2,3] The outbreak of COVID-19 has already been declared as a global pandemic by the World Health Organization on March 11, 2020.[4] To ensure effective social distancing as an infection control strategy, many nations have declared lockdown. India is also in a lockdown mode since March 24.[5] Access to standard health care has become more difficult with the strict imposition of laws and restriction of mobility. Moreover, due to the consumption of palliative care (PC) resources for acute care of infected patients,[6] providing a continuous quality PC service in advanced cancer patients has become a real challenge.
Telemedicine has emerged as a solution to these problems in various specialties involved in cancer care, including PC.[7,8,9] Newer technologies, e.g., smartphone-based applications and video calls, have made the service more dynamic.[10,11] It enables the PC physicians to assess the symptoms and provide psychological support to the patients and caregivers. It also serves as an effective triaging system during the pandemic to choose priority patients for home visits and screening of symptoms suggestive of COVID infection.[12]
These potential benefits can make telemedicine the future of health-care services, even after the lockdown period. Therefore, we have set up a 24 × 7 smartphone-based telemedicine service for cancer patients in the department of palliative medicine. Here, we share our initial experience of 50 days of such service. It gives an insight into the different characteristics of patients, their needs, barriers to access regular services, and level of satisfaction with such services. This helps identify the problem areas of the telemedicine setup and gives an idea to improve it for long-term use.
MATERIALS AND METHODS
We conducted a prospective analysis of the telemedicine service at the PC unit, in the Department of Onco-Anaesthesia and Palliative Medicine, Dr. B.R. AIRCH, AIIMS, New Delhi, from March 25, 2020, to May 13, 2020. Our department has an only phone call-based telemedicine service already in place for the consultation of our follow-up patients. However, in response to the current pandemic and anticipating more vigorous need of telemedicine service, we changed this to a smartphone-based 24 × 7 model. We transferred our previous subscriber identity module card for telemedicine service to an android smartphone with 4G internet connectivity. We used phone calls, text messages, and smartphone-based applications, e.g., WhatsApp Messenger and Skype for audiovisual consultation. We updated our telemedicine contact details in the main hospital website and teleconsultation web portal. A PC senior resident, trained for PC in cancer patients at our department, was posted for 24 × 7 for the service under the supervision of a faculty. We referred to electronic records of our department for details of individual patients, whenever needed during or after the consultation. The PC physicians managed the symptoms at their discretion. We do maintain an online record of the centers giving PC services to cancer patients in different states all over India. We provided the patients the contact numbers of those centers to procure opioids if they cannot come to our hospital. A multidisciplinary assistance was provided to the patients by providing the contact details of telemedicine service of the other specialties, if needed. We noted down the patient's reason for the call, main barriers to a hospital visit, and the assistance given to them by the physician on call. Each caller was called back within 24 h by a second person, who was not related to the previous call made to him. A separate call with an independent person was made to assess the satisfaction level to eliminate intimidation bias. Each caller was asked to measure his/her satisfaction with the service on a 4-point scale: very satisfied (4), satisfied (3), partially satisfied (2), and unsatisfied (1).
RESULTS
We analyzed the telemedicine records of a total of 314 patients over 50 days (March 25, 2020, to May 13, 2020). Among the patients who availed our teleconsultation service, 143 (45.54%) belonged to the State of Delhi and 171 (54.46%) belonged to other states. Maximum patients (123; 39.17%) were having curative therapy and 103 (32.8%) patients were under the best supportive care only. Among 314 patients, 224 (71.34%) patients were taking opioids under our follow-up. The details of the characteristics of the patients are described in Table 1.
Table 1.
Characteristics of patients who availed the telemedicine service
| Number of patients (total=314) | |
|---|---|
| Age (years) (mean±SD) | 45.39±15.63 |
| Sex (male:female) | 148:166 |
| Residence | |
| Delhi | 143 |
| Other states | 171 |
| Diagnosis | |
| Lung cancer | 36 |
| GI cancer | 38 |
| Hepatobiliary carcinoma | 37 |
| Gynecological carcinoma | 31 |
| Head and neck cancers | 42 |
| Bone and soft tissue sarcoma | 41 |
| Breast carcinoma | 33 |
| Urological carcinoma | 21 |
| Hematological | 21 |
| Others | 14 |
| Time since diagnosis | |
| <6 months | 147 |
| 6 months-1 year | 101 |
| >1 year | 66 |
| Disease status | |
| Under evaluation | 88 |
| Under active therapy | 123 |
| Best supportive care | 103 |
| Patients previously on opioids? | |
| Yes | 224 |
| No | 90 |
GI: Gastrointestinal, SD: Standard deviation
The majority of the patients availed telephone calls and text messages (n = 167, 53.18%), whereas video consultations were required for 84 (26.75%) patients. The peak frequency of calls was between 10 A.M. to 2 P.M. (37.58%) and least (4.14%) at night (10 P.M. to 6 A.M.), and the majority of them had a duration of 10–15 min (39.49%). The details of the consultations are discussed in Table 2. Among 314 patients, 157 (50%) patients sought help for symptom management; 86 patients (27.39%) needed to restock their opioid medications. Seventy-one (22.61%) patients called up for information regarding their oncological treatments from other departments involved in cancer care. The major barrier, as perceived by the caller, to avail the hospital services for their patient was restriction of movement across the state borders and lack of transport availability (in 124 patients), terminal patients (in 88 patients), and fear of getting infected (in 71 patients). We provided prescriptions through text messages for titration of oral opioids and medications for other symptoms in a total of 129 (41.08%) patients. 55 (17.52%) patients, who were from other states and needed to restock their opioids, were given contact details of other government hospitals with PC units at their native state. 22 (7%) patients, who were from Delhi, were given contact details of our community-based PC service team for home visits for symptom management. All the patients with complaints of dyspnea (36; 11.46%) were assessed via video calls. Among them, 22 patients from other states were advised to visit the nearby hospitals for the evaluation and drainage of ascitic or pleural fluid.
Table 2.
Details of the teleconsultations
| Characteristics of the calls | Number of patients |
|---|---|
| Number of calls | Number of patients (total=314) |
| Audio calls only | 63 |
| Audio + text | 167 |
| Audio + text+ visual | 84 |
| Timing of calls | Number of patients (total=314) |
| 6 A.M-10 A.M | 48 |
| 10 A.M-2 P.M | 118 |
| 2 P.M-6 P.M | 99 |
| 6 P.M-10 P.M | 36 |
| 10 P.M-6 A.M | 13 |
| Total duration of calls (min) | Number of patients (total=314) |
| <5 min | 71 |
| 5-10 min | 62 |
| 10-15 min | 124 |
| >15 min | 57 |
| Reason of call | Number of patients (total=314) |
| Symptom management | 157 |
| Pain | 98 |
| Dyspnea | 36 |
| Nausea and vomiting | 8 |
| Constipation | 10 |
| Others | 5 |
| Queries regarding oncological treatment from other departments | 71 |
| Restocking of opioids | 86 |
| Severity of symptoms | Number of patients (total=157) |
| <4/10 | 32 |
| 4-6/10 | 97 |
| >7/10 | 28 |
| Major barrier to avail the hospital service | Number of patients (total=314) |
| Sealing of borders | 124 |
| Patient is terminal | 88 |
| No social support to accompany | 31 |
| Afraid to come to hospital for fear of infection | 71 |
| What was advised at the end? | Number of patients (total=314) |
| Prescribed for oral titration of opioids | 109 |
| Prescribed oral medications for symptom management | 20 |
| Referred to the emergency of a nearby hospital in the locality for symptom management | 22 |
| Home visit by community based palliative care team with contact details suggested | 22 |
| Information of an alternative palliative care unit at the native state with contact details shared to procure opioids | 55 |
| Scheduled for our OPD visit for procurement of opioids | 12 |
| Contact details of other departments given | 71 |
| Monitored end of life care | 3 |
OPD: Outdoor patient department
The rests of the patients (14) were managed with titration of opioids and anxiolytics. Three patients with terminal dyspnea were monitored and provided with end of life care over video consultation. In those patients, oral opioid dose was escalated and the caregivers were reassured about the dignity of death. All the three patients died under our monitored supervision.
We also assessed the satisfaction level of our patients for the telemedicine service [Figure 1]. 56 patients were very satisfied and 152 patients were satisfied with the service. However, 59 patients remained partially satisfied and 47 patients were unsatisfied. The reasons for this were majorly unavailability of multidisciplinary advises over a single call (64 patients). The rest of the 42 patients believed that face-to-face consultations may be more useful for them.
Figure 1.
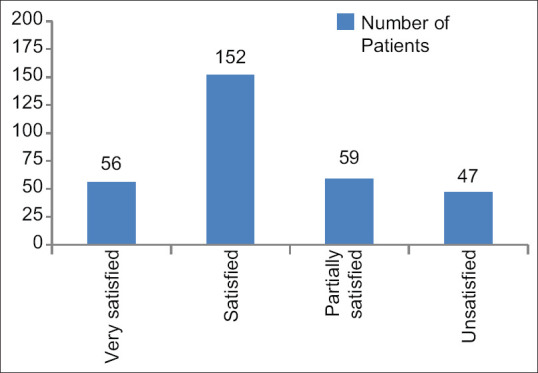
Satisfaction level of patients for telemedicine services using 4-point scale
DISCUSSION
Cancer care delivery is facing several challenges due to the COVID-19 pandemic. Telemedicine is a solution to many of the barriers faced by PC physicians when caring for cancer patients without increasing undue risk of infection. This study was developed to assess the efficacy of our new smartphone-based teleconsultation model for PC patients and to identify the needs of the patients and major problem areas for future improvement. We have provided consultations to 314 cancer patients (average daily 6.28 patients) during nationwide lockdown over 50 days.
Smartphone-based teleconsultation models have several advantages. Pak et al.[13] (2018) identified that patients and caregivers have easy access to smartphones and their applications. They also found that it is quite accurate for the assessment of physical symptoms of the patients as compared to the on-site assessment by a physician. All our 314 patients had access to the smartphones with adequate capacity to handle the common messenger applications. The major limitation of the use of these mobile-based applications is the safety of the patient's data. We suggest that the data can be transferred to another protected hospital-based record system and later can be deleted from the mobile device (store-forward-delete system).
In our study, we found that pain and dyspnea are the common symptoms, for which patients availed telemedicine service. Lesley (2020) et al.[14] have also described pain, dyspnea, nausea vomiting, and fatigue as the most common symptoms in advanced cancer patients requiring PC. Another major reason for the call was the stocking of opioid medications. In India, the Narcotic Drugs and Psychotropic Substances Act has already been identified as the major barrier to the availability of opioids.[15] Due to strict impositions of rules and punishments, it is extremely important to dispense opioids from only registered centers with appropriate forms. We tried to overcome this barrier by providing the patients with information regarding an alternative center for opioids nearby to their residence. One important aspect was the disproportionately less number of patients who called for opioid restocking. Although 224 (71.33%) patients were on opioids previously, only 86 (27.38%) patients were having the problem of restocking of them. There may be two reasons for it. First, we started dispensing opioids for at least 1 month for all patients with proper documentation since early March to decrease the frequency of hospital visits by the patients as a part of our infection control strategy. Second, we kept our outdoor service with limited capacity for opioid dispensing. As some of the patients who belong to Delhi availed for this service, they had adequate opioids for the period of lockdown.
The involvement of different specialties for cancer care is important for the holistic care of cancer patients. Hui et al.[16] (2018) explained the importance of such an approach to deliver complex care to cancer patients. Janssen et al.[17] (2017) highlighted the fact that communications and coordination between teams are important for an effective multidisciplinary approach. In our study, 71 (22.61%) patients were also in need of consultations from other departments, e.g., medical oncology, radiation oncology, and radiation oncology. They needed the information regarding the schedule of chemotherapy, radiotherapy, and surgery, information regarding oral chemotherapy-related drugs, and complications due to recent chemotherapy. Although we provided the contact number of the concerned departments, we were unable to trace back those patients whether their requirements were fulfilled or not. Moreover, they needed to make multiple calls, which was not very convenient. Thus, we suggest that a real-time video conferencing call involving physicians from multiple specialties, family members, and patient can improve the quality of our service.
Patient satisfaction is the key to assess the efficacy of any service. Although our majority of the patients were satisfied with the service, 106 patients were either partially satisfied or unsatisfied. This indicates a scope of improvement of our services. The major problem area identified was the lack of a multidisciplinary approach to the service. This was also the most common cause (64 out of 106) of lack of satisfaction among patients. This suggests that we need to develop a system for a real-time integrated system for teleconsultations involving other departments.
Our assessment had some limitations too. We were unable to assess the psychological aspects of the patients and caregivers. We could not follow up on our patients who were advised for another PC unit visit, emergency department of nearby hospitals for symptom management, or provided with the contact details of other departments. Following up such patients in the future can improve the outcome and efficacy of our service. Although all our patients had an access to smartphone services, it is important to assess the feasibility of its use in larger patient population. A large well-planned study involving patients from different backgrounds and areas of country should be conducted to assess the access of smartphone-based technologies and expertise of patients for it. Finally, we also could not assess the physician's perception of the service and problems faced by them. Future assessment of physician-reported outcomes can also help improve the service.
CONCLUSION
COVID-19 pandemic may get over it sometime, but it will change our practices for the long term. Telemedicine is going to be the future of health-care delivery systems. In PC, we deal with immunocompromised debilitated cancer patients who are at risk of infection. Hence, telemedicine is going to be helpful for us to provide holistic PC to these patients. In our study, we have found that it is feasible to assist the patients to manage their symptoms by providing real-time assessment using smartphone-based applications. Setting up a multidiscipline setup for telemedicine may improve the service and patient satisfaction significantly. In further evaluation, we also should include the psychological aspects of patients and caregivers for improving our holistic care to cancer patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Doolittle GC, Spaulding AO. Providing access to oncology care for rural patients via telemedicine. J Oncol Pract. 2006;2:228–30. doi: 10.1200/jop.2006.2.5.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith WR, Atala AJ, Terlecki RP, Kelly EE, Matthews CA. Implementation Guide for Rapid Integration of an Outpatient Telemedicine Program During the COVID-19 Pandemic [published online ahead of print, 2020 Apr 30] J Am Coll Surg. 2020 doi: 10.1016/j.jamcollsurg.2020.04.030. S1072-7515(20)30375-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elkaddoum R, Haddad FG, Eid R, Kourie HR. Telemedicine for cancer patients during COVID-19 pandemic: Between threats and opportunities? Future Oncol. 2020;16:1225–7. doi: 10.2217/fon-2020-0324. doi:10.2217/fon-2020-0324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19; 11 March, 2020. [Last accessed on 2020 Apr 20]. Available from: https://wwwwhoint/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 .
- 5.Government of India issues Orders Prescribing Lockdown for Containment of COVID19 Epidemic in the Country. [Last accessed on 2020 Apr 20]. Available from: https://wwwmhagovin/sites/default/files/PR_NationalLockdown_26032020pdf .
- 6.Radbruch L, Knaul FM, de Lima L, de Joncheere C, Bhadelia A. The key role of palliative care in response to the COVID-19 tsunami of suffering. Lancet. 2020;395:1467–9. doi: 10.1016/S0140-6736(20)30964-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grimes CL, Balk EM, Crisp CC, Antosh DD, Murphy M, Halder GE, et al. A guide for urogynecologic patient care utilizing telemedicine during the COVID-19 pandemic: Review of existing evidence. Int Urogynecol J. 2020;31:1063–89. [Google Scholar]
- 8.Sell NM, Silver JK, Rando S, Draviam AC, Mina DS, Qadan M. Prehabilitation telemedicine in Neoadjuvant surgical oncology patients during the novel COVID-19 coronavirus pandemic. Ann Surg. 2020 May 01; doi: 10.1097/SLA.0000000000004002. Ahead of Print doi:101097/SLA0000000000004002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Worster B, Swartz K. Telemedicine and palliative care: An increasing role in supportive oncology. Curr Oncol Rep. 2017;19:37. doi: 10.1007/s11912-017-0600-y. [DOI] [PubMed] [Google Scholar]
- 10.Banbury A, Nancarrow S, Dart J, Gray L, Parkinson L. Telehealth Interventions Delivering Home-based Support Group Videoconferencing: Systematic Review. J Med Internet Res. 2018;20:e25. doi: 10.2196/jmir.8090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Allaert FA, Legrand L, Abdoul Carime N, Quantin C. Will applications on smartphones allow a generalization of telemedicine? BMC Med Inform Decis Mak. 2020;20:30. doi: 10.1186/s12911-020-1036-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Porzio G, Cortellini A, Bruera E, Verna L, Ravoni G, Peris F, et al. Home care for cancer patients during COVID-19 pandemic: The double triage protocol [published online ahead of print, 2020 Mar 31] J Pain Symptom Manage. 2020 doi: 10.1016/j.jpainsymman.2020.03.021. S0885-3924(20)30172-X doi:101016/jjpainsymman202003021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pak C, In Jeon J, Kim H, Kim J, Park S, Ahn KH, et al. A smartphone-based teleconsultation system for the management of chronic pressure injuries. Wound Rep Reg. 2018;26(Suppl 1):S19–26. doi: 10.1111/wrr.2. [DOI] [PubMed] [Google Scholar]
- 14.Henson LA, Maddocks M, Evans C, Davidson M, Hicks S, Higginson IJ. Palliative care and the management of common distressing symptoms in advanced cancer: Pain, breathlessness, nausea and vomiting, and fatigue. J Clin Oncol. 2020;38:905–14. doi: 10.1200/JCO.19.00470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rajagopal MR, Joranson DE. India: Opioid availability-an update. J Pain Symptom Manag. 2007;33:615–22. doi: 10.1016/j.jpainsymman.2007.02.028. [DOI] [PubMed] [Google Scholar]
- 16.Hui D, Hannon BL, Zimmermann C, Bruera E. Improving patient and caregiver outcomes in oncology: Team-based, timely, and targeted palliative care. CA Cancer J Clin. 2018;68:356–76. doi: 10.3322/caac.21490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janssen A, Brunner M, Keep M, Hines M, Nagarajan SV, Kielly-Carroll C, et al. Interdisciplinary eHealth practice in cancer care: A review of the literature. Int J Environ Res Public Health. 2017;14:1289. doi: 10.3390/ijerph14111289. [DOI] [PMC free article] [PubMed] [Google Scholar]


