Abstract
Objective:
To understand the trend of prevalence of symptoms of coronavirus disease 2019 (COVID-19) pandemic, some studies have been conducted outside India, but for Indian patients, there is no such study available. Therefore, this study was designed to analyze the trends of symptoms in Indian patients during COVID-19 pandemic.
Methods:
A retrospective study was conducted on 100 patients (73 males, 24 females, and 3 transgenders) admitted under institutional isolation at a tertiary care center in India using a self-designed survey-based questionnaire. A descriptive analysis of results done based on age and sex.
Results:
COVID incidence recorded is high in male (73%) as compared to female (24%), yet female patients have a higher prevalence of symptoms as compared to male patients.
Conclusion:
Male patients are more as far as COVID incidence is concerned, while female patients show high prevalence of symptoms as compared to male patients. Patients presenting with COVID-positive report suffer a significant burden of symptoms, and timely recognition of symptoms and their management can significantly reduce morbidity and mortality due to COVID-19.
Keywords: Coronavirus disease, symptom prevalence, India
INTRODUCTION
In late December 2019, a new public health crisis emerged as an outbreak of pneumonia-like respiratory infection from Wuhan, China. The World Health Organization (WHO) named this infection as severe acute respiratory syndrome coronavirus 2 (SARS CoV 2) and declared it as coronavirus disease 2019 (COVID 19). Within 2 months, by the end of February 2020, every nation across the globe reported cases of coronavirus infection. Rapid human-to-human transmission led COVID-19 to become a global medical emergency, and therefore, the WHO declared COVID-19 a pandemic on March 11, 2020.[1]
The first four cases of an acute respiratory syndrome of unknown etiology were reported in Wuhan, China, on December 29, 2019, in people associated with the wet market of seafoods. The virus was originated in bats and subsequently transmitted to human through some intermediary animals and considered to be a disease of animal-to-human transmission. Most of the early cases have sort of contact history with the seafood market in a way or another. Soon after this outbreak, the secondary source of infection was noted as human-to-human transmission.[2] Till April 16, 2020, nearly 2 million cases reported worldwide, of them, 131 thousand have lost their lives.[3] To understand trends and prevalence of symptoms of COVID-19, some studies have been conducted outside India, but for the Indian population, there is no such study available. Therefore, this study was designed to study trends of symptoms in Indian patients during the COVID-19 pandemic.
STUDY DESIGN AND METHODOLOGY
A retrospective study was conducted on 100 test-positive COVID-19 patients admitted under institutional isolation during March–April 2020 at a tertiary care center in India. Of 100 patients, 73 were male, 24 were female, and 3 were transgender. Convenient sampling is done, and data are extracted from their medical records and telephonic interviews. A self-designed survey-based questionnaire is used to record their symptoms. After extraction of all data by primary investigators a descriptive analysis is done. The result has been analyzed based on age and sex. All patients have been divided into five age groups, i.e., <15 years, 16–30 years, 31–45 years, 46–60 years, and >60 years.
RESULTS
The highest symptom prevalence is noted for fever. Fever is prevalent in patients of age group 16–30 years and 31–45 years, showing a 16% prevalence in each. Shortness of breath is prevalent in 13% of the patients 16–30 years' age, 12% in 31–45 years' age group, and 13% in 46–60 years' age group. Sore throat prevalence in 16–30 years is 14%, 31–45 years is 14%, and 46–60 years is 9%. The highest prevalence of shortness of breath, fever, and sore throat is among the patients of 16–30 years and 31–45 years. The least prevalent symptom noted is urticaria which is prevalent in 4% of the patients of 31–45 years' age group. The prevalence of cough is 17% in >60 years' age group patients, while expectoration in >60 years' age group is 2%. About 32% of the patients report fatigue, with a maximum of 13% being in 31–45 years' age group. Myalgia has a maximum of 13% prevalence in 31–45 years' age group patients. The highest prevalence of headache is 9% in patients of age group 31–45 years. Diarrhea, urticaria, and anosmia are the least reported symptoms [Table 1 and Figure 1].
Table 1.
Prevalence of symptoms according to the age group
| Age (years) | Prevalence of symptoms (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cough | Expectoration | Shortness of breath | Sore throat | Fever | Myalgia | Fatigue | Headache | Diarrhea | Anosmia | Urticaria | |
| <15 | 2 | 2 | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 16-30 | 6 | 5 | 13 | 14 | 16 | 4 | 7 | 3 | 3 | 2 | 0 |
| 31-45 | 14 | 7 | 12 | 14 | 16 | 13 | 13 | 9 | 1 | 5 | 4 |
| 46-60 | 12 | 6 | 13 | 9 | 12 | 5 | 9 | 3 | 3 | 0 | 0 |
| >60 | 17 | 2 | 3 | 3 | 3 | 2 | 3 | 3 | 1 | 1 | 0 |
Figure 1.
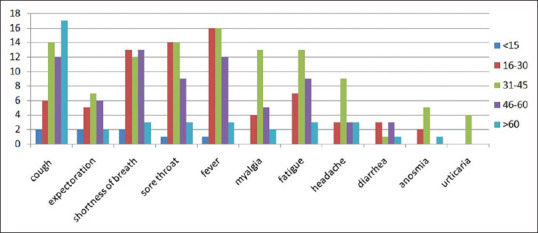
Symptom prevalence according to the age
Sex-wise prevalence of symptoms shows a maximum of 35% of the females, 11% of the males, and 2% of the transgenders with fever and a minimum prevalence of 4% of the females with urticaria. About 28% of the males, 14% of the females, and 1% of the transgenders have shortness of breath. Nearly 20% of the males, 18% of the females, and 3% of the transgenders have a sore throat. Cough is prevalent in 28% of the females, 10% of the males, and 3% of the transgenders. Expectoration is seen in 15% of the females and 7% of males. Fatigue is seen in 23% of the females, 8% of the males, and 1% of the transgenders. Myalgia is seen in 18% of the females, 5% of the males, and 1% of the transgenders. Diarrhea and anosmia are seen in 5% of the females, 1% and 3% males, respectively. Although the number of male patients was more as compared to female patients, fever has shown a 35% prevalence in females as compared to 11% in males. Cough has a 28% prevalence in females as compared to 10% in males. Similarly, myalgia, fatigue, headache, diarrhea, anosmia, and urticarial are more prevalent in females as compared to males [Table 2 and Figure 2].
Table 2.
Prevalence of symptom according to the sex
| Sex | Prevalence of symptoms (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cough | Expectoration | Shortness of breath | Sore throat | Fever | Myalgia | Fatigue | Headache | Diarrhea | Anosmia | Urticaria | |
| Male | 10 | 7 | 28 | 20 | 11 | 5 | 8 | 7 | 1 | 3 | 0 |
| Female | 28 | 15 | 14 | 18 | 35 | 18 | 23 | 11 | 5 | 5 | 4 |
| Other | 3 | 0 | 1 | 3 | 2 | 1 | 1 | 0 | 0 | 0 | 0 |
Figure 2.
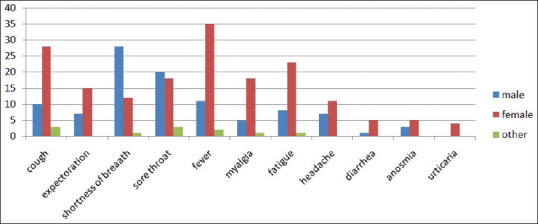
Symptom prevalence according to the sex
DISCUSSION
Clinical manifestation ranges from mild-to-severe respiratory symptoms with some even resulting in death.[4] Most common symptoms include fever, cough, myalgia, fatigue, pneumonia, and complicated dyspnea, while the least common symptoms are headache, diarrhea, hemoptysis, running nose, and phlegm producing cough.[4,5] Recovery of mild symptomatic patients occurs within a week, while severe cases experience progressive respiratory failure due to alveolar damage, leading to death.[6] Laboratory values and radiological investigations describe it as low lymphocytes and white blood cell count and new pulmonary infiltrate.[7] The diagnosis of coronavirus disease is made by reverse transcription–polymerase chain reaction, detecting positive nucleic acid of SARS CoV-2 in sputum, throat swab, and secretion of the respiratory tract.[6,8,9]
Adhikari et al. conducted a study on COVID-19 patients and reported that most common symptoms include fever, cough, myalgia, fatigue, pneumonia, and complicated dyspnea, while the least common symptoms are headache, diarrhea, hemoptysis, running nose, and phlegm producing cough.[2] Lu et al. conducted a study to look for nonrespiratory symptoms in COVID-19 patients and described that out of 72,314 COVID-19 patients, 889 had no symptoms at all. Some patients had mild urticarial.[10]
Rasmussen et al. conducted a study and reported that frequent manifestations include fever, cough, myalgia headache, and diarrhea. About 17%–29% of hospitalized patients develop respiratory distress syndrome.[11]
Li et al. conducted a study on the neuroinvasive potential of SARS CoV2 and described that the most characteristic symptom of COVID-19 is respiratory distress, but in some cases, neurological symptoms such as headache, nausea, and vomiting have also been reported. They reported that some coronaviruses are able to spread via synapse-connected route to the medullary cardiorespiratory center, and therefore, it can cause respiratory distress and failure.[12]
Kotfis and Skonieczna-Żydecka conducted a study on gastrointestinal symptoms in COVID-19 patients and found to have a less common prevalence of gastrointestinal symptoms which include nausea, vomiting, abdominal discomfort, and diarrhea.[13] Wu et al. conducted a study on ocular manifestations of COVID-19 patients and reported that 31.6% of the patients with 95% confidential interval had ocular manifestations consistent with conjunctivitis, including conjunctival hyperemia, chemosis, epiphora, or increased secretions.[14]
Sun et al. conducted a study on the pediatric population of Wuhan aged between 2 months and 15 years and described that the most common symptom in this population is polypnea, followed by fever and cough.[15]
Several public health measures can be adopted to prevent transmission of infection. Case isolation, identification and follow-up of contacts, environmental disinfection, and use of personal protective equipment are considered to be protective and effective in the prevention of disease transmission.[16]
To date, there is no specific antiviral treatment available for coronavirus disease. Recommended treatment is symptomatic and supportive.[4,5] Apart from it, reducing hospital-acquired infections and prior psychological intervention is also effective in the treatment of COVID-19.[17,18] Since there is no vaccine available till date, the best prevention of the disease is to avoid exposure to the virus.[19]
CONCLUSION
Male patients are more as far as COVID incidence is concerned, while female patients show a high prevalence of symptoms as compared to male patients. Patients presenting with COVID-positive report suffer a significant burden of symptoms, and timely recognition of symptoms and their management can significantly reduce morbidity and mortality due to COVID-19.
Limitation of the study
It is a study conducted at a tertiary care isolation center. Therefore, it may not estimate the exact prevalence of symptoms for the population.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020 [Internet] Whoint. 2020. Available from: https://wwwwhoint/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 . Last cited 2020 Jun 18.
- 2.Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infect Dis Poverty. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO COVID-19 Dashboard. Covid 19. [Last accessed on 2020 Apr 17]. Available from: https://covid19whoint/
- 4.CDC. 2019 Novel Coronavirus. Wuhan, China: 2020. [Last accessed on 2020 Feb 01]. Available from: https://wwwcdcgov/coronavirus/2019-nCoV/summaryhtml . [Google Scholar]
- 5.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yi Y, Lagniton PN, Ye S, Li E, Xu RH. COVID-19: What has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci. 2020;16:1753–66. doi: 10.7150/ijbs.45134. Published online 2020 Mar 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feng H, Liu Y, Lv M, Zhong J. A case report of COVID-19 with false negative RT-PCR test: Necessity of chest CT? Jpn J Radiol. 2020;38:409–10. doi: 10.1007/s11604-020-00967-9. doi:10.1007/s11604-020-00967-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Health Commission of People's Republic of China. Pneumonia Diagnosis and Treatment of 2019-nCoV Infection from Chinese NHC and CDC 2020. 2020. [Last accessed on 2020 Feb 01]. Available from: http://wwwnhcgovcn/xcs/zhengcwj/202001/4294563ed35b43209b31739bd0785e67/files/7a9309111267475a99d4306962c8bf78pdf .
- 10.Lu S, Lin J, Zhang Z, Xiao L, Jiang Z, Chen J, et al. Alert for non-respiratory symptoms of Coronavirus Disease 2019 (COVID-19) patients in epidemic period: A case report of familial cluster with three asymptomatic COVID-19 patients. J Med Virol Accepted Author Manuscript. doi: 10.1002/jmv.25776. doi:101002/jmv25776. [DOI] [PubMed] [Google Scholar]
- 11.Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus Disease 2019 (COVID-19) and pregnancy: What obstetricians need to know. Am J Obstet Gynecol. 2020;222:415–26. doi: 10.1016/j.ajog.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients? J Med Virol. 2020;92:552–5. doi: 10.1002/jmv.25728. doi:10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kotfis K, Skonieczna-Żydecka K. COVID-19: Gastrointestinal symptoms and potential sources of 2019-nCoV transmission. Anaesthesiology Intensive Therapy 2020 Mar. doi: 10.5114/ait.2020.93867. DOI: 105114/ait202093867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of Ocular Findings of Patients With Coronavirus Disease 2019 (COVID-19) in Hubei Province, China [published online ahead of print, 2020 Mar 31] JAMA Ophthalmol. 2020;138(5):575–578. doi: 10.1001/jamaophthalmol.2020.1291. doi:10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun D, Li H, Lu XX, Xiao H, Ren J, Zhang FR, et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center's observational study [published online ahead of print, 2020 Mar 19] World J Pediatr. 2020:1–9. doi: 10.1007/s12519-020-00354-4. doi:101007/s12519-020-00354-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wei Q, Ren Z. Disinfection measures for pneumonia foci infected by novel coronavirus in 2019. Chin J Disinfect. 2020;37:59–62. [Google Scholar]
- 17.Wang C, Wang X. Prevalence, nosocomial infection and psychological prevention of novel coronavirus infection. Chin General Pract Nurs. 2020;18:2–3. [Google Scholar]
- 18.Xu M, Zhang Y. Investigation on the psychological status of the first batch of clinical first-line support nurses to fight against pneumonia caused by novel coronavirus. Chin Nurs Res. 2020;34:1–3. [Google Scholar]
- 19.Chen WH, Strych U, Hotez PJ, Bottazzi ME. The SARS-CoV-2 Vaccine Pipeline: An Overview [published online ahead of print, 2020 Mar 3] Curr Trop Med Rep. 2020:1–4. doi: 10.1007/s40475-020-00201-6. doi:101007/s40475-020-00201-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


