Abstract
Background:
The tibial tuberosity-trochlear groove distance is used as an indicator for medial tibial tubercle transfer; however, to our knowledge, no studies have verified whether this distance is strongly affected by tubercle lateralization at the proximal part of the tibia. We hypothesized that the tibial tuberosity-trochlear groove distance is mainly affected by tibial tubercle lateralization at the proximal part of the tibia.
Methods:
Forty-four patients with a history of patellar dislocation and forty-four age and sex-matched controls were analyzed with use of computed tomography. The tibial tuberosity-trochlear groove distance, tibial tubercle lateralization, trochlear groove medialization, and knee rotation were measured and were compared between the patellar dislocation group and the control group. The association between the tibial tuberosity-trochlear groove distance and three other parameters was calculated with use of the Pearson correlation coefficient and partial correlation analysis.
Results:
There were significant differences in the tibial tuberosity-trochlear groove distance (p < 0.001) and knee rotation (p < 0.001), but there was no difference in the tibial tubercle lateralization (p = 0.13) and trochlear groove medialization (p = 0.08) between the patellar dislocation group and the control group. The tibial tuberosity-trochlear groove distance had no linear correlation with tubercle lateralization (r = 0.21) or groove medialization (r = −0.15); however, knee rotation had a good positive correlation in the patellar dislocation group (r = 0.62). After adjusting for the remaining parameters, knee rotation strongly correlated with the tibial tuberosity-trochlear groove distance (r = 0.69, p < 0.001), whereas tubercle lateralization showed moderate significant correlations in the patellar dislocation group (r = 0.42; p = 0.005).
Conclusions:
Because the tibial tuberosity-trochlear groove distance is affected more by knee rotation than by tubercle malposition, its use as an indicator for tibial tubercle transfer may not be appropriate.
Clinical Relevance:
Surgical decisions of tibial tubercle transfer should be made after the careful analysis of several underlying factors of patellar dislocation.
Although lateral patellar dislocation is a common problem in orthopaedic practice, this morbidity is multifactorial, and the treatment remains controversial. Several contributing factors have been reported, such as patella alta, trochlear dysplasia, patellar proportion, and medial patellofemoral ligament insufficiency. Historically, lateralization of the tibial tubercle has been considered an important anatomical feature1-5.
For the quantitative evaluation of tibial tubercle lateralization, Goutallier et al. described the tibial tuberosity-trochlear groove distance on axial radiographs6. Since this initial report, measuring the tibial tuberosity-trochlear groove distance has improved after the use of axial computed tomography (CT), as it is a more accurate and reliable method and is commonly used for surgical decision-making in patients with patellofemoral dislocation3. Dejour et al. reported that a tibial tuberosity-trochlear groove distance of >20 mm is generally considered pathological and as an indication for medial tibial tubercle transfer in symptomatic patients3. There have been several reports on tubercle transfer for patellar dislocation using these criteria7-11.
However, the tibial tuberosity-trochlear groove distance is theoretically affected by tibial tubercle lateralization and by trochlear groove medialization and tibiofemoral rotation. If the tibial tuberosity-trochlear groove distance is used to determine whether tibial tubercle transfer is indicated, it must be verified whether lateralization of the tubercle at the proximal part of the tibia has a large impact on this value. However, to our knowledge, no studies have been conducted to determine this. The aim of this study was to assess with use of CT the effect of lateralization of the tibial tubercle, medialization of the trochlear groove, and knee rotation on the tibial tuberosity-trochlear groove distance in patients with a history of patellar dislocation and in an age and sex-matched control group. We hypothesized that an increase in the tibial tuberosity-trochlear groove distance mostly originates from lateralization of the tubercle at the proximal part of the tibia and that it is reasonable to use this value as an indicator for tibial tubercle transfer.
Materials and Methods
Participants
We retrospectively reviewed CT images of knee joints in two groups of patients from our hospital between 2005 and 2014.
In the first group (patellar dislocation), we reviewed the images of forty-four knees in forty-four consecutive patients; there were eight male patients and thirty-six female patients, and the mean patient age (and standard deviation) was 25.1 ± 10.4 years (range, thirteen to forty-six years). The images were taken at our hospital for the diagnosis of acute and chronic lateral patellar dislocation. All of the patients were diagnosed on the basis of their history, clinical examination (e.g., patient sensation of impending dislocation and/or reduction of the patellofemoral joint in the emergency department and the presence of the apprehension sign), or magnetic resonance imaging (MRI) findings (i.e., bone edema of the lateral condyle and the medial part of the patella and a tear in the medial stabilizer)12,13. This group comprised ten patients with acute traumatic dislocation and thirty-four patients with recurrent dislocation. Patients with severe osteoarthritis and a history of surgery for patellar dislocation were excluded.
The second group (the control group) was an age and sex-matched cohort of forty-four patients (forty-four knees) with no history of patellar instability or patellofemoral symptoms; there were eight male patients and thirty-six female patients, and the mean patient age (and standard deviation) was 25.5 ± 11.1 years (range, thirteen to forty-six years). The patients in this group were consecutively selected from ordinary referrals for knee CT examinations at our hospital. Of the forty-four patients included in this group, CT examinations were performed for bipartite patella (n = 5), osteochondritis dissecans (n = 6), osteocartilage defects (n = 4), suspected stress and minor fractures (n = 6), and soft-tissue and bone tumors around the knee joint (n = 7), and sixteen individuals were volunteers. Patients with a knee ligament injury, patellofemoral disabilities, major fractures, or a history of surgery were excluded.
The present study was approved by the local ethics committee of our institution. Because of the retrospective nature of the study, informed consent was obtained only for asymptomatic volunteers.
CT Protocol
All of the knees were scanned with use of a slice CT scanner (SOMATOM Sensation 16; Siemens Medical Solutions, Erlangen, Germany) and the following parameters: 512 × 512 matrix, 1-mm thickness, approximately five to ten-second scan time, 0-mm skip between slices, field of view of 14 cm, and bone kernel. The patients were scanned in the supine position with the knee fully extended with slight external rotation as needed for comfort. Straps were wrapped over the thigh to minimize motion without a fixation device. The CT data were reconstructed with use of software for image analysis (OsiriX, version 5.5; Pixmeo, Geneva, Switzerland). Axial images of the distal femoral and proximal tibial condyle were used to measure the tibial tuberosity-trochlear groove distance, tibial tubercle lateralization, trochlear groove medialization, and knee rotation. A single experienced orthopaedic surgeon (K.T.) performed all measurements. The subjects’ identifying information (name, age, sex, and presence of dislocation) was blinded.
Tibial Tuberosity-Trochlear Groove Distance
The tibial tuberosity-trochlear groove distance was measured with use of a technique described by Schoettle et al. (Fig. 1)14. First, we drew the posterior condylar line on the image, which represented the best Roman arch, that connected the most posterior aspects of the osseous surface on the posterior femoral condyle. Next, we drew a perpendicular line through the deepest point of the trochlea. The tibial tubercle location was specified at the level of the most cephalad image in which the patellar tendon was completely in contact with the tibial tubercle. The tibial tuberosity-trochlear groove interval was measured between the most anterior point of the tibial tubercle and the deepest point of the trochlear groove, perpendicular to the posterior condylar tangents on axial CT scans.
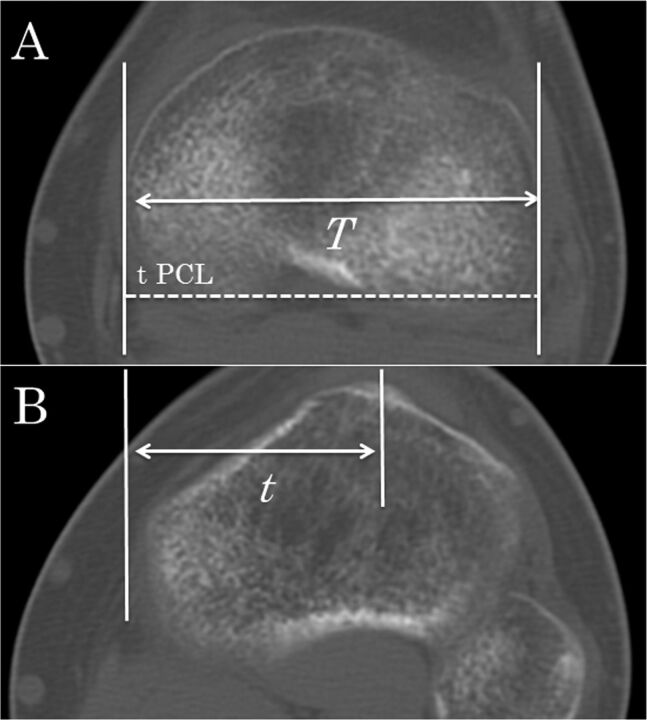
Fig. 1.
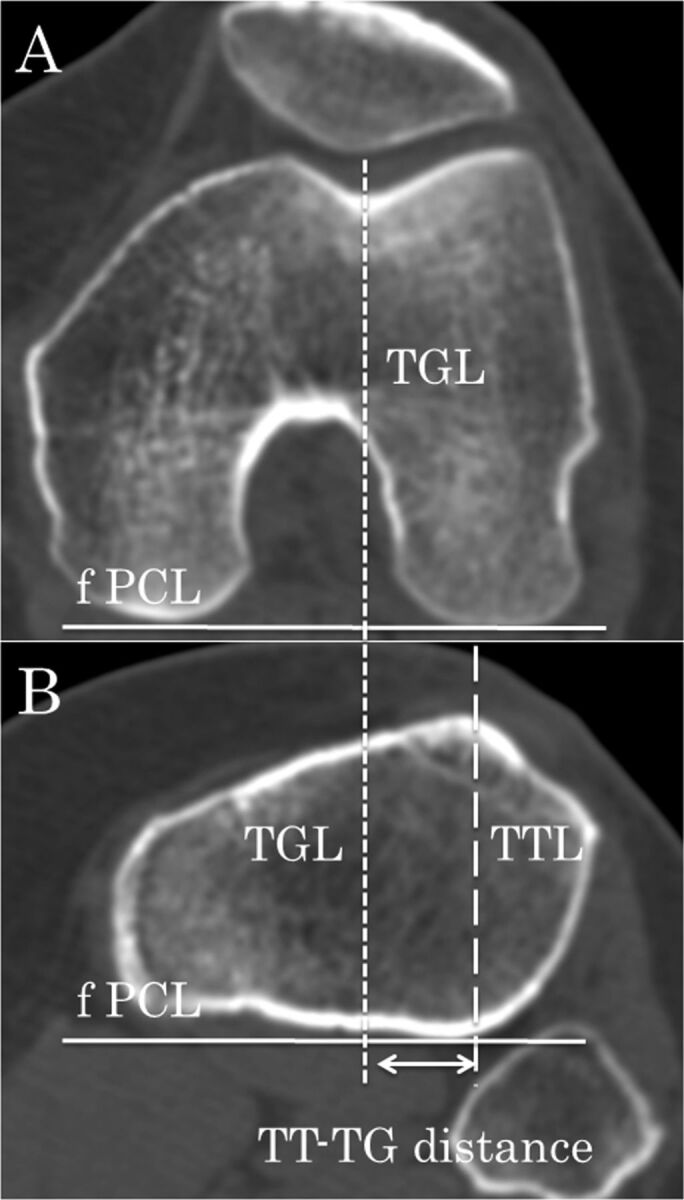
Figs. 1-A and 1-B Measurement of the tibial tuberosity-trochlear groove (TT-TG) distance. Fig. 1-A The TT-TG distance is the mediolateral distance between the midpoint of the insertion of the patellar tendon and the trochlear groove perpendicular to the femoral posterior condylar line (fPCL). TGL = trochlear groove line. Fig. 1-B The solid line indicates the femoral posterior condylar line (fPCL), the line with shorter dashes indicates the trochlear groove line (TGL), and the line with longer dashes indicates the tibial tubercular line (TTL).
Tibial Tubercle Lateralization
Tibial tubercle lateralization assessed the relative lateralized tubercle position at the proximal tibial condyle with use of a modified method by Ando (Fig. 2)15. Two slices in which the posterior condylar notch was clearly recognized and the patellar tendon was completely in contact with the tibial tubercle were used for this calculation. The width of the proximal tibial condyle was measured between two perpendicular lines to the posterior tibial condyle line, tangent to the medial and lateral border of the proximal tibial condyle (distance T). The tibial tubercle lateralized distance was defined as the mediolateral distance between the midpoint of the insertion of the patellar tendon and the medial border of the proximal tibial condyle (distance t). Tibial tubercle lateralization was calculated as t ÷ T.
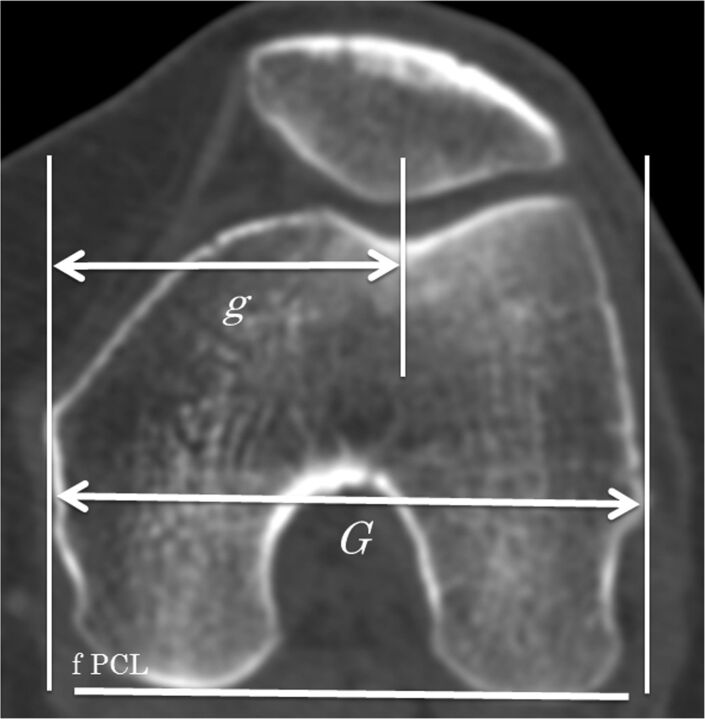
Fig. 2.
Figs. 2-A and 2-B Measurement of the tibial tuberosity lateralization. Fig. 2-A The total width of the proximal tibial condyle, which is parallel to the tibial posterior condylar line (tPCL), indicated by the dashed line, is defined as T. Fig. 2-B The distance between the medial border of the proximal tibial condyle and the tip of the tibial tubercle, which is parallel to the tPCL, is defined as t. Tibial tuberosity lateralization is calculated as t ÷ T.
Trochlear Groove Medialization
Trochlear groove medialization assessed the relative medialized position of the trochlear groove at the distal part of the femur with use of a modified method by Ando et al. (Fig. 3)16. The slice in which the lateral epicondyle and medial sulcus could be identified was used for this calculation. The width of the femoral condyle was measured along a line parallel to the posterior condylar line; this distance was defined as G. The distance between the bottom of the groove and the medial edge of the femoral condyle was defined as g. The index of the trochlear groove medialization was calculated as g ÷ G.
Fig. 3.
Measurement of the trochlear groove medialization. The total width of the distal femoral condyle, which is parallel to the femoral posterior condylar line (fPCL), denoted by a solid line, is defined as G. The distance between the medial border of the distal femoral condyle and the bottom of the trochlear groove, which is parallel to the fPCL, is defined as g. The trochlear groove medialization is calculated as g ÷ G.
Knee Rotation
Knee rotation was defined as the relative rotational difference between the distal part of the femur and proximal part of the tibia at the knee joint level by measuring the twist angle of each posterior condylar line of the proximal part of the tibia and the distal part of the femur (Fig. 4)12,17. The axial slice of the distal part of the femur was selected from the level of the deepest point of the trochlea and the axial slice of the tibial plateau was selected from the clearly recognized posterior condylar notch of the tibia. The axis of the distal part of the femur was a tangent line connecting the most posterior aspect of the medial femoral condyle and the tibial plateau and the axis of the proximal part of the tibia was a tangent line connecting the most posterior aspect of the lateral femoral condyle and the tibial plateau. The knee rotation angle was defined as the angle between these two axes. A positive angle indicated external rotation of the tibia relative to the femur.
Fig. 4.
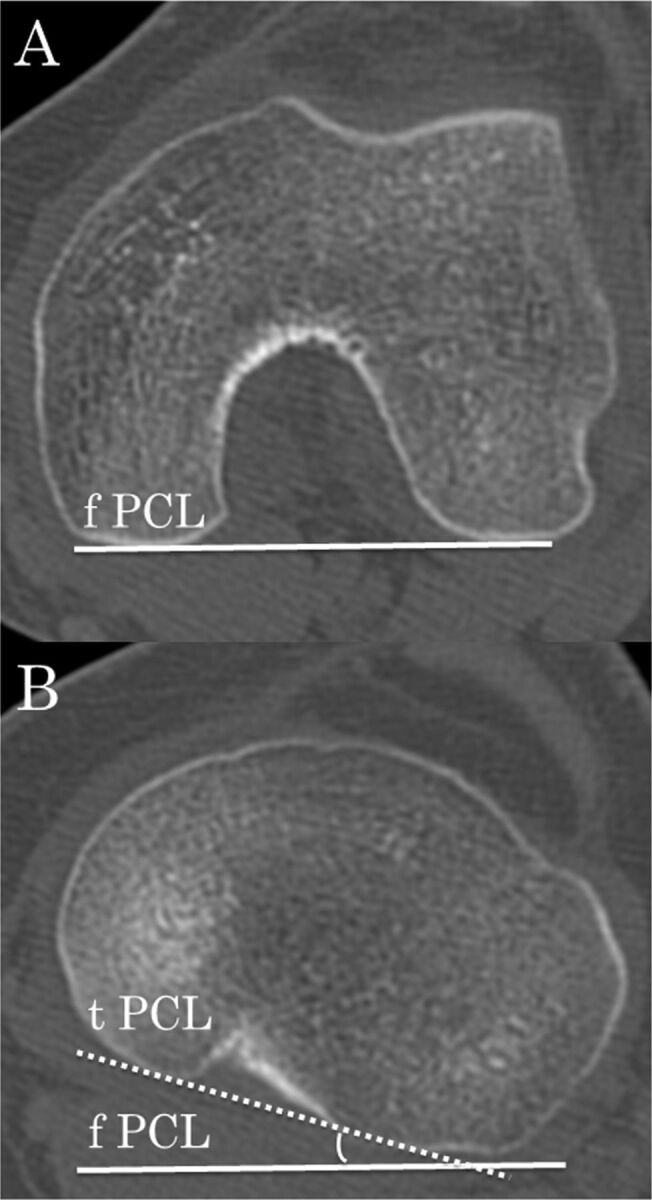
Figs. 4-A and 4-B Measurement of the knee rotation angle. Fig. 4-A The solid line denotes the femoral posterior condylar line (fPCL). Fig. 4-B Rotation is defined by the angle between the fPCL and the tibial posterior condylar line (tPCL), denoted by the dotted line. A positive angle indicates external rotation of the tibia relative to the femur.
Statistical Analysis
The intraclass and interclass correlation coefficient of the measurements was calculated in twenty randomly selected patients, and the four parameters were measured in two independent trials by two independent authors (K.T. and S.T.). A power analysis determined the number of required patients. Tibial tubercle lateralization, trochlear groove medialization, and knee rotation were defined as the primary parameters. A minimum sample size of thirty-six knees in each group was required for an α value of 0.05 and β value of 0.8, while considering a clinical difference of 2% for tibial tubercle lateralization, 2% for trochlear groove medialization, and 3° for knee rotation. Therefore, we included forty-four patients in our study. The means and standard deviations were calculated for all of the parameters, which were then compared between the patellar dislocation group and the control group with use of unpaired t tests. The strength of the linear association between the tibial tuberosity-trochlear groove distance and the other three factors was obtained with use of the Pearson correlation coefficient. Further, we calculated the partial correlation coefficient for each parameter after adjusting for the remaining variables as covariates. All of the statistical tests were performed with use of SPSS for Windows (version 21; IBM, Armonk, New York).
Source of Funding
No external funding was received for this study.
Results
The tibial tuberosity-trochlear groove distance, tibial tubercle lateralization, trochlear groove medialization, and knee rotation showed excellent to poor agreement for intraobserver and interobserver variability. The intraclass correlation coefficient was 0.85 for the tibial tuberosity-trochlear groove distance, 0.71 for tibial tubercle lateralization, 0.35 for trochlear groove medialization, and 0.98 for knee rotation. The interobserver correlation coefficient was 0.82 for the tibial tuberosity-trochlear groove distance, 0.71 for tibial tubercle lateralization, 0.65 for trochlear groove medialization, and 0.97 for knee rotation.
The tibial tuberosity-trochlear groove distance and knee rotation were significantly different between the patellar dislocation group and the control group; the tibial tuberosity-trochlear groove distance was 19.3 ± 4.2 mm for the patellar dislocation group compared with 14.4 ± 2.9 mm for the control group (p < 0.001), and the knee rotation was 8.5° ± 7.0° for the patellar dislocation group compared with 4.0° ± 3.7° for the control group (p < 0.001) (Fig. 5). However, there were no significant differences in tibial tubercle lateralization and trochlear groove medialization between the two groups; the tibial tubercle lateralization was 0.66 ± 0.03 in the patellar dislocation group compared with 0.65 ± 0.02 in the control group (p = 0.13), and the trochlear groove medialization was 0.52 ± 0.03 in the patellar dislocation group compared with 0.53 ± 0.02 in the control group (p = 0.08) (Fig. 6).
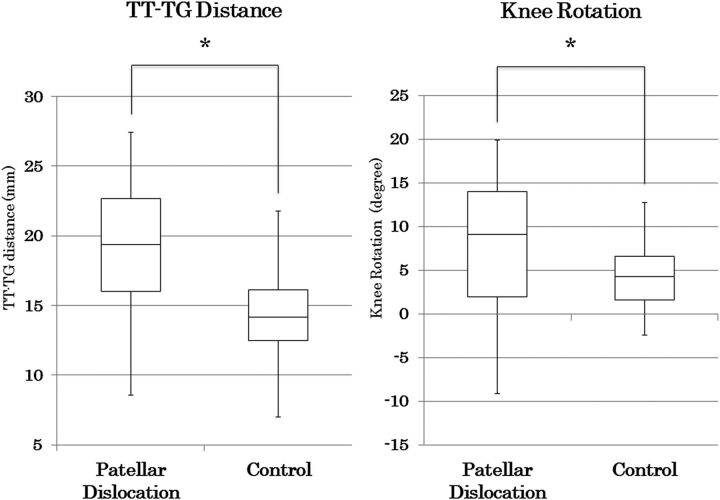
Fig. 5.
Box plots of the tibial tubercle-trochlear groove (TT-TG) distance and knee rotation in the patellar dislocation group compared with the control group. The asterisk indicates significance at p < 0.05. The error bars indicate the minimum and maximum values.
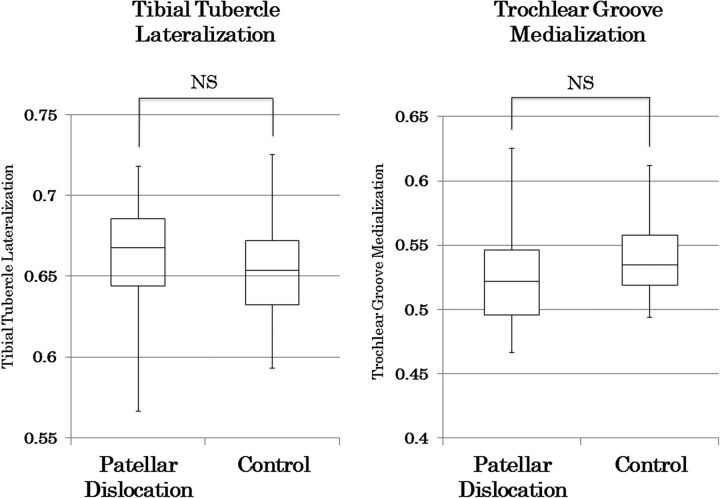
Fig. 6.
Box plots of the tibial tuberosity lateralization and trochlear groove medialization in the patellar dislocation group compared with the control group. NS = not significant. The error bars indicate the minimum and maximum values.
Table I shows the linear correlations and the associated p values between the tibial tuberosity-trochlear groove distance and the other three factors. Tibial tubercle lateralization was not significantly correlated in the patellar dislocation group, although it had a moderate correlation in the control group. Trochlear groove medialization exhibited no correlation with the tibial tuberosity-trochlear groove distance in either group. In contrast, moderate to good positive correlations were found between tibial tuberosity-trochlear groove distance and knee rotation in the patellar dislocation group and the control group.
TABLE I.
Results of Linear Correlation Analysis Between Tibial Tubercle-Trochlear Groove Distance and Each Parameter
| Patellar Dislocation |
Control |
|||
| Parameter | Coefficient | P Value | Coefficient | P Value |
| Tibial tubercle lateralization | 0.21 | 0.15 | 0.47 | 0.001 |
| Trochlear groove medialization | −0.15 | 0.33 | −0.03 | 0.84 |
| Knee rotation | 0.62 | <0.001 | 0.51 | <0.001 |
Table II shows the partial correlation coefficients and p values between the tibial tuberosity-trochlear groove distance and the other three factors. The tibial tuberosity-trochlear groove distance was significantly correlated with tibial tubercle lateralization and knee rotation; however, although knee rotation was strongly correlated with the tibial tuberosity-trochlear groove distance, tibial tubercle lateralization showed a moderate correlation in the patellar dislocation group and the control group. Furthermore, trochlear groove medialization exhibited no significant correlation with the tibial tuberosity-trochlear groove distance in the patellar dislocation group and a weak negative correlation in the control group.
TABLE II.
Results of Partial Correlation Analysis Between Tibial Tubercle-Trochlear Groove Distance After Adjusting for Other Factors
| Patellar Dislocation |
Control |
|||
| Parameter | Coefficient | P Value | Coefficient | P Value |
| Tibial tubercle lateralization | 0.42 | 0.005 | 0.55 | <0.001 |
| Trochlear groove medialization | −0.15 | 0.33 | −0.34 | 0.02 |
| Knee rotation | 0.69 | <0.001 | 0.61 | <0.001 |
Discussion
The present study’s findings unexpectedly showed that the degree of tibial tubercle lateralization in the patellar dislocation group was not significantly greater than that of the control group as had been previously considered, and knee rotation in the patellar dislocation group was significantly greater than that in the control group. Moreover, the tibial tuberosity-trochlear groove distance was more strongly affected by knee rotation and was less affected by malposition of the tibial tubercle or trochlear groove. We were unable to find other studies that showed similar findings. Our findings suggest major implications for interpreting the tibial tuberosity-trochlear groove distance.
The tibial tuberosity-trochlear groove distance is the gold-standard method for evaluating the patellar lateral force vector, and it has been validated in multiple studies for many years18-22. However, some studies have cast doubt on the usefulness of this method, because aspects such as the differences in modality23, knee angle during imaging24,25, and the presence of weight-bearing26 have been shown to change the value of the tibial tuberosity-trochlear groove distance. Sherman et al. reported that caution is needed when interpreting the tibial tuberosity-trochlear groove distance in the presence of excessive femoral anteversion and tibial external rotation9. Furthermore, according to Camathias et al., rotation of the knee joint significantly altered the tibial tuberosity-trochlear groove value; thus, it may be affected by the leg position in the CT scan, and surgeons should consider this for decision-making with regard to the realignment procedure27.
Many studies have shown greater tibial tubercle lateralization in patients with patellar dislocation than in healthy people28-30. However, most of these describe lateralization of the tibial tubercle relative to the femur, and few have examined malposition of the tubercle at the proximal part of the tibia. Ando measured lateralization of the tubercle at the proximal part of the tibia with CT and found that lateralization was 15% greater in the dislocation group than in the non-dislocation group15. However, because his method evaluated the degree of tibial tubercle displacement on the same slice as the tip of the tibial tubercle, uncertainty remains whether this is a valid method for evaluating tibial tubercle malposition at the proximal part of the tibia. Recently, Seitliger et al. used the tibial tubercle-posterior cruciate ligament distance measurement method to evaluate tubercle malposition at the proximal part of the tibia31. They found that, among forty subjects with a tibial tuberosity-trochlear groove distance of ≥20 mm, seventeen (43%) had a normal tibial tubercle-posterior cruciate ligament distance. They found no correlation between the tibial tuberosity-trochlear groove and tibial tubercle-posterior cruciate ligament distances, although they did find correlations between the former and the patellar tilting angle and knee rotation. Our findings are similar to theirs in that tubercle malposition at the proximal part of the tibia did not have a great impact on the tibial tuberosity-trochlear groove distance as expected, and there was a correlation between the tibial tuberosity-trochlear groove distance and knee rotation.
There have been some reports on the relationship between patellar dislocation and rotational malalignment of the lower leg12,32-35. Diederichs et al. used MRI to evaluate the rotational alignment of the entire lower leg, and they reported a significantly greater femoral anteversion and knee rotation in the dislocation group compared with the control group12. They emphasized the importance of rotational alignment in causing patellar dislocation. Moreover, several researchers have reported relationships between patellar dislocation and tibial torsional deformities and that good results can be obtained by performing corrective osteotomy in cases with large deformities32,33. However, Reikerås stated that parameters related to patellar dislocation such as sulcus angle, congruence angle, and tilting angle have mostly no correlation with femoral anteversion36. In addition, there was some difficulty determining the thresholds of lower-leg rotation because of its wide variation, even among healthy people37. Regardless, there have been several studies on the relationship between lower-leg rotational alignment and patellar dislocation; however, this association is controversial. In the present study, correlation analysis indicated that knee rotation has a great impact on the tibial tuberosity-trochlear groove distance. Although our evaluation was limited to only one parameter of several rotational profiles, this finding may imply a relationship between rotational alignment and patellar dislocation.
The transition to surgical treatment for patellar dislocation over time has made the effectiveness of medial tibial tubercle transfer widely apparent. We believe that such a procedure would benefit patients with tubercle malposition and normal rotational alignment of the lower leg. However, if a medial tubercle transfer is performed in a patient without major tubercle lateralization, patellofemoral tracking may not normalize, and abnormal stress on the medial patellofemoral joint may persist38. Parikh and Noyes stated that tubercle osteotomy increases external tibial torsion and exacerbates symptoms in the presence of underlying rotational malalignment39. Nakagawa et al. verified the long-term results of tibial tubercle transfer in thirty-nine cases and found that osteoarthritic changes in the patellofemoral joint had advanced in 42% of cases40. We thought that the findings from these studies may imply non-anatomic restoration of patellofemoral tracking and the importance of a thorough preoperative analysis of the underlying factors, especially tibial tubercle lateralization at the proximal part of the tibia, to obtain good postoperative results for medial tibial tubercle transfer.
The present study had several limitations. First, trochlear groove medialization and tibial tubercle lateralization were evaluated with use of new measurement methods, which produced a lower intraclass correlation coefficient value than expected. However, variation between the measured values themselves was extremely small, with interparticipant and intraparticipant error approximately within 0% to 5%, and these methods basically had similar reference points and slice imaging techniques as the tibial tuberosity-trochlear groove distance, indicating that these were valid measurement methods. Further, we did not examine the entire lower-leg rotational parameters, especially femoral anteversion and tibial torsion. We only examined knee rotation as the relative rotational difference between the distal part of the femur and the proximal part of the tibia; thus, our findings were insufficient to discuss total leg rotational alignment. However, as the main purpose of the present study was to evaluate factors affecting the tibial tuberosity-trochlear groove distance, not rotational alignment, it was not essential to assess the detailed rotational profile of the whole leg, which did not have a direct effect on the tibial tuberosity-trochlear groove distance.
In the present study, there was no difference in tubercle malposition at the proximal part of the tibia between the dislocation and control groups. Tubercle malposition had a moderate effect on the tibial tuberosity-trochlear groove distance. Additionally, the patellar dislocation group exhibited significantly greater knee rotation, which was also found to strongly affect the tibial tuberosity-trochlear groove distance. When evaluating patients with patellar dislocation who need surgical intervention, it is important to assess the etiologic factors to tailor the surgical procedure to the needs of each patient. The tibial tuberosity-trochlear groove distance may be a reasonable criterion for medial tibial tubercle transfer, if the relative malposition between the tibial tubercle and the trochlear groove is considered as a major factor of patellar dislocation. However, surgeons should recognize that this procedure may not always represent a patient-centered treatment in some patients who have a tibial tuberosity-trochlear groove elevated by knee rotation and not by lateralization of the tibial tubercle. In these patients, we think that it is appropriate to use another procedure (e.g., medial patellofemoral ligament reconstruction, proximal realignment, trochleoplasty) that is based on individual pathological conditions and is not performed with tubercle transfer simultaneously. Thus, indications for tubercle transfer should be determined by the tibial tuberosity-trochlear groove distance and also by another value that directly reflects tubercle lateralization at the proximal part of the tibia. By meticulously examining all of the influencing factors, a more patient-specific treatment strategy will be developed.
Footnotes
Investigation performed at the Department of Orthopedic Surgery, Shinshu University School of Medicine, Matsumoto, Japan
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Airanow S, Zippel H. [Femoro-tibial torsion in patellar instability. A contribution to the pathogenesis of recurrent and habitual patellar dislocations]. Beitr Orthop Traumatol. 1990. June;37(6):311-6. German. [PubMed] [Google Scholar]
- 2.Charles MD, Haloman S, Chen L, Ward SR, Fithian D, Afra R. Magnetic resonance imaging-based topographical differences between control and recurrent patellofemoral instability patients. Am J Sports Med. 2013. February;41(2):374-84. [DOI] [PubMed] [Google Scholar]
- 3.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19-26. [DOI] [PubMed] [Google Scholar]
- 4.Monk AP, Doll HA, Gibbons CL, Ostlere S, Beard DJ, Gill HS, Murray DW. The patho-anatomy of patellofemoral subluxation. J Bone Joint Surg Br. 2011. October;93(10):1341-7. [DOI] [PubMed] [Google Scholar]
- 5.Redziniak DE, Diduch DR, Mihalko WM, Fulkerson JP, Novicoff WM, Sheibani-Rad S, Saleh KJ. Patellar instability. J Bone Joint Surg Am. 2009. September;91(9):2264-75. [PubMed] [Google Scholar]
- 6.Goutallier D, Bernageau J, Lecudonnec B. [The measurement of the tibial tuberosity. Patella groove distanced technique and results (author’s transl)]. Rev Chir Orthop Reparatrice Appar Mot. 1978. Jul-Aug;64(5):423-8. French. [PubMed] [Google Scholar]
- 7.Barber FA, McGarry JE. Elmslie-Trillat procedure for the treatment of recurrent patellar instability. Arthroscopy. 2008. January;24(1):77-81. Epub 2007 Nov 5. [DOI] [PubMed] [Google Scholar]
- 8.Koëter S, Diks MJ, Anderson PG, Wymenga AB. A modified tibial tubercle osteotomy for patellar maltracking: results at two years. J Bone Joint Surg Br. 2007. February;89(2):180-5. [DOI] [PubMed] [Google Scholar]
- 9.Sherman SL, Erickson BJ, Cvetanovich GL, Chalmers PN, Farr J, 2nd, Bach BR, Jr, Cole BJ. Tibial tuberosity osteotomy: indications, techniques, and outcomes. Am J Sports Med. 2013. November 6;42(8):2006-17. Epub 2013 Nov 6. [DOI] [PubMed] [Google Scholar]
- 10.Tecklenburg K, Feller JA, Whitehead TS, Webster KE, Elzarka A. Outcome of surgery for recurrent patellar dislocation based on the distance of the tibial tuberosity to the trochlear groove. J Bone Joint Surg Br. 2010. October;92(10):1376-80. [DOI] [PubMed] [Google Scholar]
- 11.Tsuda E, Ishibashi Y, Yamamoto Y, Maeda S. Incidence and radiologic predictor of postoperative patellar instability after Fulkerson procedure of the tibial tuberosity for recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2012. October;20(10):2062-70. Epub 2011 Dec 28. [DOI] [PubMed] [Google Scholar]
- 12.Diederichs G, Köhlitz T, Kornaropoulos E, Heller MO, Vollnberg B, Scheffler S. Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med. 2013. January;41(1):51-7. Epub 2012 Nov 7. [DOI] [PubMed] [Google Scholar]
- 13.Elias DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002. December;225(3):736-43. [DOI] [PubMed] [Google Scholar]
- 14.Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J. The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006. January;13(1):26-31. Epub 2005 Jul 14. [DOI] [PubMed] [Google Scholar]
- 15.Ando T. Factors affecting the rectus femoris-patellar tendon Q-angle, measured using a computed tomographic scan. J Orthop Sci. 1999;4(2):73-7. [DOI] [PubMed] [Google Scholar]
- 16.Ando T, Hirose H, Inoue M, Shino K, Doi T. A new method using computed tomographic scan to measure the rectus femoris-patellar tendon Q-angle comparison with conventional method. Clin Orthop Relat Res. 1993. April;(289):213-9. [PubMed] [Google Scholar]
- 17.Eckhoff DG, Johnston RJ, Stamm ER, Kilcoyne RF, Wiedel JD. Version of the osteoarthritic knee. J Arthroplasty. 1994. February;9(1):73-9. [DOI] [PubMed] [Google Scholar]
- 18.Balcarek P, Jung K, Ammon J, Walde TA, Frosch S, Schüttrumpf JP, Stürmer KM, Frosch KH. Anatomy of lateral patellar instability: trochlear dysplasia and tibial tubercle-trochlear groove distance is more pronounced in women who dislocate the patella. Am J Sports Med. 2010. November;38(11):2320-7. Epub 2010 Aug 16. [DOI] [PubMed] [Google Scholar]
- 19.Balcarek P, Jung K, Frosch KH, Stürmer KM. Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med. 2011. August;39(8):1756-61. Epub 2011 May 12. [DOI] [PubMed] [Google Scholar]
- 20.Dickens AJ, Morrell NT, Doering A, Tandberg D, Treme G. Tibial tubercle-trochlear groove distance: defining normal in a pediatric population. J Bone Joint Surg Am. 2014. February 19;96(4):318-24. [DOI] [PubMed] [Google Scholar]
- 21.Pandit S, Frampton C, Stoddart J, Lynskey T. Magnetic resonance imaging assessment of tibial tuberosity-trochlear groove distance: normal values for males and females. Int Orthop. 2011. December;35(12):1799-803. Epub 2011 Mar 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pennock AT, Alam M, Bastrom T. Variation in tibial tubercle-trochlear groove measurement as a function of age, sex, size, and patellar instability. Am J Sports Med. 2014. February;42(2):389-93. Epub 2013 Nov 13. [DOI] [PubMed] [Google Scholar]
- 23.Camp CL, Stuart MJ, Krych AJ, Levy BA, Bond JR, Collins MS, Dahm DL. CT and MRI measurements of tibial tubercle-trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med. 2013. August;41(8):1835-40. Epub 2013 Jul 15. [DOI] [PubMed] [Google Scholar]
- 24.Dietrich TJ, Betz M, Pfirrmann CW, Koch PP, Fucentese SF. End-stage extension of the knee and its influence on tibial tuberosity-trochlear groove distance (TTTG) in asymptomatic volunteers. Knee Surg Sports Traumatol Arthrosc. 2014. January;22(1):214-8. Epub 2012 Dec 23. [DOI] [PubMed] [Google Scholar]
- 25.Miyanishi K, Nagamine R, Murayama S, Miura H, Urabe K, Matsuda S, Hirata G, Iwamoto Y. Tibial tubercle malposition in patellar joint instability: a computed tomograpy study in full extension and at 30 degree flexion. Acta Orthop Scand. 2000. June;71(3):286-91. [DOI] [PubMed] [Google Scholar]
- 26.Izadpanah K, Weitzel E, Vicari M, Hennig J, Weigel M, Südkamp NP, Niemeyer P. Influence of knee flexion angle and weight bearing on the Tibial Tuberosity-Trochlear Groove (TTTG) distance for evaluation of patellofemoral alignment. Knee Surg Sports Traumatol Arthrosc. 2014. November;22(11):2655-61. Epub 2013 May 29. [DOI] [PubMed] [Google Scholar]
- 27.Camathias C, Pagenstert G, Stutz U, Barg A, Müller-Gerbl M, Nowakowski AM. The effect of knee flexion and rotation on the tibial tuberosity-trochlear groove distance. Knee Surg Sports Traumatol Arthrosc. 2015. January 21 Epub 2015 Jan 21. [DOI] [PubMed] [Google Scholar]
- 28.Insall J. Current Concepts Review: patellar pain. J Bone Joint Surg Am. 1982. January;64(1):147-52. [PubMed] [Google Scholar]
- 29.Metin Cubuk S, Sindel M, Karaali K, Arslan AG, Akyildiz F, Ozkan O. Tibial tubercle position and patellar height as indicators of malalignment in women with anterior knee pain. Clin Anat. 2000;13(3):199-203. [DOI] [PubMed] [Google Scholar]
- 30.Tsujimoto K, Kurosaka M, Yoshiya S, Mizuno K. Radiographic and computed tomographic analysis of the position of the tibial tubercle in recurrent dislocation and subluxation of the patella. Am J Knee Surg. 2000. Spring;13(2):83-8. [PubMed] [Google Scholar]
- 31.Seitlinger G, Scheurecker G, Högler R, Labey L, Innocenti B, Hofmann S. Tibial tubercle-posterior cruciate ligament distance: a new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med. 2012. May;40(5):1119-25. Epub 2012 Mar 13. [DOI] [PubMed] [Google Scholar]
- 32.Cameron JC, Saha S. External tibial torsion: an underrecognized cause of recurrent patellar dislocation. Clin Orthop Relat Res. 1996. July;(328):177-84. [PubMed] [Google Scholar]
- 33.Drexler M, Dwyer T, Dolkart O, Goldstein Y, Steinberg EL, Chakravertty R, Cameron JC. Tibial rotational osteotomy and distal tuberosity transfer for patella subluxation secondary to excessive external tibial torsion: surgical technique and clinical outcome. Knee Surg Sports Traumatol Arthrosc. 2014. November;22(11):2682-9. Epub 2013 Jun 6. [DOI] [PubMed] [Google Scholar]
- 34.Sanfridsson J, Arnbjörnsson A, Fridén T, Ryd L, Svahn G, Jonsson K. Femorotibial rotation and the Q-angle related to the dislocating patella. Acta Radiol. 2001. March;42(2):218-24. [PubMed] [Google Scholar]
- 35.Turner MS. The association between tibial torsion and knee joint pathology. Clin Orthop Relat Res. 1994. May;(302):47-51. [PubMed] [Google Scholar]
- 36.Reikerås O. Patellofemoral characteristics in patients with increased femoral anteversion. Skeletal Radiol. 1992;21(5):311-3. [DOI] [PubMed] [Google Scholar]
- 37.Schneider B, Laubenberger J, Jemlich S, Groene K, Weber HM, Langer M. Measurement of femoral antetorsion and tibial torsion by magnetic resonance imaging. Br J Radiol. 1997. June;70(834):575-9. [DOI] [PubMed] [Google Scholar]
- 38.Kuroda R, Kambic H, Valdevit A, Andrish JT. Articular cartilage contact pressure after tibial tuberosity transfer. A cadaveric study. Am J Sports Med. 2001. Jul-Aug;29(4):403-9. [DOI] [PubMed] [Google Scholar]
- 39.Parikh S, Noyes FR. Patellofemoral disorders: role of computed tomography and magnetic resonance imaging in defining abnormal rotational lower limb alignment. Sports Health. 2011. March;3(2):158-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nakagawa K, Wada Y, Minamide M, Tsuchiya A, Moriya H. Deterioration of long-term clinical results after the Elmslie-Trillat procedure for dislocation of the patella. J Bone Joint Surg Br. 2002. August;84(6):861-4. [DOI] [PubMed] [Google Scholar]