Abstract
Background:
Neurofilament light chain (NfL), an index of neuroaxonal injury, is a promising diagnostic and prognostic fluid biomarker with high translational value in many neurodegenerative disorders. Blood NfL measurement has been an exciting and active field of research in idiopathic Parkinson disease (PD) and atypical parkinsonisms. However, blood NfL levels in these parkinsonisms from existing literature were inconsistent. No comprehensive meta-analysis has ever been conducted.
Methods:
Three major biomedical electronic databases PubMed, Embase, and Web of Science were comprehensively searched from inception to July 10, 2020. This protocol will be prepared based on the guidelines recommended by the statement of Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P). Original observational studies that measured blood (serum/plasma) NfL concentrations in patients with parkinsonisms (multiple system atrophy [MSA], progressive supranuclear palsy [PSP], corticobasal syndrome [CBS], and dementia with Lewy bodies [DLB]), and healthy controls (HCs) will be included. Quality assessment of the included studies will be performed using the Newcastle Ottawa Scale (NOS). Meta-analyses will be conducted using the STATA software version 13.0. The standardized mean differences as the measure of effect size and 95% confidence intervals were calculated for each comparison of blood NfL levels. Heterogeneity analysis, sensitivity analysis, publication bias, subgroup analysis, and meta-regression analysis will be carried out to test the robustness of the results.
Results:
The meta-analysis will obtain the effect sizes of blood NfL levels in the following comparisons: PD versus HC, MSA versus HC, PSP versus HC, CBS versus HC, DLB versus HC, MSA versus PD, PSP versus PD, CBS versus PD, and DLB versus PD.
Conclusions:
The present meta-analysis will provide the quantitative evidence of NfL levels in idiopathic PD and atypical parkinsonisms, hoping to facilitate differential diagnoses in clinical practice.
Registration number:
INPLASY202070091.
Keywords: blood, meta-analysis, neurofilament light chain, Parkinson disease, parkinsonism
1. Introduction
Parkinsonism is a neurological syndrome characterized by bradykinesia, tremor, rigidity, and postural instability, referring to a group of neurodegenerative disorders with considerable overlap in symptoms but with heterogeneity in presentation and pathology.[1,2,3] The most common cause of parkinsonism is idiopathic Parkinson disease (PD) that presents typical asymmetrical motor symptoms with slow progression and marked and sustained response to dopaminergic treatment.[4,5] Unlike idiopathic PD, atypical parkinsonisms, including multiple system atrophy (MSA), progressive supranuclear palsy (PSP), corticobasal syndrome (CBS), and dementia with Lewy bodies (DLB), show additional clinical signs like gaze palsy, apraxia, ataxia, early cognitive decline, and dysautonomia.[1,2,6] These atypical parkinsonisms generally progress more rapidly with poorer prognosis and poorer response to dopaminergic therapy than idiopathic PD.[1,2,7] Correct diagnoses of parkinsonian disorders are important for patient counseling, prognostic assessment, and therapeutic implications, but also research purposes. However, their differential diagnoses on clinical grounds remain challenging particularly in early disease stages.[2,5,8] Sustained efforts have been made to develop reliable biomarkers to aid their accurate diagnoses.[2,9,10,11,12,13,14,15]
Neurofilament light chain (NfL) is among the most promising candidate biomarkers of neuroaxonal injury irrespective of the underlying cause and has been extensively investigated in neurodegenerative diseases.[16,17,18,19,20,21] Recent meta-analyses have shown that cerebrospinal fluid (CSF) NfL levels were increased significantly in PSP,[16] MSA,[16] and DLB.[17] By contrast, CSF NfL levels were not increased in idiopathic PD.[16] CSF levels of NfL have shown the potential value in the discrimination of idiopathic PD from atypical parkinsonisms.[22,23,24,25] CSF and blood NfL levels are highly correlated that is related to neurodegeneration.[26,27,28] Compared to CSF that needs to perform a lumbar puncture, blood (serum/plasma) is an easier and more rapidly accessible biospecimen with relatively limited restrictions in clinical practice. With the development of ultrasensitive assay technologies in recent years, a growing number of studies have moved to investigate blood (serum/plasma) NfL levels in idiopathic PD and atypical parkinsonisms. Atypical parkinsonisms commonly showed increased blood NfL levels.[27,28,29,30] However, the degree of elevation varied considerably between these disorders. Besides, blood NfL levels in idiopathic PD were inconsistent across studies.[26,27,28,29,30,31,32] A meta-analysis is needed to quantitatively pool individual small studies to improve the power to detect differences. Thus, we performed a meta-analysis of available studies that analyzed blood (serum/plasma) NfL levels in idiopathic PD and atypical parkinsonisms. We will compare differences of blood (serum/plasma) NfL levels between patients with idiopathic PD and healthy controls (HCs), between patients with atypical parkinsonism subtypes and HCs, and between patients with idiopathic PD and atypical parkinsonism subtypes.
2. Methods
2.1. Search strategies
Three major biomedical electronic databases PubMed, Embase, and Web of Science were comprehensively searched from inception to July 10, 2020. The following search terms were used: (neurofilament OR (neurofilament light chain) OR nfl) AND ((Parkinson disease) OR parkinsonism OR Parkinson∗ OR (atypical parkinsonian disorders) OR (multiple system atrophy) OR (progressive supranuclear palsy) OR (Steele-Richardson-Olszewski syndrome) OR (corticobasal syndrome) OR (corticobasal degeneration) OR (dementia with Lewy bodies) OR (Lewy body dementia)) AND (blood OR serum OR plasma). Additionally, references of eligible articles and relevant systematic reviews/meta-analyses will be hand-searched.
This protocol will be prepared based on the guidelines recommended by the statement of Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P).[33]
2.2. Eligibility criteria
2.2.1. Inclusion criteria
Studies will be included if they: were original observational studies (including case-control, cohort, and cross-sectional studies) in English; included patients with idiopathic PD and atypical parkinsonisms (MSA, PSP, DLB, and CBS) according to the established diagnostic criteria; measured blood (serum/plasma) NfL concentrations in patients with parkinsonisms and HCs; provided sufficient information for meta-analysis (number of participants and mean and standard deviation [SD] for blood NfL levels for each group). If some data were not eligible, they will be transformed from available data or will be obtained using graph-based data mining methods.
2.2.2. Exclusion criteria
The following exclusion criteria will be applied: studies were in the form of reviews, letters, editorials, conference abstracts, animal research, case reports, and protocols; studies enrolled repetitive patient samples or were overlapped with another study with a larger sample size. In case of longitudinal studies, we will only extract baseline data for analysis.
The flowchart of study selection following the PRISMA statement[34] is presented in Figure 1.
Figure 1.
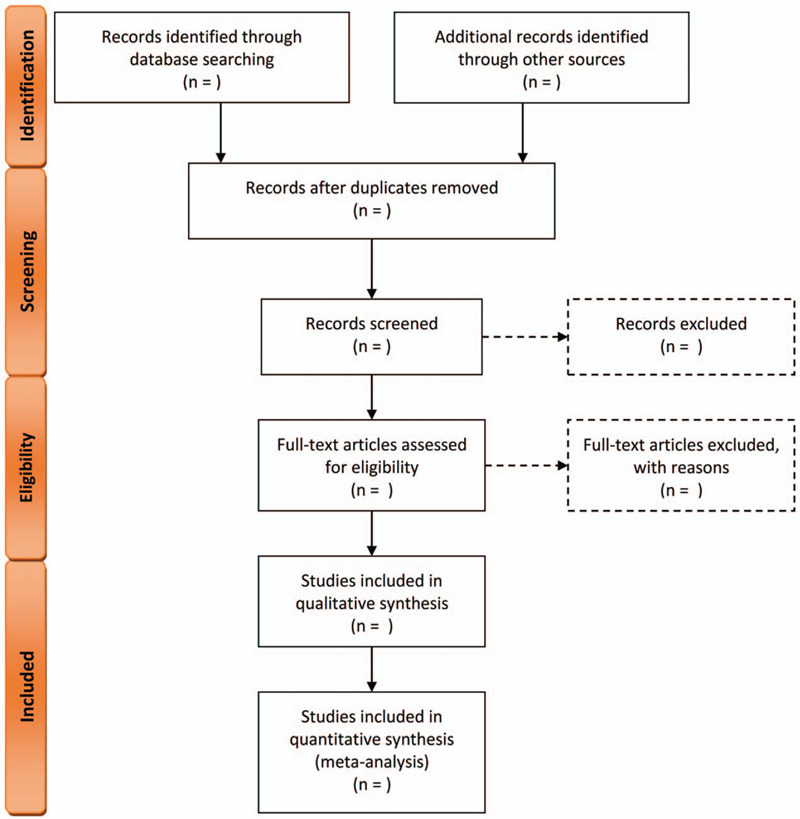
The flowchart of study selection following the PRISMA statement. PRISMA = Preferred Reporting Items for Systematic Review and Meta-Analysis.
2.3. Data extraction
Data from eligible studies will be extracted using a standardized spreadsheet, including the following information: the first author's surname, year of publication, type of parkinsonisms, the numbers of patients and healthy controls, age, gender distribution, the mean and SD values of the blood NfL levels of each group, NfL analysis methods, analysis kit brand, disease duration, Hoehn and Yahr (H-Y) scale, Unified Parkinson's Disease Rating Scale, part III (UPDRS-III) score, and Mini-Mental State Examination (MMSE) score.
2.4. Quality assessment
Quality assessment of the included studies will be performed using the Newcastle Ottawa Scale (NOS).[35] This scale includes 3 main fields of selection (0–4 scores), comparability (0–3 scores), and exposure (0–3 scores). The NOS score lower than 6 scores will be considered a low-quality methodology.
2.5. Data synthesis and statistics
Meta-analyses will be conducted using the STATA software version 13.0 (StataCorp, College Station, TX). The standardized mean differences (SMD) as the measure of effect size and 95% confidence intervals (CI) were calculated of each comparison of blood NfL levels (PD vs HC, MSA vs HC, PSP vs HC, CBS vs HC, DLB vs HC, MSA vs PD, PSP vs PD, CBS vs PD, and DLB vs PD). Study heterogeneity will be estimated with the I2 statistic. A fixed-effects model will be used if there was no obvious statistical heterogeneity with I2 less than 50%; otherwise, the random-effects model will be selected. I2 < 50%, between 50% and 75%, and I2 > 75% will be deemed as low, moderate, and high heterogeneity, respectively.
To examine whether overall results were influenced by a single study, sensitivity analyses will be performed. A funnel plot will be created and Egger test will be analyzed to test the potential publication bias. Subgroup analyses and meta-regression analyses will be conducted to examine whether potential moderators influence the meta-analysis effect sizes. Meta-regression analyses will be only performed when relevant data were available from more than 10 studies.
Study selection, quality assessment, and data extraction will be performed by one author and verified by another.
2.6. Ethics and dissemination
Ethics Committee approval was waived because this meta-analysis will be performed using the data from published studies that will not involve any human participants or animals. Once the meta-analyses are complete, it will be published in conferences or a peer-reviewed journal.
3. Discussion
NfL is a promising diagnostic and prognostic fluid biomarker with high translational value in many neurological disorders.[36,37,38] Due to its convenience and lesser invasiveness in clinical practice, blood NfL measurement has been an exciting and active field of research.[36,39] Idiopathic PD and atypical parkinsonisms are different in the clinical course, prognosis, and therapy needs. Recent studies have shown that blood NfL levels added to their differential diagnoses. [27,40] However, previous studies on NfL levels in idiopathic PD and atypical parkinsonisms were inconsistent. The meta-analysis will obtain the effect sizes of blood NfL levels in the following comparisons: PD versus HC, MSA versus HC, PSP versus HC, CBS versus HC, DLB versus HC, MSA versus PD, PSP versus PD, CBS versus PD, and DLB versus PD. The present meta-analysis will provide quantitative evidence of NfL levels in these disorders, hoping to facilitate differential diagnoses in clinical practice.
Author contributions
Conceptualization: HongZhou Wang, LiJian Han, PingLei Pan
Data curation: HongZhou Wang, WanHua Wang
Formal analysis: HongZhou Wang
Funding acquisition: PingLei Pan
Investigation: HongZhou Wang, WanHua Wang, HaiCun Shi
Methodology: HongZhou Wang, WanHua Wang, HaiCun Shi
Project administration: LiJian Han, PingLei Pan
Resources: HongZhou Wang, WanHua Wang, HaiCun Shi
Software: HongZhou Wang, WanHua Wang
Supervision: LiJian Han
Validation: PingLei Pan
Visualization: HongZhou Wang, WanHua Wang
Writing – original draft: HongZhou Wang, WanHua Wang
Writing – review & editing: LiJian Han, PingLei Pan
Footnotes
Abbreviations: CBS = corticobasal syndrome, CI = confidence intervals, CSF = cerebrospinal fluid, DLB = dementia with Lewy bodies, HCs = healthy controls, MMSE = Mini-Mental State Examination, MSA = multiple system atrophy, NfL= neurofilament light chain, PD = Parkinson disease, PRISMA-P = Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols, PSP = progressive supranuclear palsy, SD = standard deviation, SMD = standardized mean differences, UPDRS-III = Unified Parkinson's Disease Rating Scale, part III.
How to cite this article: Wang H, Wang W, Shi H, Han L, Pan P. Blood neurofilament light chain in Parkinson disease and atypical parkinsonisms: A protocol for systematic review and meta-analysis. Medicine. 2020;99:40(e21871).
HZWang and WHW contributed equally to this work.
This work was supported by the National Natural Science Foundation of China (81601161).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Bhidayasiri R, Rattanachaisit W, Phokaewvarangkul O, et al. Exploring bedside clinical features of parkinsonism: a focus on differential diagnosis. Parkinsonism Relat Disord 2019;59:74–81. [DOI] [PubMed] [Google Scholar]
- [2].Deutschlander AB, Ross OA, Dickson DW, et al. Atypical parkinsonian syndromes: a general neurologist's perspective. Eur J Neurol 2018;25:41–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Respondek G, Stamelou M, Hoglinger GU. Classification of atypical parkinsonism per pathology versus phenotype. Int Rev Neurobiol 2019;149:37–47. [DOI] [PubMed] [Google Scholar]
- [4].Kalia LV, Lang AE. Parkinson's disease. Lancet 2015;386:896–912. [DOI] [PubMed] [Google Scholar]
- [5].Rizzo G, Copetti M, Arcuti S, et al. Accuracy of clinical diagnosis of Parkinson disease: a systematic review and meta-analysis. Neurology 2016;86:566–76. [DOI] [PubMed] [Google Scholar]
- [6].Armstrong MJ, McFarland N. Recognizing and treating atypical Parkinson disorders. Handb Clin Neurol 2019;167:301–20. [DOI] [PubMed] [Google Scholar]
- [7].Glasmacher SA, Leigh PN, Saha RA. Predictors of survival in progressive supranuclear palsy and multiple system atrophy: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 2017;88:402–11. [DOI] [PubMed] [Google Scholar]
- [8].Tolosa E, Wenning G, Poewe W. The diagnosis of Parkinson's disease. Lancet Neurol 2006;5:75–86. [DOI] [PubMed] [Google Scholar]
- [9].Parnetti L, Gaetani L, Eusebi P, et al. CSF and blood biomarkers for Parkinson's disease. Lancet Neurol 2019;18:573–86. [DOI] [PubMed] [Google Scholar]
- [10].Filippi M, Sarasso E, Agosta F. Resting-state Functional MRI in Parkinsonian Syndromes. Mov Disord Clin Pract 2019;6:104–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ramaswamy P, Christopher R, Pal PK, et al. MicroRNAs to differentiate Parkinsonian disorders: advances in biomarkers and therapeutics. J Neurol Sci 2018;394:26–37. [DOI] [PubMed] [Google Scholar]
- [12].Buchert R, Buhmann C, Apostolova I, et al. Nuclear imaging in the diagnosis of clinically uncertain parkinsonian syndromes. Dtsch Arztebl Int 2019;116:747–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Saeed U, Compagnone J, Aviv RI, et al. Imaging biomarkers in Parkinson's disease and Parkinsonian syndromes: current and emerging concepts. Transl Neurodegener 2017;6:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Strafella AP, Bohnen NI, Perlmutter JS, et al. Molecular imaging to track Parkinson's disease and atypical parkinsonisms: new imaging frontiers. Mov Disord 2017;32:181–92. [DOI] [PubMed] [Google Scholar]
- [15].Hoglinger GU, Kassubek J, Csoti I, et al. Differentiation of atypical Parkinson syndromes. J Neural Transm (Vienna) 2017;124:997–1004. [DOI] [PubMed] [Google Scholar]
- [16].Wang SY, Chen W, Xu W, et al. Neurofilament light chain in cerebrospinal fluid and blood as a biomarker for neurodegenerative diseases: a systematic review and meta-analysis. J Alzheimers Dis 2019;72:1353–61. [DOI] [PubMed] [Google Scholar]
- [17].Zhao Y, Xin Y, Meng S, et al. Neurofilament light chain protein in neurodegenerative dementia: a systematic review and network meta-analysis. Neurosci Biobehav Rev 2019;102:123–38. [DOI] [PubMed] [Google Scholar]
- [18].Karantali E, Kazis D, Chatzikonstantinou S, et al. The role of neurofilament light chain in frontotemporal dementia: a meta-analysis. Aging Clin Exp Res 2020;Online ahead of print. [DOI] [PubMed] [Google Scholar]
- [19].Li D, Shen D, Tai H, et al. Neurofilaments in CSF as diagnostic biomarkers in motor neuron disease: a meta-analysis. Front Aging Neurosci 2016;8:290.1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Xu Z, Henderson RD, David M, et al. Neurofilaments as biomarkers for amyotrophic lateral sclerosis: a systematic review and meta-analysis. PLoS One 2016;11:e0164625.1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Forgrave LM, Ma M, Best JR, et al. The diagnostic performance of neurofilament light chain in CSF and blood for Alzheimer's disease, frontotemporal dementia, and amyotrophic lateral sclerosis: a systematic review and meta-analysis. Alzheimers Dement (Amst) 2019;11:730–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Cong S, Xiang C, Wang H, et al. Diagnostic utility of fluid biomarkers in multiple system atrophy: a systematic review and meta-analysis. J Neurol 2020;Online ahead of print. [DOI] [PubMed] [Google Scholar]
- [23].Ge F, Ding J, Liu Y, et al. Cerebrospinal fluid NFL in the differential diagnosis of parkinsonian disorders: a meta-analysis. Neurosci Lett 2018;685:35–41. [DOI] [PubMed] [Google Scholar]
- [24].Hu X, Yang Y, Gong D. Cerebrospinal fluid levels of neurofilament light chain in multiple system atrophy relative to Parkinson's disease: a meta-analysis. Neurol Sci 2017;38:407–14. [DOI] [PubMed] [Google Scholar]
- [25].Sako W, Murakami N, Izumi Y, et al. Neurofilament light chain level in cerebrospinal fluid can differentiate Parkinson's disease from atypical parkinsonism: evidence from a meta-analysis. J Neurol Sci 2015;352:84–7. [DOI] [PubMed] [Google Scholar]
- [26].Oosterveld LP, Verberk IMW, Majbour NK, et al. CSF or serum neurofilament light added to alpha-Synuclein panel discriminates Parkinson's from controls. Mov Disord 2020;35:288–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Marques TM, van Rumund A, Oeckl P, et al. Serum NFL discriminates Parkinson disease from atypical parkinsonisms. Neurology 2019;92:e1479–86. [DOI] [PubMed] [Google Scholar]
- [28].Hansson O, Janelidze S, Hall S, et al. Blood-based NfL: a biomarker for differential diagnosis of parkinsonian disorder. Neurology 2017;88:930–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Gagliardi D, Meneri M, Saccomanno D, et al. Diagnostic and prognostic role of blood and cerebrospinal fluid and blood neurofilaments in amyotrophic lateral sclerosis: a review of the literature. Int J Mol Sci 2019;20:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Jabbari E, Holland N, Chelban V, et al. Diagnosis across the spectrum of progressive supranuclear palsy and corticobasal syndrome. JAMA Neurol 2020;77:377–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Sampedro F, Perez-Gonzalez R, Martinez-Horta S, et al. Serum neurofilament light chain levels reflect cortical neurodegeneration in de novo Parkinson's disease. Parkinsonism Relat Disord 2020;74:43–9. [DOI] [PubMed] [Google Scholar]
- [32].Lin YS, Lee WJ, Wang SJ, et al. Levels of plasma neurofilament light chain and cognitive function in patients with Alzheimer or Parkinson disease. Sci Rep 2018;8:17368.1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647.1–25. [DOI] [PubMed] [Google Scholar]
- [34].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097.1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Ottawa: The Ottawa Hospital Research Institute; 2009. [Google Scholar]
- [36].Alirezaei Z, Pourhanifeh MH, Borran S, et al. Neurofilament light chain as a biomarker, and correlation with magnetic resonance imaging in diagnosis of CNS-related disorders. Mol Neurobiol 2020;57:469–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Gafson AR, Barthélemy NR, Bomont P, et al. Neurofilaments: neurobiological foundations for biomarker applications. Brain 2020;143:1975–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Loeffler T, Schilcher I, Flunkert S, et al. Neurofilament-light chain as biomarker of neurodegenerative and rare diseases with high translational value. Front Neurosci 2020;14:579.1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Mariotto S, Sechi E, Ferrari S. Serum neurofilament light chain studies in neurological disorders, hints for interpretation. J Neurol Sci 2020;416:116986.1–3. [DOI] [PubMed] [Google Scholar]
- [40].Mangesius S, Mariotto S, Ferrari S, et al. Novel decision algorithm to discriminate parkinsonism with combined blood and imaging biomarkers. Parkinsonism Relat Disord 2020;77:57–63. [DOI] [PubMed] [Google Scholar]


