Abstract
Human immunodeficiency virus (HIV) supresses immune system, primarily cell-mediated immunity. Cluster of differentiation 4 (CD4) cell count, viral load, and oral lesions are the most important laboratory parameters to evaluate the evolution of acquired immunodeficiency syndrome. The present study aims to determine the incidence of HIV-related oral lesions with CD4 cell count and viral load in Yunnan, China.
A cross-sectional study was conducted from December 2007 to December 2009, in 1812 HIV positive patients from Department of Infectious Diseases in Kunming Third People's Hospital. CD4, CD8, and viral load data were collected and analyzed statistically using SPSS 11.3.
Out of 1812 HIV positive patients, 929 (51.27%) were associated with 1 or more oral lesions. The most common oral lesions observed were Candida Pseudomembranous (13.75%), Candida erythematous (10.93%), Oral hairy leukoplakia (7.95%), Aphthous ulcer (6.18%), Herpes simplex infection (5.58%). In most patients with oral lesions, the CD4 cell count was < 200/μL. The incidence of oral lesions was lower when CD4 count was > 200/μL and with undetectable (P < .01) HIV viral load. Almost no oral lesions was observed when CD4 count > 500/μL (P < .01). With highly active antiretroviral therapy, reduction in HIV-related oral lesions was observed especially in Candida erythematous, Candida Pseudomembranous, Oral hairy leukoplakia, and Aphthous ulcer.
The higher incidence of oral lesions with lower CD4 count (<200/μL) in HIV-infected patients indicated importance of CD4 cell count in identifying disease progression.
Keywords: CD4, highly active antiretroviral therapy (HAART), HIV-viral load, human immunodeficiency virus (HIV), oral lesions
1. Introduction
Acquired immunodeficiency syndrome (AIDS) is caused by a retrovirus known as human immunodeficiency virus (HIV) which breaks down the body's immune system leaving a complex of symptoms, neurological disorders, unusual malignancies, and infections.[1]
HIV is a global pandemic disease affecting around 37.9 million people around the world.[2] Two major targets of HIV infection are the central nervous system and the immune system. Profound immunosuppression, primarily affecting the cell-mediated immunity, is the hallmark of HIV. It has a specific affinity for cluster of differentiation 4 (CD4) T cells[3] with at least 1 manifestation in the head and neck area,[4] such as oral lesions.[5] CD4 cell count, viral load, and oral lesions are significant predictive markers of severe immunosuppression and disease progression because they may represent the early signs of the disease.[6]
Oral manifestations such as Kaposi's sarcoma (KS), oral candidiasis, and oral hairy leukoplakia (OHL) were reported to have high incidence in HIV-positive patients.[7] For oral diseases described in HIV-positive patients, 3 main groups were established: Group 1: lesions seen (occasionally) in HIV infection and exhibiting a potential association; Group 2: lesions less commonly associated with HIV infection; and Group 3: lesions strongly associated with HIV infection. These oral lesions may lead to compromised facial appearance, difficulty in eating, inability to swallow, discomfort, and considerable pain. Apart from their diagnostic importance, oral manifestations may be of prognostic importance and also serves as clinical correlates with viral load and CD4 cell counts.[8] Early management of these oral lesions will improve the overall quality of life in HIV-infected patients.
Several studies have reported strong correlation between the laboratory parameters (viral load and CD4 cell count) and oral lesions prevalence in HIV-positive patients.[9,10] Recent studies reported high incidence of oral lesions with increased viral load and low CD4 cell count.[11]
The introduction and recommendation of treatment for HIV infection in the form of antiretroviral therapy—especially as combination therapy, commonly known as highly active antiretroviral therapy (HAART)—has changed the disease progression drastically. HAART regimen is a combination of at least 3 antiviral drugs: 2 nucleoside reverse transcriptase inhibitors (NRTIs) with either a protease inhibitor or a non-nucleoside reverse transcriptase inhibitors (NNRTI). Studies have emphasized decrease in viral load and oral lesions with an increase in CD4 count in HIV-positive patients under HAART with time.[12,13]
Hence CD4 cell count, viral load, and oral lesions are the most important laboratory parameters to evaluate the evolution of AIDS. The aim of the present study is to determine the relation between CD4 cell count and viral load on oral lesions in Chinese HIV-infected and AIDS patients.
2. Methods
2.1. Study population and design
This cross-sectional study was conducted in HIV-positive patients hospitalized between December 2007 to December 2009 in Kunming Third People's Hospital Infection Division/Kunming AIDS Clinical Diagnosis and Treatment Centre. The study was approved by the Medical Ethics Committee of Kunming Third People's Hospital and informed consent was obtained from the participants.
2.2. Inclusion and exclusion criteria
HIV-positive patients confirmed by HIV antibody test, hospitalized from December 2007 to December 2009, were included. All cases were confirmed by HIV antibody test in Yunnan Province or prefecture Centres for Disease Control and Prevention (CDC).
2.3. HIV antibody detection
The detection of HIV antibody was done in 2 steps: primary screening using Enzyme linked immunosorbent assay and confirmation test by Western-Blot. The diagnostic criteria for HIV infection was considered based on 2001 China Standard.
2.4. Assessment of oral lesions
The classification and diagnosis of oral lesions was based on WHO (1993) standards. Four dentists participated in diagnosis. The diagnosis was done under natural light or the light source of the dental chair using instruments like mouth glasses, tweezers, probes, and tongue depressors. The pathological diagnosis was made for the lesions observed as far as possible.
2.5. Laboratory procedures
2.5.1. T cell subsets count
CD4 and CD8 T lymphocyte cell count was done using the FACSCalibur flow cytometer (BD Company, Franklin Lakes, NJ, USA). CD4 T lymphocyte count was done 3 months before and after oral examination.
2.5.2. HIV-1 RNA viral load determination
The viral load was estimated using bDNA (branched DNA) assay. The results were expressed as copies/mL of virus nucleic acid detected in every milliliter of blood. The detection limit was 50 copies/mL (log 1.7 copies/mL).
2.6. HAART usage plan
HAART was used for more than 3 months in 417 patients, including 295 males and 122 females. HAART was given in 2 schemes.
One NNRTI and 2 NRTI: Efeveren 600 mg, once a day or nevirapine 200 mg, twice a day + lamivudine 300 mg, once a day + zidovudine 300 mg, twice a day or stavudine 15 mg, twice a day or dehydroxyl glycoside 125 mg, twice a day.
One PI and 2 NRTIs: Indinavir 800 mg, once every 8 hours + lamivudine 300 mg, once a day + zidovudine 300 mg, twice a day or stavudine 15 mg, twice a day.
2.7. Statistical analysis
Descriptive variables were expressed as mean ± standard deviation. Logistic regression analysis (univariate and multivariate) was used to analyze the influence of factors like transmission routes, CD4, age, sex and education on oral lesions. Presence of oral lesion was the predictive variable in the study. Statistical analysis was carried out with SPSS11.3 software package.
3. Results
3.1. Study population epidemiology
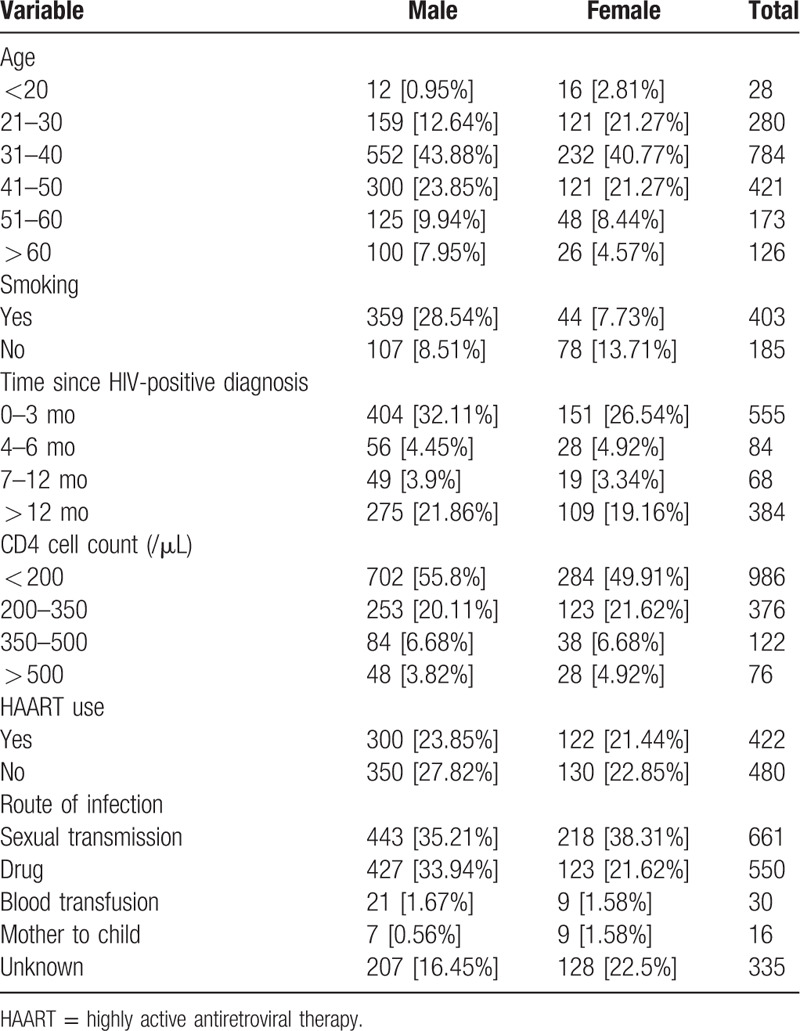
A total of 1812 HIV-positive patients from 10 regions in Yunnan Province were included in the study. The baseline characteristics of study patients included is presented in Table 1. The education level of 62.9% of HIV-positive patients included was junior high school and below.
Table 1.
Population epidemiology.
3.2. Characteristics of oral lesions
Among the 1812 patients, 929 (51.27%) had HIV-related oral lesions, of which 648 (69.75%) were males and 281 (30.25%) were females. During the study, 21 different types of oral lesions were monitored, of which 7 lesions were found to be most common. An average of 0.72 lesions was observed in each patient. No cases of necrotizing ulcerative gingivitis or necrotizing ulcerative periodontitis were observed in this study. The incidence of 1 or 2 oral lesions was found to be high accounting for 92.78% (862/929). Only 1 patient had more than 5 kinds of oral lesions.
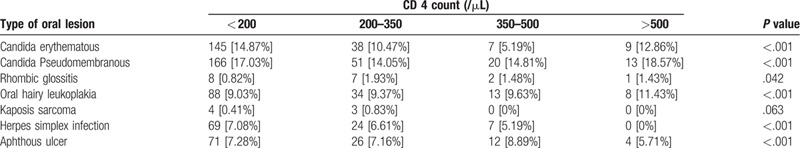
3.3. Oral lesions and CD4 cell count
Regardless of HAART, 1545 HIV-positive patients had CD4 T lymphocyte data. Based on CD4 T lymphocyte count, the patients were divided into 4 groups: <200/μL, 200 to 350/μL, 351 to 500/μL, and >500/μL. It was observed that CD4 count of 50.42% patients was below 350/μL, and for 56.52% patients, it was below 200/μL.
The highest incidence of oral lesions was seen when CD4 count < 200/μL, indicating lower the CD4 count, higher the incidence of oral lesions. The incidence of 7 common HIV-related oral lesions categorized as per CD4 cell count is presented in Table 2. The relationship between oral lesions except Kaposi sarcoma and CD4 count was found to be significant (P < .05).
Table 2.
Oral lesions and CD4 cell count.
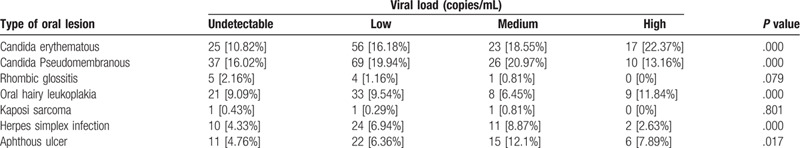
3.4. Oral lesions and viral load
Regardless of HAART, 448 patients were monitored for viral load. Based on viral load, the patients were divided into 4 groups: undetectable, low, medium, and high. The relationship between viral load and the occurrence of 7 kinds of oral lesions has been described in Table 3. Except for Candida erythematous and oral hairy leukopenia, the incidence of other oral lesions was low with high viral load. From the P value, the relationship between all types of oral lesions and viral load except for Kaposi sarcoma [0.801] and Rhombic glossitis [0.079] was found to be significant (P < .05).
Table 3.
Oral lesions and viral load.
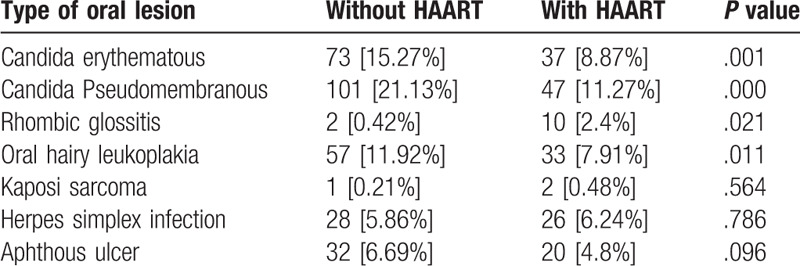
3.5. Oral lesions and HAART
The incidence of 7 kinds of oral lesions between patients with HAART and without HAART was observed and compared (Table 4). From the results, incidence of oral lesions was found to decrease with HAART except for Rhombic glossitis, Kaposi sarcoma, and Herpes simplex infection. The results indicated that oral lesions were significantly influenced by therapy, except for Kaposi sarcoma, Herpes simplex infection, and Aphthous ulcer.
Table 4.
Incidence of oral lesions and mean CD4 cell count with HAART.
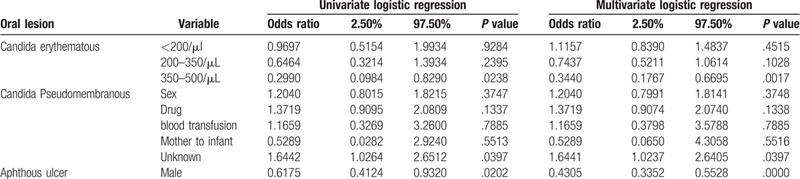
3.6. Factors affecting oral lesions
Multivariate logistic regression was used to analyze the influence of transmission routes, CD4 count, age, sex, and education on oral lesions (Table 5). It was observed that Candida erythematous was influenced by CD4 count (351–500 μL) with an odds ratio (OR) of 0.34 whereas Candida pseudomembranous was dependent on route of transmission (unknown) with an OR of 1.64 and aphthous ulcer by gender (male), OR of 0.43.
Table 5.
Factors affecting oral lesions.
4. Discussion
Oral manifestations, the earliest and most important indicators of HIV infection, are seen in 50% of HIV-infected patients[14,15] and about 80% of them will be due to acquired immunodeficiency.[16] The present study assessed the prevalence of oral lesions and their association with CD4 count and HIV viral load. From our results, Candida pseudomembranous (13.75%) was found to be more prevalent, followed by Candida erythematous (10.93%), OHL (7.95%), oral aphthous ulcer (6.18%) which was in accordance with literature.[17,18] It is noteworthy to mention that even in current times, Candida albicans is still the most prevalent condition in HIV patients.[19]
Among all oral lesions, the incidence of oral candidiasis was reported to be highest with 11% to 81% in developing countries,[10,20,21] 5% to 92% in the United States,[22] and 20.6% to 56% in China.[17] With oral candidiasis, there is continuous decline in CD4 count and rapid increase in viral load.[23] In contrary to this, some studies reported no association between oral candidiasis and CD4 cell count or viral load.[24,25] Flanagan et al[26] reported a negative relationship between CD4 count and oral lesions but not with viral load. However, we observed that CD4 count negatively correlated with incidence of oral lesions whereas a definitive relationship was not observed between viral load and incidence of oral lesions.
According to the classification and diagnostic criteria of dental characterization of AIDS developed by the WHO Collaborative Centre for Oral Representation of AIDS Infection in 1992, among 1812 HIV-positive patients, 929 (51.27%) had some type of oral lesions with total of 1306 lesions. Lower proportion of Rhombic glossitis and KS was seen in this study which may be related to route of HIV infection in patients included or may be attributed ethnic differences or may be region of lesion considered. KS, characteristic to HIV infection[27,28] was observed in 7 patients, contrary to other reports.[20] However, KS cases were not reported in a study from China,[9] Nigeria,[29] and Brazil[30] which agrees with the current data.
In the present study, 14 (0.77%) patients were found to have linear gingival erythema, which was in agreement with earlier studies.[31] Acute necrotizing ulcerative gingivitis and periodontitis can sometimes develop into necrotizing stomatitis which is one of the most serious oral infections in HIV patients.[32] In our study, 3 cases (0.17%) of necrotizing stomatitis were observed.
Even though no specific CD4 threshold is associated with oral lesions in immunological diseases like HIV, a decline in CD4 count was reported. For example, immunological diseases like major histocompatibility complex, class II deficiency, hyper IgM syndrome lead to decrease in CD4 count and increase in incidence of candidiasis, hepatic infections, and oral ulcerations.[33,34,35] Similarly, HIV invades mainly human immune cells such as CD4 cells, CD8 cells, monocytes, macrophages thereby compromising the cellular and humoral immune functions.[36] Owing to the fact that the loss of immune function is associated with declining CD4 counts, the CDC has proposed that a patient with lowest count to be associated with severe immune suppression, signifying the progression to AIDS.[37] Additionally, incidence of oral ulcers in HIV patients destroys the integrity of mucosal membrane,[38] aiding fungal growth and causing imbalance in oral flora.[39] In agreement, higher incidence of HIV-related oral lesions was observed when CD4 cell count is < 200/μL in current study. These results support the use of CD4 cell count as an indicator of HIV-related oral lesions and predictor of disease progression. From the results of multivariate analysis, Candida erythematous was found to be influenced by CD4 cell count which was in accordance with previous literature.[40]
Decrease in the occurrence of oral lesions in patients under HAART has been well documented.[41,42] Even in the present study, HIV-related oral lesions reduced with HAART. Additionally, HAART is also efficient in significantly reducing Candida erythematous, Candida Pseudomembranous, OHL, and aphthous ulcer. However, no significant difference was observed in case of Rhombic glossitis, KS, and Herpes simplex infection. Although HAART helps in controlling opportunistic infections like oral lesions, persistent systemic lymphadenopathy, infectious soft warts and KS, complete restoration of immune function is not achieved as it cannot completely eradicate the virus. In the current study, it was observed that increase in CD4 count was not consistent with inhibition of virus in patients under HAART. We observed enhanced immune function and clinical symptoms even with high HIV viral load in few cases, whereas even with nondetectable viral load, CD4 count was low with higher prevalence of HIV-related oral lesions. These observations suggest that CD4 count is more important in prediction of disease progression.
The merit of the present study is the relatively large number of study population considered. To our knowledge this is the first study in China assessing both CD4 cell count and viral load in the incidence of HIV-related oral lesions. However, the fact that the study was conducted only in Yunnan Province limits the extrapolation of results and its generalization.
5. Conclusion
The results of the study suggest that CD4 cell count can be used as an indicator for predicting and managing oral lesions in HIV patients. Given that with HAART, the incidence of HIV-related oral lesions decreased, timely initiation of HAART therapy will help in preventing oral lesions and delay opportunistic infections in HIV patients.
Author contributions
Conceptualization: Wen Shu, Kaiwen Duan.
Data curation: Wen Shu, Chengwen Li, Fei Du, Jinsong Bai, Kaiwen Duan.
Funding acquisition: Kaiwen Duan.
Methodology: Wen Shu, Chengwen Li, Fei Du, Jinsong Bai, Kaiwen Duan.
Supervision: Kaiwen Duan.
Writing – original draft: Wen Shu, Chengwen Li, Fei Du, Jinsong Bai, Kaiwen Duan.
Writing – review & editing: Wen Shu, Chengwen Li, Fei Du, Jinsong Bai, Kaiwen Duan.
Footnotes
Abbreviations: AIDS = acquired immunodeficiency syndrome, bDNA = branched DNA, CD4 = cluster of differentiation 4, CD8 = cluster of differentiation 8, CDC = centres for disease control and prevention, HAART = highly active antiretroviral therapy, HIV = human immunodeficiency virus, KS = Kaposi Sarcoma, NNRTIs = non-nucleoside reverse transcriptase inhibitors, NRTIs = nucleoside reverse transcriptase inhibitors, OC = oral candidiasis, OR = odds ratio, OHL = oral hairy leukoplakia, PI = protease inhibitor.
How to cite this article: Shu W, Li C, Du F, Bai J, Duan K. A Real World, Cross Sectional Study of Oral Lesions and their Association with CD4 Cell Counts and HIV Viral Load in Yunnan, China. Medicine. 2020;99:40(e22416).
All authors contributed to data analysis, drafting, or revising the article, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
This study was supported by grants from National Natural Science Foundation of China (grant No. 30860315, 81160135).
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors have no conflicts of interest to disclose.
References
- [1].Khiangte L, Vidyabati RK, Singh MK, et al. A study of serum lipid profile in human immunodeficiency virus (HIV) infected patients. J Indian Acad Clin Med 2007;8:307–11. [Google Scholar]
- [2].Global Health Observatory (GHO) data [Internet]. https://www.who.int/gho/hiv/en/ (Last accessed on 5 February 2020). [Google Scholar]
- [3].Jindwani K, Singh K, Dadlani H. A study of oral lesions among H.I.V. positives in a tertiary care hospital. Biomed Res 2013;24:40–2. [Google Scholar]
- [4].Rosenberg RA, Schneider KL, Cohen NL. Head and neck presentations of acquired immunodeficiency syndrome. Otolaryngol Head Neck Surg 1985;93:700–5. [DOI] [PubMed] [Google Scholar]
- [5].Pinheiro A, Marcenes W, Zakrzewska JM, et al. Dental and oral lesions in HIV infected patients: a study in Brazil. Int Dent J 2004;54:131–7. [DOI] [PubMed] [Google Scholar]
- [6].Mellors JW, Muñoz A, Giorgi JV, et al. Plasma viral load and CD4 + lymphocytes as prognostic markers of HIV-1 infection. Ann Intern Med 1997;126:946–54. [DOI] [PubMed] [Google Scholar]
- [7].Sontakke SA, Umarji HR, Karjodkar F. Comparison of oral manifestations with CD4 count in HIV-infected patients. Indian J Dent Res 2011;22:732. [DOI] [PubMed] [Google Scholar]
- [8].Bravo IM, Correnti M, Escalona L, et al. Prevalence of oral lesions in HIV patients related to CD4 cell count and viral load in a Venezuelan population. Med Oral Patol Oral Cirugia Bucal 2006;11:E33–9. [PubMed] [Google Scholar]
- [9].Tsang PC, Samaranayake LP. Oral manifestations of HIV infection in a group of predominantly ethnic Chinese. J Oral Pathol Med 1999;28:122–7. [DOI] [PubMed] [Google Scholar]
- [10].Ranganathan K, Reddy BV, Kumarasamy N, et al. Oral lesions and conditions associated with human immunodeficiency virus infection in 300 south Indian patients. Oral Dis 2000;6:152–7. [DOI] [PubMed] [Google Scholar]
- [11].Ceballos-Salobreña A, Gaitán-Cepeda LA, Ceballos-Garcia L, et al. Oral lesions in HIV/AIDS patients undergoing highly active antiretroviral treatment including protease inhibitors: a new face of oral AIDS? AIDS Patient Care STDS 2000;14:627–35. [DOI] [PubMed] [Google Scholar]
- [12].Gaurav S, Keerthilatha PM, Archna N. Prevalence of oral manifestations and their association with CD4/CD8 ratio and HIV viral load in South India. Int J Dent 2011;2011:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Shetty S, Kattappagari K, Hallikeri K, et al. Evaluation of oral lesions in HIV seropositive individuals and its correlation with CD4 + T-lymphocytic count. J Dr NTR Univ Health Sci 2016;5:123–9. [Google Scholar]
- [14].Ponnam SR, Srivastava G, Theruru K. Oral manifestations of human immunodeficiency virus in children: an institutional study at highly active antiretroviral therapy centre in India. J Oral Maxillofac Pathol 2012;16:195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Bajpai S, Pazare AR. Oral manifestations of HIV. Contemp Clin Dent 2010;1:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Coogan MM, Greenspan J, Challacombe SJ. Oral lesions in infection with human immunodeficiency virus. Bull World Health Organ Sep 2005;83:700–6. [PMC free article] [PubMed] [Google Scholar]
- [17].Classification and diagnostic criteria for oral lesions in HIV infection EC-Clearinghouse on Oral Problems Related to HIV Infection and WHO Collaborating Centre on Oral Manifestations of the Immunodeficiency Virus. J Oral Pathol Med 1993;22:289–91. [PubMed] [Google Scholar]
- [18].MacPhail LA, Greenspan JS. Oral ulceration in HIV infection: investigation and pathogenesis. Oral Dis 1997;3: suppl 1: S190–3. [DOI] [PubMed] [Google Scholar]
- [19].Patil S, Majumdar B, Sarode SC, et al. Oropharyngeal candidosis in HIV-infected patients—an update. Front Microbiol 2018;9:980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Anil S, Challacombe SJ. Oral lesions of HIV and AIDS in Asia: an overview. Oral Dis 1997;3 suppl:S36–40. [DOI] [PubMed] [Google Scholar]
- [21].Itula PF, Mackenzie SB, Lewis K, et al. Orofacial manifestations and seroprevalence of HIV infection in Namibian dental patients. Oral Dis 1997;3 suppl:S51–3. [DOI] [PubMed] [Google Scholar]
- [22].Lamster IB, Begg MD, Mitchell-Lewis D, et al. Oral manifestations of HIV infection in homosexual men and intravenous drug users. Study design and relationship of epidemiologic, clinical, and immunologic parameters to oral lesions. Oral Surg Oral Med Oral Pathol 1994;78:163–74. [DOI] [PubMed] [Google Scholar]
- [23].Ramírez-Amador V, Esquivel-Pedraza L, Sierra-Madero J, et al. The changing clinical spectrum of human immunodeficiency virus (HIV)-related oral lesions in 1,000 consecutive patients: a 12-year study in a referral center in Mexico. Medicine (Baltimore) 2003;82:39–50. [DOI] [PubMed] [Google Scholar]
- [24].Liu X, Liu H, Guo Z, et al. Association of asymptomatic oral candidal carriage, oral candidiasis and CD4 + lymphocyte count in HIV-positive patients in China. Oral Dis 2006;12:41–4. [DOI] [PubMed] [Google Scholar]
- [25].Erköse G, Erturan Z. Oral Candida colonization of human immunodeficiency virus infected subjects in Turkey and its relation with viral load and CD4 + T-lymphocyte count. Mycoses 2007;50:485–90. [DOI] [PubMed] [Google Scholar]
- [26].Flanagan MA, Barasch A, Koenigsberg SR, et al. Prevalence of oral soft tissue lesions in HIV-infected minority children treated with highly active antiretroviral therapies. Pediatr Dent 2000;22:287–91. [PubMed] [Google Scholar]
- [27].Kua HW, Merchant W, Waugh MA. Oral Kaposi's sarcoma in a non-HIV homosexual White male. Int J STD AIDS 2004;15:775–7. [DOI] [PubMed] [Google Scholar]
- [28].Lynen L, Zolfo M, Huyst V, et al. Management of Kaposi's sarcoma in resource-limited settings in the era of HAART. AIDS Rev 2005;7:13–21. [PubMed] [Google Scholar]
- [29].Adedigba MA, Ogunbodede EO, Jeboda SO, et al. Patterns of oral manifestation of HIV/AIDS among 225 Nigerian patients. Oral Dis 2008;14:341–6. [DOI] [PubMed] [Google Scholar]
- [30].Pedreira EN, Cardoso CL, Barroso E, et al. Epidemiological and oral manifestations of HIV-positive patients in a specialized service in Brazil. J Appl Oral Sci 2008;16:369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Patton LL, Phelan JA, Ramos-Gomez FJ, et al. Prevalence and classification of HIV-associated oral lesions. Oral Dis 2002;8: suppl 2: 98–109. [DOI] [PubMed] [Google Scholar]
- [32].Folayan MO. The epidemiology, etiology, and pathophysiology of acute necrotizing ulcerative gingivitis associated with malnutrition. J Contemp Dent Pract 2004;5:28–41. [PubMed] [Google Scholar]
- [33].Notarangelo LD, Duse M, Ugazio AG. Immunodeficiency with hyper-IgM (HIM). Immunodefic Rev 1992;3:101–21. [PubMed] [Google Scholar]
- [34].Elhasid R, Etzioni A. Major histocompatibility complex class II deficiency: a clinical review. Blood Rev 1996;10:242–8. [DOI] [PubMed] [Google Scholar]
- [35].Atkinson JC, O’Connell A, Aframian D. Oral manifestations of primary immunological diseases. J Am Dent Assoc 2000;131:345–56. [DOI] [PubMed] [Google Scholar]
- [36].Février M, Dorgham K, Rebollo A. CD4 + T cell depletion in human immunodeficiency virus (HIV) infection: role of apoptosis. Viruses 2011;3:586–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Saini R. Oral lesions: a true clinical indicator in human immunodeficiency virus. J Nat Sci Biol Med 2011;2:145–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Heron SE, Elahi S. HIV infection and compromised mucosal immunity: oral manifestations and systemic inflammation. Front Immunol 2017;8:241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Martins N, Ferreira ICFR, Barros L, et al. Candidiasis: predisposing factors, prevention, diagnosis and alternative treatment. Mycopathologia 2014;177:223–40. [DOI] [PubMed] [Google Scholar]
- [40].Bodhade AS, Ganvir SM, Hazarey VK. Oral manifestations of HIV infection and their correlation with CD4 count. J Oral Sci 2011;53:203–11. [DOI] [PubMed] [Google Scholar]
- [41].Nicolatou-Galitis O, Velegraki A, Paikos S, et al. Effect of PI-HAART on the prevalence of oral lesions in HIV-1 infected patients. A Greek study. Oral Dis 2004;10:145–50. [DOI] [PubMed] [Google Scholar]
- [42].Tamí-Maury IM, Willig JH, Jolly PE, et al. Prevalence, incidence, and recurrence of oral lesions among HIV-infected patients on HAART in Alabama: a two-year longitudinal study. South Med J 2011;104:561–6. [DOI] [PubMed] [Google Scholar]


