Abstract
Pneumoperitoneum has always been considered a surgical emergency as it represents a perforation of the gastrointestinal tract. Although several cases of pneumoperitoneum with pneumatosis intestinalis (PI) have been reported, the characteristics of such cases remain unclear. The current study aimed to clarify the clinical characteristics of pneumoperitoneum cases with PI detected using computed tomography (CT).
This descriptive study was conducted at a single center. In a total of 18,513 abdominal CT scans obtained between January 2010 and February 2017, extraluminal free air was detected in 254 examinations of 182 cases. The medical records and CT images of these 182 patients were retrospectively analyzed.
Pneumoperitoneum with PI was detected through 23 examinations in 21 cases, and the average age of the patients was 80.1 years. The frequency was 0.12% in all abdominal CT examinations, but 24.7% in the 85 cases with extraluminal free air, excluding iatrogenic air. PI was classified as benign in 20 cases and as life-threatening in 1 case. The majority of cases with benign PI showed good general and local findings and little leukocytosis, while the case with life-threatening PI showed severe conditions. No evidence of bowel wall discontinuity, segmental bowel-wall thickening, perivisceral fat stranding, and abscesses were observed. Ascites were detected less frequently in the cases with PI than in the other pneumoperitoneum cases (P < .01). Pneumoperitoneum and PI occasionally recurred, and PI and/or extraluminal free air generally disappeared quickly.
Pneumoperitoneum with PI is a relatively common condition in older patients, and the majority of cases are caused by benign PI. The characteristics of pneumoperitoneum cases with benign PI include well-maintained physical conditions, normal laboratory data, absence of CT findings indicative of peritonitis, and infrequent ascites. In pneumoperitoneum cases with PI, predicting whether the PI is benign or life-threatening is clinically very important, whereas the presence of extraluminal free air is considered to be insignificant.
Keywords: computed tomography, extraluminal free air, nonsurgical pneumoperitoneum, pneumatosis intestinalis, pneumoperitoneum
1. Introduction
Pneumoperitoneum is considered one of the most important signs of severe intraabdominal disease. Diagnosis of pneumoperitoneum is generally based on the presence of intraperitoneal free air under the diaphragm on upright plain radiography, or between the free edge of the liver and the lateral wall of the peritoneal cavity on left lateral decubitus radiography.[1] Advances in computed tomography (CT) have enabled the detection of smaller amounts of extraluminal free air, including intraperitoneal free air.[2,3] The increased use of CT scanning at many medical institutions, as well as improvements in CT scanning resolution, have improved the diagnostic quality of acute abdominal disease.
Conversely, several cases of pneumoperitoneum that do not require surgical intervention, known as a spontaneous or nonsurgical pneumoperitoneum, have been reported.[4,5,6,7,8] Thus, not all cases of pneumoperitoneum require laparotomy because the presence of free air does not necessarily indicate a life-threatening intraperitoneal perforation. Despite the description of various nonsurgical causes of pneumoperitoneum, unnecessary surgery is often performed as a result of the difficulty in obtaining an accurate diagnosis.
Pneumatosis intestinalis (PI) is an uncommon condition in which gas is found in a linear or cystic form in the submucosa or subserosa of the bowel wall and is one of the main abdominal causes of nonsurgical pneumoperitoneum.[8,9,10] PI is most sensitively identified by CT,[11] and the majority of recent studies on pneumoperitoneum with PI have involved CT.[12,13,14,15,16] However, these previous studies have been limited to case reports, and the clinical analysis of pneumoperitoneum with PI is currently insufficient. This study retrospectively analyzed pneumoperitoneum cases with PI detected using CT in order to clarify the clinical characteristics of the cases.
2. Methods
This retrospective descriptive study was conducted at a single center, and was approved by the Fujimi-Kogen Medical Center Ethics Committee (Approval No. 54). A total of 18,513 abdominal CT examinations (14,556 plain CT and 3957 contrast-enhanced CT) were performed at Fujimi-Kogen Hospital of Fujimi-Kogen Medical Center between January 2010 and February 2017. All examinations were ordered by medical doctors in the outpatient, inpatient, or emergency departments. All CT examinations were performed using a 32-slice multi-detector CT scanner (Aquilion 32, Toshiba, Japan), using a collimated slice thickness of 1 mm. All findings of the CT scan images were reported in our database.
The database was searched using “free air” as the keyword to identify cases with extraluminal free air. Extraluminal free air consists of intraperitoneal, intramesenteric, and retroperitoneal free air and was detected in 253 examinations of 182 patients. The medical records and CT images of the 182 patients were reviewed to confirm the cause of the free air.
2.1. Imaging analysis
PI was simultaneously detected in 21 of 182 cases; in the 21 cases, plain CT examination was performed in 20, and both plain and contrast-enhanced CT examinations were performed in one. Plain CT images of pneumoperitoneum cases with PI were reevaluated. The CT findings that were evaluated included bowel wall discontinuity, segmental bowel-wall thickening, perivisceral fat stranding, intraabdominal abscess, ascites, extraluminal free air, portal venous gas, and PI.
In each case, the maximum diameter of the largest pocket of intraperitoneal free air, located either under the abdominal wall or in the perihepatic space, was measured in order to estimate the amount of extraluminal free air. We did not measure intramesenteric or retroperitoneal free air because the maximum diameter of the intramesenteric or retroperitoneal air could not be measured accurately.
PI was defined as the presence of air in the bowel wall and was identified using lung window settings.[11] The PI grades were classified according to the following criteria: mild as bubbly, linear, or circular air (Fig. 1A and B) in or along <10 cm of the bowel wall; and severe as air in or along ≥10 cm of the bowel wall, or air not only in the bowel wall but also in the mesentery (Fig. 1C).
Figure 1.

Pneumatosis intestinalis was identified using lung window settings. A: Bubbly air (black arrows) in sigmoid colon. B: Linear and circular air (black arrows) in the small intestine. C: Air in the small intestine (white arrows) and in the mesentery (black arrows).
2.2. Statistical analysis
Statistical analysis was performed using the Chi-square test and Mann–Whitney U test using the StatView 5.0 statistical software package (Abacus Concepts, Berkeley, CA). P-value <.05 was considered significant.
3. Results
3.1. Frequency of pneumoperitoneum with PI
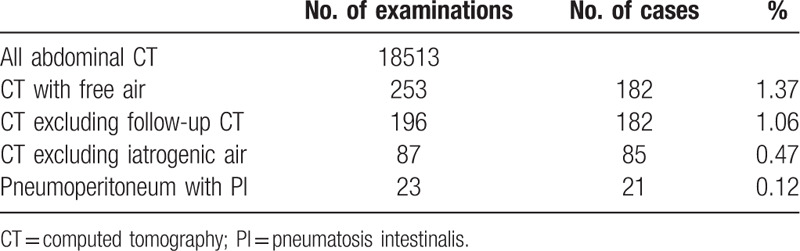
Out of the 18,513 abdominal CT examinations, extraluminal free air was detected in 253 examinations of 182 cases. Follow-up CT examinations were performed in 182 patients to observe the clinical course after the detection of extraluminal free air, and extraluminal free air was detected in 57 examinations. Of the 196 examinations of 182 cases, excluding the 57 follow-up examinations, iatrogenic air was detected in 109 examinations. The iatrogenic air consisted of air after laparotomy in 87 examinations, air after gastrointestinal endoscopic therapeutic procedure in 14 examinations, and air after other therapeutic procedures in 8 examinations. Out of the 87 examinations of 85 cases excluding iatrogenic air, PI was simultaneously detected through 23 examinations in 21 cases. The frequency of pneumoperitoneum with PI was 0.12% in all abdominal CT examinations (Table 1).
Table 1.
Frequency of pneumoperitoneum with pneumatosis intestinalis.
3.2. Causes of extraluminal free air
The causes of the extraluminal free air in the 85 cases, excluding iatrogenic air, are outlined in Table 2, and colorectal perforation was found to be the most common cause of extraluminal free air. The frequency of pneumoperitoneum cases with PI was 24.7%, and was the second most common finding, while perforated duodenal ulcer was the third most common cause.
Table 2.
Causes of extraluminal free air.

3.3. Indications for CT scan
The indications for the 23 CT examinations in 21 cases were as follows. There were 6 examinations for acute abdominal diseases, 6 examinations for digestive symptoms, 3 examinations for fever, 2 examinations for abdominal tumors, 1 examination for urological disease, 1 examination for multiple trauma, and 1 examination for consciousness disturbance. Furthermore, there were 2 examinations for intraperitoneal free air observed in other examination and 1 examination for PI observed in other examination.
3.4. Clinical features
The clinical features of pneumoperitoneum cases with PI are presented in Table 3. Pneumoperitoneum cases with PI tended to be older. In total, 20 patients had a good general condition and were successfully treated with no treatment or mild symptomatic treatment such as short-term antibiotic administration and/or infusion; these cases were classified as benign forms of PI. One case showed shock vital signs, and died after 1 day, and was diagnosed with bowel necrosis; thus, the case was classified as life-threatening. None of the patients underwent laparotomy.
Table 3.
Clinical features of pneumoperitoneum cases with pneumatosis intestinalis.
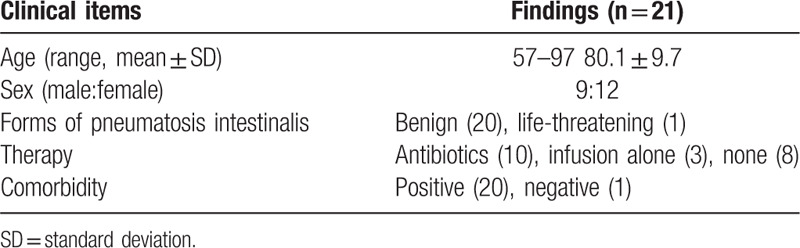
In total, 20 of the 21 patients had comorbidities such as cardiovascular, digestive, neurological, and endocrine disorders; 1 patient had bronchial asthma, 3 patients received steroids, 1 patient received α-glucosidase, and 1 case received chemotherapy for cancer. No specific comorbidities were observed among the cases.
3.5. Symptoms and laboratory data
The symptoms and laboratory data of the cases with benign PI are presented in Table 4. The chief complaints of the cases varied, but all cases had a good general condition, and many showed no peritoneal signs. Abdominal tenderness was observed in 2 cases, and both abdominal tenderness and slight muscular defense were observed in 2 cases. Although no leukocytosis was observed in several cases, CRP levels were found to be elevated.
Table 4.
Symptoms and laboratory data of cases with a benign form of pneumatosis intestinalis.

A case with a life-threatening form of PI showed shock vital signs, conscious disturbance, severe peritoneal signs, leukocytosis, and a high CRP level.
3.6. CT findings when pneumoperitoneum with PI was detected
The CT findings are summarized in Table 5. There was no evidence of bowel wall discontinuity, segmental bowel wall thickening, perivisceral fat stranding, and abscesses. The presence of ascites was observed in 6 cases, including a case with life-threatening PI. Portal venous gas was observed in a patient with life-threatening PI, intraperitoneal free air was detected in 20 cases, and retroperitoneal free air alone was detected in 1 case. The maximum diameter of intraperitoneal free air varied among cases.
Table 5.
Computed tomography (CT) findings of pneumoperitoneum with pneumatosis intestinalis.

Ascites were compared between the 21 pneumoperitoneum cases with PI and the other 64 cases with pneumoperitoneum excluding iatrogenic air. Ascites were detected in 6 cases of pneumoperitoneum with PI and in 42 other pneumoperitoneum cases. The presence of ascites was significantly lower in pneumoperitoneum cases with PI (P = .003).
The maximum diameter of intraperitoneal free air was compared between mild and severe grades of PI, and no significant differences in the maximum diameter of intraperitoneal free air were observed between the grades (P = .999) (Fig. 2).
Figure 2.

Maximum diameter of intraperitoneal free air and grade of pneumatosis intestinalis. No significant differences in the maximum diameter of intraperitoneal free air were observed between the grades (P = .999).
3.7. Chronological changes in CT findings
Follow-up CT examination was performed in 6 cases in order to observe the clinical course within 7 days after the detection of pneumoperitoneum. When the follow-up CT was performed, extraluminal free air alone was detected in 2 cases, PI alone was detected in 1 case, and neither PI nor extraluminal free air was detected in 3 cases.
A total of 92 abdominal CT examinations were performed in cases of pneumoperitoneum with benign PI between January 2010 and February 2017. Excluding 20 CT examinations when pneumoperitoneum with PI was detected, and 6 follow-up CT examinations, 66 CT examinations were reevaluated for the presence of extraluminal free air and PI, and the results are presented in Fig. 3. PI was metachronously observed in 5 cases, and pneumoperitoneum with PI was observed twice in 1 case.
Figure 3.

Chronological changes in computed tomography (CT) findings in pneumoperitoneum cases with benign pneumatosis intestinalis (PI). F-CT = Follow-up CT; P + PI = pneumoperitoneum with pneumatosis intestinalis;  Both free air and pneumatosis intestinalis positive CT examination;
Both free air and pneumatosis intestinalis positive CT examination;  Pneumatosis intestinalis positive CT examination;
Pneumatosis intestinalis positive CT examination;  Free air-positive CT examination;
Free air-positive CT examination;  CT examination; N = number of CT examinations.
CT examination; N = number of CT examinations.
4. Discussion
In this study, we demonstrated that the frequency of pneumoperitoneum with PI was 0.12% among all abdominal CT examinations. Among the cases of extraluminal free air without iatrogenic air, PI was observed in 24.7% of cases. This was the second highest frequency after colorectal perforation, indicating that pneumoperitoneum cases with PI are relatively common. In 2000, Mularski et al[9] reported in a review article that pneumoperitoneum was caused by visceral perforation in 85% to 95% of all occurrences, while in 5% to 15% of cases, pneumoperitoneum had another cause that did not require emergency surgery. These observations were based on several reports using plain radiography rather than CT examination; however, CT has improved since 2000, and has been increasingly adopted by many medical institutions worldwide. The increased imaging detection of PI could be because of the increased use of CT technology and the increased incidence of PI associated with new surgical procedures and medications.[11] The present study is the first to clarify the frequency of pneumoperitoneum with PI detected using CT.
PI is a sign, not a disease, and therefore its significance is directly related to the patient's overall clinical status.[10] Life-threatening PI, also called pathologic or fulminant, is associated with an acute bacterial process, sepsis, and necrosis of the bowel, while benign PI can be totally asymptomatic and observed as an incidental finding.[17] In the majority of cases in the current study were classified as benign, and only one was classified as life-threatening. PI can result in pneumoperitoneum caused by the rupture of subserosal cysts.[10,17] Jamart[18] reported that pneumoperitoneum was present in 9% of PI cases, while DuBose et al[19] reported that intraperitoneal free air was detected in 19.8% of PI cases. The mean ages of patients with PI reported by Wu et al,[20] DuBose et al,[19] and Saito et al[21] were 45.3, 56.6, and 64.7 years, respectively. The ages of our cases were particularly high compared with those of the patients enrolled in the aforementioned studies, and the current study may indicate that PI readily leads to ruptures in older patients.
PI has been found in adults with obstructive pulmonary disease, and is associated with a wide variety of conditions including pyloric stenosis, collagen vascular disease, and ischemic bowel disease. PI has also been observed after endoscopy and drug therapy, jejunoileal bypass, and transplantation, particularly after administration of steroids and chemotherapy for cancer.[10] In addition, more recently, treatment with α-glucosidase inhibitors was reported to be a cause of PI.[22] Although the majority of pneumoperitoneum cases with PI exhibited comorbidities in the current study, no specific shared comorbidities were found.
Clinical findings and laboratory data varied according to the type of PI. The majority of cases with benign PI showed well-maintained general and local conditions and normal laboratory data. Mularski et al[6] reported that nonsurgical causes of pneumoperitoneum should be considered when abdominal pain and distension are minimal and peritoneal signs, fever, and leukocytosis are absent. Several reported cases of pneumoperitoneum with PI showed similar physical conditions and laboratory data.[12,13,14,15,16,23] Conversely, a case with life-threatening PI showed serious conditions and abnormal laboratory data.
In the CT findings of pneumoperitoneum cases with PI, bowel wall discontinuity, segmental bowel-wall thickening, perivisceral fat stranding, and abscesses were not observed in all cases; these CT findings are indicative of acute bowel disease and gastrointestinal perforation.[24,25] From these results, the absence of CT findings indicative of peritonitis and infrequent ascites represent radiological findings commonly found in pneumoperitoneum cases with PI. It is noteworthy that there were no significant differences in the maximum diameter of the intraperitoneal free air between the grades of PI. Therefore, PI can be considered to cause pneumoperitoneum, even if the PI is minimal and the extraluminal free air is significant.
Recurrent pneumoperitoneum with PI has been reported.[16,26,27] Our chronological CT analysis showed relapses of PI and pneumoperitoneum with PI, suggesting that pneumoperitoneum recurs with the recurrence of PI. Furthermore, PI and/or extraluminal free air often disappeared quickly. These findings indicate that extraluminal free air alone can be detected in pneumoperitoneum cases caused by PI when CT examination is delayed, and suggest that PI may be one of the causes of extraluminal free air in idiopathic pneumoperitoneum cases.
Pneumoperitoneum represents a perforation of the gastrointestinal tract and is considered a surgical emergency. However, in the current study, most pneumoperitoneum with PI was caused by benign PI, and pneumoperitoneum was considered to be a nonsurgical pneumoperitoneum. Thus, it is clinically very important to determine whether the PI is benign or life-threatening in pneumoperitoneum cases with PI, whereas the presence of extraluminal free air is not considered to be significant. Ho et al[11] reported that the imaging appearance of benign and life-threatening PI is very similar, and the correlation with clinical history, physical examination, and laboratory test results is the best indicator of benign or life-threatening PI. Furthermore, DuBose et al[19] reported that hyperlactemia, in combination with either hypotension/pressor requirement or peritonitis, was strongly associated with life-threatening PI. Intestinal ischemia and mesenteric vascular disease are the main causes of life-threatening PI.[11] Barmase et al[28] reported that contrast-enhanced CT was an effective noninvasive modality for the diagnosis of mesenteric ischemia; Kammerer et al[29] and Garcia et al[30] also reported the usefulness of contrast-enhanced CT in the diagnosis of non-occlusive mesenteric ischemia. Therefore, complete physical examinations, laboratory data (including lactate), and contrast-enhanced CT are necessary if life-threatening PI is suspected.
This study has a limitation of small number of cases, especially cases with life-threatening PI. Therefore, the characteristics of cases with benign PI could be determined, but not those of cases with life-threatening PI. Despite this limitation, this study comprises the largest number of pneumoperitoneum cases with PI at this time. In the future, it will be necessary to analyze many cases from multiple centers in order to fully validate our findings.
In conclusion, pneumoperitoneum with PI detected using CT is relatively common, and PI may lead to ruptures more readily in elderly patients. The most common cause of extraluminal free air was benign PI, and the characteristics of cases with benign PI included well-maintained general and local conditions, normal laboratory data, absence of CT findings indicative of peritonitis, and infrequent ascites. Differential diagnosis of PI types is clinically very important in pneumoperitoneum cases with PI.
Acknowledgments
The authors appreciate the cooperation of Mr Hideto Nagai in the Department of Clinical Radiology of Fujimi-Kogen Hospital. They would like to thank Editage (www.editage.com) for English language editing.
Author contributions
Conceptualization: Wataru Adachi.
Investigation: Wataru Adachi, Tomohito Matsushita, Yasuaki Yashiro, Jiro Imura, Hideki Shiozawa, Kyo Kishimoto.
Writing – original draft: Wataru Adachi, Yasuaki Yashiro.
Footnotes
Abbreviations: CT = computed tomography, PI = pneumatosis intestinalis.
How to cite this article: Adachi W, Matsushita T, Yashiro Y, Imura J, Shiozawa H, Kishimoto K. Clinical characteristics of pneumoperitoneum with pneumatosis intestinalis detected using computed tomography: A descriptive study. Medicine. 2020;99:40(e22461).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Pinto A, Miele V, Schillirò ML, et al. Spectrum of signs of pneumoperitoneum. Semin Ultrasound CT MR 2016;37:3–9. [DOI] [PubMed] [Google Scholar]
- [2].Stapakis JC, Thickman D. Diagnosis of pneumoperitoneum: abdominal CT vs. upright chest film. J Comput Assist Tomogr 1992;16:713–6. [PubMed] [Google Scholar]
- [3].Singh JP, Steward MJ, Booth S, et al. Evolution of imaging for abdominal perforation. Ann R Coll Surg Engl 2010;92:182–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gantt CB, Jr, Daniel WW, Hallenbeck GA. Nonsurgical pneumoperitoneum. Am J Surg 1977;134:411–4. [DOI] [PubMed] [Google Scholar]
- [5].van Gelder HM, Allen KB, Renz B, et al. Spontaneous pneumoperitoneum. A surgical dilemma. Am Surg 1991;57:151–6. [PubMed] [Google Scholar]
- [6].Mularski RA, Ciccolo ML, Rappaport WD. Nonsurgical causes of pneumoperitoneum. West J Med 1999;170:41–6. [PMC free article] [PubMed] [Google Scholar]
- [7].Madura MJ, Craig RM, Shields TW. Unusual causes of spontaneous pneumoperitoneum. Surg Gynecol Obstet 1982;154:417–20. [PubMed] [Google Scholar]
- [8].Williams NMA, Watkin DFL. Spontaneous pneumoperitoneum and other nonsurgical causes of intraperitoneal free gas. Postgrad Med J 1997;73:531–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Mularski RA, Sippel JM, Osborne ML. Pneumoperitoneum: a review of nonsurgical causes. Crit Care Med 2000;28:2638–44. [DOI] [PubMed] [Google Scholar]
- [10].Heng Y, Schuffler MD, Haggitt RC, et al. Pneumatosis intestinalis: a review. Am J Gastroenterol 1995;90:1747–58. [PubMed] [Google Scholar]
- [11].Ho LM, Paulson EK, Thompson WM. Pneumatosis intestinalis in the adult: benign to life-threatening causes. AJR Am J Roentgenol 2007;188:1604–13. [DOI] [PubMed] [Google Scholar]
- [12].Imai K, Doi Y, Takata N, et al. Successful conservative treatment of pneumatosis intestinalis associated with intraperitoneal free air: report of a case. Surg Today 2012;42:992–6. [DOI] [PubMed] [Google Scholar]
- [13].Furihata T, Furihata M, Ishikawa K, et al. Does massive intraabdominal free gas require surgical intervention? World J Gastroenterol 2016;22:7383–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Dhadlie S, Mehanna D, McCourtney J. Pneumatosis intestinalis a trap for the unwary: case series and literature review. Int J Surg Case Rep 2018;53:214–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Belkhir A, Jrad M, Sebei A, et al. Pneumatosis cystoides intestinalis revealed after a hand-to-hand aggression: a case report. Int J Surg Case Rep 2019;62:100–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Pata F, Di Saverio S. Pneumatosis cystoides intestinalis with pneumoperitoneum. N Engl J Med 2019;380:e17. [DOI] [PubMed] [Google Scholar]
- [17].Galandiuk S, Fazio VW. Pneumatosis cystoides intestinalis. A review of the literature. Dis Colon Rectum 1986;29:358–63. [DOI] [PubMed] [Google Scholar]
- [18].Jamart J. Pneumatosis cystoides intestinalis. A statistical study of 919 cases. Acta Hepato-Gastroenterol 1979;26:419–22. [PubMed] [Google Scholar]
- [19].DuBose JJ, Lissauer M, Maung AA, et al. EAST Pneumatosis Study Group. Pneumatosis Intestinalis Predictive Evaluation Study (PIPES): a multicenter epidemiologic study of the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 2013;75:15–23. [DOI] [PubMed] [Google Scholar]
- [20].Wu LL, Yang YS, Dou Y, et al. A systemic analysis of pneumatosis cystoides intestinalis. World J Gastroenterol 2013;19:4973–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Saito D, Hayashida M, Miura M, et al. Clinical characteristics of patients with pneumatosis cystoides intestinalis. Nihon Shokakibyo Gakkai Zasshi 2015;112:494–9. (in Japanese with English Abstract). [DOI] [PubMed] [Google Scholar]
- [22].Kojima K, Tsujimoto T, Fujii H, et al. Pneumatosis cystoides intestinalis induced by the α-glucosidase inhibitor miglitol. Intern Med 2010;49:1545–8. [DOI] [PubMed] [Google Scholar]
- [23].Sooby P, Harshen R, Joarder R. An unusual triad of pneumatosis intestinalis, portal venous gas and pneumoperitoneum in an asymptomatic patient. J Surg Case Rep 2015;4:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hainaux B, Agneessens E, Bertinotti R, et al. Accuracy of MDCT in predicting site of gastrointestinal tract perforation. AJR Am J Roentgenol 2006;187:1179–83. [DOI] [PubMed] [Google Scholar]
- [25].Kim HC, Yang DM, Kim SW, et al. Gastrointestinal tract perforation: evaluation of MDCT according to perforation site and elapsed time. Eur Radiol 2014;24:1386–93. [DOI] [PubMed] [Google Scholar]
- [26].Alassaf M. Recurring spontaneous aseptic pneumoperitoneum presenting secondary to an unrelated chief complaint: a case report. Int J Surg Case Rep 2015;7:96–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Beetz O, Kleine M, Vondran FWR, et al. A case of recurrent pneumoperitoneum and pneumatosis intestinalis after bilateral lung transplant. Exp Clin Transplant 2019;1:124–7. [DOI] [PubMed] [Google Scholar]
- [28].Barmase M, Kang M, Wig J, et al. Role of multidetector CT angiography in the evaluation of suspected mesenteric ischemia. Eur J Radiol 2011;80:e582–7. [DOI] [PubMed] [Google Scholar]
- [29].Kammerer S, Schuelke C, Berkemeyer S, et al. The role of multislice computed tomography (MSCT) angiography in the diagnosis and therapy of non-occlusive mesenteric ischemia (NOMI): could MSCT replace DSA in diagnosis? PLoS One 2018;13:e0193698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].García PC, Campos EM, Gonzalo AF, et al. Non-occlusive mesenteric ischaemia: CT findings, clinical outcomes and assessment of the diameter of the superior mesenteric artery. Br J Radiol 2018;20170492. [DOI] [PMC free article] [PubMed] [Google Scholar]


