Abstract
Reverse shoulder arthroplasty is a common procedure. While dislocation is a common complication, there are few reports documenting dislocation with associated polyethylene liner dissociation from the humeral tray. There have been 4 instances of this occurrence over 9 years at our institution, and there are specific radiographic clues for diagnosis. Recognizing polyethylene liner dissociation on imaging is important prior to treatment. In a “routine” dislocation, closed reduction may be attempted but when the polyethylene is dissociated, open reduction is the only treatment option, as closed reduction can damage the components. Dislocations with polyethylene dissociation may not be initially recognized, prompting a non-operative period leading to wear and metallosis. These 4 cases demonstrate key findings present on imaging to recognize the difference between a dislocation with and without polyethylene liner dissociation, namely the subluxation appearance rather than dislocation.
Keywords: reverse shoulder arthroplasty, shoulder arthroplasty dislocation, dissociated components, polyethylene dissociation, implant failure
CASE SERIES
Case 1
Presentation
A 58-year-old male was treated with a right reverse shoulder arthroplasty (RSA) for rotator cuff arthropathy. The patient had a dislocation event approximately five months after his index procedure while lifting a heavy piece of furniture, and he presented to the emergency department where radiographs where obtained demonstrating a subluxated appearance of the RSA components (Fig. 1). Closed reduction was attempted but failed. He presented to clinic one week after failed reduction, and at this time there was concern that the components might also be infected due to changes in the appearance of the incision scar. Plain radiographs and computed tomography (CT) images were concerning for dislocation, however the polyethylene was not appreciated. There was apparent loosening of the humeral stem, which was consistent with infection, so open treatment was planned.
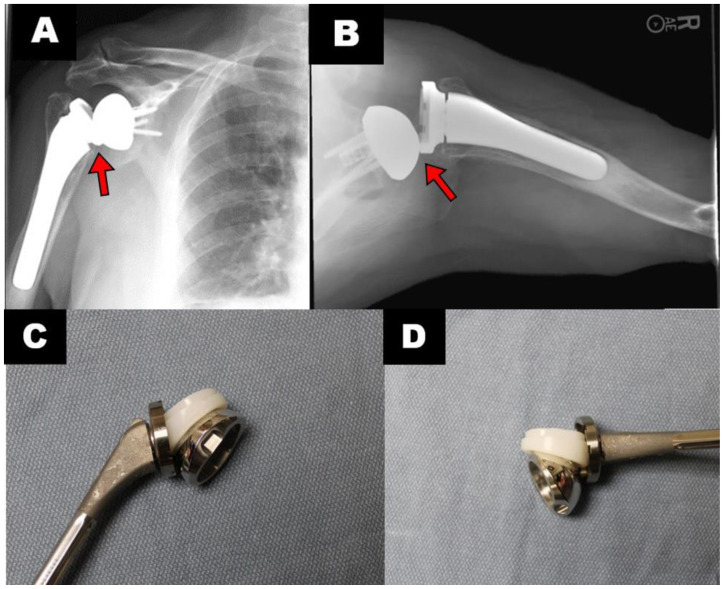
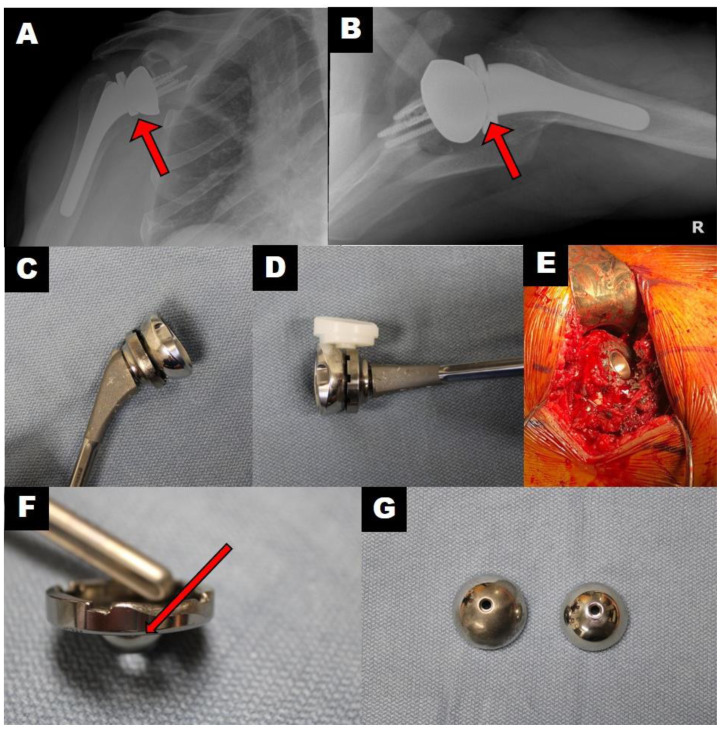
Figure 1.
A 58-year-old male with reverse shoulder arthroplasty dislocation with polyethylene liner dissociation
Findings/technique-Anteroposterior (A) and axillary lateral (B) radiographic views demonstrate dislocation with complete polyethylene liner dissociation with subluxation appearance (less than 100% displacement) compared to a full dislocation (arrow). This is only possible with the liner dissociation. Photographs of components demonstrating the positioning of the humeral stem, tray and polyethylene liner in relation to the glenosphere that corresponds with the previous radiographs (C & D).
Treatment
The patient underwent operative exploration of the shoulder. Upon entering the shoulder joint, the polyethylene was found to be completely dissociated from the humeral tray. The patient was also found to have extensive loosening of the humeral component. An antibiotic spacer was then placed, and the patient was placed on appropriate antibiotic regimen. Intraoperative samples grew Cutibacterium acnes (C. acnes). The patient was treated definitively with the antibiotic spacer.
Case 2
Presentation
A 61-year-old male with Parkinson’s disease was treated with a left RSA for rotator cuff arthropathy. The patient had an uncomplicated postoperative period. Approximately 8 months postoperatively, the patient had a dislocation event precipitated by his dog jerking on his leash. When seen in clinic, there was a palpable mass anteriorly with concern that it might be the humeral liner, and the patient noted exquisite pain. Images taken acutely at an outside emergency department were read as negative (Fig. 2, a–b). Our own review of the imaging was concerning for complete polyethylene dissociation, and a CT scan was obtained demonstrating subluxation of the components (Fig. 2, c–d). Therefore, open treatment was planned for presumed polyethylene liner dissociation.
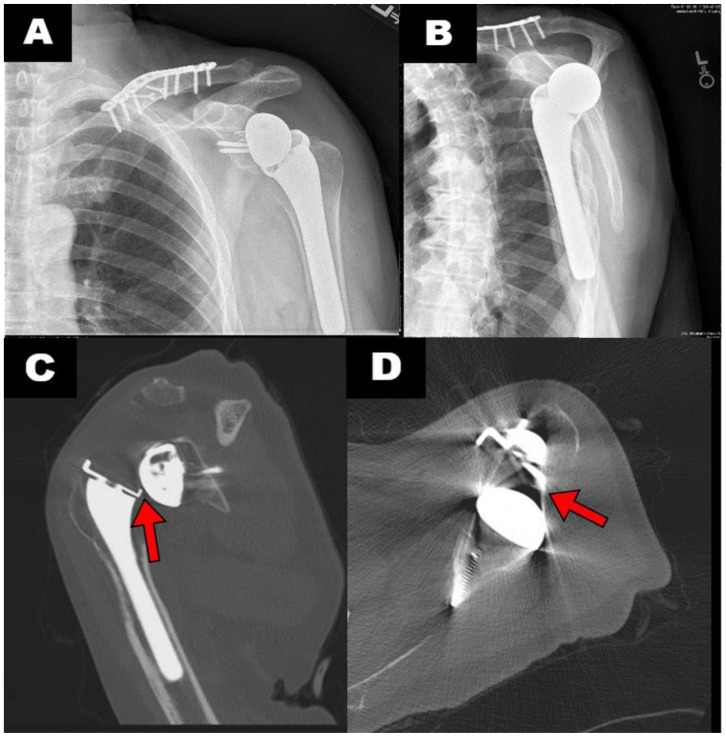
Figure 2.
A 61-year-old male with reverse shoulder arthroplasty dislocation with polyethylene liner dissociation
Findings/technique - Anteroposterior (A) and scapular Y (B) radiographic views taken acutely in the emergency department and not felt to represent a dislocation. An axillary lateral view was not obtained. A CT scan was taken with representative coronal (C) and axial (D) cuts demonstrating the subluxated appearance (arrows) that is found with polyethylene dissociation.
Treatment
The patient underwent revision reverse shoulder arthroplasty of the affected side. Intraoperatively the polyethylene was completely dissociated. There was no concern intraoperatively for infection. A larger glenosphere was implanted and a constrained liner was placed. Intraoperative cultures returned positive for C. acnes, and the patient was placed on antibiotic therapy. The patient was last seen 4 months out from his most recent surgery and had no further complications, was without pain, and denied any instability symptoms. His range-of-motion is 140 degrees in forward flexion and 45 degrees of external rotation with his elbow at his side.
Case 3
Presentation
A 74-year-old male was treated with a right RSA for rotator cuff nine years prior to presentation at our facility. He had sustained multiple dislocations and infections in the past, which were treated with hardware explantations and placement of an antibiotic spacer as well as revision hardware implantation. His most recent surgery was a revision right RSA reimplantation after clearance of an infection eight months prior to presentation to our facility. He sustained a dislocation with complete polyethylene dissociation after a fall from ground level (Fig. 3, a–b), and open treatment was planned.
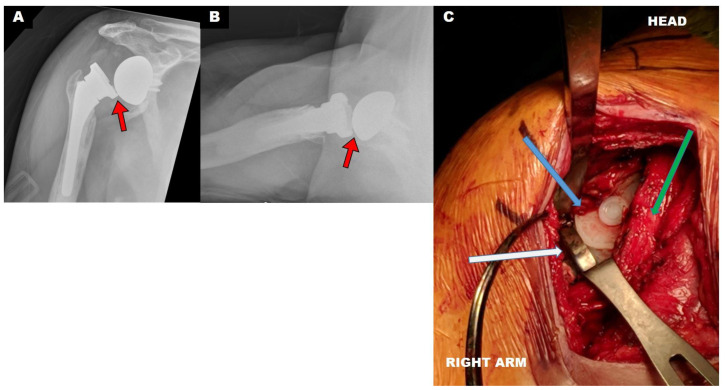
Figure 3.
A 74-year-old male with reverse shoulder arthroplasty (RSA) dislocation with polyethylene liner dissociation
Findings/Technique - Anteroposterior (A) and axillary lateral (B) radiographic views again demonstrating the subluxated appearance found with polyethylene dissociation (red arrow). This patient had previously received revision RSA for prior dislocations. Despite the relatively normal appearance of the axillary radiograph (which is obtained by placing the arm in abduction) the anteroposterior radiograph clearly demonstrates the subluxation consistent with complete polyethylene dissociation (red arrow). Upon entry into the shoulder joint during surgery, the completely dissociated polyethylene was visualized (C). The patient is in a beach chair position with a view into the deltopectoral approach to the shoulder. The humeral tray (white arrow), polyethylene (blue arrow), and subscapularis/glenohumeral capsule (green arrow) are visualized.
Treatment
The patient underwent revision reverse shoulder arthroplasty of the affected side. Intraoperatively the polyethylene was completely dissociated (Fig. 3c). The previous components were well fixed and intraoperative frozen sections were negative for infection, so revision was undertaken. The glenosphere was retained, but a constrained polyethylene liner and a thicker humeral tray were used. The patient’s intraoperative cultures also returned positive for C. acnes and the patient was placed on antibiotic therapy. His most recent follow-up was 4 months after surgery. At that time, he had full active and passive range-of-motion and was without pain or complaints of instability.
Case 4
Presentation
A 60-year-old male was treated with a right RSA for rotator cuff arthropathy. The patient had an uncomplicated postoperative course until one month postoperatively, when the patient had a dislocation event precipitated by reaching his right arm behind his back to pick up a chair. The patient presented to his nearest hospital’s emergency department, where he underwent a closed reduction. Pre-reduction radiographs demonstrated a complete dislocation without suspected polyethylene dissociation (Fig. 4). The post-reduction images were thought to demonstrate a concentric reduction at the time by his treating physicians and he was immobilized in a sling. He presented to our clinic two weeks later with exam finding of crepitus with active and passive range-of motion and sensations of instability. At that time, new radiographs were felt to demonstrate polyethylene dissociation, with the glenosphere in direct contact with the humeral tray (Fig. 5, a–d). These radiographs demonstrate the glenosphere deep to the lip of the humeral tray, which is not possible if the polyethylene spacer were in place. Open treatment was offered to the patient, which he did not wish to initially undergo and elected a trial of non-operative management. Four weeks later, the patient continued having symptoms of painful grinding and crepitus with any shoulder motion and desired operative treatment.
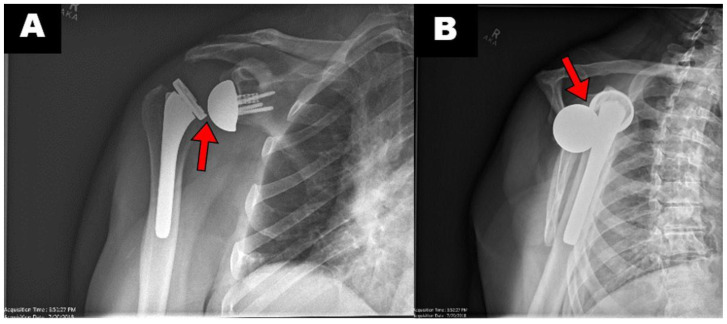
Figure 4.
A 60-year-old male with reverse shoulder arthroplasty dislocation without polyethylene liner dissociation
Findings/Technique - Anteroposterior (A) and scapular Y (B) radiographic views of first dislocation at outside hospital prior to reduction attempt (arrow). This is consistent with a complete dislocation without polyethylene dissociation based on near 100% displacement of the components.
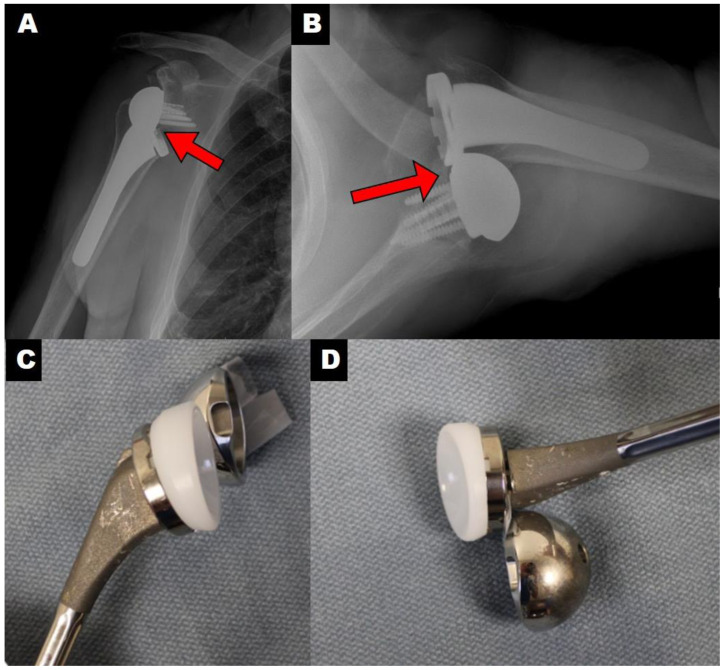
Figure 5.
A 60-year-old male with reverse shoulder arthroplasty dislocation with polyethylene liner dissociation
Findings/Technique - Anteroposterior (A) and axillary lateral (B) radiographic views of what was read as a concentric reduction. Further review of these radiographs demonstrate that the glenosphere is contacting the humeral tray (red arrows), which should not be possible if the polyethylene is in its proper location. Photographs taken in coronal (C) and axial (D) planes demonstrating the position of the components intraoperatively. Intraoperative photograph showing significant metallosis. Head is at the top of the picture and arm is at the bottom (E). Gross appearance of the patient’s components (F) after hardware removal, noting the wear to the edge of the humeral tray (red arrow) as well as the burnishing of the patient’s glenosphere (G, left) as compared to a new one (G, right).
Treatment
The patient underwent revision reverse shoulder arthroplasty. Upon entering the shoulder joint, the polyethylene was found to be dissociated from the humeral tray. The polyethylene exhibited significant wear. There was extensive metallosis present in the shoulder (Fig. 5e), and the glenosphere and metal humeral tray also demonstrated wear from the unintended metal-on-metal articulation (Fig. 5, f–g). Due to the wear, the components were replaced, and the polyethylene was upsized to increase stability. The patient’s most recent follow-up was five months postoperatively, at which time he was doing well without further complication. His range of motion on exam was 130° forward flexion, abduction to 10°, external rotation of 30° with the elbow at the side and internal rotation to the level of his belt. He has smooth motion about the components with no crepitus, pain, or complaints of instability.
DISCUSSION
Etiology & Demographics
RSA is a common technique for treating difficult shoulder pathology. It is most commonly used in the setting of symptomatic rotator cuff arthropathy and in patients older than 75 for primary osteoarthritis given their high degree of concomitant rotator cuff tears [1]. One of the most common complications of RSA is dislocation, with a reported incidence as high as 4.7% in one study [2]. There is a paucity of literature documenting polyethylene dissociation from the humeral tray during dislocations, mostly in case reports and series [3–5].
Kohan et al reviewed the etiology of dislocation in their own patients and proposed the following contributors: intraoperative soft-tissue tensioning, age, history of prior instability events, asymmetric liner wear, mechanical liner failure, axillary nerve injury causing deltoid weakness, and impingement due to heterotopic ossification[6]. Traumatic incidents can be a cause as well. Arm position at time of dislocation in RSA is a combination of arm extension, internal rotation and adduction. Patients often place their shoulder at risk when standing up out of a chair while pushing off with their hand or while reaching backward behind the plane of their torso to grab objects.
Clinical & Imaging findings
Clinically, the findings are often fairly obvious though occasionally can be missed because arthroplasty dislocations can have milder symptoms than an anatomic dislocation. The patient will present with a traumatic event followed by immediate loss of range of motion frequently accompanied by pain.
It is important to recognize key imaging findings to help clue the surgeon and radiologist that the polyethylene has been completely dissociated from the humeral tray. The apparent key imaging finding seems to be the appearance of a subluxation rather than a complete dislocation with near 100% to greater than 100% displacement (Fig 6). The glenohumeral joint is a finite space, so only a nearly complete or complete dislocation should be possible if the polyethylene remains in place. When the polyethylene is out of place, the dislocation will instead present on radiographs as a subluxation with significantly less than 100% displacement.
Figure 6.
A 68-year-old male with reverse shoulder arthroplasty dislocation without polyethylene liner dissociation
Technique - Anteroposterior (A) and axillary lateral (B) radiographic views demonstrating a complete dislocation in which the polyethylene liner remains attached to the humeral tray.
Findings - The images show at least 100% displacement (arrow). Photographs of components demonstrating the positioning of the humeral stem, tray and polyethylene liner in relation to the glenosphere that corresponds with the previous radiographs (C & D).
Treatment & Prognosis
Our institution has performed 543 primary RSA over a 9-year period from 2009–2018 by a single surgeon. There have been a total of 26 dislocations (4.7%). All RSA were performed with the Exactech Equinoxe Reverse Shoulder System (Gainesville, FL). There were four patients identified with complete polyethylene liner dissociation from the humeral tray. Though there are reports of closed reduction after RSA dislocation successful in the literature [7, 8], the typical treatment at our institution is open reduction, which has been shown in recent studies to be successful in 85% of cases after primary RSA dislocations, as compared to a 60% success rate with closed reduction [9]. If closed reduction is successfully performed in the emergency department at our institution, it is usually for pain control, and the patient still receives a revision with component exchange. However, there are substantial risks to closed reduction in the rare event that the polyethylene has dissociated. Namely, the reduction will not be successful as there is no surface for the glenosphere component to rest in the humeral tray without a liner present. This will also cause significant damage to the components that are put in contact with one another if multiple attempts are performed. The surgeon can often retain metal components during the open reduction if the metallic surfaces are not scratched. Burnished and scratched surfaces, however, can further lead to increased wear and particle debris, which can lead to osteolysis, aseptic loosening of components, and ultimately failure of the prosthesis long-term.
The rate of polyethylene dissociation calculated at our institution for this case series is 15.4% of all dislocations, or 0.7% of all RSA. The consequences of missing this could be detrimental to the patient. For example, if a patient is thought to be well reduced but is having significant crepitus, this can lead to significant wear of the metallic components of the RSA with need for revision that might not have been otherwise necessary if open reduction were performed early (this occurred with the patient in case 4). This patient’s implants demonstrated severe wear after only 4 weeks of attempted non-operative treatment per the patient’s wishes. This required a more involved revision with a potentially higher complication rate. There was also significant metallosis in the patient’s shoulder joint at the time of surgery. If the metallic microscopic fragments are not completely removed, this can lead to higher risk of complications like osteolysis or even pseudotumor formation. It is difficult to remove metallosis surgically and requires extensive debridement that otherwise might not have been necessary.
Case 2 demonstrates that these instances of dislocation with polyethylene dissociation can be missed if the physician reviewing the imaging is not looking closely for it. A physician may be fooled and think the components are properly reduced as these findings are subtle in comparison to the frank and obvious dislocation that is usually seen. The patient complained of grinding and acutely reduced range-of-motion sustained after his dislocation event. This should lead to suspicion of a polyethylene dissociation and should prompt more advanced imaging for diagnosis. The CT obtained for this patient was done almost 2 months later for pre-operative planning and clearly showed a subluxation of the components. Had this been recognized initially, it could have possibly prevented any wear on his original components while he was waiting for definitive treatment and saved cost. This can also cause repetitive trauma leading to susceptibility for infection.
It should also be noted that 3 of the 4 dislocations presented were infected. It is important to have appropriate clinical suspicion, and we recommend sending tissue for frozen pathology sections as well as multiple samples for cultures, and treating with appropriate antibiotics if cultures become positive postoperatively.
Differential Diagnoses
Differential diagnosis of RSA instability should include dislocation both with and without polyethylene liner dissociation, infection, catastrophic failure with component loosening, and humerus or scapula fracture. Plain radiographs help elucidate the cause of instability.
TEACHING POINT
Reverse Shoulder Arthroplasty (RSA) dislocation with polyethylene liner dissociation is a rare event that has different imaging than a non-dissociated dislocation, namely subluxation of the components rather than complete or near-complete dislocation. It is important to have a high suspicion for this when reviewing radiographs after RSA instability event. In cases where RSA dislocation with polyethylene liner dissociation is recognized, it is now our institution’s policy to proceed with an open reduction and revision of components as necessary and avoid any attempt at a closed reduction.
Table 1.
Summary table for polyethylene liner dissociation after reverse shoulder arthroplasty (RSA) dislocation.
| Etiology | Dissociation of polyethylene component after reverse shoulder arthroplasty dislocation |
| Incidence | Dislocation incidence as high as 4.7%, rate of polyethylene dissociation for this case series is 15.4% of all dislocations, or 0.7% of all RSA |
| Gender ratio | No determinant |
| Age predilection | Unknown |
| Risk factors | Intraoperative soft-tissue tensioning, age, history of prior instability events, asymmetric liner wear, mechanical liner failure, axillary nerve injury causing deltoid weakness, impingement due to heterotopic ossification, traumatic events |
| Treatment | Open reduction and revision of components as needed, without attempt at closed reduction |
| Prognosis | Resolution after revision surgery |
| Findings on imaging | Appearance of a subluxation of prosthesis rather than a complete dislocation with near 100% to greater than 100% displacement |
Table 2.
Differential diagnosis table for polyethylene liner dissociation versus standard dislocation.
| Entity | X-ray | Computed Tomography |
|---|---|---|
| Reverse shoulder arthroplasty with polyethylene liner dissociation | Subluxation of the components with less than 100% displacement | Though appearing located on x-ray, the prosthesis will be subluxated less than 100% on computed tomography |
| Reverse shoulder arthroplasty with standard dislocation | Complete dislocation of components | Complete dislocation of components with less than 100% displacement |
ACKNOWLEDGEMENTS
The authors would like to thank our clinical research associates, Charlotte Gavalas and Judith Kyrkos
ABBREVIATIONS
- C. acnes
Cutibacterium acnes
- CT
Computed tomography
- RSA
Reverse shoulder arthroplasty
REFERENCES
- 1.Sellers TR, Abdelfattah A, Frankle MA. Massive Rotator Cuff Tear: When to Consider Reverse Shoulder Arthroplasty. Curr Rev Musculoskelet Med. 2018;11(1):131–140. doi: 10.1007/s12178-018-9467-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20(1):146–157. doi: 10.1016/j.jse.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Garberina MJ, Williams GR., Jr Polyethylene dissociation after reverse total shoulder arthroplasty: the use of diagnostic arthroscopy. J Shoulder Elbow Surg. 2008;17(1):e16–18. doi: 10.1016/j.jse.2007.02.131. [DOI] [PubMed] [Google Scholar]
- 4.Nizlan NM, Campbell PT, Skirving AP. Dissociated polyethylene liner after a reverse shoulder replacement: a case report. J Shoulder Elbow Surg. 2009;18(5):e26–28. doi: 10.1016/j.jse.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 5.Patel KA, Boyd KL, Renfree KJ, Hattrup SJ. Polyethylene dissociation from humeral stem status after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(11):e346–e351. doi: 10.1016/j.jse.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 6.Kohan EM, Chalmers PN, Salazar D, Keener JD, Yamaguchi K, Chamberlain AM. Dislocation following reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(7):1238–1245. doi: 10.1016/j.jse.2016.12.073. [DOI] [PubMed] [Google Scholar]
- 7.Cheung E, Willis M, Walker M, Clark R, Frankle MA. Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2011;19(7):439–449. [PubMed] [Google Scholar]
- 8.Zhou HS, Chung JS, Yi PH, Li X, Price MD. Management of complications after reverse shoulder arthroplasty. Curr Rev Musculoskelet Med. 2015;8(1):92–97. doi: 10.1007/s12178-014-9252-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chalmers BP, Wagner ER, Sperling JW, Cofield RH, JS-S Treatment and outcomes of reverse shoulder arthroplasty dislocations. J Shoulder Elbow Arthrop. 2017;1:1–6. [Google Scholar]