Abstract
Wandering spleen is a rare condition in which the spleen is hypermobile due to laxity or lack of its supporting ligaments. It can be located anywhere in the abdomen besides its usual position. The other terms that are used to describe this condition are splenic ptosis, displaced spleen, dislocated spleen and ectopic spleen. Splenic torsion is a dreaded complication and the usual cause of symptoms. There is a high chance of missing the diagnosis as it remains asymptomatic or may be incidentally discovered on radio-imaging done for a different purpose. An acute abdomen is the most common presentation. Here we describe an unusual case presenting with torsion of the wandering spleen that was adherent to the right ovary.
Keywords: Acute abdomen, Wandering spleen, torsion, splenectomy, splenopexy
CASE REPORT
A 20-year-old female patient presented with a lump in the abdomen for the past 3 years. The patient gave a history of recurring bouts of abdominal pain requiring hospitalization. On examination, the patient was stable and not in acute pain. She was afebrile [temperature 37.5 Celsius] and vitals were stable [heart rate 80 bpm, blood pressure 118/78mm Hg recorded in the right arm in supine position].
A palpable lump was observed in the mid lower abdomen, which was mobile from side to side, the examination of the rest of the abdomen revealed no other abnormality.
Laboratory values included a hemoglobin level of 12.5 g/dl, a WBC count of 10,500/mm3, and a normal platelet count of 1.9 lakh/mm3. Urine analysis was normal.
Ultrasonography of the abdomen revealed a well-defined hypoechoic lesion measuring 7.8 × 7cm located in the lower central abdomen with no obvious origin from any intrabdominal organ. Internal color flow was seen in the mass and the adjacent ovary. The spleen was not visualized in the left hypochondrium. The right ovary was seen high up and lying adjacent to this structure (Figure 1). Contrast-enhanced CT and non-contrast MRI of the abdomen and pelvis was done to confirm the findings of the USG. Contrast-enhanced CT showed a well-defined, heterogeneous, enhancing mass lesion measuring 8 × 7cm in the central lower abdomen; splenic vessels were seen entering the lesion with a whorled appearance suggesting that it was a wandering spleen with torsion. There was a complete eventration of the left hemidiaphragm, the spleen was not visualized in the left hypochondrium. The right ovary was slightly bulky, measuring 3.2 × 2 × 3.5cm and was adherent to the structure with no intervening fat plane (Figure 2).
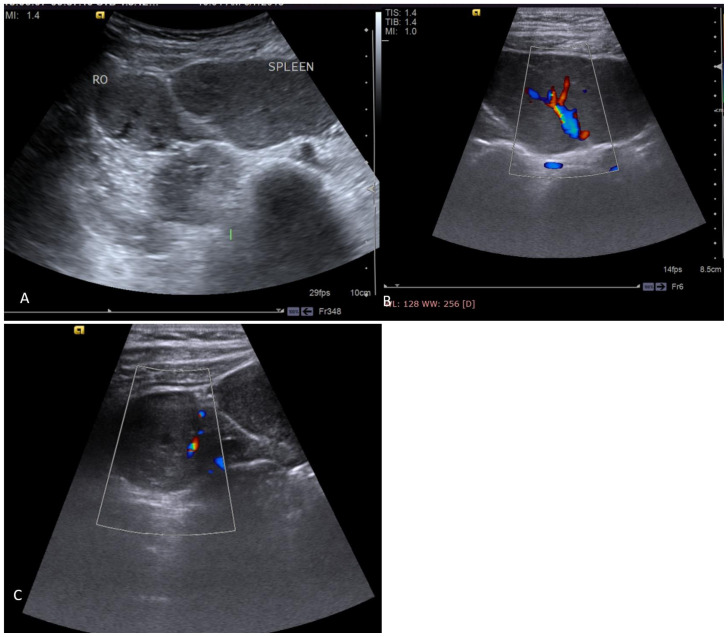
Figure 1.
20-year-old female with torsion of wandering spleen with its adherence to the right ovary.
FINDINGS:
Figure 1 A (Transverse B mode) & B, C(Transverse duplex mode) ultrasound scan shows a well-defined solid lesion measuring 7.8 × 7cm with echo pattern similar to spleen in the lower abdomen with internal vascular pattern as expected in spleen. The right ovary (RO) with a few follicles within is seen abutting the lesion. The right ovary also shows color flow within
TECHNIQUE: Real-time ultrasound images of the lower abdomen acquired on Siemens Acuson s2000 with 4–9 MHz curvilinear probe.
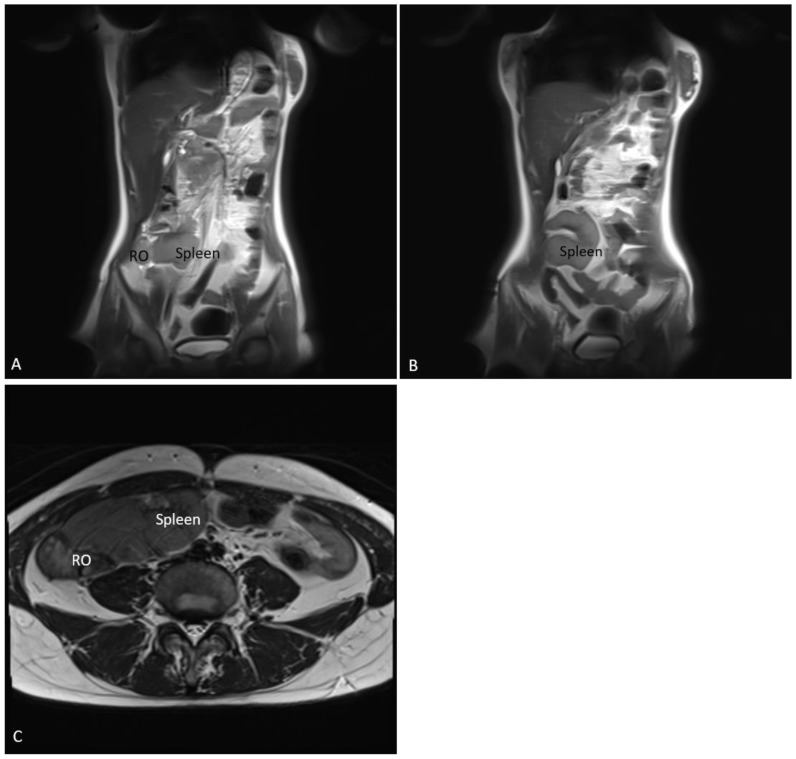
Figure 2.
20-year-old female with torsion of wandering spleen with its adherence to the right ovary.
FINDINGS: Contrast-enhanced axial and coronal CT sections show left-sided diaphragmatic eventration and ectopic location of the spleen measuring 8 × 7cm in the mid-lower abdomen with right ovary (RO) abutting to its right margin. Spleen shows homogeneous enhancement.
TECHNIQUE: Axial contrast-enhanced CT of the abdomen in the venous phase with coronal reformat. (120 KVp, 200 mAs, 5mm slice thickness, iohexol (350mg/ml of iodine) 80ml contrast)
Non-contrast MRI of the abdomen revealed same findings of splenic tissue in central lower abdomen and confirmed the location of right ovarian tissue showing multiple follicles adjacent to it with no intervening fat plane (Figure 3).
Figure 3.
20-year-old female with torsion of wandering spleen with its adherence to the right ovary.
Findings: Axial and coronal T2W MR images show left diaphragmatic eventration and spleen in the lower mid-abdomen with right ovary abutting it.
Technique: 3T magnet strength, T2 WI axial [TR 5200, TE 97], HASTE coronal [TR 1600, TE 87], non-contrast scans
Previous two serial imaging done at a gap of nearly a year were available with the patient, which showed this lesion i.e. spleen at varying locations in the pelvis and the lower abdomen. There was significant change in the splenic size between the two previous scans and diffusely hypoattenuating spleen in the older scan with normal homogeneous enhancement on the second scan. The adhered right ovary which changed position with that of the spleen was also noted in both scans. A diagnosis of wandering spleen with intermittent partial torsion and detorsion, adhered right ovary and left diaphragmatic eventration was given (Figure 4).
Figure 4.
20-year-old female with torsion of wandering spleen with its adherence to the right ovary.
FINDINGS: Figure 4 (A–B): Contrast enhanced CT done in Aug 2016 (coronal and axial reformats) show large hypoenhancing ovoid mass in the midline and right side of lower abdomen with absence of spleen in left hypochondrium(ectopic spleen) and right ovary (RO) abutting its right margin with left sided diaphragmatic eventration.
Figure 4C: Contrast enhanced CT done in July 2017 shows significantly reduced size of spleen with normal homogeneous enhancement and right ovary (RO) abutting its right margin.
TECHNIQUE for A & B: Axial contrast-enhanced CT of the abdomen in the venous phase with coronal reformat. (120 KVp, 100 mAs, 5mm slice thickness, iohexol (350mg/ml of iodine) 80ml contrast)
TECHNIQUE for C: Axial contrast-enhanced CT of the abdomen in the venous phase with coronal reformat. (120 KVp, 130 mAs, 5mm slice thickness, iohexol (350mg/ml of iodine) 80ml contrast)
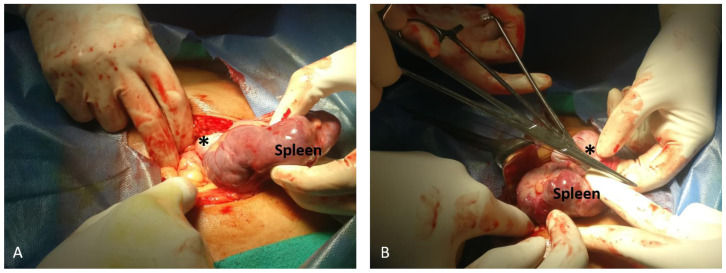
Due to the recurrence and persistence of abdominal pain and limitation of surgical expertise, splenectomy was planned. Prior consent for right oophorectomy was also taken if required. At laparotomy, the tissue was purplish, similar in appearance to splenic tissue. The right ovary was found to be adherent to it however it could be easily separated. (Figure 5). Splenectomy was performed and ovary was left in situ. The postoperative period was uneventful. The patient has not complained of any recurrence of the pain in the follow-up visits up to 1 year from the surgery.
Figure 5.
Operative images showing ovary (denoted by *) attached to the spleen attributable to flimsy adhesions and thus could be separated easily.
In our case, it was hypothesized that an element of perisplenitis due to repeated self-limiting episodes of splenic torsion caused its adhesion to the adjacent right ovary. In all the scans available to us, the ovary was adjacent to the wandering spleen and changed locations along with it and may have also undergone incomplete torsion with the spleen.
DISCUSSION
Etiology & Demographics
Wandering spleen is a rare entity (incidence of <0.2%) characterized by absence of splenic tissue at its normal location in the left hypochondrium, and presence of a long vascular pedicle by the virtue of which it is mobile and can be located in any intraabdominal site or more commonly pelvis [1,2,3]. This condition is distinct from conditions like splenosis and accessory spleen [2]. It occurs due to error in the development of the normal supporting ligaments of the spleen with absent or malformed gastrosplenic and splenorenal ligament [2]. It is mostly congenital, can occur in patients of either sex but most frequently presenting at 20–40 years of age. Under the age of 10 years, the male-female ratio is 1:1, but for those older than 10 years, the ratio is 1:7.
Acquired cases are encountered in females of childbearing age group, it is postulated that laxity of ligaments and abdominal walls during pregnancy may have a role to play in it [4,5].
Spleen develops in the dorsal mesogastrium and failure of dorsal mesogastrium to fuse with the posterior parietal peritoneum leads to non-formation of supporting ligaments of the spleen. These include the gastrosplenic, splenorenal and the phrenicolic ligaments. The wandering spleen has an unduly long vascular pedicle which is prone to torsion and resultant splenic infarction [1,2].
Clinical & Imaging findings
This condition may remain asymptomatic in a large proportion of patients and may be detected incidentally on abdominal imaging. It can attract the physicians’ interest as it simulates a mass lesion. The other common manifestation is due to torsion which might present as an acute abdomen or as chronic dull aching pain due to venous congestion caused by intermittent partial torsion and detorsion [6]. Other rare presentations that have been described are mechanical mass effect causing urinary retention and constipation; and pathological disturbances of the spleen including thrombocytopenia, hypersplenism and lymphoma. Still rarer complications include gastric volvulus, variceal hemorrhage and rarely, acute pancreatitis or necrosis due to torsion of mobile pancreatic tail [7].
The classical clinical triad for wandering spleen has been described by Gindrey and Piquard as i) a hard ovoid mass having a notched edge, ii) painless movement of the mass towards the left upper abdomen, with movement in any other direction being painful and unpleasant and iii) resonant note on percussion of the left upper abdomen. However, this entity is rarely suspected clinically and hence overlooked [6,7,8].
An abdominal radiograph may be the first investigation a patient undergoes. Findings of a soft tissue density in central or lower abdomen displacing the surrounding bowel loops with the transverse and descending colon in the left hypochondrium have been described.
In the current scenario, patients with a palpable abdominal mass or abdominal pain invariably undergo an ultrasound examination of the abdomen which reveals an absence of splenic echoes in their normal location with a solid mass and a “hilum” in the region of the palpable swelling [6]. Color doppler can aid in diagnosing torsion and infarction of this wandering spleen which is a surgical emergency [9]. Non visualization of intraparenchymal blood flow with an increased resistive index of the splenic artery > 0.8 is suggestive of splenic infarction [10].
A contrast-enhanced CT is usually the next investigation ordered on seeing a doubtful wandering spleen on sonography or it may be an incidental finding on contrast-enhanced CT. In addition to the information provided by the sonography, the exact course of vessels supplying this ‘mass’ can be traced and findings like the swirling of the pedicle, vascular engorgement, hypo enhancing areas suggesting infarct, vein thrombosis, ascites and adjacent fat stranding implying a torsion can be demonstrated [3,11,12].
MRI using T1 and T2W sequences is a reasonable radiation free alternative to identify wandering splenic tissue; with post contrast T1W scans helping to identify tissue viability. Infarcted tissue appears hyperintense on T2W images with absence of enhancement on post contrast T1W images. MR angiography can help to visualize and evaluate the splenic vascular pedicle [13,14].
A technetium-99m sulphur colloid scan is used to identify ectopic splenic tissue in problematic cases when the splenic architecture is distorted, or the vascular pedicle is not seen [3].
Treatment & Prognosis
Management options for these patients depend on whether the splenic tissue is viable or infarcted, the surgeon going forth with a splenopexy or a splenectomy as indicated [3, 15].
Differential Diagnoses
Wandering spleen needs to be differentiated from other entities.
Accessory spleen/splenunculus
It is a congenital condition where smaller nodules of splenic tissue are seen adjacent to the parent tissue [6]. Splenosis is a similar condition diagnosed in the setting of previous trauma or abdominal surgery.
Absent Spleen
Absence of splenic tissue in the left hypochondrium or elsewhere in abdominal cavity.
Splenogonadal fusion
It is another similar entity although very rare, restricted to isolated case reports. Splenogonadal fusion is of 2 types according to Putschar and Manion classification: continuous and discontinuous [16]. Continuous type: a splenic cord providing a straight anatomic connection between spleen and gonad. It is more commonly associated with other congenital anomalies. Discontinuous type: accessory splenic tissue in a capsulated unit with the gonad. The accessory splenic tissue, in this case, has no connection to the normal spleen.
Embryologically, the spleen develops close to the primordia of gonads and mesonephros. It has been almost exclusively reported in males and on the left side with M: F= 15:1 [17]. A hypothesis for this male preponderance may be due to the inaccessibility of female gonad to examination. In males, it is invariably associated with undescended testes.
TEACHING POINT
Torsion of wandering spleen is a rare surgical cause of acute and recurrent abdominal pain and the radiologist is usually the first to suggest the diagnosis, hence its awareness is of utmost importance. Diagnostic imaging particularly CT is of utmost importance for narrowing the broad possibility for the patient’s nonspecific complain of abdominal pain.
Table 1.
Summary table for wandering spleen.
| Etiology | Error in development of the normal supporting ligaments of the spleen with absent or malformed gastrosplenic and splenorenal ligament, with long vascular pedicle leading to mobile splenic tissue |
| Incidence | <0.2% |
| Gender ratio | Under the age of 10 years, the male-female ratio is 1:1, but for those older than 10 years, the ratio is 1:7. |
| Age predilection | 20–40yrs |
| Risk factors | Congenital condition Acquired-in multiparous females, due to laxity of abdominal wall |
| Treatment | Splenopexy is preferred if splenic tissue is viable, Splenectomy if tissue is infarcted |
| Prognosis | Depends on stage of diagnosis; usually good if detected and corrected in time |
| Findings on imaging |
|
Table 2.
Differential diagnosis table for wandering spleen.
| US | CT | Pattern of contrast enhancement | Scintigraphy (Technitium-99m sulphur colloid scan) | |
|---|---|---|---|---|
| Wandering spleen | Empty left hypochondrium, with splenic echoes seen elsewhere in abdomen | Exact course of vessels and complications can be assessed, in addition to findings on USG. | Usually homogenous enhancement, however in the presence of torsion with infarcts, enhancement is heterogeneous | Increased uptake; identify ectopic splenic tissue in problematic cases, when the splenic architecture is distorted, or the vascular pedicle is not seen. |
| Accessory spleen/ splenunculus | Congenital condition; Smaller solid lesions with echogenicity similar to spleen usually seen adjacent to normally located splenic tissue | Small well-defined solid nodules showing same enhancement as parent spleen | Homogenous, paralleling that of spleen | Increased uptake in parent spleen and splenunculi |
| Splenosis | Acquired condition seen after trauma or surgery; auto implantation of one or more focal deposits of tissue having similar echogenicity as parent splenic tissue | Small well-defined solid nodules showing same enhancement as parent spleen | Homogenous, paralleling that of spleen | Increased uptake in parent spleen and ectopic spleen |
| Absent spleen | Congenital condition, no splenic echoes in left hypochondrium or elsewhere in abdomen/ pelvis | Splenic tissue not seen in the abdomen or pelvis | Not applicable | No uptake seen |
ABBREVIATIONS
- bpm
Beats per minute
- cm
Centimeters
- CT
Computed tomography
- IVU
Intravenous urography
- kVp
Kilovolt peak
- M: F
Male: female ratio
- mAs
Milliampere second
- mm Hg
Millimeters of mercury
- MRI
Magnetic resonance imaging
- T2WI
T2 weighted imaging
- Yrs
Years
REFERENCES
- 1.Varga I, Galfiova P, Adamkov M, Danisovic L, Polak S, Kubikova E, et al. Congenital anomalies of the spleen from an embryological point of view. Medical Science Monitor. 2009 Dec;1:15. [PubMed] [Google Scholar]
- 2.Dahiya N, Karthikeyan D, Vijay S, Kumar T, Vaid M. Wandering spleen: unusual presentation and course of events. Indian Journal of Radiology and Imaging. 2002 Aug;1:12. PMID. [Google Scholar]
- 3.Reisner DC, Burgan CM. Wandering spleen: an overview. Current problems in diagnostic radiology. 2017 Feb 16; doi: 10.1067/j.cpradiol.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Simpson A, Ashby EC. Torsion of the wandering spleen. Br J Surg. 1965 May;52:344–346. doi: 10.1002/bjs.1800520506. [DOI] [PubMed] [Google Scholar]
- 5.Safioleas MC, Stamatakos MC, Diab AI, Safioleas PM. Wandering spleen with torsion of the pedicle. Saudi MedJ. 2007;28(1) [PubMed] [Google Scholar]
- 6.Gordon DH, Burrell MI, Levin DC, Mueller CF, Becker JA. Wandering spleen-the radiological and clinical spectrum. Radiology. 1977 Oct;125(1) doi: 10.1148/125.1.39. [DOI] [PubMed] [Google Scholar]
- 7.Qazi SA, Mirza SM, Muhammad AA, Al Arrawi MH, Al-Suhaibani YA. Wandering spleen. Saudi J Gastroenterol. 2004;10:1–7. [PubMed] [Google Scholar]
- 8.Bourrel P. 3 male cases of ectopic spleen. Ann Chir. 1967;21(23):1415–9. [PubMed] [Google Scholar]
- 9.Liu HT, Lau KK. Wandering spleen: an unusual association with gastric volvulus. American Journal of Roentgenology. 2007 Apr;188(4) doi: 10.2214/AJR.05.0672. [DOI] [PubMed] [Google Scholar]
- 10.Nemcek AA, Jr, Miller FH, Fitzgerald SW. Acute torsion of a wandering spleen: diagnosis by CT and duplex Doppler and color flow sonography. AJR American journal of roentgenology. 1991 Aug;157(2):307–9. doi: 10.2214/ajr.157.2.1853811. [DOI] [PubMed] [Google Scholar]
- 11.Ely AB, Zissin R, Copel L, Vasserman M, Hertz M, Gottlieb P, et al. The wandering spleen: CT findings and possible pitfalls in diagnosis. Clinical radiology. 2006 Nov;1:61. doi: 10.1016/j.crad.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Swischuk LE, Williams JB, John SD. Torsion of wandering spleen: The whorled appearance of the splenic pedicle on CT. PediatrRadiol. 1993;23 doi: 10.1007/BF02012458. [DOI] [PubMed] [Google Scholar]
- 13.Deux JF, Salomon L, Barrier A, Callard P, Bazot M. Acute torsion of wandering spleen: MRI findings. American Journal of Roentgenology. 2004 Jun;182(6):1607–8. doi: 10.2214/ajr.182.6.1821607. [DOI] [PubMed] [Google Scholar]
- 14.Alam A, Ram MS. Torsion of wandering spleen: diagnosis using magnetic resonance imaging. Medical journal, Armed Forces India. 2006 Jan;62(1):81. doi: 10.1016/S0377-1237(06)80169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stringel G, Soucy P, Mercer S. Torsion of the wandering spleen: splenectomy or splenopexy. Journal of pediatric surgery. 1982 Aug 1;17(4):373–5. doi: 10.1016/s0022-3468(82)80492-2. [DOI] [PubMed] [Google Scholar]
- 16.Putschar WGJ, Manion WC. Splenic-gonadal fusion. Am J Pathol. 1956:21. [Google Scholar]
- 17.Garragher AM. One hundred years of splenogonadal fusion. Urology. 1990:35. doi: 10.1016/0090-4295(90)80097-7. [DOI] [PubMed] [Google Scholar]