Abstract
Coronavirus disease 2019 (COVID-19) will have a lasting impact on public health. In addition to the direct effects of COVID-19 infection, physical distancing and quarantine interventions have indirect effects on health. While necessary, physical distancing interventions to control the spread of COVID-19 could have multiple impacts on people living with opioid use disorder, including impacts on mental health that lead to greater substance use, the availability of drug supply, the ways that people use drugs, treatment-seeking behaviors, and retention in care. The degree to which COVID-19 will impact the opioid epidemic and through which of the possible mechanisms that we discuss is important to monitor. We employed simulation modeling to demonstrate the potential impact of physical distancing on overdose mortality.
Keywords: COVID-19, Opioid use disorder, Overdose, RESPOND
1. Background
Coronavirus disease 2019 (COVID-19) will have a lasting impact on public health. In addition to the direct effects of COVID-19 infection, physical distancing and quarantine interventions have indirect effects on health. Socially vulnerable populations, including people living with opioid use disorder (OUD), are at risk for these indirect effects because of their limited social and economic capital.
While necessary, physical distancing interventions to control the spread of COVID-19 could have multiple impacts on people living with OUD. Individuals who are ready to seek treatment may be unwilling to enter a medical setting during a pandemic or may face service closures. People may find it difficult to remain engaged with care and face increased relapse risk. Some programs are using telehealth to reduce barriers (American Psychiatric Association, n.d.; U.S. Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation, 2018), but whether existing office-based addictions treatment can replace capacity with telehealth remains uncertain.
COVID-19 could also increase opioid overdose deaths by disrupting drug supplies, resulting in traffickers using available—and potentially more lethal—substances. Physical distancing may also disrupt drug use partnerships and isolate people when they use, increasing the risk of overdose death (CDC/NCHS, 2018), and restrict naloxone and emergency medical response access. Finally, isolation could negatively impact mental health, potentially causing more people to turn to substance use as a form of coping.
The degree to which COVID-19 will impact the opioid epidemic and through which of the possible mechanisms that we have discussed is important to monitor. We employed simulation modeling to investigate physical distancing impacts on initiation of and retention in medications for opioid use disorder (MOUDs), and consequent impact on overdose mortality over the coming year.
2. Methods
We used the researching effective strategies to prevent opioid death (RESPOND) model to simulate the population living with OUD in Massachusetts (MA). RESPOND is a dynamic population state–transition model that simulates the trajectory of OUD and treatment effects on drug use and overdose. The model is calibrated to historical population size and opioid outcomes in MA, and generates realistic overdose counts (Nolen, White, Wang, et al., 2020).
We assumed that physical distancing and epidemic response measures will have two OUD treatment impacts: 1) decrease the MOUD initiation rate; and 2) lower MOUD retention. We made simplifying assumptions that the impacts of physical distancing are immediate, and also immediately return to pre-COVID levels when physical distancing ends. We initiated the simulation with the OUD population in MA on March 1, 2020, and projected outcomes over one year (March 1, 2021). Because the impact of physical distancing on MOUD initiation and retention is not known, we developed feasible scenarios to investigate trends over time. We assumed three durations of physical distancing interventions (3 months, 6 months, 12 months) and two effect sizes of physical distancing (20% to 40% reduction in MOUD initiation and retention). We report simulated overdose mortality and compare deaths to projected overdose mortality in a counterfactual simulation of “no COVID epidemic.”
3. Results
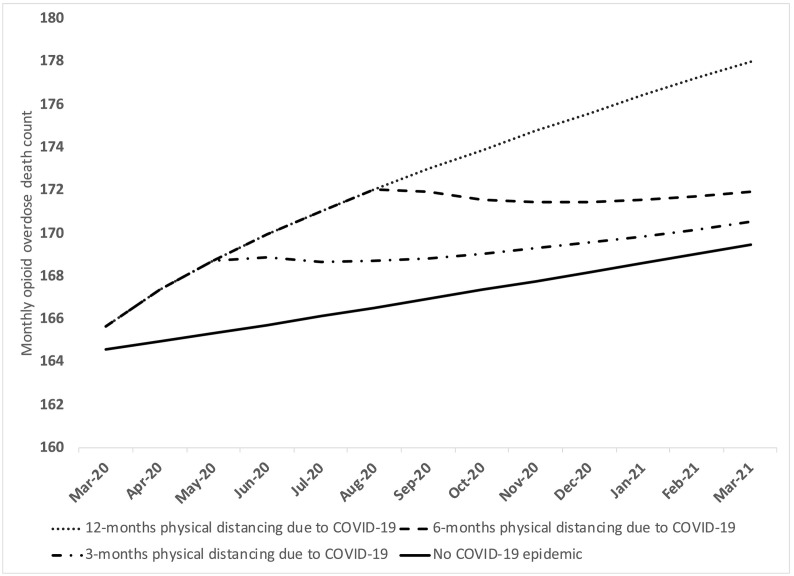
Decreasing treatment initiation and retention rates on MOUD resulted in higher overdose death in MA. Overdose mortality in 2021 remained elevated compared to the counterfactual of “no COVID-19 epidemic,” even when physical distancing measures ended after three months (Fig. 1 ). In every scenario of physical distancing duration and effect, overdose rates remained elevated in March 2021 compared to what we would have expected were we never to have had the COVID pandemic (Fig. 1).
Fig. 1.
Impact of various durations of physical distancing interventions on opioid overdose deaths in Massachusetts March 2020–March 2021.
The horizontal axis reflects simulated calendar time. The vertical axis is denominated in terms of fatal overdose counts. Each line represents a different duration of physical distancing intervention, assuming a 20% reduction in the rate of both initiation onto medications for opioid use disorder, and retention on medications.
4. Discussion
The COVID pandemic will likely have long-term negative implications for the opioid epidemic, resulting in increased overdoses, even if the impacts of COVID-19 on OUD care are modest and relatively short-lived. We likely underestimate the full impact of COVID-19 by not modeling changes to drug supply, social isolation, reduced effectiveness of naloxone, or reduced access to emergency medical services. This analysis is based on feasible scenarios of MOUD use and the impact of COVID-19 on treatment initiation and retention. While it is possible that changes to OUD care delivery, such as telemedicine, could improve OUD care in the future, it is very unlikely that the COVID-19 pandemic will somehow result in increased OUD care seeking at a time when all other healthcare is “on hold.” It is therefore essential that we make all possible efforts now to ensure MOUD treatment access and retention during the physical distancing period through telehealth, naloxone distribution, and peer-to-peer services. Since the COVID-19 epidemic is directly intersecting with an ongoing overdose epidemic, a concentrated effort to address the needs of people living with OUD is critical to enhancing public health during this crisis.
CRediT authorship contribution statement
Linas, BP: Conceptualization, formal analysis, resources, funding acquisition, writing and revising.
Savinika A: formal analysis, project administration, writing and revising.
Barbosa, C: results interpretation writing and revising.
Mueller, PP: results interpretation writing and revising.
Cerda, M: results interpretation writing and revising.
Keyes, K: results interpretation writing and revising.
Chhatwal, J: results interpretation writing and revising.
Funding statement
This work is funded by the National Institute of Drug Addiction R01DA046527, P30DA040500, UM1DA049415, UM1DA049394, UM1DA049412.
References
- American Psychiatric Association. Practice guidance for COVID-19. Available at: https://www.psychiatry.org/psychiatrists/covid-19-coronavirus/practice-guidance-for-covid-19. Accessed March 30, 2020.
- CDC/NCHS, National vital statistics system, mortality. CDC WONDER, Atlanta, GA: US Department of Health and Human Services, CDC; 2018. Available at https://wonder.cdc.gov. Accessed March 27.2020.
- Nolen S., White L.F., Wang J., et al. A population simulation model for opioid policymaking in Massachusetts. Medical Decision Making. 2020;40 [Google Scholar]
- U.S. Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation. Using telehealth to support opioid use disorder treatment. November, 2018. Available at: https://aspe.hhs.gov/system/files/pdf/260276/OUDTeleIB.pdf. Accessed March 27. 2020.