Abstract
Background:
Patellar tendon ruptures have routinely been repaired with transosseous suture tunnels. The use of knotless suture anchors for repair has been suggested as an alternative.
Purpose:
To compare the load to failure and gap formation of patellar tendon repair at the inferior pole of the patella with knotless suture anchor tape versus transosseous sutures. A secondary objective was to investigate whether either technique shows an association between bone density and load to failure.
Study Design:
Controlled laboratory study.
Methods:
A total of 20 human tibias with attached patellar and quadriceps tendons were sharply incised at the bone-tendon junction at the inferior pole of the patella. A total of 10 tendons were repaired using 2 knotless suture anchors in the inferior pole of the patella and a single suture tape with 2 core sutures. The other 10 tendons were repaired using No. 2 suture passed through 3 transosseous tunnels. A distracting force was then applied through the suture in the quadriceps tendon. Gap distance through load cycling at the repair site and maximum load at repair failure were then measured. Bone density was measured using computed tomography scanning.
Results:
No difference was found in the mean load to failure of knotless patellar tendon repair versus transosseous suture repair (367.6 ± 112.2 vs 433.9 ± 99 N, respectively; P = .12). After 250 cycles, the mean repair site gap distance was 0.85 ± 0.45 mm for the knotless patellar tendon repair versus 2.94 ± 2.03 mm for the transosseous suture repair (P = .03). A small correlation, although not statistically significant, was found between bone density and load to failure for the knotless tape repair (R 2 = 0.228; P = .66). No correlation was found between bone density and load to failure for the transosseous repair (R 2 = 0.086; P = .83).
Conclusion:
Suture tape repair with knotless anchors for repair of patellar tendon rupture has comparable load to failure with less gap formation than transosseous suture repair. There is a small correlation between bone density and failure load for knotless anchor repair, which may benefit from further investigation.
Clinical Relevance:
Using knotless suture anchors for patellar tendon rupture repair would allow for a smaller incision, less dissection, and likely shorter operating time.
Keywords: patellar tendon tear, knotless suture tape anchor, transosseous patellar tendon repair, suture tape, bone density
Ruptures of the patellar tendon are rare, accounting for approximately 0.6% of soft tissue musculoskeletal injuries.4 They are most common in males younger than 40 years of age and are usually the result of direct trauma.1 Zernicke et al23 estimated that a healthy tendon can withstand up to 17.5 times a subject’s body weight before failing; however, other factors may predispose patients to tendon rupture, such as chronic renal failure, rheumatoid arthritis, repetitive microtrauma, lupus erythematous, fluoroquinolone use, or history of steroid use.16 Patellar tendon ruptures are categorized into 3 types by location of the rupture: inferior pole of the patella, midsubstance, and tibial tuberosity. The inferior pole of the patella is also referred to as the osteotendinous junction, and ruptures in that location are the most common.2,14 Therefore, we focused our study on repairs of this type of rupture. Surgery is required to fix complete patellar tendon ruptures at the osteotendinous junction.12,15,21 Surgical options include transosseous sutures, primary end-to-end opposition with protective metal wiring, and suture anchors.12
The most commonly used method for a patellar tendon rupture at the inferior pole of the patella is repair via transosseous sutures.10 However, this method is quite invasive and requires exposure of the entire patella and multiple passes through the intact patellar tendon. This may damage the patellar tendon and lengthen recovery time.11 Other drawbacks associated with this procedure include risk of penetrating the articular surface of the patella and the technical difficulty of attaching the patellar tendon anteriorly over the inferior pole of the patella.11
The suture anchor repair is a newer technique that has become commonly and successfully used in the upper extremity for tendon and ligament attachment to bone.2 Suture anchors provide several advantages over the traditional transosseous approach, including the need for a smaller incision, less tissue dissection, shorter operation time, and no involvement of the intact quadriceps tendon.3 Suture anchors are also believed to allow earlier return of range of motion and a faster recovery compared with other techniques.6 In addition to these clinical benefits, suture anchors have been shown to be biomechanically comparable with, if not superior to, the traditional transosseous technique.2,6,14
Another promising, newer surgical technique uses suture tape. Suture tape is composed of similar materials as high-tensile strength suture but is wider and therefore has more surface area. The increased surface area in contact with the tissue theoretically allows for more dispersion of force throughout the repaired tendon.8 In a head-to-head comparison, Gnandt et al9 demonstrated that suture tape had a greater mean load to failure than suture of the same size in both whipstitch and Krackow-stitch models. Using a quadriceps tendon model, Kindya et al13 found that suture anchors with suture tape significantly outperformed transosseous repair and standard suture anchor repair in initial tendon displacement, stiffness, and ultimate load to failure. Although that study demonstrated the benefit of a knotless suture tape repair for the quadriceps tendon, the investigators did not analyze the same suture tape technique on the patellar tendon.13
The aim of our study was to compare the load to failure and gap formation of patellar tendon repair at the inferior pole of the patella with knotless suture anchor tape versus transosseous sutures. A secondary objective was to investigate whether either of these techniques would show an association between bone density and load to failure. We hypothesized that there would be no difference in load to failure between knotless anchor fixation using suture tape versus transosseous repair for inferior pole patellar tendon rupture and that knotless tape repair would result in less gap formation. Additionally, we hypothesized that there would be a correlation between load to failure and bone density with the suture anchor repair.
Methods
The biomechanics laboratory at Louisiana State University Health provided 20 fresh-frozen cadaveric human tibias with attached patellar tendon, patella, and quadriceps tendon harvested from fresh-frozen cadavers. Before testing, computed tomography (CT) scanning was performed to establish bone density. After CT scanning, the patellar bones were segmented in 3D Slicer (www.slicer.org), and mean density was measured in Hounsfield units (HU) using the built-in quantification tool.7
The tibial components of the specimens were potted using Bondo polyester resin (Bondo Corporation) in metal boxes. The patellar tendons were sharply incised with a scalpel at the bone-tendon junction at the inferior pole of the patella. Excess tissue was then debrided from the inferior pole of the patella to allow for accurate placement of sutures and anchors as well as to allow for more accurate testing measurements.
A total of 10 patellar tendons were repaired using a single suture tape (Fibertape, Arthrex, Naples, FL) and 2 knotless suture anchors (4.75 mm; SwiveLock, Arthrex) placed in the inferior pole of the patella, based on a method previously described.13 To do this, the suture tape was started by passing the attached needle through the proximal end of the tendon, either medially or laterally. Next, 5 Krackow stitches were made with the tape running distally down the side of the tendon. Another 5 Krackow stitches were then made with the tape running proximally up the opposite side of the tendon, leaving 2 strands coming out of the proximal aspect of the tendon. All the suture in the soft tissue was pretensioned by the same surgeon (P.A.M.) A drill and tap were then used at the junction of the medial and middle third and junction of the lateral and middle third of the inferior pole of the patella to prepare the bone for the suture anchor. Each end of the suture tape was loaded within the eyelet of the suture anchor going into the respective side of the patella. It should be noted that the tape was initially loaded with all of the slack pulled out of the tape so that the eyelet was juxtaposed to the cut end of the tendon. When malleting the anchor handle, it was observed that the tape cut into the bone and caused the anchor to pull out. To prevent this, the tape was loaded with 20 mm of slack for all repairs to accommodate the 20-mm insertion stem for the 19.1--mm length anchor (Figure 1).
Figure 1.
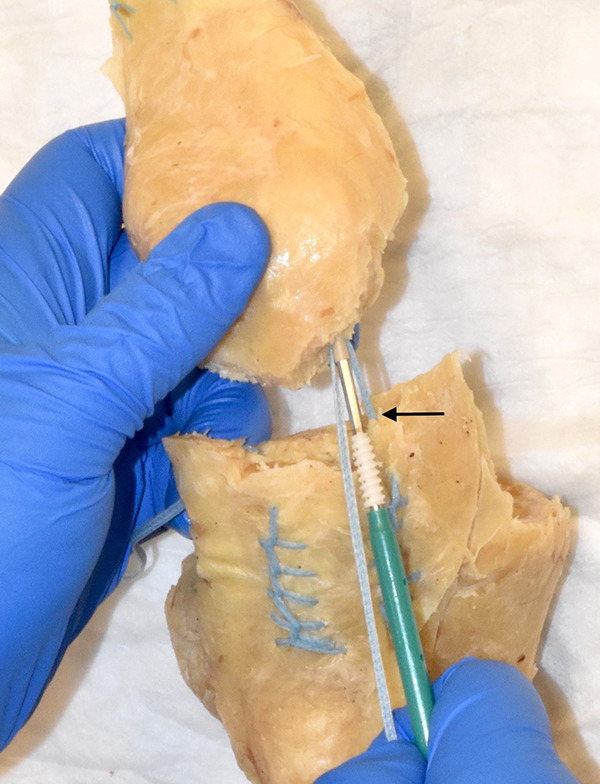
A knotless anchor patellar repair. The black arrow denotes the 20 mm of slack preloaded into the polyethylene tape between the eyelet and the tendon. The tape is then locked on the slots of the insertion handle before insertion of the metal shaft into the predrilled patellar holes. This slack was preloaded to prevent the tape from cutting into the bone.
The slack was preloaded so that before insertion of the anchor, there was 20 mm of tape between the eyelet and the tape-tendon junction. When the driver was inserted fully, this placed the tendon directly on the patellar bone without the tape cutting into the inferior pole of the patella. The final portion of the anchor was then screwed into the patella to complete its placement. The surgeon passed the additional core suture through the proximal tendon and tied the suture using a surgeon’s knot with 7 throws (Figures 2A and 3A). The single suture tape technique was selected, as it has been described by previous surgeons.13 Also, the suture tape offers the benefit of minimizing the suture burden for the tendon, and it would be difficult to fit 2 sets of suture tape in a single tendon.
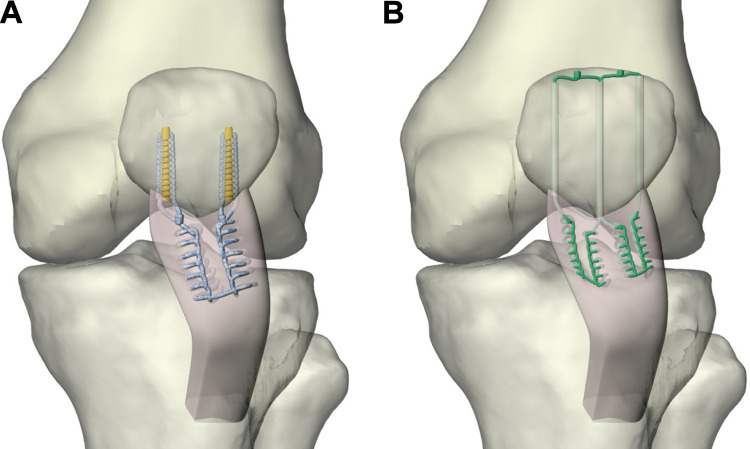
Figure 2.
Three-dimensional illustration of patella tendon repair techniques. (A) Left patellar tendon knotless tape repair with 1 polyethylene tape and 2 knotless anchors inserted into the inferior pole of the patella. The repair is supplemented with 2 core sutures from each anchor. (B) Left patellar tendon transosseous repair. A total of 3 transosseous holes are drilled through the patella, and 4 sutures are passed through these holes with 2 knots tied over the superior pole of the patella.
Figure 3.

Patella tendon cadaver repair constructs for biomechanical testing. (A) A left patellar tendon knotless tape repair with 1 polyethylene tape and 2 knotless anchors inserted into the inferior pole of the patella. The repair is supplemented with 2 core sutures from each anchor. (B) A right patellar tendon transosseous repair. A total of 3 transosseous holes are drilled through the patella, and 4 sutures are passed through these holes with 2 knots tied over the superior pole of the patella.
A total of 10 tendons were repaired using two No. 2 high-strength sutures (Fiberwire, Arthrex, Naples, Florida) passed through transosseous tunnels. Krackow suturing was performed in the same fashion as the tendons repaired with suture anchor. However, each suture was run proximally up the central aspect of the tendon for 5 throws, again using 5 Krackow stitches, leaving 4 suture tails. A 2.0-mm drill was then used to create 3 longitudinal tunnels in the medial, lateral, and central aspects of the patella from distal to proximal. A beath pin was used to pass the suture ends through their respective tunnels. The 2 central strands were both passed through the middle tunnel. The suture ends were then pulled taut so that the tendon was reapproximated to the inferior pole of the patella. The ends were then tied to their respective ends over the superior aspect of the patella using a surgeon’s knot with 7 throws (Figures 2B and 3B). The transosseous technique was used as a control because it is consistent with multiple described, previously tested techniques.6,14 All knots were tied by the same orthopaedic surgeon (P.A.M.), who also tied the knots for the tendons repaired with tape and anchors. Two No. 2 high-strength sutures were then passed in a similar fashion, using the Krackow stitch, through the intact quadriceps tendon. A loop was left in the ends of both tied sutures to allow for attachment of the testing devices.
The repairs were tested using a servohydraulic testing machine (model 8874; Instron). The tibial bones were anchored to the machine frame while the quadriceps tendon was loaded in tension through a No. 2 high-strength suture, which was Krackow stitched through the quadriceps tendon (Figure 4). The knees were tested in a simulated fully extended position. This position was chosen to decrease the variability in the data. In addition, at our institution, the postoperative protocol for patellar tendon repair includes initial immobilization with the knee locked in extension, so our study mimics this time-zero, early healing phase. Our study methods were similar to the studies performed by Ettinger et al6 and Sherman et al,19 which allows our results to be compared with previously published biomechanical data.
Figure 4.
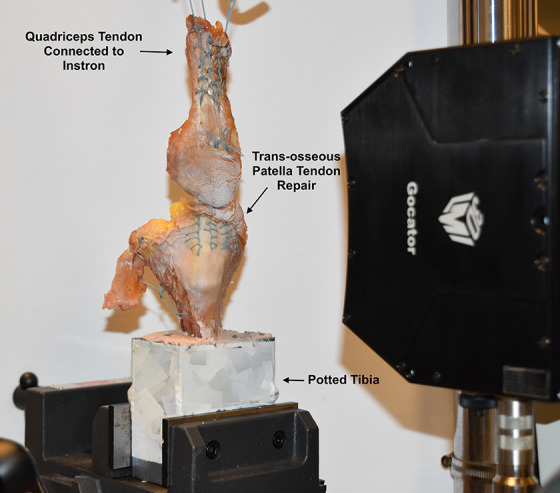
A right transosseous patellar tendon repair specimen loaded in the Instron testing machine. The tibia is potted, and the quadriceps is attached to a tension device via suture.
Before testing, each construct was tensioned at 80 N to tighten the sutures. The testing was performed in 2 phases. In the first phase, we tested the repair for fatigue applying a sinusoidal load ranging from 20 to 60 N at a frequency of 1 Hz for a total of 250 cycles. The second phase evaluated the strength to failure by applying a ramp load at a rate of 20 mm/s. During testing, the tendon gap was measured using a 3-dimensional snapshot sensor (Gocator 3506) configured to capture a field of view of 27 × 45 mm with a resolution of 20 µm and an accuracy of 12 μm. To reduce glare during image acquisition, the tissues were sprayed with Zinc Stearate Facsure NDT Developer (Weld-Aid Products). Tendon gapping was monitored at 0, 20, 125, and 250 cycles. To measure the tendon gap, the middle third of the patellar bone was discretized in vertical sections with 100-µm spacing, and the largest measured gap was used as measure for the study (Figure 5).
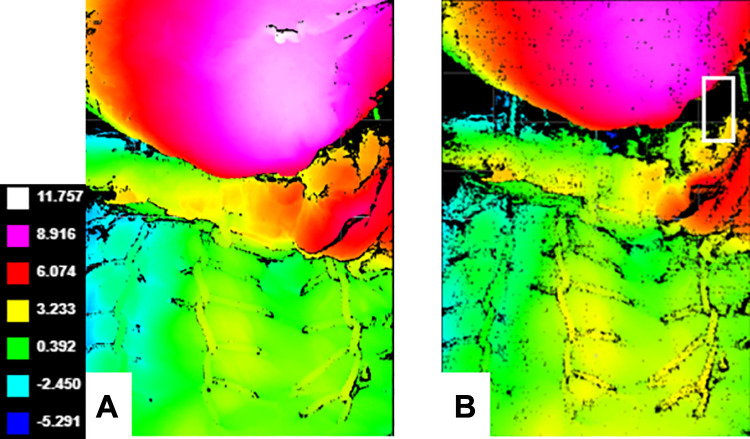
Figure 5.
Right transosseous patellar tendon repair. The patella is colored pink and red while the patellar tendon is green. Construct shape and deformation were captured by a high-resolution 3-dimensional scanner. (A) Color mapping images of a patellar tendon repair. The distance represents the distance along the axis of the scanner. (B) Color mapping images of patellar tendon gapping after failure. The white rectangle is around the area with the largest measured gap within the central third of the patella.
Additional values of stiffness and energy to failure were calculated with the resultant force-displacement graphs.
Statistical Analysis
An a priori power analysis was performed to determine the number needed in each group, as well as a post hoc power analysis. Descriptive data such as age and sex of the cadavers were compared using 2-sample t test and chi-square test, respectively. Biomechanical data such as load, stiffness, and gapping were compared between the 2 groups using 2-sample t test. The relationship between bone density (HU) and the load to failure was determined using the coefficient of determination (R 2).
Results
Drawing on a previous study13 that compared knotless suture tape tendon repair versus transosseous suture for the quadriceps tendon, we performed an a priori power analysis.12,17,23 The number needed for a 1 – B of 0.8 was determined to be 5 in each group. A post hoc power analysis on gapping after 250 cycles was performed. With a sample size of 10 in each group, it was determined that 1 – B was 0.94.
The mean age of the cadaveric specimens in the transosseous suture repair group was 62.1 ± 4.1 years, which was not significantly different from the age of 65.5 ± 12 years in the knotless repair group (P = .40). There were 6 female and 4 male cadaveric knees in the transosseous suture repair group versus 7 female and 3 male knees in the knotless repair group, with no significant difference in sex distribution between groups (P = .64).
Load to Failure
No difference was found in the mean load to failure of knotless patellar tendon repair versus transosseous suture repair: 367.6 ± 112.2 versus 433.9 ± 99 N, respectively (P = .12) (Figure 6). All 10 of the knotless repairs failed due to screw pullout, whereas all 10 of the transosseous suture repairs failed due to suture breakage. A significant difference was found in the mode of failure between both groups (P < .001). Stiffness in the 2 groups was 36.7 ± 10 versus 33.7 ± 8.5 N/mm, respectively (P = .7). Energy to maximum load in the 2 groups was 10.6 ± 6.5 versus 10.8 ± 4.4 J, respectively (P = .9).
Figure 6.
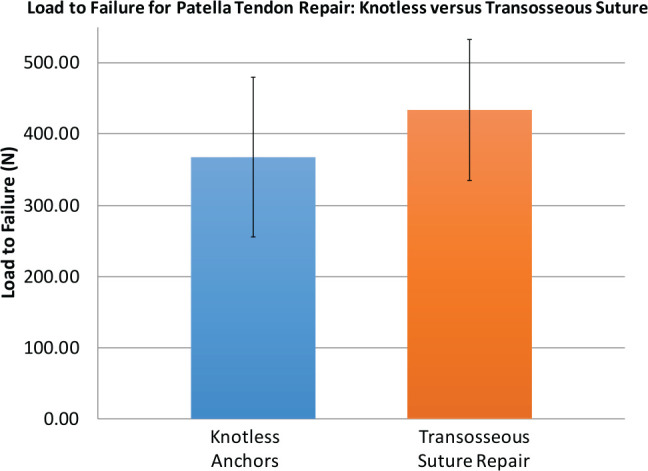
Load to failure for knotless anchor repair with polyethylene tape versus transosseous suture repair. No difference was found in the mean load to failure of knotless patellar tendon repair versus transosseous suture repair (P = .12). SD is represented by error bars.
Gapping
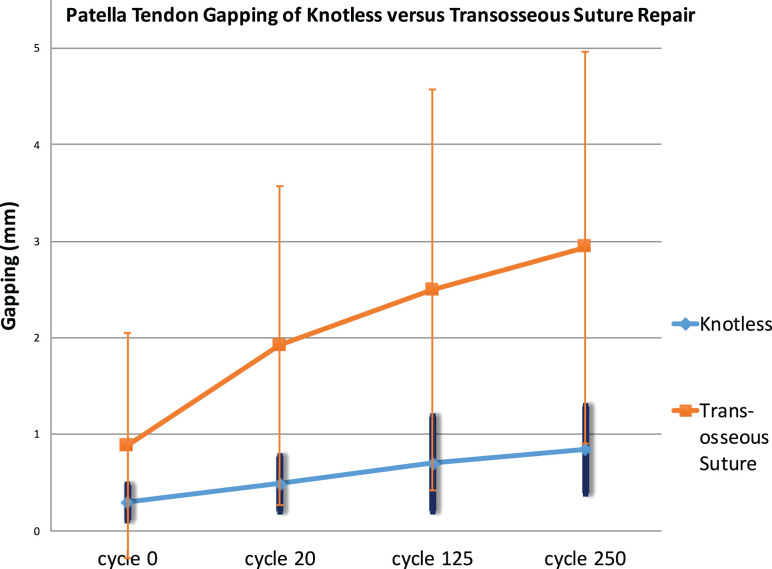
After completion of the repair, the mean repair gap was 0.30 ± 0.18 mm for the knotless patellar tendon repair versus 0.89 ± 1.17 mm for the transosseous suture repair. No statistical difference was found in the tendon repair gap distance immediately after the repair between both groups (P = .23). The knotless patellar tendon repair had a significantly smaller gap distance as soon as 20 cycles (P = .04) as well as at 125 cycles (P = .015). After 250 cycles, the increase in gap distance was larger for the transosseous suture repair versus the knotless patellar tendon repair (increase of 2.16 ± 1.25 vs 0.55 ± 0.44 mm; P = .01). After 250 cycles, the mean repair site gap distance was 0.85 ± 0.45 mm for the knotless patellar tendon repair versus 2.94 ± 2.03 mm for the transosseous suture repair (P = .03) (Figure 7). Although the knotless group had less gapping, both the knotless group and transosseous group had increased gapping after 250 cycles (P = .01 and P = .001, respectively).
Figure 7.
Patellar tendon gapping after transosseous versus knotless repair. Gapping was measured after 0, 20, 125, and 250 cycles. After 250 cycles, the increase in gap distance was larger for the transosseous suture repair versus the knotless patellar tendon repair (increase of 2.16 ± 1.25 vs 0.55 ± 0.44 mm, respectively; P = .01). SD is represented by error bars.
Bone Density
No difference was found in the bone density of the patellae in the knotless repair versus transosseous repair groups (P = .39) (see Table 1). We noted a small correlation, although not statistically significant, between bone density and load to failure for the knotless tape repair (R 2 = 0.228; P = .66). No correlation was seen between bone density and load to failure for the transosseous repair (R 2 = 0.086; P = .83).
TABLE 1.
Patellar Bone Density in Hounsfield Units (HU) for Knotless Anchor Versus Transosseous Suture Patellar Tendon Repair
| Repair Type | Bone Density, HU, mean ± SD | R 2 | P Value |
|---|---|---|---|
| Knotless anchors | 270 ± 53 | 0.228a | .66 |
| Transosseous suture | 234 ± 53 | 0.086a | .83 |
| P value | .39 |
aCorrelation coefficient of each group is reported for the relationship of bone density and load to failure.
Discussion
The current study showed the knotless anchor tape repair had less repair site gap formation compared with the transosseous suture repair; however, there was no significant difference in load to failure. Additionally, we found no significant difference in stiffness or energy until failure.
Previous biomechanical comparisons between knotted suture anchors and transosseous sutures have measured the gap formation and the mean load to failure for patellar tendon repair. Overall, the results have been mixed. For the mean load to failure, Bushnell et al2 found no significant difference among their suture anchor group (779 N), transosseous Fiberwire group (730 N), and transosseous Ethibond group (763 N). Ettinger et al6 tested 2 suture anchor groups, titanium (597 N) and hydroxyapatite (689 N), with both having a significantly higher average load to failure than their transosseous group (301 N). Lanzi et al14 also found higher average load to failure in their suture anchor group (669 N) than in their transosseous group (582 N).
Sherman et al19 compared a 3-corkscrew anchor group (258.8 N) versus a transosseous tunnel group (287 N) with no significant differences in gapping or load to failure. Similar to Bushnell et al2 and Sherman et al,19 we found no significant difference in mean load to failure between our suture anchor group (367 N) and our transosseous group (433 N). Our load-to-failure values for knotless anchor were lower than those reported by Bushnell et al; however, 4 Fiberwire sutures were used in that study, whereas we used a single suture tape for the anchor repairs in the current study. Interestingly, our values were higher than those reported by Sherman et al,19 even though their study used 3 anchors versus 2 in our study. The main differences in this study are the use of suture tape as well as the knotless anchor fixation type of the tape versus a threaded corkscrew anchor. Additionally, different methods of testing the repair may account for the difference in reported values. Another aspect to consider for both studies is increased suture burden to the soft tissue when more suture strands are used.
Bushnell et al2 found that suture anchors (4.1 mm) had significantly less gap formation than either the Fiberwire (6.7 mm) or Ethibond (8.5 mm) transosseous groups at 250 cycles. Ettinger et al6 also found significantly less gap formation in both of their suture anchor groups, titanium (2.9 mm) and hydroxyapatite (3.7 mm), compared with the transosseous group (17.2 mm) over the first 20 cycles. Lanzi et al14 found that suture anchors (2.16 mm) had significantly less gap formation than transosseous sutures (5.71 mm) after 1000 cycles. Sherman et al19 tested patellar tendon suture anchor repair versus transosseous repair, showing no difference in gapping at the end of their study (2.92 and 3.33 mm, respectively; P = .120).
The transosseous repair group in our study had a large amount of gapping variability, whereas the knotless tape repair group had much less variability. This may be due to asymmetric tensioning of suture limbs in the transosseous group. This increased variability may also be due to the increased working length of the suture compared with the knotless tape repair; perhaps the much longer suture material that is run through the entire length of the patella allows more length for variability.
Although our study showed less gap formation with the anchor tape repair, our gap values were also smaller after 250 cycles compared with the studies that tested to similar cycle numbers.19 These differences may be accounted for by individual repair technique, method of measuring gap, or the technique used to stress the repair. Gelberman et al8 found that gapping of >3 mm had a significant effect on accrual of strength and stiffness with time in tendon repairs.
One study evaluated knotless suture tape repair of the quadriceps tendon but did not evaluate patellar tendon repairs. Kindya et al13 compared transosseous tunnels, threaded anchors, and knotless anchors with suture tape. They demonstrated results similar to those of our study, with the knotless tape construct showing less gapping than the other groups. However, Kindya et al showed a higher load to failure for the knotless tape group, whereas our study showed no difference with respect to load to failure. Sherman et al20 showed that a threaded suture anchor repair had less gap formation than a transosseous suture (7.7 vs 10.7 mm, respectively), although they reported similar ultimate loads to failure (286.0 vs 250.5 N, respectively). However, Sherman et al20 used 3 suture anchors with 3 Fiberwire sutures for the suture anchor group and used 3 Fiberwire sutures for the transosseous suture group. Our study used only 2 suture anchors and a suture tape, instead of wire, to balance the theoretical trade-offs of distributing stress within the tendon while minimizing further tissue damage with more needle passes.
Although several previous biomechanical comparisons have found superiority in suture anchors compared with transosseous suture2,6,14 as well as suture tape compared with traditional suture,9 we found that they were comparable, with the exception of repair site gapping. Although evidence indicates that suture anchors can outperform transosseous sutures biomechanically, Roudet et al18 suggested that the clinical evidence thus far does not demonstrate superiority of either technique. Regardless of whether suture anchors are biomechanically superior or noninferior to transosseous sutures, suture anchors are less invasive, involve less dissection, and entail a shorter operating time, making them an enticing option for surgeons. More specifically, the transosseous tunnels require access to the proximal and distal aspects of the patella, requiring longer and larger dissection and subsequent closure.5 Suture anchor fixation has also shown favorable clinical results. Colombelli et al5 reported good to excellent results at 12-month follow-up in patients with quadriceps or patellar tendon rupture treated with suture anchor fixation, with no major complications. However, further clinical trials should be performed comparing transosseous sutures versus suture anchors with suture tape to determine whether the surgical advantages are worth the increased cost and whether suture tape is more effective in pathologic tendons.
Our secondary research question analyzed the bone density of our specimens to see whether there was a correlation with load to failure. In the upper extremity, it has been demonstrated that increased bone density correlates with increased pull-out strength of suture anchors.22 Our results did show a small correlation between load to failure and bone density in repairs performed with anchors and suture tape. This relationship was not present between bone density and transosseous repairs. This may indicate that suture anchor repair would have a higher load to failure for younger patients with higher bone density; the cadaveric specimens we used were from people in their 60s, whereas injured patients are typically younger. Further studies could be performed to see whether there is an age–bone density correlation with anchor fixation or whether there is a density threshold for the use of suture anchors.
Limitations
Limitations to our study include the use of cadaveric tissue, which is a limitation shared by many biomechanical studies. First, cadaveric tissue does not exhibit any healing processes that might affect outcomes as clinical trials progress; however, it does simulate a time zero repair. Second, although being able to strip away all other connective tissue except the tendon being tested is useful in isolating the strength of the repair, it does not necessarily directly correlate with how a repair will perform when acted upon by the surrounding tissue, such as the extensor retinaculum, in a real patient. Third, we manufactured these tendon ruptures in donor tendons. Therefore, it was not known whether predisposing conditions that can result in a patellar tendon rupture or attenuation were present, which could affect the suture-tendon interface. Although suture tape with suture anchors was comparable with transosseous sutures in our study, perhaps in clinical trials where some of the affected tendons have preexisting pathology, the extra width and surface area of the suture tape will allow it to have a more secure suture-tendon interface.
Another set of limitations entailed the 2 techniques used. The knotless suture tape repair involved a single suture tape with 2 core sutures, whereas the transosseous repair used 2 sets of suture. As mentioned previously, the single suture tape technique was selected because it has been described by previous surgeons.13 Also, the suture tape offers the benefit of minimizing the suture burden for the tendon, and it would be difficult to fit 2 sets of suture tape in a single tendon. The transosseous technique was used as a control because it is consistent with multiple described, previously tested techniques.6,14
Conclusion
Suture tape repair with knotless anchors for patellar tendon rupture repair has comparable load to failure as transosseous suture repair, with less gap formation. We found a small correlation between bone density and failure load for knotless anchor repair that may benefit from further investigation.
Acknowledgment
We acknowledge Alan Ogden for his assistance in scanning and testing the patellar tendon construct as well as Anna Hoefler for her assistance with manuscript preparation.
Footnotes
Final revision submitted March 31, 2020; accepted April 14, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: P.A.M. has received faculty/speaker fees from Aastrom Biosciences and honoraria from Vericel. R.S.B. has received educational support from Midsouth Orthopedics, consulting fees from Zimmer Biomet, and hospitality payments from Arthrex and Zimmer Biomet. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the LSU Institutional Review Board.
References
- 1. Albuquerque RP, Prado J, Hara R, et al. Estudo epidemiológico das rupturas tendinosis do mecanismo extensor do joelho em um hospital de nível I. Rev Bras Ortop. 2012;47:719–723.27047890 [Google Scholar]
- 2. Bushnell BD, Byram IR, Weinhold PS, Creighton RA. The use of suture anchors in repair of the ruptured patellar tendon: a biomechanical study. Am J Sports Med. 2006;34(9):1492–1499. [DOI] [PubMed] [Google Scholar]
- 3. Capiola D, Re L. Repair of patellar tendon rupture with suture anchors. Arthroscopy. 2007;23(8):906.e901–e904. [DOI] [PubMed] [Google Scholar]
- 4. Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39(12):1338–1344. [DOI] [PubMed] [Google Scholar]
- 5. Colombelli A, Polidoro F, Guerra G, Belluati A. Patellar and quadriceps tendons acute repair with suture anchors. Acta Biomed. 2019;90(suppl 1):209–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ettinger M, Dratzidis A, Hurschler C, et al. Biomechanical properties of suture anchor repair compared with transosseous sutures in patellar tendon ruptures: a cadaveric study. Am J Sports Med. 2013;41(11):2540–2544. [DOI] [PubMed] [Google Scholar]
- 7. Fedorov A, Beichel R, Kikinis R, et al. 3D slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging. 2012;30(9):1323–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gelberman RH, Boyer MI, Brodt MD, Winters SC, Silva MJ. The effect of gap formation at the repair site on the strength and excursion of intrasynovial flexor tendons: an experimental study on the early stages of tendon-healing in dogs. J Bone Joint Surg Am. 1999;81(7):975–982. [DOI] [PubMed] [Google Scholar]
- 9. Gnandt RJ, Smith JL, Nguyen-Ta K, McDonald L, LeClere LE. High-tensile strength tape versus high-tensile strength suture: a biomechanical study. Arthroscopy. 2016;32(2):356–363. [DOI] [PubMed] [Google Scholar]
- 10. Greis PE, Holmstrom MC, Lahav A. Surgical treatment options for patellar tendon rupture, part I: acute. Orthopedics. 2005;28(7):672–679. [DOI] [PubMed] [Google Scholar]
- 11. Ho HM, Lee WK. Traumatic bilateral concurrent patellar tendon rupture: an alternative fixation method. Knee Surg Sports Traumatol Arthrosc. 2003;11(2):105–111. [DOI] [PubMed] [Google Scholar]
- 12. Kellersmann R, Blattert TR, Weckbach A. Bilateral patellar tendon rupture without predisposing systemic disease or steroid use: a case report and review of the literature. Arch Orthop Trauma Surg. 2005;125(2):127–133. [DOI] [PubMed] [Google Scholar]
- 13. Kindya MC, Konicek J, Rizzi A, Komatsu DE, Paci JM. Knotless suture anchor with suture tape quadriceps tendon repair is biomechanically superior to transosseous and traditional suture anchor-based repairs in a cadaveric model. Arthroscopy. 2017;33(1):190–198. [DOI] [PubMed] [Google Scholar]
- 14. Lanzi JT, Felix J, Tucker CJ, et al. Comparison of the suture anchor and transosseous techniques for patellar tendon repair: a biomechanical study. Am J Sports Med. 2016;44(8):2076–2080. [DOI] [PubMed] [Google Scholar]
- 15. Ravalin RV, Mazzocca AD, Grady-Benson JC, Nissen CW, Adams DJ. Biomechanical comparison of patellar tendon repairs in a cadaver model: an evaluation of gap formation at the repair site with cyclic loading. Am J Sports Med. 2002;30(4):469–473. [DOI] [PubMed] [Google Scholar]
- 16. Rosa B, Campos P, Barros A, Karmali S, Goncalves R. Spontaneous bilateral patellar tendon rupture: case report and review of fluoroquinolone-induced tendinopathy. Clin Case Rep. 2016;4(7):678–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rosner B. Fundamentals of Biostatistics. Cengage Learning; 2015. [Google Scholar]
- 18. Roudet A, Boudissa M, Chaussard C, Rubens-Duval B, Saragaglia D. Acute traumatic patellar tendon rupture: early and late results of surgical treatment of 38 cases. Orthop Traumatol Surg Res. 2015;101(3):307–311. [DOI] [PubMed] [Google Scholar]
- 19. Sherman S, Black B, Mooberry M, et al. Biomechanical evaluation of suture anchor versus transosseous tunnel patellar tendon repair techniques. J Knee Surg. 2019;32:825–832. [DOI] [PubMed] [Google Scholar]
- 20. Sherman SL, Copeland ME, Milles JL, Flood DA, Pfeiffer FM. Biomechanical evaluation of suture anchor versus transosseous tunnel quadriceps tendon repair techniques. Arthroscopy. 2016;32(6):1117–1124. [DOI] [PubMed] [Google Scholar]
- 21. Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am. 1981;63(6):932–937. [PubMed] [Google Scholar]
- 22. Tingart MJ, Apreleva M, Zurakowski D, Warner JJ. Pullout strength of suture anchors used in rotator cuff repair. J Bone Joint Surg Am. 2003;85(11):2190–2198. [DOI] [PubMed] [Google Scholar]
- 23. Zernicke RF, Garhammer J, Jobe FW. Human patellar-tendon rupture. J Bone Joint Surg Am. 1977;59(2):179–183. [PubMed] [Google Scholar]