Abstract
Background:
Inter-professional collaboration (IPC) is an important prerequisite for successful patient care. Even though inter-professional education (IPE) is increasingly common in undergraduate medical education, few IPE approaches explicitly address the IPC among medical students and students of psychology. IPE videos can be used to give learners the opportunity to gather relevant knowledge from different professional perspectives. So far it has been unclear whether it is enough when the topic of the video itself is inter-professional or if it is necessary for experts from different professions explicitly to appear in the video.
Methods:
In an online experiment, medical students watched 1 of 2 videos about Parkinson’s disease (PD) and the care of PD patients. The information was either provided by protagonists from only 1 profession (ie, physicians; mono-professional condition) or provided by protagonists from 2 different professions (ie, physicians and a psychologist; inter-professional condition). Attitude toward inter-professional interaction and learning, evaluation of the entertaining and illustrative character of the video, attitude toward physicians and psychologists, importance of IPC, evaluation of psychological treatment support, and knowledge acquisition served as dependent variables.
Results:
The analysis was based on 140 participants (74 in the mono-, 66 in the inter-professional condition). We found that the inter-professional video was perceived to be more entertaining than the mono-professional video (t(138) = −2.227; P = .028; d = 0.38). The inter-professional video was also considered to be more illustrative (t(138) = −6.269; P < .001; d = 1.06). Moreover, participants improved their attitude toward physicians by watching the video (F(1,138) = 4.860, P < .001, η2p = 0.11), but they did not change their attitude toward psychologists (P = .146). Participants who watched the inter-professional video considered IPC to be more important than participants who watched the mono-professional video (t(138) = −7.954; P < .001; d = 1.354). Finally, the inter-professional video led to better performance in the knowledge test (t(138) = −2.285; P = .024; d = 0.04).
Conclusion:
Inter-professional videos showing explicitly the appearance of experts from different professions come along with several advantages. We discuss the implications of their application in educational practice.
Trial registration:
The study was pre-registered on the pre-registration platform AsPredicted (aspredicted.org) before we began data collection (registration number: #33143). The pre-registration document can be accessed via the following link: https://aspredicted.org/blind.php?x=gd5hd8.
Keywords: Inter-professional collaboration, inter-professional education, medical students, video, experimental study, deep brain stimulation, Parkinson’s disease
Background
In the health-care sector, inter-professional collaboration (IPC) is an important requirement for patient safety1 and for a high quality of patient care.2,3 Therefore, the implementation of inter-professional training in medical education is continually more in demand.4-6 Many patients are in contact with representatives from several health professions, and especially many chronic patients have a need for both medical and psychological support. Patients with chronic diseases have often co-morbid illnesses—as is the case for patients with Parkinson’s disease (PD). PD “is associated with substantial physical and mental co-morbidity” (p. 1).7 The cardinal symptoms in PD are motor symptoms (tremor, bradykinesia, rigidity, and postural instability).8 In addition, PD is often associated with non-motor symptoms like autonomic dysfunctions9 and/or psychiatric conditions like dementia, depression, and anxiety.7,10 Some treatment options, like deep brain stimulation (DBS), are very sophisticated and should be accompanied by an inter-professional team. DBS is a neurosurgical procedure used to alleviate symptoms of PD that involves the implantation of remote-controlled electrodes into certain brain areas.11 Since this surgery often comes along with strong anxiety12 and alterations of affect,13 interprofessional treatment, including psychologists for example, is recommended.14 This example illustrates the importance of smooth IPC between medical doctors and psychologists in clinical practice.
Ward et al15 have requested that “Psychologists must embrace their identity as health professionals and engage their learners in IPE [interprofessional education] so that the emerging cognitive schemata of healthcare that is developed includes the profession of psychology” (p. 250). These authors are concerned that otherwise “healthcare teams and health professionals will not understand the value, roles, or potential contributions of psychologists in enhancing patient care outcomes.” (p. 250). At first glance, this concern seems rather surprising, as the medical and psychological professions are already somewhat associated. Psychologist have been working in medical schools in clinical (eg, clinical intervention, diagnosis) as well as non-clinical fields (eg, research, teaching) for more than 100 years.16 However, psychologists are not necessarily directly involved in IPE activities. The Interprofessional Education Collaborative, for example, developed their first report about the core competencies for collaborative practice in 2011 without involving psychologists at all. Only the updated version from 2016 integrated input from the American Psychological Association.17 Even though IPE settings are more and more common in undergraduate medical education, only a few IPE programs17-20 explicitly address the IPC among medical students and students of psychology. But there is great demand for IPE settings that integrate psychological and medical perspectives.21
Videos in medical education
One approach toward integrating psychological and medical perspectives in an IPE context is the provision of educational videos. Videos are already widely used in health communication22,23 and medical education, because they are an illustrative teaching format24,25 and are effective for teaching procedural knowledge.26,27 Recent findings indicate that video formats show great potential for the acquisition of inter-professional competences28 and are considered to be relevant for inter-professional learning. This can be explained on the basis of Bandura’s social learning theory, especially with regard to the fact that observational learning is suitable for the acquisition of social behavior.29,30 The observation of successful communication among professionals from different fields could therefore have an impact on both the acquisition of knowledge and the attitude toward interprofessional work. Furthermore, videos provide learners with the opportunity to capture the big picture31 and therefore to develop metacognitive competences that are relevant for IPC.32 At the same time, the protagonists’ professional identity influences how information is processed by the viewers.33 Videos are relatively easy to implement and could provide the opportunity for students to experience medical and psychological role models in related clinical settings. In a previous study,28 medical and physiotherapy students watched the same video that was interprofessional in 2 ways: The topic truly required an interprofessional approach, and protagonists from 2 different health professions appeared as role models. So far it has been unclear whether it is sufficient for making viewers learn about IPC and improving their attitude toward IPC and the collaborating professions simply to have the topic of the video be interprofessional, or if it is additionally necessary to have experts from multiple different professions explicitly appear in the video. To answer this research question, we investigated the impact of 2 different presentation formats in a medical video that dealt with a highly interprofessional topic: The procedures and treatments for DBS surgery34 for patients with PD.35 The 2 conditions differed only in the video’s presentation format: While 1 video presented a surgical procedure and discussion about this surgery among physicians only (mono-professional condition), the other video used the same material but additionally included a psychologist in the discussion (inter-professional condition).
Hypotheses
Based on social learning theory29,30 we hypothesized that presentation format (mono-professional vs inter-professional) would have an impact on people’s attitudes toward IPC. We hypothesized that the attitude of participants in the inter-professional condition toward inter-professional interaction (Hypothesis 1a) and inter-professional learning (Hypothesis 1b) would improve more than that of participants in the mono-professional condition.
Furthermore, we hypothesized that the presentation format would have an impact on the evaluation of the videos. The mono-professional presentation is more consistent with medical students’ previous perspective and requires less mental effort.36 An inter-professional video, in contrast, provides different perspectives, and explicitly observing role-models from different professions might therefore be considered more vivid and concrete. Thus, we hypothesized that the video in the inter-professional condition would be evaluated as more entertaining (Hypothesis 2a) and more illustrative of inter-professional collaboration (Hypothesis 2b) than in the mono-professional condition.
DBS is pertinent for psychologist as well as for physicians. In both videos psychological as well as medical perspectives were explicitly presented (if only by physicians in the mono-professional condition). Thus, we hypothesized that the attitude of participants in both conditions would improve toward psychologists and toward physicians by watching the video (Hypothesis 3a). As the viewers in the inter-professional condition were more clearly and more obviously confronted with both perspectives by observing role-models from both professions, we also hypothesized that this improvement would be stronger in the inter-professional condition than in the mono-professional condition (Hypothesis 3b).
Moreover, we assumed that the presentation format would have an impact on the evaluation of the importance of IPC. Since the participants explicitly observed experts from different professions, we hypothesized that participants in the inter-professional condition would assess IPC’s importance to be greater than participants in the mono-professional condition (Hypothesis 4).
Finally, we hypothesized that the presentation format would have an impact on the evaluation of psychological support during treatment. According to Xiao and Bavel,37 even implicit devaluation of a social outgroup disappeared when 2 groups were presented as being cooperative (instead of competitive). The inter-professional video format made the relevance of cooperation more evident than the mono-professional video. We hypothesized that participants in the inter-professional condition would evaluate psychological support during treatment more positively than participants in the mono-professional condition (Hypothesis 5) after watching the video.
The perception of a video as entertaining might foster knowledge acquisition.38 A positive affective state helps encoding and storing information39,40 and thus may in turn facilitate knowledge acquisition. Based on these assumptions, we posed an open research question to examine whether there is an impact of presentation format on knowledge acquisition.
Methods
Study design
The study had a mixed design with presentation format (mono- vs inter-professional) as between-group factor and pre/post-comparison as within-group factor. Attitude toward interprofessional interaction and learning, evaluation of the entertaining and illustrative character of the video, attitude toward physicians and psychologists, importance of IPC, evaluation of psychological treatment support, and knowledge acquisition served as dependent variables.
Participants
A total of 288 participants were recruited from the mailing list of the online video platform Sectio chirurgica (www.sectio-chirurgica.de).41 They followed a link that was addressed specifically to medical students, pointing out that participation was voluntary and anonymous. About 202 participants completed the questionnaire, but 60 failed the manipulation check that asked which professions were represented in the video that the participants had seen. This relatively high number of people who failed the manipulation check is quite typical for online studies that use videos as stimulus material42 as some participants lack the necessary motivation to concentrate sufficiently on the contents. Two participants were excluded from the analysis as they were not medical students. Data of 140 participants thus remained for analysis (see Figure 1): 74 participants were in the mono-professional condition (40 females, 34 males) and 66 (41 females, 25 males) in the inter-professional condition. The participants’ medical training ranged between the first and the tenth semesters, with most of the participants in earlier semesters (M = 4.15; SD = 2.64). Their mean age was 23.13 years old (SD = 3.53). Participants could win vouchers for an online shop.
Figure 1.
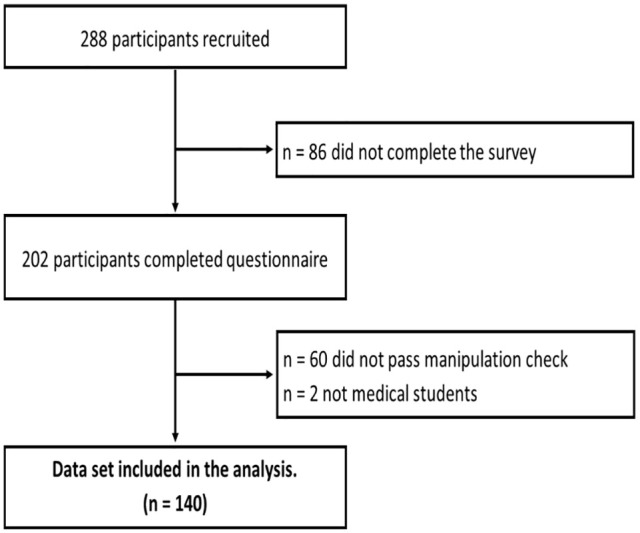
Flow diagram.
Procedure
The study was conducted online in January 2020. Prior to the video presentation participants completed a demographic questionnaire that asked for their education history, age, and gender. Participants’ professional identification, attitude toward psychological and medical treatment, and rating of interprofessional learning and interaction36-38 were also measured. Participants then watched a shortened episode from the medical online video platform Sectio chirurgica about a DBS surgical procedure, but the video differed in the 2 conditions. In the mono-professional condition the video showed the essential elements of the procedure and 2 physicians talking about DBS for PD. The inter-professional condition was identical to the mono-professional condition, but with additional comments by a psychologist. All of the professionals shown in the videos were male professors from the local university. They were all well known for their scientific reputation so that both professions were presented with the same level of status, power, and expertise.
After watching the video, participants again filled in questionnaires on their attitude toward psychological and medical treatment and their rating of inter-professional learning and interaction. They were also asked to evaluate the video’s entertainment value and its illustration of IPC. Then participants took a knowledge test. Finally, participants were informed about the aim of the study and the manipulation that was applied.
Material and measurements
The videos were shortened versions of a full episode, edited to 8:22 min videos. The inter-professional condition additionally presented an interview with a psychologist conducted by a medical doctor, which provided a psychological position to DBS treatment. The interview video had been cut in between at various to the topic relevant points in the other film (4:44 min in total).
Attitude toward IPC
Attitudes toward IPC interaction and learning were measured by the IP-interaction and IP-learning subscales43-45 from the University of the West of England Interprofessional Questionnaire (UWE-IP). Both subscales comprised 9 items each that were measured on 5-point Likert scales. Reliability of these scales were Cronbach’s alpha = 0.712 (IP-interaction) and Cronbach’s alpha = 0.823 (IP-learning), respectively.
Evaluation of the video
The participants’ evaluation of the video was measured by 2 scales. The first scale rated the entertainment value of the video with 6 items. Reliability of this scale was Cronbach’s alpha = 0.824. The second scale rated how well the video illustrated IPC with 3 items with a reliability of Cronbach’s alpha = 0.889. All items were measured on 5-point Likert scales (Table 1).
Table 1.
Video evaluation scale.
| Entertainment | 1 (I don’t agree at all) | 2 | 3 | 4 | 5 (I fully agree) |
|---|---|---|---|---|---|
| I thought the video was entertaining. | ○ | ○ | ○ | ○ | ○ |
| I found the video exciting. | ○ | ○ | ○ | ○ | ○ |
| The video was thrilling. | ○ | ○ | ○ | ○ | ○ |
| I found the video diverting. | ○ | ○ | ○ | ○ | ○ |
| I had fun watching this video. | ○ | ○ | ○ | ○ | ○ |
| I was fascinated by this video. | ○ | ○ | ○ | ○ | ○ |
| Illustrative character. | |||||
| The video provided good insight into the cooperation of different professions. | ○ | ○ | ○ | ○ | ○ |
| Watching the video prepared me for an interprofessional cooperation with psychologists. | ○ | ○ | ○ | ○ | ○ |
| I think the video gave me a better understanding of the actions and thinking of other professionals. | ○ | ○ | ○ | ○ | ○ |
Attitude toward the professions
Participants’ attitudes toward the medical and psychological professions was measured with an adapted version of Marteau et al scale46 with 4 items on 7-point Likert scales, with a separate assessment of the medical and the psychological professions (see Table 2). Reliability of this scale was Cronbach’s alpha = 0.948.
Table 2.
Attitude toward the professions.
| I think that in the in the
context of DBS, the support of the patient by a doctor/a
psychologist is. . .. | ||||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| Useless | ○ | ○ | ○ | ○ | ○ | ○ | ○ | Useful |
| Harmful | ○ | ○ | ○ | ○ | ○ | ○ | ○ | Beneficial |
| Unimportant | ○ | ○ | ○ | ○ | ○ | ○ | ○ | Important |
| A bad thing | ○ | ○ | ○ | ○ | ○ | ○ | ○ | A good thing |
Evaluation of the importance of IPC
A scale was created to evaluate the importance of IPC for DBS. This scale contained 6 items on a 5-point Likert scale (see Table 3). Reliability of this scale was Cronbach’s alpha = 0.815.
Table 3.
Evaluation of the importance of IPC.
| (I don’t agree at all) | 1 | 2 | 3 | 4 | 5 (I fully agree) |
|---|---|---|---|---|---|
| The patient’s preparation for a neurosurgical intervention should be carried out both by physicians and psychologists. | ○ | ○ | ○ | ○ | ○ |
| A close cooperation between psychologists and doctors is important for patient’s complete information. | ○ | ○ | ○ | ○ | ○ |
| Inter-professional cooperation between psychologists and doctors is beneficial for an ideal therapeutic outcome. | ○ | ○ | ○ | ○ | ○ |
| The involvement of psychological specialists to care for patients during treatment makes sense for patients. | ○ | ○ | ○ | ○ | ○ |
| The involvement of psychological specialists to care for patients during treatment is helpful for patients. | ○ | ○ | ○ | ○ | ○ |
| Patients who have received DBS should be monitored afterwards by psychologists. | ○ | ○ | ○ | ○ | ○ |
Evaluation of psychological support during treatment
A scale with 4 items was created to evaluate the psychological support during treatment. Reliability of these scales were Cronbach’s alpha = 0.675. Due to this low level of reliability,47,48 we did not include this scale in the analysis. Hypothesis 5 could therefore not be tested.
Knowledge acquisition
In the knowledge test the participants had to judge 7 statements as correct or incorrect. In addition, they were asked 2 multiple choice questions (see Table 4). For each question the level of confidence for each answer was also rated on a scale ranging from 1 (very unconfident) to 6 (very confident). To reduce the probability of guessing, a balanced negative marking method was used49 where each answer was analyzed for correctness (+1 = correct answer; −1 = wrong answer) and multiplied with the confidence score. The questions of the knowledge test included only content that was shown in identical form in both videos.
Table 4.
Knowledge test.
| Multiple choice | Multiple answers can be correct | Confidence rating |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Very unconfident ——- very
confident | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | ||||
| As imaging techniques are not sufficient for optimal trajectories planning, additional methods need to be applied. Which ones? | Electrophysiological methods | ▯ | |||||||
| Audiometric methods | ▯ | ||||||||
| Electroneurographic methods | ▯ | ||||||||
| Transcranial Doppler methods | ▯ | ||||||||
| The cardinal symptoms of Parkinson’s disease are called the triad. These include: | Amnesia | ▯ | |||||||
| Akinesia | ▯ | ||||||||
| Aphasia | ▯ | ||||||||
| Mutism | ▯ | ||||||||
| Rigor | ▯ | ||||||||
| Tremor | ▯ | ||||||||
| Forced choice | Please choose |
Confidence rating |
|||||||
| Correct | Wrong | Not at all ————– absolutely | |||||||
| About 80% of patients suffering from Parkinson’s disease are treated with DBS. | ▯ | ▯ | ○ | ○ | ○ | ○ | ○ | ○ | |
| About 80% of deep brain stimulation surgeries are performed on patients with Parkinson’s disease. | ▯ | ▯ | ○ | ○ | ○ | ○ | ○ | ○ | |
| To avoid cerebral damage, gyri should be avoided in trajectory planning. | ▯ | ▯ | ○ | ○ | ○ | ○ | ○ | ○ | |
| The symptoms of akinesia and rigor can easily be reduced by stimulating fibrous tracts in the zona incerta. | ▯ | ▯ | ○ | ○ | ○ | ○ | ○ | ○ | |
| Depression in Parkinson’s disease is caused by cerebral cell death. | ▯ | ▯ | ○ | ○ | ○ | ○ | ○ | ○ | |
| Tremor can be reduced by stimulating the anterior subthalamic nucleus. | ▯ | ▯ | ○ | ○ | ○ | ○ | ○ | ○ | |
Statistical analysis
We performed data analysis using IBM SPSS 22 for Windows (IBM Corp., Armonk, NY). Internal consistency of all scales was determined by calculating Cronbach’s alpha (α). We tested age distribution with a t-test and gender distribution with a chi-squared test. To test the assumptions of Hypotheses 1 and 3, mixed-design ANOVAs with condition as between-group factor and the pre/post-comparison as within-group factor were calculated. To test Hypotheses 2 and 4, as well as for the open research question, independent samples t-tests were used.
All data are reported as means (M) ± standard deviations (SD), unless otherwise noted. The level of significance was set at P < .050. Cohen’s d and partial eta squared (η2p) are reported as indicators of effect size.
Results
Equivalence of student groups
We controlled the age and gender distributions of the 2 conditions. They did not differ from each other in age (t(138) = 0.406; P = .686) or gender (χ2 = 3.457; P = .063).
Attitude toward IPC
Hypothesis 1a stated that the attitude of participants in the inter-professional condition toward inter-professional interaction would improve more than that of participants in the mono-professional condition. The data did not support this hypothesis. We found only a significant main effect for time (Pre: M = 3.48, SD = 0.56; Post: M = 3.59, SD = 0.51; F(1,137) = 5.176, P < .024; η2p = 0.036), but no significant interaction effect between time and condition (P = .223).
Hypothesis 1b assumed that the students’ attitudes toward IPC learning would improve by observing the inter-professional video. Again, there was a significant effect for time (Pre: M = 3.79, SD = 0.87; Post: M = 3.91, SD = 0.80; F(1,137) = 6.482, P = .012, η2p = 0.045), but no significant interaction effect for time x condition (F(1,137) = 0.364, P = .547).
Evaluation of the video
We hypothesized that the video in the inter-professional condition would be evaluated as more entertaining (Hypothesis 2a) and more illustrative of IPC (Hypothesis 2b) than in the mono-professional condition. Hypothesis 2a was supported by the data; participants of the inter-professional condition evaluated the video as more entertaining (M = 2.65; SD = 0.45) than participants of the mono-professional condition (M = 2.47; SD = 0.49; t(138) = −2.227; P = .028; d = 0.38).
Hypothesis 2b was supported by the data as well. The inter-professional video was reported to be more illustrative of IPC (M = 3.20; SD = 1.03) than the mono-professional video (M = 2.17; SD = 0.92; t(138) = −6.269; P < .001; d = 1.06).
Attitude toward the professions
We hypothesized that the attitudes of participants in both conditions would improve toward psychologists and toward physicians by watching the video (Hypothesis 3a). We also assumed that this improvement would be stronger in the inter-professional condition than in the mono-professional condition (Hypothesis 3b).
The data partly supported Hypothesis 3a. The attitudes of participants did improve toward physicians by watching the video (Pre: M = 6.48, SD = 0.75; Post: M = 6.75, SD = 0.55; F(1,138) = 4.860, P < .001, η2p = 0.11), but their attitudes toward psychologists did not change significantly (Pre: M = 2.22, SD = 0.55; Post: M = 2.41, SD = 1.66; F(1,138) = 2.135, P = .146). The assumptions of Hypothesis 3b were not supported by the data: Participants’ positive attitudes toward physicians increased more strongly in the mono-professional condition (F(1,138) = 4.151, P = .044, η2p = 0.03) than in the inter-professional condition (see Figure 2). No interaction-effect was found for attitude toward psychologists (F(1,138) = 0.392, P = .532).
Figure 2.
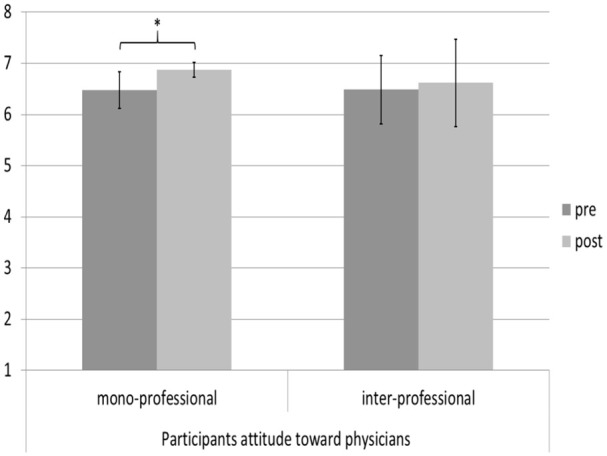
Participants’ attitudes toward physicians before and after watching the video.
Evaluation of the importance of IPC
We hypothesized that participants in the inter-professional condition would assess the importance of IPC for DBS to be greater than participants in the mono-professional condition (Hypothesis 4). The data supported this hypothesis. Participants who watched the inter-professional video considered IPC to be more important (M = 4.18; SD = 0.48) than participants who watched the mono-professional video (M = 3.53; SD = 0.48; t(138) = −7.954; P < .001; d = 1.35).
Knowledge acquisition
After watching the video, participants in the inter-professional condition performed better in the knowledge test (M = 8.32; SD = 10.45) than those in the mono-professional condition (M = 4.25; SD = 10.54; t(138) = −2.285; P = .024; d = 0.04).
Discussion
Medical IPE videos can be used independently of time and location to give learners the opportunity to gather relevant knowledge from different professional perspectives.50 We investigated whether it is sufficient if the topic of the video itself is inter-professional (though being presented by representatives of only 1 profession), or if it is necessary for experts from different professions explicitly to appear in the video. The data collected in this study supported some but not all of our hypotheses. We therefore cannot provide final answers to the research questions, though some of our findings are valuable. On the one hand, our findings support the idea that the explicit appearance of experts from different professions is superior to a mono-professional presentation. We found that the inter-professional video was perceived to be more entertaining and more illustrative. This finding is in line with other studies that found that students perceived learning under the supervision of experts from professions other than their own to be rewarding and beneficial.51 Such experiences also open new perspectives for learners at all levels.52 A previous study38 found that the acquisition of clinical knowledge was mediated by the entertainment aspect of a video. In the study presented here we also found that participants in the inter-professional condition learned more than the participants in the mono-professional condition. In addition, we found that participants in the inter-professional condition perceived IPC in the clinical context of DBS to be more important than participants in the mono-professional condition. This is an encouraging finding, as the main aim of IPE interventions is to foster IPC in clinical practice. However, based on this result, we cannot go so far as to say that the students’ attitudes would actually result in more inter-professional behavior in clinical practice.
On the other hand, we have findings that did not support the idea that inter-professional videos are better for teaching inter-professional perspectives. Regarding the participants’ attitudes toward IPC learning and IPC interaction, we found no superiority of the inter-professional video compared to the mono-professional video. Both videos were equally effective in fostering positive attitudes toward IPC learning and IPC interaction. Based on this finding, it seems that for fostering positive attitudes toward IPE, the most important aspect is that the topic of the video itself is inter-professional. This was the case in the present investigation using the topic DBS for patients with PD. However, according to our results, the additional explicit appearance of a representative of a second profession does not seem to be necessary to improve the attitude.
In the inter-professional condition, participants’ attitudes toward physicians improved less than in the mono-professional condition. In addition, we found that the video presentation only affected participants’ attitude toward physicians, but not toward psychologists. One reason for this could be that, due to the fact that in the mono-professional condition, the physicians appeared as the only responsible actors, the impression was created that they, and only they, perform particularly great medical services. Especially medical students as prospective doctors could be susceptible to this perception. In the inter-professional condition, however, the physicians had to share part of their fame with the psychologists. Since all the participants were medical students, these findings must be interpreted with caution. We do not know to what extent their own professional identity had an impact on the findings. Research has shown that members of one’s own social group are often rated more favorably than members of other groups.53 In future studies, medical as well as psychological students should participate to control for the influence of participants’ own professional identity.
Limitations
Although we consider our study to be a contribution to the development and use of IPE videos in medical education, we need to discuss some limitations. First, all of the participants were medical students, and most of them were at an early stage of their training. Thus, we cannot generalize these results to other healthcare-education populations. Moreover, although the videos showed experts from different professions contributing their profession-specific knowledge and perspectives, they did not really interact with each other. Future studies should make use of other topics that display a more obvious interaction among different healthcare professions.
Also, the protagonists in our videos were exclusively men. Further studies could investigate the extent to which the gender of the health professionals involved has an impact on the perceptions of the viewers. In addition, the videos in both conditions differed regarding their length. Even though the knowledge test only asked for content that was identical in both videos, participants in the inter-professional condition had more time to deal with the topic in general.
Finally, it is still unclear how well these effects on inter-professional learning would transfer to inter-professional everyday practice. Findings which are reported about this question are based on active IPE programs and show rather low or inconsistent results.2,3,54-56 For future research, long-term studies are required to investigate to what extent IPE videos can affect real clinical outcomes.
Conclusion
This experimental study compared 2 possible IPE video formats to foster inter-professional learning in healthcare education. To represent IPC, we used the example of collaboration among physicians and psychologists. An advantage of IPE videos is that they are easy to implement in existing curricula, or they can be used as add-ons to curricular training, to illustrate and foster IPC. Although the data did not support all of the hypotheses, we may conclude that the explicit appearance of experts from different professions in an educational video had a positive influence on how medical students perceived the video and how they evaluated IPC. The inter-professional video also led to better performance on a knowledge test of the medical students in this study.
Acknowledgments
We would like to thank all participants who gave up their time to participate. We also would like to thank the Department of General Practice and Health Services Research (University Hospital Heidelberg, Heidelberg, Germany) for the permission for the use of the translated version of the UWE-IP questionnaire and Simone Korger for her assistance in data collection.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research reported here was supported by a grant from the German Bundesministerium für Bildung und Forschung (BMBF); Grant number: 16DHL1030.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ Contributions: JG: Conceptualization (equal), Data curation (lead), Formal analysis (lead), Investigation (lead), Methodology (equal), Resources (equal), Software (equal), Validation (equal), Visualization (lead), Writing-original draft (equal), Writing review & editing (equal).
JK: Conceptualization (equal), Formal analysis (supporting), Funding acquisition (lead), Investigation (supporting), Methodology (supporting), Project administration (lead), Supervision (lead), Validation (lead), Writing-original draft (supporting), Writing-review & editing (supporting).
TS: Conceptualization (supporting), Data curation (supporting), Funding acquisition (supporting), Methodology (supporting), Project administration (supporting), Resources (equal), Writing-original draft (supporting), Writing-review & editing (supporting).
BH: Funding acquisition (lead), Project administration (supporting), Supervision (equal).
MB: Conceptualization (equal), Data curation (supporting), Formal analysis (supporting), Funding acquisition (supporting), Investigation (supporting), Methodology (equal), Project administration (lead), Resources (equal), Software (equal), Supervision (lead), Validation (lead), Writing-original draft (equal), Writing-review & editing (supporting).
Ethics Approval and Consent to Participate: This research was performed in accordance with the Declaration of Helsinki. This study had full approval by the ethics committee of Leibniz-Institut für Wissenmedien (approval number: 16DHL1030). All participants took part voluntarily and anonymously. They gave written informed consent and were informed about privacy protection, their right to terminate participation at any time without disadvantages, and about the general purpose of the study.
ORCID iD: Johannes Großer  https://orcid.org/0000-0002-0015-2966
https://orcid.org/0000-0002-0015-2966
References
- 1. Gill A, Cowart J, Hatfield C, et al. Patient safety interprofessional training for medical, nursing, and pharmacy students [published online ahead of print June 15, 2017]. MedEdPORTAL Publ. doi: 10.15766/mep_2374-8265.10595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guraya SY, Barr H. The effectiveness of interprofessional education in healthcare: a systematic review and meta-analysis. Kaohsiung J Med Sci. 2018;34:160-165. [DOI] [PubMed] [Google Scholar]
- 3. Solomon P, Baptiste S, Hall P, et al. Students’ perceptions of interprofessional learning through facilitated online learning modules [published online ahead of print August 26, 2010]. Med Teach. doi: 10.3109/0142159X.2010.495760. [DOI] [PubMed] [Google Scholar]
- 4. Barr H, Freeth D, Hammick M, Koppel I, Reeves S. The evidence base and recommendations for interprofessional education in health and social care [published online ahead of print January 01, 2006]. J Interprof Care. doi: 10.1080/13561820600556182. [DOI] [PubMed] [Google Scholar]
- 5. Walkenhorst U, Mahler C, Aistleithner R, et al. Positionspapier GMA-ausschuss–interprofessionelle ausbildung in den gesundheitsberufen. Gms Z Med Ausbild. 2015;32:95424-95442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wilhelmsson M, Pelling S, Ludvigsson J, Hammar M, Dahlgren LO, Faresjö T. Twenty years experiences of interprofessional education in Linköping - Ground-breaking and sustainable [published online ahead of print July 06, 2009]. J Interprof Care. doi: 10.1080/13561820902728984. [DOI] [PubMed] [Google Scholar]
- 7. McLean G, Hindle JV., Guthrie B, Mercer SW. Co-morbidity and polypharmacy in Parkinson’s disease: insights from a large Scottish primary care database [published online ahead of print July 01, 2017]. BMC Neurol. doi: 10.1186/s12883-017-0904-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jankovic J. Parkinson’s disease: clinical features and diagnosis [published online ahead of print April 01, 2008]. J Neurol Neurosurg Psychiatry. doi: 10.1136/jnnp.2007.131045. [DOI] [PubMed] [Google Scholar]
- 9. Micieli G, Tosi P, Marcheselli S, Cavallini A. Autonomic dysfunction in Parkinson’s disease. Neurol Sci. 2003;24:S32-S34. [DOI] [PubMed] [Google Scholar]
- 10. Landau S, Harris V, Burn DJ, et al. Anxiety and anxious-depression in Parkinson’s disease over a 4-year period: a latent transition analysis. Psychol Med. 2016;46:657-667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bronstein JM, Tagliati M, Alterman RL, et al. Deep brain stimulation for Parkinson disease an expert consensus and review of key issues. Arch Neurol. 2011;68:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Perozzo P, Rizzone M, Bergamasco B, et al. Deep brain stimulation of subthalamic nucleus: behavioural modifications and familiar relations. Neurol Sci. 2001;22:81-82. [DOI] [PubMed] [Google Scholar]
- 13. Synofzik M, Schlaepfer TE. Stimulating personality: ethical criteria for deep brain stimulation in psychiatric patients and for enhancement purposes. Biotechnol J. 2008;31511-31520. [DOI] [PubMed] [Google Scholar]
- 14. Morishita T, Fayad SM, Higuchi MA, Nestor KA, Foote KD. Deep brain stimulation for treatment-resistant depression: systematic review of clinical outcomes. Neurotherapeutics. 2014;11:475-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ward W, Zagoloff A, Rieck C, Robiner W. Interprofessional education: opportunities and challenges for psychology [published online ahead of print February 16, 2018]. J Clin Psychol Med Settings. doi: 10.1007/s10880-017-9538-3. [DOI] [PubMed] [Google Scholar]
- 16. Robiner WN, Dixon KE, Miner JL, Hong BA. Psychologists in medical schools and academic medical centers: over 100 years of growth, influence, and partnership [published online ahead of print March 03, 2014]. Am Psychol. doi: 10.1037/a0035472. [DOI] [PubMed] [Google Scholar]
- 17. Interprofessional Educational Collaborative, Practice IC, Values U. Core Competencies for Interprofessional Collaborative Practice : 2016 Update. Washington, DC: Interprofessional Education Collaborative; 2016. [Google Scholar]
- 18. Anderson GL, Lovejoy DW. Predoctoral training in collaborative primary care: an exam room built for two. Prof Psychol Res Pract. 2000;31:692-697. [Google Scholar]
- 19. Bridges DR, Davidson RA, Odegard PS, Maki I V, Tomkowiak J. Interprofessional collaboration: three best practice models of interprofessional education [published online ahead of print April 08, 2011]. Med Educ Online. doi: 10.3402/meo.v16i0.6035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Köllner V, Foltin Y, Speidel V, Müller AK, Jäger J. Anamnesegruppen als Einstieg in die Gesprächsführung und Arzt - Patient-Beziehung. Med Welt. 2016;67:9-13. [Google Scholar]
- 21. Cubic B, Mance J, Turgesen JN, Lamanna J. Interprofessional education: preparing psychologists for success in integrated primary care. J Clin Psychol Med Settings. 2012;19:84-92. [DOI] [PubMed] [Google Scholar]
- 22. Eggeling M, Bientzle M, Shiozawa T, Cress U, Kimmerle J. The impact of visualization format and navigational options on laypeople’s perception and preference of surgery information videos: randomized controlled trial and online survey. J Particip Med. 2018;10:e12338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Eggeling M, Bientzle M, Cress U, Shiozawa T, Kimmerle J. The impact of physicians’ recommendations on treatment preference and attitudes: a randomized controlled experiment on shared decision-making [published online ahead of print November 11, 2020]. Psychol Heal Med. doi: 10.1080/13548506.2019.1687917. [DOI] [PubMed] [Google Scholar]
- 24. Welsher A, Grierson LEM. Enhancing technical skill learning through interleaved mixed-model observational practice [published online ahead of print February 03, 2017]. Adv Heal Sci Educ. doi: 10.1007/s10459-017-9759-0. [DOI] [PubMed] [Google Scholar]
- 25. Grosser J, Bientzle M, Kimmerle J. A literature review on the foundations and potentials of digital teaching scenarios for interprofessional health care education [published online ahead of print May 14, 2020]. Int J Environ Res Public Health. doi: 10.3390/ijerph17103410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Domuracki K, Wong A, Olivieri L, Grierson LEM. The impacts of observing flawed and flawless demonstrations on clinical skill learning. Med Educ. 2015;49: 186-192. [DOI] [PubMed] [Google Scholar]
- 27. Bientzle M, Minje J, Cress U, Kimmerle J. Therapeutic touch in exercise videos: a randomized experiment of the impact on the evaluation of therapists’ competence and viewers’ self-reliance. Front Sport Act Living. 2019;1:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Grosser J, Bientzle M, Shiozawa T, Hirt B, Kimmerle J. Observing interprofessional collaboration: Impact on attitude and knowledge acquisition [published online ahead of print July 31, 2020]. Anat Sci Educ. doi: 10.1002/ase.2007. [DOI] [PubMed] [Google Scholar]
- 29. Bandura A. Social cognitive theory of mass communication. Media Psychol. 2001;3:265-299. [Google Scholar]
- 30. Bandura A. Social Foundations of Thought and Action : A Social Cognitive Theory/Albert Bandura. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 31. Hober C, Bonnel W. Student Perceptions of the Observer Role in High-Fidelity Simulation. Clin Simul Nurs. 2014;10:507-514. doi: 10.1016/j.ecns.2014.07.008. [DOI] [Google Scholar]
- 32. Clark PG. What would a theory of interprofessional education look like? Some suggestions for developing a theoretical framework for teamwork training. J Interprof Care. 2006;20:577-589. [DOI] [PubMed] [Google Scholar]
- 33. König L, Jucks R. Hot topics in science communication: aggressive language decreases trustworthiness and credibility in scientific debates. Public Underst Sci. 2019;28:401-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Machado A, Rezai AR, Kopell BH, Gross RE, Sharan AD, Benabid AL. Deep brain stimulation for Parkinson’s disease: surgical technique and perioperative management. Mov Disord. 2006;21:S247-S258. [DOI] [PubMed] [Google Scholar]
- 35. Bientzle M, Kimmerle J, Eggeling M, Cebi I, Weiss D, Gharabaghi A. Evidence-based decision aid for patients with parkinson disease: protocol for interview study, online survey, and two randomized controlled trials. JMIR Res Protoc. 2020;9:e17482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Van Gog T, Rummel N. Example-based learning: integrating cognitive and social-cognitive research perspectives. Educ Psychol Rev. 2010;22:155-174. [Google Scholar]
- 37. Xiao YJ, Van Bavel JJ. Sudden shifts in social identity swiftly shape implicit evaluation. J Exp Soc Psychol. 2019;83:55-69. [Google Scholar]
- 38. Grosser J, Bientzle M, Shiozawa T, Hirt B, Kimmerle J. Acquiring clinical knowledge from an online video platform: a randomized controlled experiment on the relevance of integrating anatomical information and clinical practice. Anat Sci Educ. 2018;12:478-484. [DOI] [PubMed] [Google Scholar]
- 39. Fredrickson BL. What good are positive emotions? Rev Gen Psychol. 1998;2:300-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Isen AM. A role for neuropsychology in understanding the facilitating influence of positive affect on social behavior and cognitive processes. In: Lopez SJ, Snyder CR, eds. Oxford Handbook of Positive Psychology. New York: Oxford University Press; 2009:503-518. [Google Scholar]
- 41. Hirt B, Shiozawa T, Herlan S, Wagner H-J, Küppers E. Surgical prosection in a traditional anatomical curriculum—Tübingens’ Sectio chirurgica. Ann Anat. 2010;192:349-354. [DOI] [PubMed] [Google Scholar]
- 42. Jun E, Hsieh G, Reinecke K. Types of motivation affect study selection, attention, and dropouts in online experiments. Proc ACM Human Comput Interact. 2017;1:1-5. [Google Scholar]
- 43. Mahler C, Berger S, Pollard K, et al. Translation and psychometric properties of the German version of the University of the West of England Interprofessional Questionnaire (UWE-IP). J Interprof Care. 2017;31:105-109. [DOI] [PubMed] [Google Scholar]
- 44. Pollard KC, Miers ME, Gilchrist M. Collaborative learning for collaborative working? Initial findings from a longitudinal study of health and social care students. Health Soc Care Community. 2004;12:346-358. [DOI] [PubMed] [Google Scholar]
- 45. Pollard K, Miers ME, Gilchrist M. Second year scepticism: pre-qualifying health and social care students’ midpoint self-assessment, attitudes and perceptions concerning interprofessional learning and working. J Interprof Care. 2005;19:251-268. [DOI] [PubMed] [Google Scholar]
- 46. Marteau TM, Dormandy E, Michie S. A measure of informed choice. Heal Expect. 2001;4:99-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rasch B, Hofmann W, Friese M, Naumann E. Quantitative Methoden 2: Einführung in die Statistik für Psychologen und Sozialwissenschaftler. Berlin: Springer-Lehrbuch; 2010. [Google Scholar]
- 48. Janczyk M, Pfister R. Inferenzstatistik Verstehen. Berlin, Heidelberg: Springer; 2013. [Google Scholar]
- 49. Gardner-Medwin AR, Gahan M. Formative and summative confidence-based assessment. Proceedings of the 7th International Computer-Aided Assessment Conference; July 2003:147-155; Loughborough, UK. [Google Scholar]
- 50. van Es EA, Tunney J, Goldsmith LT, Seago N. A framework for the facilitation of teachers’ analysis of video. J Teach Educ. 2014;65:340-356. [Google Scholar]
- 51. Chipchase L, Allen S, Eley D, McAllister L, Strong J. Interprofessional supervision in an intercultural context: a qualitative study. J Interprof Care. 2012;26:465-471. [DOI] [PubMed] [Google Scholar]
- 52. Ruiz MG, Ezer H, Purden M. Exploring the nature of facilitating interprofessional learning: findings from an exploratory study. J Interprof Care. 2013;27:489-495. [DOI] [PubMed] [Google Scholar]
- 53. Sollami A, Caricati L, Mancini T. Attitudes towards interprofessional education among medical and nursing students: the role of professional identification and intergroup contact. Curr Psychol. 2018;37905-37912. [Google Scholar]
- 54. McCutcheon LRM, Alzghari SK, Lee YR, Long WG, Marquez R. Interprofessional education and distance education: A review and appraisal of the current literature [published online ahead of print June 02, 2017]. Curr Pharm Teach Learn. doi: 10.1016/j.cptl.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 55. Karim R, Ross C. Interprofessional education (IPE) and chiropractic. J Can Chiropr Assoc. 2008;52:76-78. [PMC free article] [PubMed] [Google Scholar]
- 56. Reeves S, Pelone F, Harrison R, Goldman J, Zwarenstein M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2017;6:CD000072. [DOI] [PMC free article] [PubMed] [Google Scholar]


