Abstract
Patients with lower limb edema are frequently referred to vascular specialists for evaluation. Multiple etiologies must be considered and often more than one cause may be present. Notably, the role of lymphatic system regardless of the underlying pathology has been underestimated. A thorough history and physical examination and a carefully considered laboratory and imaging evaluation are critical in differentiating causes. In this opinion article, we propose a diagnostic algorithm that incorporates a systematic approach to the patient with leg swelling and provides an efficient pathway for the differential diagnosis for this problem.
Keywords: Chronic venous disease, lymphedema, vascular medicine
Introduction
Lower limb edema is a common and challenging diagnostic problem often with a significant impact. It is defined as swelling caused by an increase in interstitial fluid that exceeds the capacity of physiologic lymphatic drainage. In most cases it occurs when fluid accumulates in subcutaneous tissues leading to volume expansion, although congenital etiologies and lipedema may result in excessive soft tissue in the lower extremities. Fluid collection can be a result of many etiologies including a range of local or systemic disorders, including infra-inguinal superficial and deep venous reflux, supra and infra inguinal deep vein obstruction, and primary and secondary lymphatic diseases. Although the most likely singular cause of unilateral lower limb edema in individuals over 50 years old is venous disease, the etiology is often multifactorial.1 Symptoms can be debilitating and subsequently impact quality of life with significant costs to society.2–5 Recent work has demonstrated that chronic edema negatively impacts physical and psychological health and reduces quality of life.6 As such, in this opinion article, we propose a practical diagnostic approach to accurately and efficiently identify the causes of chronic edema in affected patients and to institute appropriate therapy.
History
Lower limb swelling may present to the clinician in several ways. It is essential to take a complete patient history to facilitate accurate, efficient, and cost-effective diagnostic testing and management. The site of swelling and any associated manifestations should be assessed, including whether it is unilateral, bilateral equal or bilateral but asymmetric, along with any changes that occur with its severity with position and time of day. Swelling may be asymptomatic, although it can be associated with symptoms such as aching, pain, heaviness, characteristic venous or lymphatic skin changes or prior or active ulcerations of the lower limb. Patients may describe a sudden onset of limb swelling, a gradual onset or a more long-standing condition. Common causes of leg swelling based on acuity and unilateral or bilateral symptoms are shown in Table 1.
Table 1.
Common causes of leg edema in the western world.
| Unilateral |
Bilateral |
||
|---|---|---|---|
| Recenta | Chronicb | Recenta | Chronicb |
| Unilateral DVT | Primary venous disease | Bilateral DVT | Chronic venous disease/post-thrombotic syndrome |
| Ruptured Baker's cyst | Post-thrombotic syndrome | Acute heart failure | Pulmonary hypertension |
| Ruptured leg muscle | Iliac vein compression | Acute renal/liver failure | Heart/renal/liver failure |
| Compartment syndrome | Lymphedema | IVC thrombosis | Idiopathic edema |
| Intramuscular hematoma | Vascular malformation | IVC tumors | Chronic IVC occlusion, IVC aplasia/hypoplasia |
| Infection | Reflux sympathetic dystrophy | Drugs | Drugs (see Table 2) |
| Superficial vein thrombosis | Mass/tumorc | Bilateral infections | Lymphedema |
| Mass/tumorc | Venous advential cystic disease | Lipedema | |
| Fracture | Infection | Pregnancy, premenstrual edema | |
| Sprain/strain | Static foot disorders | Obesity | |
| Insect/animal bites | Radiation | Malabsorption syndrome, hypoalbunemia | |
| Atrophy/hypertrophy | Spinal cord injury/immobility | ||
| Overgrowth syndromes | Static foot disorders | ||
| Thyroid disease | |||
| Obstructive sleep apnea |
Note: Arteriovenous fistulas involving large vessels can present with acute or chronic and unilateral or bilateral swelling. More commonly it presents as a chronic condition.
aRecent definition includes acute (<3 days) and sub-acute (3 days – 3 months).
bChronic definition >3 months.
cCan occur in the pelvis or extremity. If chronic, more likely to be benign.
Unilateral swelling favors primary and secondary causes of venous or lymphatic compromise and bilateral or generalized swelling suggests systemic etiologies as noted in Table 1. Bilateral but asymmetric cases can have unilateral causes on each leg of different etiologies or varying degrees, or a unilateral cause superimposed on a background of systemic disease. Lymphedema and venous edema can also be bilateral unequal and bilateral equal, although bilateral equal is less common with venous etiologies below the IVC since the disease is often asymmetric at any one point in time.
Assessing the duration of symptoms is important, with acute swelling (<72 h) more characteristic of etiologies such as DVT, infection, trauma, exacerbation of a medical condition such as congestive heart failure, or recent medication changes. Chronic swelling may be due to venous insufficiency, lymphatic dysfunction, static foot disorders, or more longstanding medical etiologies. Additionally, swelling due to venous disease typically worsens with dependency during the day and improves with elevation. Venous edema is also commonly associated with complaints of aching, heaviness, or fatigue of the limbs. Focal pain may suggest a musculoskeletal or joint issue. Reflex sympathetic dystrophy (complex regional pain syndrome) must also be considered with a significantly painful chronically swollen limb. Lymphedema is usually painless and may present with classic signs of foot involvement and skin changes or with just mild swelling that is pitting.2–4 Lipedema almost always is bilateral, spares the feet, and presents with disproportionate pain, tenderness, and an unusual tendency to bruise easily. It is important to recognize that the often-referenced clinical findings are not always the rule with these conditions.
A complete history of venous disorders including the presences of varicose veins, prior VTE, or prior events that could provoke VTE, and of personal or familial clotting issues and a history of prior superficial and deep venous interventions should be obtained. Provoking events could be trauma, prolonged bedrest, history of lower limb interventions including joint arthroplasty, arterial interventions, or vein harvesting for heart bypass. Previous abdominal or pelvic surgery, malignancy, or radiation history is also important as an antecedent to both venous and lymphatic etiologies of edema.2–5
Assessment for systemic diseases is necessary, particularly in older patients with multiple comorbid conditions that could be contributing to their primarily bilateral leg edema. New onset or exacerbations of cardiac, renal, hepatic, endocrine issues may be a cause. A history of unexplained weight loss or adenopathy might suggest malignant venous compression.
A detailed review of the patient’s medications must also be performed. Any changes in regimens should be considered in relation to swelling onset. Numerous medications (Table 2) can lead to lower limb edema. Calcium channel blockers, especially of the dihydropyridine class such as amlodipine, are common culprits, with lower limb edema found in nearly 50% of patients on this agent.2–4
Table 2.
Drugs that may cause leg swelling.
| Anti-hypertensive drugs |
| Calcium channel blockers |
| Beta blockers |
| Clonidine |
| Hydralazine |
| Minoxidil |
| Methyldopa |
| Hormones |
| Corticosteroids |
| Estrogen |
| Progesterone |
| Testosterone Gabapentinoids |
| Pregabalin |
| Gabapentin |
| Chemotherapy |
| Docetaxel |
| Gemcitabine |
| Pemetrexed |
| Lenolidamide/thalidomide |
| Targeted immunotherapy |
| Other |
| Non-steroidal anti-inflammatory drugs |
| Pioglitazone, rosiglitazone |
| Monoamine oxidase inhibitors |
| Pramipexole |
It is very important to note that there are often several factors responsible for swelling in any given patient and it is incumbent on the physician to determine the relative contribution of each. This will allow a more complete diagnosis and help the physicians to prioritize management to address the most important or impactful etiologies.
Physical examination
A complete physical examination is as essential to the clinical history in establishing the etiology of swelling. Although the main complaint is in the lower limbs, evaluation of the heart, lungs, and abdomen are important to assess for systemic etiologies or contributing factors. Increased jugular venous distension or crackles in the lungs may be due to heart failure, a distended abdomen with ascites or scleral icterus suggests hepatic disease, and abdominal incisions can reveal past surgeries. Extensive prominent veins in the lower abdomen may be a sign of inferior vena cava occlusion. Obesity with a large abdomen also may contribute to bilateral lower limb edema.2–4
It is important to assess both lower limbs, even if the complaint is unilateral. Often the other limb is also swollen and may provide clues as the causes of swelling in the more affected limb. The distribution of swelling should be noted. More focal swelling of a calf may be a DVT, SVT, infection, or secondary to injury, while swelling involving the entire limb or bilateral limbs is more likely due to a proximal pathophysiology or systemic process. Examination of the feet is also important. In lymphedema, swelling affects the dorsum of the foot in most cases and is associated with squaring of the toes and the foot, toe nail deformities (ski jump like), as well as skin thickening as characterized by inability to pinch a skin fold on the dorsum of the base of the second toe (a positive Kaposi-Stemmer sign). In advanced stages, the skin becomes hyperkeratotic with verrucous cobblestone-like papules, plaques, and nodules. In lipedema, the feet are generally spared, disproportionate swelling is noted from the ankles to the waist when compared with the torso above and a same distribution of swelling may also be seen in the upper limbs. The presence of pitting should also be noted, with a lack of pitting common in stages II and III lymphedema regardless of its cause as well as in lipedema. Pain, range of motion, and presence of neurologic abnormalities can help identify focal musculoskeletal, neurologic issues, and DVT.7,8
The skin of the lower extremities needs to be thoroughly examined. Infection and thrombophlebitis can be accompanied by erythema and increased warmth. The presence of varicose veins, especially with a gaiter distribution of hemosiderin staining, eczematous dermatitis, or atrophy blanche is indicative of venous insufficiency. Active or healed ulcerations, particularly in the region of the medial malleolus and lipodermatosclerotic skin changes suggest more advanced venous disease. An endocrine disorder can be accompanied by thin and shiny skin with bilateral swelling. Moreover, pretibial myxedema can present with a variety of cutaneous changes including hyperpigmentation, plaques, and/or nodules masquerading lymphedema. Additionally, although it is rare to have swelling with arterial insufficiency in the absence of critical limb ischemia, a thorough pulse exam should be performed on the bilateral lower limbs. This can assist identifying patients with mixed arterial and venous issues, patients with peripheral arterial disease with systemic etiologies of edema, and for appropriateness of compression therapy.2–4 Another condition that contributes alone or in combination with other pathologies in developing edema are foot disorders which impair the patient from adequate utilizing the calf muscle pump with ambulation.9 It is often observed in the clinical practice, but few specialists assess for this.
Diagnostic testing
If a systemic issue is suspected, appropriate laboratory tests should be performed. Complete blood count, a metabolic panel including evaluation of creatine, urinalysis, thyroid panel, atrial natriuretic peptide, hepatic enzymes, and albumin level may reveal abnormalities depending on the etiology. A D-dimer level may be helpful in evaluating for a possible acute DVT in the appropriate context.2,4 These tests can usually be performed by the primary care physician or cardiologist with concurrent imaging studies by the vascular specialist if needed.
Duplex ultrasound (DUS) is the initial and often the only imaging test in patients with swollen lower limbs without a clear cause based on history, physical and laboratory exam, or when further details are required to make therapeutic decisions. This non-invasive, low cost exam can survey the extremities for vascular and non-vascular causes of both acute and chronic swelling and offers a reproducible method of viewing venous anatomy, valve function, and patency. With sensitivity and specificity rate >90% for DVT, venous reflux, and non-vascular etiologies, swelling can be readily and robustly evaluated.10,11
DUS can also assess the venous anatomy in the abdomen and pelvis to look for thrombosis or compression by adjacent arteries or masses. Visualization of pelvic anatomy may be difficult for less experienced operators, or because of gas-filled intestinal loops, or obesity.10,11 If additional imaging of the abdomen or pelvis is necessary after DUS, contrast-enhanced venous phase computed tomography (CT) or magnetic resonance (MR) imaging are alternatives. Mass effect by tumor or enlarged lymph nodes, iliocaval compression/obstruction, and general venous anatomy can be easily visualized. Additionally, MR imaging can be used for evaluating musculoskeletal or neurologic etiologies.4
Venography with intravascular ultrasound (IVUS) is another modality available for not only assessment but for guiding and establishing the anatomical results of endovascular treatment of abdominal/pelvis venous etiologies of lower limb edema. Although this is an invasive approach, venous lesions, stenoses, and compression can be assessed with sensitivity >85%.12 Venography with IVUS should be reserved for the occasional cases where DUS, CT, or MR imaging are inconclusive or as part of a procedure with the intent to endovascularly treat a venous obstruction.
Although lymphedema is usually a clinical diagnosis, imaging techniques can be used for confirmation or planning for surgical intervention. Direct contrast lymphangiography has largely been abandoned for the evaluation of a swollen extremity due to its technical complexity and complications. Currently, lymphoscintigraphy is the gold standard. It generally utilizes Tc-99m radiolabeled sulphur colloid which is injected in the intradermally in the second and third web spaces of the feet with serial imaging using a scintigraphic camera for the assessment of lymph movement from the feet to the chest.7,8 Indocyanine green (IGD) lymphography has been increasingly used to identify and stage lymphedema by plastic surgeons prior to and during certain types of treatment and is also used for objective staging and follow-up after surgery.13 MR lymphography with and without contrast is a promising method providing good imaging and planning but rigorous assessment of the examination, availability, and interpretation expertise is lacking.14,15
Diagnostic algorithm for chronic lower extremity swelling
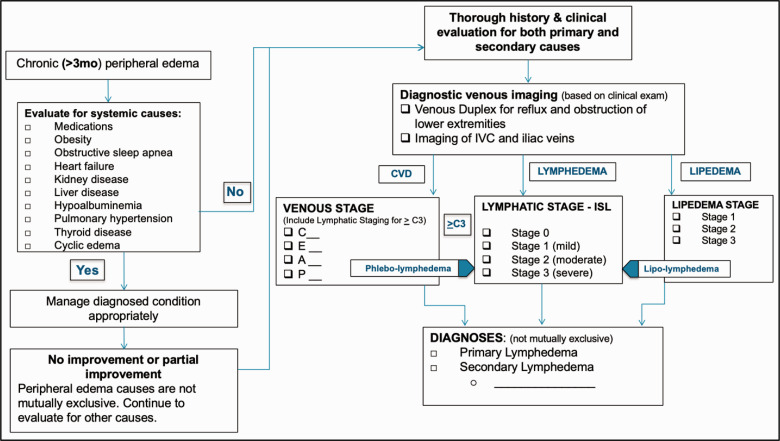
A practical diagnostic approach based on the concepts discussed above is illustrated in Figure 1. If there are no identified systemic causes or if there is no improvement or partial improvement following management of defined systemic causes, a more comprehensive evaluation for underlying primary or secondary causes is undertaken using the logic discussed in the prior sections. The diagnostic steps should be tailored to the patient’s history, clinical exam, and the potential benefits of interventions that require imaging to avoid over-testing and follow a cost-effective approach. In an era where multiple tests are ordered often without a proper history and clinical examination, it is vital to reduce costs and appropriate allocation of resources.
Figure 1.
Proposed diagnostic algorithm for chronic lower extremity swelling.
Evaluation includes a more detailed venous and lymphatic history and physical as well as a venous DUS of the lower extremities. Evaluation of the venous system includes imaging for reflux and obstruction. Duplex ultrasound offers good differential diagnosis and can detect other causes such as popliteal cysts, masses, hematoma, effusions, etc.16 If venous pathology is identified, proper staging of the patient’s chronic venous disease should be performed using the CEAP classification. Patients with advanced venous disease (chronic venous insufficiency or C3–C6) and swelling usually have combined venous and lymphatic disease. It is now accepted that over 90% of reabsorption of the capillary filtrate occurs via the lymphatics and not the venules. Increased filtration caused by venous hypertension can overwhelm the capacity of the lymphatic system and lead to swelling. When this occurs for an extended period, irreversible injury to the lymphatics can lead to swelling that will not resolve after correction of the venous pathology; such swelling is clinically described as phlebolymphedema. Unabated venous hypertension increases capillary filtration which can ultimately overload lymphatic fluid transportation leading to clinical phlebolymphedema.17,18 Venous disease by this mechanism, not cancer and its therapeutics, is now recognized as the most common cause of lymphedema in the western world.1
If the cause of the swelling is likely venous based on appearance but if venous disease is either not identified by lower extremity DUS or if the severity of the venous findings does not completely explain the degree of swelling, a venous DUS of the pelvic veins is suggested. DUS is also suggested for recent slow onset unilateral or bilateral edema in older patients not otherwise explained to exclude retroperitoneal masses compressing the IVC or iliac veins in the abdomen and pelvis.
Obesity can functionally cause iliac vein and IVC obstruction resulting in edema with all the CVD stigmata without identified infra-inguinal venous disease. Although iliac vein DUS, CT, or MR may be needed in cases of more recent slowly developing edema to exclude a mass, the finding of an iliac vein compression by an iliac artery is likely of less importance than morbid obesity as a cause and the latter should be addressed first.
Venous imaging is normal in most patients with primary lymphedema and lipedema. Both pathologies are mostly diagnosed based on history and characteristic features on physical exam. However, it is important to recognize that not all patients have these classic findings. Lymphatic imaging may be helpful when the typical appearance of lymphedema is not present or when surgical treatment is being considered in patients with no evidence of significant venous disease. DUS can help identify patients with lymphedema and lipedema by excluding significant venous disease and demonstrating subcutaneous fluid or excessive adipose tissue accumulation, respectively. Appropriate staging of these patients is part of the evaluation and helpful in management and to follow progression of disease.19,20
The diagnostic steps should be tailored to the patient’s history and clinical exam to avoid over-testing and follow a cost-effective approach. In an era where multiple tests are ordered often without a proper history and clinical examination, it is vital to reduce costs and appropriate allocation of resources. This is particularly true for patients with leg edema as it is very common finding both in an acute and chronic stage.
Conclusions
In approaching lower limb edema, a variety of etiologies must be considered. Careful history and physical examination are essential in the differentiation of causes and subsequent selection of cost effective and appropriate diagnostic testing. This differential diagnostic pathway facilitates a systematic approach to patients presenting with either acute or chronic leg swelling in a unilateral or bilateral fashion.
Acknowledgments
Acknowledgements
The proposed algorithm (Figure 1) in addition to the authors (AG, NL, SD) was constructed by Anthony Comerota, Thomas O’Donnell, Christopher Pittman.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
None required.
Guarantor
NL.
Contributorship
AG and NL were involved with conception and design of the manuscript. All authors researched, wrote, reviewed and edited the manuscript and approved the final version of the manuscript.
ORCID iD
Pamela S Kim https://orcid.org/0000-0003-4578-5844
References
- 1.Dean SM, Valenti E, Hock K, et al. The clinical characteristics of lower extremity lymphedema in 440 patients. J Vasc Surg Venous Lymphat Disord 2020; 8: 851–859. [DOI] [PubMed] [Google Scholar]
- 2.Ely JW, Osheroff JA, Chambliss ML, et al. Approach to leg edema of unclear etiology. J Am Board Fam Med 2006; 19: 148–160. [DOI] [PubMed] [Google Scholar]
- 3.Evans NS, Ratchford EV. The swollen leg. Vasc Med 2016; 21: 562–564. [DOI] [PubMed] [Google Scholar]
- 4.Trayes KP, Studdiford JS, Pickle S, et al. Edema: diagnosis and management. Am Fam Phys 2013; 88: 102–110. [PubMed] [Google Scholar]
- 5.Thaler HW, Pienaar S, Wirnsberger G, et al. Bilateral leg edema in an older woman. Z Gerontol Geriat 2015; 48: 49–51. [DOI] [PubMed] [Google Scholar]
- 6.Moffatt CJ, Aubeeluck A, Franks PJ, et al. Psychological factors in chronic edema: a case-control study. Lymphat Res Biol 2017; 15: 252–261. [DOI] [PubMed] [Google Scholar]
- 7.Rockson SG. Current concepts and future directions in the diagnosis and management of lymphatic vascular disease. Vasc Med 2010; 15: 223–231. [DOI] [PubMed] [Google Scholar]
- 8.Tiwari A, Cheng KS, Button M, et al. Differential diagnosis, investigation, and current treatment of lower limb lymphedema. Arch Surg 2003; 138: 152–161. [DOI] [PubMed] [Google Scholar]
- 9.Uhl JF, Chahim M, Allaert FA. Static foot disorders: a major risk factor for chronic venous disease? Phlebology 2012; 27: 13–18. [DOI] [PubMed] [Google Scholar]
- 10.Malgor RD, Labropoulos N. Diagnosis of venous disease with duplex ultrasound. Phlebology 2013; 1: 158–161. [DOI] [PubMed] [Google Scholar]
- 11.Garcia R, Labropoulos N. Duplex ultrasound for the diagnosis of acute and chronic venous diseases. Surg Clin North Am 2018; 98: 201–218. [DOI] [PubMed] [Google Scholar]
- 12.Saleem T, Knight A, Raju S. Diagnostic yield of intravascular ultrasound in patients with clinical signs and symptoms of lower extremity venous disease. J Vasc Surg Venous Lymphat Disord 2020; 8: 634–639. [DOI] [PubMed] [Google Scholar]
- 13.Yamamoto T, Narushima M, Doi K, et al. Characteristic indocyanine green lymphography findings in lower extremity lymphedema: the generation of a novel lymphedema severity staging system using dermal backflow patterns. Plast Reconstr Surg 2011; 127: 1979–1986. [DOI] [PubMed] [Google Scholar]
- 14.Chavhan GB, Amaral JG, Temple M, et al. MR lymphangiography in children: technique and potential applications. Radiographics 2017; 37: 1775–1790. [DOI] [PubMed] [Google Scholar]
- 15.Pabon-Ramos WM, Raman V, Schwartz FR, et al. Magnetic resonance lymphangiography of the central lymphatic system: technique and clinical applications. J Magn Reson Imaging 2020. Epub ahead of print. DOI: 10.1002/jmri.27069. [DOI] [PubMed] [Google Scholar]
- 16.Labropoulos N, Shifrin DA, Paxinos O. New insights into the development of popliteal cysts. Br J Surg 2004; 91: 1313–1318. [DOI] [PubMed] [Google Scholar]
- 17.Levick JR, Michel CC. Microvascular fluid exchange and the revised Starling principle. Cardiovasc Res 2010; 87: 198–210. [DOI] [PubMed] [Google Scholar]
- 18.Mortimer PS, Rockson SG. New developments in clinical aspects of lymphatic disease. J Clin Invest 2014; 124: 915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Internal Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2013 consensus document of the International Society of Lymphology. Lymphology 2013; 46: 1–11. [PubMed] [Google Scholar]
- 20.Szél E, Kemény L, Groma G, et al. Pathophysiological dilemmas of lipedema. Med Hypotheses 2014; 83: 599–606. [DOI] [PubMed] [Google Scholar]