Abstract
Black and Hispanic communities in the U.S. have endured a disproportionate burden of COVID-19-related morbidity and mortality. Racial and ethnic health disparities such as these are frequently aggravated by inequitable access to healthcare resources in disadvantaged communities. Yet, no known studies have investigated disadvantaged communities' access to COVID-19-related healthcare resources. The current study accordingly examined racial and ethnic differences in (1) April 2020 COVID-19 total and positive viral test rates across 177 New York City (NYC) ZIP Code Tabulation Areas (ZCTA); and (2) November 2019–April 2020 licensed and intensive care unit (ICU) hospital bed access across 194 NYC ZCTAs. Pairwise analyses indicated higher COVID-19 total and positive test rates per 1000 persons in majority Black and Hispanic vs. majority White ZCTAs (CI [0.117, 4.55]; CI [2.53, 5.14]). Multiple linear regression analyses indicated that higher percentage of Black and Hispanic residents predicted more total COVID-19 tests per 1000 persons (p < 0.05). In contrast, majority Black and Hispanic ZCTAs had fewer licensed and ICU beds (CI [6.50, 124.25]; CI [0.69, 7.16]), with social disadvantage predicting lower licensed and ICU bed access per 1000 persons (p < 0.01). While news reports of inequitable access to COVID-19-related healthcare resources in ethnocultural minority communities have emerged, this is the first study to reveal that social disadvantage may be a major driver of hospital resource inequities in Black and Hispanic communities. Thus, it will be imperative to enact policies that ensure equitable allocation of healthcare resources to socially disadvantaged communities to address current and future public health crises.
Keywords: Covid-19, Health disparities, Social disadvantage, Race, Ethnicity, Hospital resources, Viral testing
1. Introduction
Socially disadvantaged communities in the U.S. have borne a disproportionate burden of COVID-19-related morbidity and mortality, with Black and Hispanic communities enduring among the nation's heaviest rates of COVID-19 incidence and deaths—paralleling prior viral pandemics (Centers for Disease Control and Prevention, 2020a; 2020b; Garg, 2020; Hutchins et al., 2009). These disparate COVID-19-related morbidity and mortality rates reflect a longstanding history of systemic racism, which has produced limited socioeconomic opportunities and unjust social conditions in U.S. racial/ethnic minority communities that contribute to glaring health disparities (Boyd et al., 2020; Poteat et al., 2020). For example, without a universal healthcare system in the U.S., Black and Hispanic Americans are frequently faced with inequitable access to expensive, robust health insurance exchanges (Kirby and Kaneda, 2005; Poteat et al., 2020). This correspondingly leads to high out-of-pocket healthcare costs that discourage help-seeking behaviors and health service use for treating chronic diseases, such as obesity and diabetes, which (1) are more prevalent among Black and Hispanic compared to White Americans, and (2) have been identified as comorbidities known to exacerbate COVID-19 severity (Carnethon et al., 2017; Richardson et al., 2020). This linear accumulation of inequities illustrates heightened COVID-19-related risk, while serving as a harbinger of the cumulative impact of systemic inequities plaguing socially disadvantaged communities in the U.S. (Chowkwanyun and Reed, 2020; Williams and Cooper, 2020).
According to theories around social determinants of health, racial and ethnic health disparities are largely a function of inequitable access to health-promoting living and working conditions (Braveman et al., 2011). For example, Blacks and Hispanics are more likely to live in underresourced neighborhoods that lack access to key healthcare resources (Kirby and Kaneda, 2005). Fundamental cause theory posits that racial and ethnic disparities in new diseases are driven not by a disease's specific characteristics or risk factors but by social determinants—e.g., socioeconomic status, residential segregation—that inhibit disadvantaged groups' access to essential health-protective resources for avoiding disease (Centers for Disease Control and Prevention 2020; Phelan et al., 2010). This theory discloses the critical influence that unequal access to health-protective resources may have in driving COVID-19-related health disparities. Yet, no known studies have examined access to essential COVID-19-related healthcare resources (i.e., viral tests, hospital beds) in Black and Hispanic communities, or the extent to which social disadvantage predicts access to these resources. This, in turn, has limited policymakers' ability to target and reduce COVID-19-related racial and ethnic disparities (Morrison, 2020).
To address this gap, we compared access to COVID-19-related resources of viral testing and licensed (i.e., the number of beds any given hospital is licensed to operate) and intensive care unit (ICU) hospital beds in majority Black and Hispanic vs. majority White communities in New York City (NYC). NYC has one of the nation's largest hospital systems—comprising acute care, community, teaching, and research hospitals—which includes the NYC Health+ public hospital system that serves patients on publicly subsidized health insurance exchanges (Medicare, Medicaid), as well as those that do not have health insurance. We examined NYC because it possessed the nation's most COVID-19 cases during the April 2020 peak in morbidity and mortality, with approximately 6206 positive test cases, 1682 hospitalizations, and 571 confirmed deaths reported on April 6, 2020: NYC's single worst day of COVID-19-related morbidity and mortality (NYC Health, 2020b). Finally, with NYC Black and Hispanic populations bearing a disproportionate COVID-19 burden—age-adjusted rates of hospitalized cases and fatalities per 100,000 persons as of May 13, 2020 of 448.3 and 265.0 for Blacks and 367.7 and 259.2 for Hispanics vs. 195.6 and 130.3 for Whites, respectively (NYC Health, 2020b)—examining the distribution of healthcare resources before and during the April 2020 COVID-19 peak in NYC may serve to inform policies and practices that effectively reduce these notable health disparities.
2. Methods
2.1. Data
Using NYC Department of Health and Mental Hygiene data from April 6, 2020 (NYC Health, 2020b), we identified all NYC Zip Code Tabulation Areas (ZCTA) with publicly-reported COVID-19 testing data, then classified each ZCTA as composed of either majority Black and Hispanic (i.e., ≥ 51% Black and Hispanic) or majority White (i.e., ≥ 51% non-Hispanic White). With the vast COVID-19 disparities in Black and Hispanic communities, this classification served to (1) illustrate resource disparities in these communities, while (2) accounting for the considerable overlap of Black and Hispanic residents within NYC ZCTAs. Study analyses were situated at the ZCTA unit of analysis, with the following COVID-19-related resource variables by ZCTA: (1) total and positive COVID-19 tests per 1000 persons, and (2) November 2019, March 2020, and April 2020 licensed and ICU hospital bed counts for all NYC hospitals with 24-h emergency departments treating COVID-19 patients (Melby et al., 2020; NYC Health, 2020a). This study utilized publicly available data aggregated to ZCTAs that did not involve human subjects, and was thus determined to be exempt from ethical compliance by the Chapman University Institutional Review Board.
To calculate licensed and ICU hospital bed variables, we geolocated all hospitals meeting the above criteria, identified each hospital's total number of licensed and ICU beds (Melby et al., 2020; NYC Health, 2020a), and mapped total licensed and ICU beds per 1000 persons within 1.22 miles of each ZCTA centroid (generating 2.44 mile buffers) to match U.S. residents' average distance of 2.44 miles to the nearest hospital (Centers for Disease Control and Prevention, 1999). Finally, we collected 2018 American Community Survey 5-Year data to obtain ZCTA population density, percent Black and Hispanic, percent female, percent over 50 years of age, median household income, and percent unemployment (U.S. Census Bureau, 2018). All data were joined at the ZCTA-level in ArcMap v.10.5.
2.2. Statistical analysis
Analyses were conducted in IBM SPSS v.25. We calculated mean number of licensed/ICU hospital beds per 1000 persons within 1.22-mile buffers of each NYC ZCTA centroid for November 2019 (pre-pandemic), and March (early pandemic) and April (pandemic peak in NYC) 2020 to illustrate temporal resource change in response to the dramatic increase in COVID-19 related morbidity and mortality. Independent t-tests compared majority Black and Hispanic vs. majority White ZCTAs for April 6, 2020 (1) total and positive COVID-19 tests per 1000 persons (n = 177 ZCTAs with publicly-available testing data); and (2) licensed and ICU hospital beds per 1000 persons (n = 194). To explore associations between COVID-19 resources and social disadvantage, three stepwise multiple linear regression models were developed with dependent variables—per 1000 persons—consisting of total tests, licensed beds, and ICU beds, respectively, regressed by (step 1) demographic variables of ZCTA population density, percent Black and Hispanic, percent female, and percent over 50 years of age; and (step 2) social disadvantage variables of median household income and percent unemployment. Variance inflation factors were below 2.60.
3. Results
As seen in Fig. 1 , in November 2019, per 1000 persons, majority White ZCTAs had on average 69.5 licensed beds whereas majority Black and Hispanic ZCTAs had 8.0 beds—a striking disparity in pre-pandemic resources. On March 26, 2020, with the COVID-19 epidemic overwhelming NYC hospital systems, licensed beds per 1000 persons increased in majority White ZCTAs to 73.5 beds vs. 8.4 beds in majority Black and Hispanic ZCTAs. By April 6, 2020—the single day peak of COVID-19 cases in NYC—mean licensed beds per 1000 persons increased to 75.5 in majority White vs. 10.1 in majority Black and Hispanic ZCTAs.
Fig. 1.
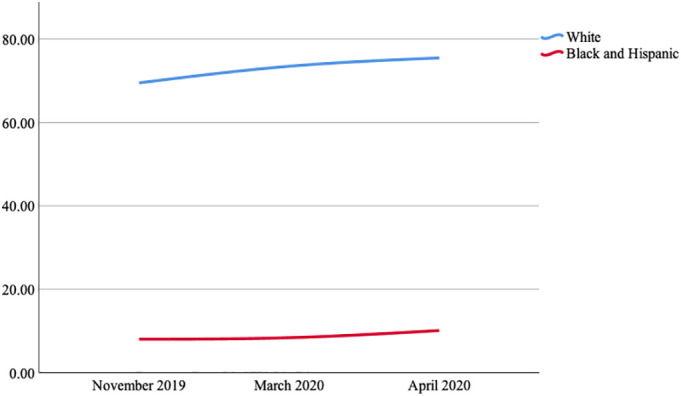
Licensed Hospital Beds Per 1000 Persons in New York City Zip Code Tabulation Areas by Date by Race and Ethnicity.
Independent t-tests indicated that COVID-19 total and positive tests were higher per 1000 persons in majority Black and Hispanic vs. majority White ZCTAs (t = 2.08, 95% CI [0.117, 4.55]; t = 5.79, 95% CI [2.53, 5.14]), with 23.3 vs. 21.0 total tests and 14.2 vs. 10.4 positive tests, respectively. Yet, despite having higher COVID-19 positive test rates—suggesting greater COVID-19 burden and resource need—by April 6, majority Black and Hispanic ZCTAs still had fewer licensed and ICU beds per 1000 persons vs. majority White ZCTAs (t = 2.21, 95% CI [6.50, 124.25]; t = 2.41, 95% CI [0.69, 7.16]), with differences of 10.1 vs. 75.5 licensed hospital beds and 0.4 vs. 4.4 ICU beds per 1000 persons, respectively.
Regressions indicated that our predictor demographic and social disadvantage variables accounted for 28.0%, 20.0%, and 22.7% of the variance for our three COVID-19-related resource variables of total tests, licensed beds, and ICU beds per 1000 persons, respectively. For the total tests model, ZCTA percent Black and Hispanic and percent over 50 years of age significantly predicted (p < 0.05) increases in total COVID-19 tests administered per 1000 persons, whereas population density significantly predicted (p < 0.001) decreases in total COVID-19 tests administered per 1000 persons (Table 1 ). For both beds models, population density, percent female, and median household income significantly predicted (p < 0.05) licensed and ICU bed increases per 1000 persons (Table 1). Notably, ZCTA percentage Black and Hispanic significantly predicted licensed and ICU bed decreases in Step 1, but did not in Step 2 after accounting for our social disadvantage variables of median household income and percent unemployment.
Table 1.
Regression of predictor variables on total tests, licensed beds, and ICU beds per 1000 persons. Boldface indicates statistical significance (*p < 0.05 **p < 0.01 ***p < 0.001). Final model β reported.
| Total tests |
Licensed beds |
ICU beds |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| R2 | β | (95% CI) | R2 | β | (95% CI) | R2 | β | (95% CI) | |
| Step 1 | 0.29*** | 0.15*** | 0.17*** | ||||||
| Population density | −0.367*** | (−0.00012, −0.00005) |
0.275*** | (0.001, 0.002) | 0.280*** | (0.000031, 0.000099) | |||
| Percent black/Hispanic | 0.216* | (0.003, 0.100) | 0.095 | (−0.537, 1.446) | 0.072 | (−0.032, 0.066) | |||
| Percent female | −0.088 | (−0.674, 0.163) | 0.177* | (1.488, 18.008) | 0.189** | (0.113, 0.924) | |||
| Percent age 50+ years | 0.275*** | (0.147, 0.484) | −0.106 | (−1.258, 5.581) | −0.086 | (−0.080, 0.255) | |||
| Step 2 | 0.28 | 0.20** | 0.23*** | ||||||
| Median household income | 0.003 | (−0.000043, 0.000042) | 0.253** | (0.001, 0.003) | 0.259** | (0.000015, 0.000096) | |||
| Percent unemployment | −0.038 | (−0.623, 0.424) | −0.150 | (−18.507, 2.911) | −0.164 | (−0.951, −0.100) | |||
4. Discussion
Study findings revealed that during the March–April COVID-19-related surge in hospital bed capacity throughout NYC, despite bearing a disproportionate burden of COVID-19-related hospitalizations and deaths, majority Black and Hispanic communities—which possessed dramatically lower pre-pandemic bed capacities—continued to suffer alarming disparities in bed capacity vs. majority White communities (Centers for Disease Control and Prevention, 2020b; Garg, 2020). While some patients were transferred to hospitals in more affluent areas that could accommodate them, this highly inequitable access to healthcare resources during the surge mirrors the well-publicized installation of 2500 emergency hospital beds within predominantly White, high-income locations including Manhattan's Javits Center and Pier 90, and Brooklyn Cruise Terminal, while patients in nearby majority Black and Hispanic-serving hospitals (e.g., Elmhurst Hospital) perished due to inadequate bed capacities (Dwyer, 2020).
More positively, when we examined COVID-19 testing rates, majority Black and Hispanic communities completed more tests, possibly indicating that NYC officials appropriately allocated viral testing resources to communities based on need. All testing in NYC was free and confidential, with hundreds of testing sites and mobile testing units throughout the city. Thus, directly addressing cost, anonymity, and geographic accessibility of viral testing may have encouraged help-seeking behaviors and health service use within NYC's Black and Hispanic communities, paving the way for curbing the cumulative impact of broader health disparities and systemic inequities (Braveman et al., 2011; Poteat et al., 2020). Unfortunately, COVID-19 positive test rates were higher in majority Black and Hispanic communities, indicating that Black and Hispanic residents may have been hindered by limited access to health-promoting living and working conditions. Furthermore, access to licensed and ICU beds in majority Black and Hispanic communities remained shockingly low despite the surge, with this disparity appearing to be partially accounted for by median household income in our regressions. Thus, our findings align with fundamental cause theory in suggesting that social disadvantage, as evidenced by median household income in this study, was a primary driver of inequitable hospital bed access that affected NYC's Black and Hispanic communities during the COVID-19 crisis (Phelan et al., 2010).
There are several limitations to the current study. First, the study may have benefitted from supplementary analyses accounting for access to additional health-promoting resources such as health clinics, COVID-19 viral testing centers, and personal protective equipment (e.g., N95 respirators and surgical masks). Second, ZCTA-level analyses of prevalence of comorbidities known to associate with COVID-19 severity (e.g., obesity, diabetes, hypertension) may have provided a more robust understanding of Black and Hispanic morbidity and mortality in the NYC context (Richardson et al., 2020). Third, ZCTA-level race and ethnic total and positive viral testing data have yet to be released, thus limiting our ability to identify COVID-19-related health disparities within ZCTAs. Fourth, we recognize that ZCTA-level total and positive viral testing data may not fully characterize the COVID-19 burden in NYC's Black and Hispanic communities. Finally, we were unable to make causal inferences due to the cross-sectional design of this study.
5. Conclusion
Without a universal healthcare system, appropriate allocation of limited life-saving resources to overwhelmed hospital systems in disadvantaged communities is critical to reducing morbidity and mortality during public health crises. News reports have revealed that while NYC hospitals serving disadvantaged communities were besieged by COVID-19 patients, driving mortality rates, some patients were eventually transferred to hospitals in less affected, more affluent communities possessing thousands of empty critical-care beds (Dwyer, 2020). However, temporary solutions such as these that attempt to compensate for the lack of an integrated healthcare system only highlight longstanding systemic racism that has contributed to community-level resource inequities that compromise health and well-being in disadvantaged communities. Finally, policies stemming from systemic racism, which have historically limited access to socioeconomic and healthcare resources in Black and Hispanic communities in the U.S. (Boyd et al., 2020; Poteat et al., 2020), may have contributed to inequitable mortality rates in NYC. Therefore, addressing systemic racism and long-standing resource inequities will be critical to redressing racial and ethnic health disparities in U.S. communities.
Funding
This work was supported by COVID-19 Rapid Response Research funding provided by the Kay Family Foundation via Chapman University.
Declaration of Competing Interest
The authors have no conflicts of interest to disclose.
Acknowledgments
Jason A. Douglas would like to thank his research team—Jacy Sera, Elmer Camargo, Olivia Lounsbury, Emma Hughes, Emma Rothleutner, and Jeremy Tang—for their tireless data collection efforts.
References
- Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; 2020, March 31. Coronavirus Disease 2019 (COVID-19) in the U.S.https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html [Google Scholar]
- Boyd R.W., Lindo E.G., Weeks L.D., McLemore M.R. On racism: A new standard for publishing on racial health inequities. Health Affairs Blog. 2020 doi: 10.1377/hblog20200630.939347. [DOI] [Google Scholar]
- Braveman P., Egerter S., Williams D.R. The social determinants of Health: coming of age. Annu. Rev. Public Health. 2011;32(1):381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- Carnethon Mercedes R., Jia Pu, George Howard, Albert Michelle A., Anderson Cheryl A.M., Bertoni Alain G., Mujahid Mahasin S., Latha Palaniappan, Taylor Herman A., Monte Willis, Yancy Clyde W. Cardiovascular Health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136(21):e393–e423. doi: 10.1161/CIR.0000000000000534. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau . US Census Bureau; 2018. 2018 Data Profiles | American Community Survey.https://www.census.gov/acs/www/data/data-tables-and-tools/data-profiles/ [Google Scholar]
- Centers for Disease Control and Prevention Distance to Nearest Hospital reference. 1999:8. https://www.cdc.gov/nchs/data/ahcd/distance_to_nearest_hospital_file.pdf [Google Scholar]
- Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; 2020, Februry 11. COVID-19 in Racial and Ethnic Minority Groups.https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html [Google Scholar]
- Chowkwanyun M., Reed A.L. Racial Health disparities and Covid-19—caution and context. N. Engl. J. Med. 2020;383(3):201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- Dwyer J. Nearby Was “Plenty of Space”. The New York Times; 2020, May 14. One hospital was besieged by the virus.https://www.nytimes.com/2020/05/14/nyregion/coronavirus-ny-hospitals.html [Google Scholar]
- Garg S. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 states, march 1–30, 2020. MMWR. Morbidity and Mortality Weekly Report. 2020;69 doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NYC Health . 2020. 213 Hospitals in New York with total beds.https://profiles.health.ny.gov/hospital/bed_type/Total+Beds [Google Scholar]
- NYC Health COVID-1 Data. 2020. https://www1.nyc.gov/site/doh/covid/covid-19-data.page
- Hutchins S.S., Fiscella K., Levine R.S., Ompad D.C., McDonald M. Protection of racial/ethnic minority populations during an influenza pandemic. Am. J. Public Health. 2009;99(S2):S261–S270. doi: 10.2105/AJPH.2009.161505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby J.B., Kaneda T. Neighborhood socioeconomic disadvantage and access to Health care. J. Health Soc. Behav. 2005;46(1):15–31. doi: 10.1177/002214650504600103. [DOI] [PubMed] [Google Scholar]
- Melby C., Gu J., Rojanasakul M. 2020. Mapping New York City Hospital beds as coronavirus cases surge.https://www.bloomberg.com/graphics/2020-new-york-coronavirus-outbreak-how-many-hospital-beds/ [Google Scholar]
- Morrison A. Democratic lawmakers call for racial data in virus testing. AP NEWS. 2020, March 30 https://apnews.com/c0e58c2e0de70169ef000ce3666c285a [Google Scholar]
- Phelan J.C., Link B.G., Tehranifar P. Social conditions as fundamental causes of Health inequalities theory, evidence, and policy implications. J. Health Soc. Behav. 2010;51(1 suppl):S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Poteat T., Millett G., Nelson L.E., Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann. Epidemiol. 2020 doi: 10.1016/j.annepidem.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., Barnaby D.P., Becker L.B., Chelico J.D., Cohen S.L., Cookingham J., Coppa K., Diefenbach M.A., Dominello A.J., Duer-Hefele J., Falzon L., Gitlin J., Hajizadeh N., Harvin T.G. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020 doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Cooper L.A. COVID-19 and Health Equity—A New Kind of “Herd Immunity”. JAMA. 2020;323(24):2478–2480. doi: 10.1001/jama.2020.8051. [DOI] [PubMed] [Google Scholar]


