Abstract
The pulmonary manifestations of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection or coronavirus disease 2019 (COVID-19) are well known. The literature on neurological manifestations and complications in patients with COVID-19 has been increasing but is still sparse. At present, there are only a few reported case reports and clinical studies on neurological manifestations of COVID-19, of which ischemic stroke is one of the most common ones. Coagulopathy and vascular endothelial dysfunction have been proposed as the complications of COVID-19 which can ultimately lead to ischemic stroke. In this case report, we present a case of multifocal ischemic stroke in a patient with COVID-19. This patient had persistent encephalopathy and dysarthria after recovering from hypoxic respiratory failure and subsequently developed ischemic stroke in multiple vascular territories during hospital admission.
Abbreviations: COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; ATS/IDSA, American Thoracic Society and Infectious Disease Society of America; CT, computed tomography; RT PCR, reverse transcription polymerase chain reaction; L, liters; μl, microliters; MRI, magnetic resonance imaging; ng, nanogram; BUN, blood urea nitrogen; CRP, C-reactive protein; aPTT, activated partial thromboplastin time; DWI, diffusion weighted image; ADC, apparent diffusion coefficient; FLAIR, fluid attenuated inversion recovery; SWI, susceptible weighted imaging
Keywords: Coronavirus disease 2019, COVID-19, Embolic stroke, Severe acute respiratory syndrome coronavirus 2, SARS-CoV-2, Stroke, MRI brain
Highlights
-
•
Hypercoagulopathy and vascular endothelial dysfunction have been proposed as complications of COVID 19 which can lead to stroke.
-
•
Diagnoses of stroke in critically ill patients hospitalized with COVID-19 using MRI brain can be challenging due to multiple factors.
-
•
Patient with COVID-19 with stroke in multiple vascular territories after he had persistent encephalopathy and dysarthria.
-
•
MRI brain is more sensitive and specific modality to detect brain tissue that has been damaged by an ischemic stroke than a CT head.
1. Introduction
In December 2019, a novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) originated in Wuhan, China, which is now a worldwide pandemic [[1], [2], [3]]. The pulmonary manifestations of coronavirus disease 2019 (COVID-19) are well known. The evidence of neurological manifestations and complications in patients with COVID-19 has been increasing but is still sparse. Currently, there are a few reported case reports and clinical studies on neurological manifestations of COVID-19. Stroke is one of the major neurological complications seen in patients with COVID-19 [[3], [4], [5]].
According to the Mao et al. study, 5% of hospitalized patients in Wuhan had acute strokes [6]. However, patients were diagnosed based on clinical examination and only head computed tomography (CT), magnetic resonance imaging (MRI) of brain was avoided to reduce the risk of infection. Diagnosis of stroke in patients hospitalized with COVID-19 using MRI brain can be challenging due to multiple factors, which includes risk of cross contamination to other patients and technologists, prolonged down time for sanitization after each scan delaying the availability of MRI imaging for other patients, inability of critical patients to tolerate lying supine for the prolonged duration of the scan.
In this case report, we present MRI brain findings of a 51-year-old man with COVID-19 who was diagnosed with stroke in multiple vascular territories after he had persistent encephalopathy and dysarthria during his prolonged hospitalization.
2. Case report
A 51-year-old obese male was placed on self-quarantine after testing positive for SARS-CoV-2 on nasopharyngeal swab PCR. He had symptoms of fever, mild cough and diarrhea for a few days. Four days after the initial diagnosis, he presented to the Emergency Department with worsening dyspnea and was found to have an oxygen saturation of 74% on room air. His medical comorbidities included hypertension and hyperlipidemia. Patient was febrile, tachypneic, tachycardic and appeared in acute distress, using his abdominal accessory muscles for respiration.
Initial workup revealed lymphopenia, mild hyponatremia, elevated transaminases and inflammatory markers including C reactive protein 70.4 mg/L (range < 8 mg/L), lactate dehydrogenase 611 U/L (98–192 U/L) and ferritin 1138 ng/mL (range 24–336 ng/mL). D-dimer was also mildly elevated at 306 ng/mL (range < 232 ng/mL). His aPTT was 29.9 s and platelet count were 174,000/uL.
Chest radiograph demonstrated bilateral peripherally based infiltrates. Subsequently, patient underwent CT angiogram of the chest and venous doppler study of lower extremities for suspected pulmonary embolism and deep vein thrombosis respectively; both studies were negative.
Patient was admitted to the intensive care unit and required intubation with mechanical ventilation for acute hypoxic respiratory failure secondary to SARS-CoV-2 infection. He also required vasopressors for hypovolemic shock. Patient was treated with hydroxychloroquine, azithromycin, tocilizumab infusion. On the fourth day after admission, patient became oliguric and was noted to have D-dimer elevated to 5163 ng/mL. He was diagnosed with acute kidney injury due to ineffective renal perfusion. He underwent hemodialysis for five consecutive days with gradual improvement of his renal function. The patient was maintained on heparin for deep venous thrombosis prophylaxis and received heparin as needed during dialysis. He was extubated after 10 days of mechanical ventilation during which he was mostly comatose with limited neurological examination. Upon extubating, his speech was noted to be dysarthric and he was noted to be encephalopathic.
CT brain without contrast was ordered on day 17 after admission and did not show any acute intracranial abnormalities. He was re-tested negative for COVID-19 twenty days after admission. For further workup of persistent encephalopathy, slurred speech and lack of improvement, MRI of the brain without contrast was obtained on day 23 of admission.
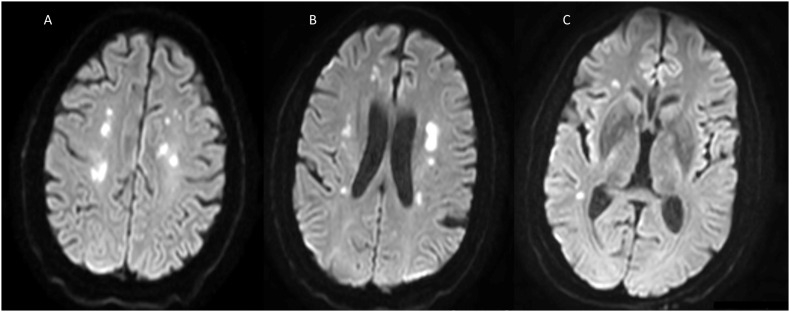
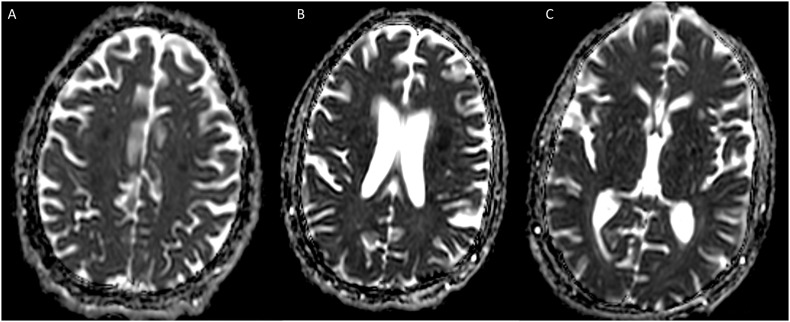
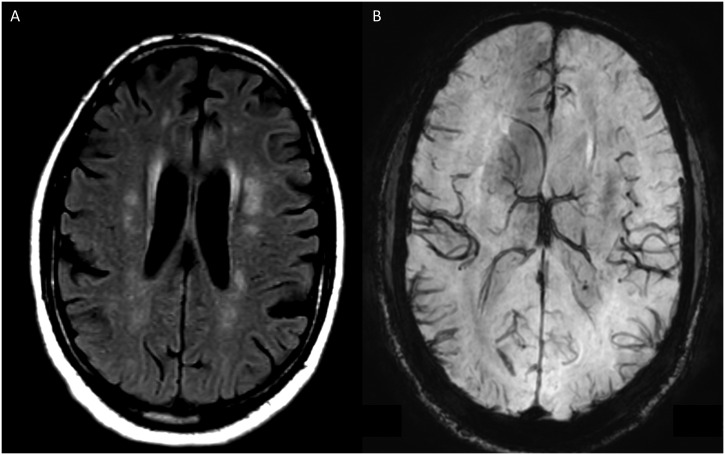
MRI of the brain demonstrated multiple areas of restricted diffusion in the frontal, parietal and temporal lobes bilaterally on diffusion weighted imaging (DWI) sequence (Fig. 1A – 1C) with corresponding hypointense signal on apparent diffusion coefficient (ADC) sequences (Fig. 2A- 2C), consistent with acute ischemic strokes. These areas also demonstrated hyperintensity in frontoparietal periventricular deep white matter on T2 fluid attenuated inversion recovery sequence (T2-FLAIR) (Fig. 3A). Axial susceptible weighted imaging (SWI) demonstrate no signal drop out to suggest any abnormal blood product for hemorrhage (Fig. 3B).
Fig. 1.
Axial images of the Diffusion Weighted Imaging (DWI) sequence at different levels (A, B and C) demonstrates multifocal diffusion restriction (hyperintense signal on DWI) involving the centrum semiovale, frontoparietal and temporal periventricular deep white matter.
Fig. 2.
Axial images of the Apparent diffusion coefficient (ADC) sequence at different levels (A, B and C) demonstrates hypointense signals corresponding to hyperintense foci on DWI, involving centrum semiovale, frontoparietal and temporal deep white matter consistent with acute ischemic stroke.
Fig. 3.
T2- Fluid attenuated inversion recovery (T2-FLAIR) axial image (Fig. A) demonstrates hyperintensity corresponding to the restricted diffusion areas in frontoparietal periventricular deep white matter. Corresponding susceptible weighted imaging (SWI) axial image (Fig. B) demonstrates no signal drop out to suggest any abnormal blood products and rules out hemorrhage.
On neurological examination, the National Institute of Health Stroke Scale (NIHSS) was 3 (2 for patient unable to answer the month and his age, and 1 for mild-to-moderate dysarthria). He was not aphasic but had mild dysarthria. Cranial nerves were grossly intact. His motor and sensory exam were normal throughout. Telemetry showed normal sinus rhythm and there was no evidence of atrial fibrillation. Magnetic resonance angiography of the head did not show any intracranial stenosis in anterior or posterior circulation. Carotid Doppler ultrasound did not reveal bilateral carotid stenosis. Transthoracic echocardiogram showed normal left ventricular size and function and was negative for intra-cardiac shunt. Patient was started on aspirin 81 mg and high intensity atorvastatin 40 mg daily. Patient was then discharged to acute rehabilitation unit with a cardiac event monitor for 30 days.
3. Discussion
Stroke is one of the major thrombotic complications seen with SARS-CoV-2 infection. Based on the Mao et al. study [6] and the case series of acute large vessel strokes reported from Oxley et al. [3], all ages are vulnerable. There are several proposed mechanisms for increased risk of cerebrovascular disease during COVID-19 [4,[7], [8], [9]]. Impaired vasoreactivity coupled with complement activation and thrombin production can lead to arterial thrombotic events [9]. As known with any infective causes, SARS-CoV-2 viremia can also lead to a severe cytokine storm in patients with COVID-19, leading to drastic endothelial dysfunction and progressive micro and macrovascular thrombosis. Elevation in the lab values of D-dimer and prothrombin time seen clinically could support this phenomenon [7,8]. Activation of the coagulation cascade leading to disseminated intravascular coagulation can significantly contribute to the multiorgan involvement in patients with COVID-19, resulting in acute ischemic stroke, cerebral venous sinus thrombosis or intracerebral hemorrhage [7,8]. This is the most likely pathophysiology of multiple embolic strokes in bilateral hemispheres described in this case. It is also important to note that our case was on low molecular weight heparin only for deep venous thrombosis (DVT) prophylaxis. He was not placed on therapeutic anticoagulation, which has been a practice at some centers on admission for all COVID-19 patients, when no absolute contraindications exist. It is unclear if therapeutic anticoagulation could have prevented the strokes in this case.
The differential diagnosis for above case includes posterior reversible encephalopathy syndrome (PRES), cerebral venous thrombosis, hypoxic ischemic encephalopathy, acute hemorrhagic necrotizing encephalopathy. In a large Italian multicenter retrospective observational study by Mahammedi A et al., out of 108 COVID-19 cases with acute neurological manifestations, 31% were found to have acute ischemic stroke, 12% had cerebral venous thrombosis, 10% had nonspecific encephalopathy, 6% showed intracranial hemorrhage, whereas 5% each with posterior reversible encephalopathy syndrome (PRES) and acute encephalopathy [10]. Moreover, a case of acute hemorrhagic necrotizing encephalopathy was reported in COVID-19 by Poyiadji et al. [11]. Our patient had multiple etiologies (acute kidney failure requiring hemodialysis, hypoxic respiratory failure, electrolyte disturbances, intensive care unit delirium) to explain his persistent encephalopathy initially but he continued to be encephalopathic even after correction and treatment of those causes. MRI brain was thereby done to rule out a primary neurological cause and it showed multiple embolic ischemic stroke. MRI brain was not suggestive of viral encephalopathy or hemorrhagic necrotizing encephalopathy.
Currently, there is paucity of data to support therapeutic anticoagulation for primary prevention of stroke in COVID-19 patients. However, therapeutic anticoagulation should be strongly considered in patients at high risk for coagulopathy determined by laboratory measures which may include elevated platelet count, prothrombin time, fibrinogen, fibrinogen degradation products and D-dimer [12]. In the future, it will be important to compare the incidence of ischemic stroke in population of patients on prophylactic therapeutic anticoagulation versus only on coagulation for DVT prophylaxis.
In a French study which reported neurologic features in severe SARS-CoV-2 infection in fifty-eight consecutive patients, thirteen patients had MRI brain performed for unexplained encephalopathy symptoms [5]. Two patients were found to have an area of acute stroke and one patient had an area of subacute ischemic stroke [5]. Yet, all three had no focal neurological symptoms. Hence, MRI brain imaging can be a useful modality to diagnose ischemic strokes in patients with persistent neurological symptoms who have recovered from severe COVID-19.
There can be several challenges in obtaining MRI brain imaging in COVID-19 patients. The biggest risk is of cross contamination to other patients and technologists. Also, MRI suite requires prolonged down time for sanitization after each scan which can delay the availability of MRI imaging for other patients. MRI brain imaging can also be labor intensive on many of the COVID-19 patients as they are critically ill on mechanical ventilation and also may be unable to tolerate lying supine for the prolonged duration of the MRI scan. However, since MRI brain is more sensitive and specific modality to detect brain tissue that has been damaged by an ischemic stroke than a CT head [13]. It is important to consider MRI brain for accurate diagnosis in patients with unexplained neurological symptoms in COVID-19. Last but not the least, MRI brain imaging should be considered in all critically ill COVID-19 patients with neurological symptoms, as using clinical diagnosis and CT imaging could be only capturing the tip of the iceberg of cerebrovascular disease in COVID-19 [13].
4. Teaching point
When suspecting stroke timely performing MRI brain imaging could be very essential in all critically ill COVID-19 patients, as it has been found to be more sensitive than other imaging modalities such as CT scan. However, it is to be noted that CT scan is still the first imaging modality for suspected ischemic or hemorrhagic stroke, but MRI should be done diligently for selected COVID-19 patients when the CT is negative or the imaging findings does not correspond to the clinical presentation.
Though there is lagging data on the use of anticoagulants to prevent stroke in COVID-19 patients, therapeutic anticoagulation should be kept under consideration especially in patients with a high risk for hypercoagulopathy.
Consent
West Virginia University, Institutional Review Board approved waiver of HIPPA authorization for this case report. No patient identifiers were used in the case report.
Disclosures
Apoorv Prasad Reports no disclosure.
Saurabh Kataria Reports no disclosure.
Samiksha Srivastava Reports no disclosure.
Dhairya Lakhani Reports no disclosure.
Shitiz Sriwastava Reports no disclosure.
All authors have equally contributed for the paper.
CRediT authorship contribution statement
Drafting the manuscript: Apoorv Prasad, Saurabh Kataria, Samiksha Srivastava, Dhairya Lakhani, Shitiz Sriwastava.
Editing and Final Draft: Apoorv Prasad, Saurabh Kataria, Shitiz Sriwastava.
Declaration of competing interest
All authors declared no potential conflicts of interest.
Acknowledgments
Institutional Review Board of West Virginia University authorized the publication of this case report under protocol #2004958561.
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oxley T.J., Mocco J., Majidi S., Kellner C.P., Shoirah H., Singh I.P. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020:382. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Y., Wang M., Zhou Y., Chang J., Xian Y., Mao L. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. SSRN Electron J. 2020 doi: 10.2139/ssrn.3550025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Helms J., Kremer S., Merdji H., Clere-Jehl R., Schenck M., Kummerlen C. Neurologic features in severe SARS-COV-2 infection. N Engl J Med. 2020;382 doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mao L., Jin H., Wang M., Hu Y., Chen S., He Q. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nath A. Neurologic complications of coronavirus infections. Neurology. 2020;94 doi: 10.1212/WNL.0000000000009455. [DOI] [PubMed] [Google Scholar]
- 8.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J. COVID-19: consider cytokine storm syndromes and immunosuppression. The Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Umapathi T., Kor A.C., Venketasubramanian N., Lim C.C.T., Pang B.C., Yeo T.T. Large artery ischaemic stroke in severe acute respiratory syndrome (SARS) J Neurol. 2004;251 doi: 10.1007/s00415-004-0519-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahammedi A., Saba L., Vagal A., Leali M., Rossi A., Gaskill M. Imaging in neurological disease of hospitalized COVID-19 patients: an Italian multicenter retrospective observational study. Radiology. 2020 doi: 10.1148/radiol.2020201933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19–associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020 doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18 doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Radmanesh A., Raz E., Zan E., Derman A., Kaminetzky M. Brain imaging use and findings in COVID-19: a single academic center experience in the epicenter of disease in the United States. Am J Neuroradiol. 2020 doi: 10.3174/ajnr.a6610. [DOI] [PMC free article] [PubMed] [Google Scholar]