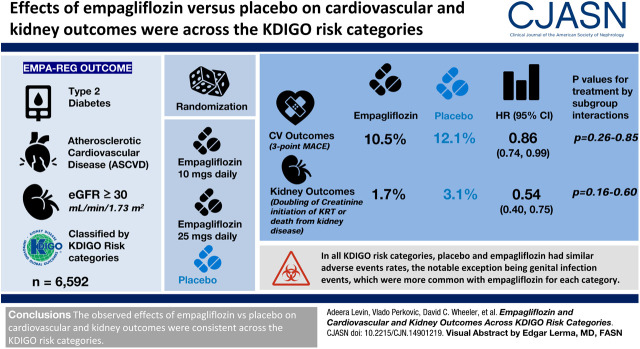
Visual Abstract
Keywords: diabetic nephropathy, empagliflozin, glomerular filtration rate, KDIGO, kidney disease, SGLT2 inhibition
Abstract
Background and objectives
In the Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG Outcome), empagliflozin, in addition to standard of care, significantly reduced risk of cardiovascular death by 38%, hospitalization for heart failure by 35%, and incident or worsening nephropathy by 39% compared with placebo in patients with type 2 diabetes and established cardiovascular disease. Using EMPA-REG Outcome data, we assessed whether the Kidney Disease Improving Global Outcomes (KDIGO) CKD classification had an influence on the treatment effect of empagliflozin.
Design, setting, participants, & measurements
Patients with type 2 diabetes, established atherosclerotic cardiovascular disease, and eGFR≥30 ml/min per 1.73 m2 at screening were randomized to receive empagliflozin 10 mg, empagliflozin 25 mg, or placebo once daily in addition to standard of care. Post hoc, we analyzed cardiovascular and kidney outcomes, and safety, using the two-dimensional KDIGO classification framework.
Results
Of 6952 patients with baseline eGFR and urinary albumin-creatinine ratio values, 47%, 29%, 15%, and 8% were classified into low, moderately increased, high, and very high KDIGO risk categories, respectively. Empagliflozin showed consistent risk reductions across KDIGO categories for cardiovascular outcomes (P values for treatment by subgroup interactions ranged from 0.26 to 0.85) and kidney outcomes (P values for treatment by subgroup interactions ranged from 0.16 to 0.60). In all KDIGO risk categories, placebo and empagliflozin had similar adverse event rates, the notable exception being genital infection events, which were more common with empagliflozin for each category.
Conclusions
The observed effects of empagliflozin versus placebo on cardiovascular and kidney outcomes were consistent across the KDIGO risk categories, indicating that the effect of treatment benefit of empagliflozin was unaffected by baseline CKD status.
Clinical Trial registry name and registration number:
EMPA-REG OUTCOME, NCT01131676
Introduction
CKD occurs in approximately 40% of patients with type 2 diabetes (1) and leads to a higher risk of mortality and morbidity (2,3). CKD is also a strong risk factor for cardiovascular disease (4). For example, in a large Canadian general population cohort of >900,000 individuals, the proportion of deaths from cardiovascular disease was higher with decreasing eGFR, from 28% in individuals with normal kidney function to 58% in patients with kidney failure (5). As such, treatment of CKD places a major burden on health care systems in terms of resources and costs (6,7). Therefore, there is a strong health and economic imperative to improve clinical outcomes in people with CKD and type 2 diabetes (8). Despite the introduction of novel treatment strategies for type 2 diabetes, it remains uncertain if these approaches can positively affect the course of cardiovascular and kidney disease in patients with type 2 diabetes (9).
In the Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG OUTCOME), a large cardiovascular outcome study in patients with type 2 diabetes and established cardiovascular disease (10), the sodium-glucose cotransporter-2 (SGLT2) inhibitor empagliflozin significantly reduced the risk of cardiovascular death by 38%, risk of hospitalization for heart failure by 35% (10), and risk of incident or worsening nephropathy by 39%, and it decreased progression of kidney disease (11). The urinary albumin-creatinine ratio (UACR) also improved, irrespective of baseline UACR levels, although these improvements were of greatest clinical relevance in patients with elevated baseline UACR levels (12).
The Kidney Disease Improving Global Outcomes (KDIGO) CKD classification system provides a two-dimensional framework for categorizing patients on the basis of eGFR and UACR as markers of kidney function and damage (3). These guidelines have evolved over time to include an increasingly detailed description of the relationship between GFR, albuminuria, and prognosis, which has improved our understanding of CKD in multiple populations (3). Patients with low eGFR levels and higher urinary albumin excretion rates are at higher risk of both adverse kidney and adverse cardiovascular outcomes, allowing the KDIGO CKD classification system to be adapted into a risk “heat map” as used in this analysis.
The 2012 KDIGO classification framework is a useful tool for assessing severity of kidney disease. However, it is not known whether this classification system is associated with treatment response. Here, we report a post hoc comparison of cardiovascular and kidney outcomes in participants in EMPA-REG OUTCOME using the KDIGO classification to determine the effect of baseline KDIGO risk category on treatment effect.
Materials and Methods
Study Design
EMPA-REG OUTCOME was a randomized, double-blind, placebo-controlled, multinational trial (NCT01131676; registration date May 27, 2010). Patients entered a 2-week, open-label, placebo run-in prior to randomization (1:1:1) to empagliflozin 10 mg, empagliflozin 25 mg, or placebo once daily in addition to standard of care for type 2 diabetes and cardiovascular risk management. Randomization was performed with the use of a computer-generated random sequence and interactive voice and web response system, and it was stratified according to the glycated hemoglobin (HbA1c) level at screening (<8.5% or ≥8.5%), body mass index at randomization (<30 or ≥30), kidney function at screening (eGFR of 30–59, 60–89, or ≥90 ml/min per 1.73 m2), and geographic region. Investigators were encouraged to treat cardiovascular risk factors in order to achieve optimal standard of care according to local guidelines (10,13).
The EMPA-REG OUTCOME trial was conducted in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonisation Good Clinical Practice guidelines, and it was approved by local authorities. An independent ethics committee or institutional review board approved the clinical protocol at each participating center. All of the patients provided written informed consent before study entry.
Cardiovascular outcome events and deaths were prospectively adjudicated by clinical events committees. Kidney events were reported by investigators and were not adjudicated. The trial continued until at least 691 patients experienced an adjudicated event included in the primary composite outcome: first occurrence of three-point major adverse cardiovascular event (MACE; composite of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke). Kidney function at baseline was assessed using the creatinine-based GFR estimating equations on the basis of the Modification of Diet in Renal Disease (MDRD) formula.
Participants
Eligible patients were adults with type 2 diabetes (HbA1c≥7.0% and ≤9.0% for treatment-naïve patients and HbA1c≥7.0% and ≤10.0% for patients on background glucose-lowering therapy), a body mass index of ≤45 kg/m2, established cardiovascular disease, and eGFR≥30 ml/min per 1.73 m2 (according to MDRD).
Outcomes and Analyses
Prespecified cardiovascular outcomes included three-point MACE and its individual components (i.e., myocardial infarction, stroke, and cardiovascular death), hospitalization for heart failure, and all-cause mortality.
Prespecified kidney outcomes have been previously described in detail and included incident or worsening nephropathy (composite of progression to macroalbuminuria, doubling of serum creatinine accompanied by eGFR of ≤45 ml/min per 1.73 m2, initiation of KRT, or death from kidney disease) and progression to macroalbuminuria (11). Additionally, a post hoc analysis looked at the composite of doubling of serum creatinine, initiation of KRT, or death from kidney disease.
Cardiovascular and kidney outcomes were analyzed in subgroups by baseline KDIGO risk category (3).
Changes in eGFR values were assessed over time alongside a prespecified eGFR slope analysis for three prespecified study periods (treatment initiation effects from baseline to week 4; chronic maintenance treatment effects from week 4 to last value on treatment; and post-treatment effects from last value on treatment to follow-up) (14).
Analyses were performed in patients treated with at least one dose of study drug, and they compared the placebo and pooled empagliflozin groups. A Cox proportional hazards model was used to investigate the consistency of treatment effect on cardiovascular and kidney outcomes across subgroups. The model included terms for age, sex, baseline HbA1c category, baseline body mass index category, geographical region, treatment, baseline KDIGO risk category, and treatment by baseline KDIGO risk category interaction.
Calculation of eGFR slopes within the three prespecified study periods was performed by applying a separate random coefficient model for each period, allowing for random intercept and random slope per patient (14).
Safety data were analyzed by Poisson regression of first event using log of time at risk as offset and including factors for treatment, KDIGO risk category, and treatment by baseline KDIGO risk category interaction, yielding incidence rate ratios to assess differences between the empagliflozin and placebo groups across KDIGO risk categories.
All analyses were performed on a nominal two-sided α=0.05 without adjustment for multiplicity.
Results
The EMPA-REG OUTCOME trial has been described previously (10,13). A total of 7028 patients were randomized to study treatment from September 2010 to April 2013; 7020 patients at 590 sites in 42 countries received one or more doses of study drug (placebo, n=2333; empagliflozin 10 mg, n=2345; empagliflozin 25 mg, n=2342) (11). The median duration of treatment was 2.6 years (interquartile range, 1.9−3.4), and the median observation time was 3.1 years (interquartile range, 2.2−3.6); 97% of patients completed the trial.
Baseline Characteristics
The distribution of patients across the KDIGO risk categories is shown in Table 1. Among 7020 participants, baseline eGFR and UACR measurements were available for 6952 patients (99%; empagliflozin, n=4635; placebo, n=2317). Baseline characteristics and concomitant medications were similar between the placebo and empagliflozin groups across the KDIGO risk categories.
Table 1.
Baseline characteristics and concomitant medications of participants were similar between treatment groups across Kidney Disease Improving Global Outcomes risk categories
| Parameter | Kidney Disease Improving Global Outcomes Risk Categorya | |||||||
|---|---|---|---|---|---|---|---|---|
| Low | Moderately Increased | High | Very High | |||||
| Placebo, n=1099 | Empagliflozin,b n=2223 | Placebo, n=675 | Empagliflozin,b n=1343 | Placebo, n=357 | Empagliflozin,b n=710 | Placebo, n=186 | Empagliflozin,b n=359 | |
| Men | 787 (72) | 1571 (71) | 490 (73) | 970 (72) | 254 (71) | 500 (70) | 136 (73) | 255 (71) |
| Age, yr | 62±9 | 61±8 | 64±9 | 64±9 | 66±9 | 66±8 | 66±8 | 67±8 |
| BMI, kg/m2 | 30.5±5.2 | 30.5±5.2 | 31.0±5.2 | 30.7±5.3 | 30.7±5.4 | 30.6±5.3 | 30.2±5.3 | 30.6±5.7 |
| HbA1c, % | 8.0±0.8 | 8.0±0.8 | 8.1±0.9 | 8.1±0.9 | 8.2±0.9 | 8.2±0.9 | 8.2±0.9 | 8.1±0.8 |
| Systolic BP, mm Hg | 133±16 | 132±15 | 138±17 | 137±17 | 139±20 | 139±19 | 140±19 | 141±18 |
| Diastolic BP, mm Hg | 77±10 | 77±9 | 77±11 | 77±10 | 76±11 | 76±10 | 76±10 | 75±10 |
| LDL cholesterol, mg/dl | 83±34 | 85±35 | 85±34 | 85±36 | 89±39 | 88±37 | 89±39 | 90±40 |
| eGFR (MDRD), ml/min per 1.73 m2 | 83±16 | 84±17 | 74±20 | 74±20 | 60±19 | 61±20 | 44±8 | 43±9 |
| ≥60 | 1099 (100) | 2223 (100) | 470 (70) | 926 (69) | 145 (41) | 286 (40) | 0 | 0 |
| <60 | 0 | 0 | 205 (30) | 417 (31) | 212 (59) | 424 (60) | 186 (100) | 359 (100) |
| UACR, mg/g | ||||||||
| <30 | 1099 (100) | 2223 (100) | 205 (30) | 417 (31) | 76 (21) | 139 (20) | 2 (1) | 10 (3) |
| 30–300 | 0 | 0 | 470 (70) | 926 (69) | 136 (38) | 285 (40) | 69 (37) | 126 (35) |
| >300 | 0 | 0 | 0 | 0 | 145 (41) | 286 (40) | 115 (62) | 223 (62) |
| UACR, median (IQR), mg/g | 7.1 (4.4−14.1) | 8.0 (5.3−14.1) | 43.3 (16.8−94.6) | 43.3 (17.7−89.3) | 141.4 (37.1−630.3) | 134.4 (39.8−484.4) | 406.2 (110.5−908.8) | 422.6 (114.0−1067.0) |
| Background medications | ||||||||
| ACE inhibitors/ARBs | 846 (77) | 1754 (79) | 556 (82) | 1119 (83) | 305 (85) | 585 (82) | 147 (79) | 299 (83) |
| Diuretics | 405 (37) | 841 (38) | 295 (44) | 605 (45) | 172 (48) | 360 (51) | 110 (59) | 216 (60) |
| History of heart failure | 95 (9) | 181 (8) | 77 (11) | 146 (11) | 48 (13) | 84 (12) | 23 (12) | 50 (14) |
| Smoking status | ||||||||
| Never smoked | 464 (42) | 902 (41) | 260 (39) | 556 (41) | 144 (40) | 288 (41) | 80 (43) | 164 (46) |
| Ex-smoker | 489 (45) | 967 (44) | 326 (48) | 623 (46) | 169 (47) | 353 (50) | 85 (46) | 164 (46) |
| Currently smokes | 146 (13) | 354 (16) | 89 (13) | 164 (12) | 44 (12) | 69 (10) | 21 (11) | 31 (9) |
| Duration of diabetes, yr | ||||||||
| ≤1 | 35 (3) | 78 (4) | 11 (2) | 31 (2) | 2 (1) | 14 (2) | 4 (2) | 5 (1) |
| >1–5 | 216 (20) | 424 (19) | 103 (15) | 189 (14) | 41 (12) | 65 (9) | 10 (5) | 25 (7) |
| >5–10 | 301 (27) | 597 (27) | 159 (24) | 344 (26) | 69 (19) | 156 (22) | 35 (19) | 64 (18) |
| >10 | 547 (50) | 1124 (51) | 402 (60) | 779 (58) | 245 (69) | 475 (67) | 137 (74) | 265 (74) |
| Metformin use | 885 (81) | 1752 (79) | 514 (76) | 1022 (76) | 219 (61) | 476 (67) | 104 (56) | 172 (48) |
| Insulin use | 447 (41) | 933 (42) | 338 (50) | 648 (48) | 211 (59) | 412 (58) | 130 (70) | 232 (65) |
BMI, body mass index; HbA1c, glycated hemoglobin; MDRD, Modification of Diet in Renal Disease; UACR, urinary albumin-creatinine ratio; IQR, interquartile range; ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker.
Sixty-eight patients were excluded as the subgroup variable was missing.
Pooled. Data are n (%) or mean ± SD unless otherwise indicated.
The proportions of patients by KDIGO risk category in the overall study population are shown in Figure 1. As expected, randomization led to similar distributions of all patients between placebo and treatment groups within each KDIGO category (approximately 47%, 29%, 15%, and 8% in each treatment group for the low, moderately increased, high, and very high KDIGO risk categories, respectively).
Figure 1.
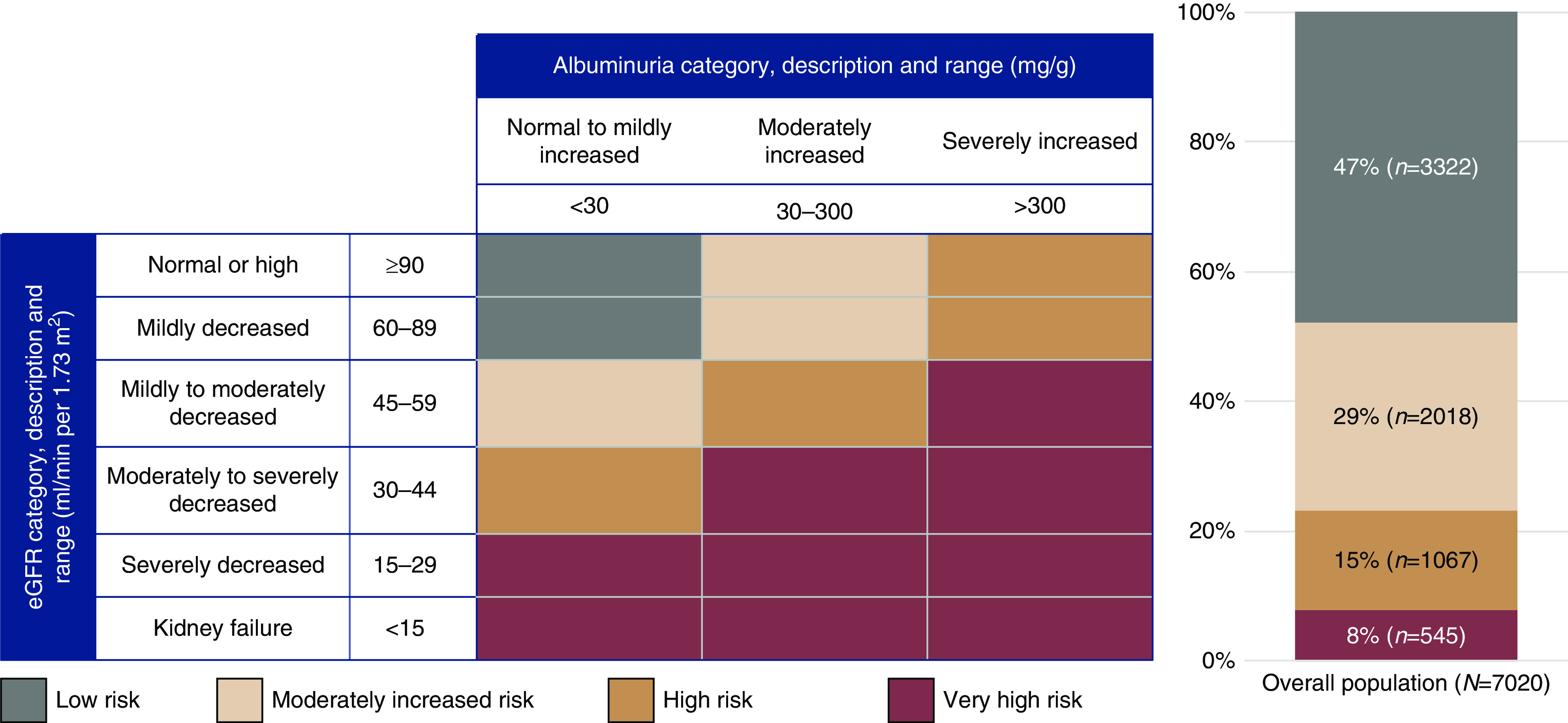
Proportions of patients by Kidney Disease Improving Global Outcomes (KDIGO) risk category in the overall trial population, showing that almost half of patients (47%) were in the low-risk category. The KDIGO “heat map” showing prognosis of CKD by GFR and albuminuria category is shown for reference (3). Of all treated patients, baseline eGFR and urine albumin-creatinine ratio measurements were available for 4635 patients on empagliflozin (98.9%) and 2317 patients on placebo (99.3%). Reprinted from ref. 3, with permission.
Cardiovascular Outcomes Stratified by Kidney Disease Improving Global Outcomes Risk Status at Baseline
The event rates for all outcomes presented were higher with higher KDIGO risk category for both the empagliflozin- and placebo-treated groups (Figure 2). However, for each of the cardiovascular outcomes (three-point MACE; fatal/nonfatal myocardial infarction and fatal/nonfatal stroke cardiovascular death; hospitalization for heart failure; and all-cause mortality), the reductions in risk with empagliflozin versus placebo were consistent for patients with low, moderately increased, high, and very high KDIGO risk category at baseline (the P values for treatment by subgroup interactions across all cardiovascular outcomes ranged from 0.26 to 0.85) (Figure 2).
Figure 2.
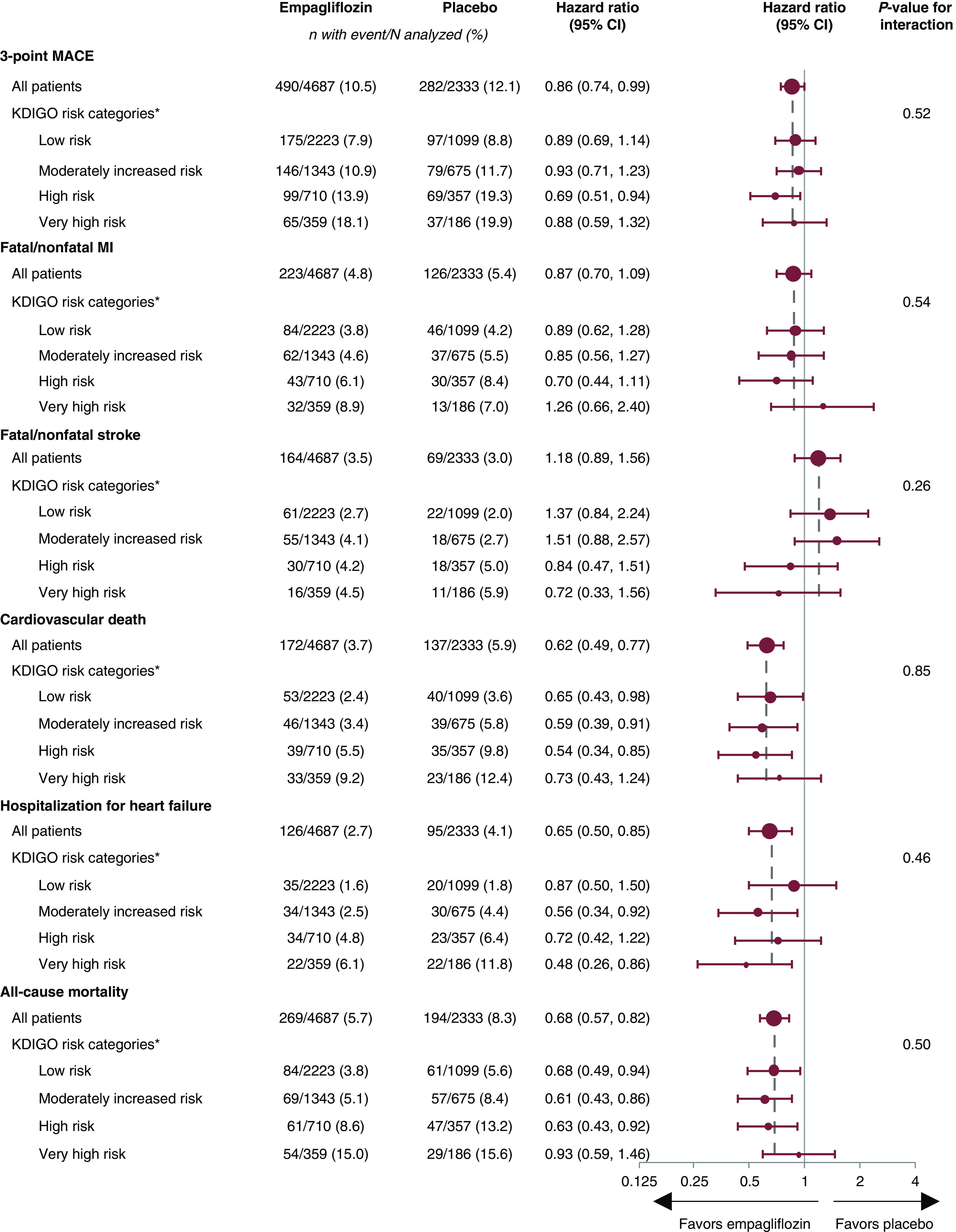
Forest plot showing that the risk reduction of cardiovascular outcomes with empagliflozin versus placebo is consistent across KDIGO risk categories. *Sixty-eight patients were excluded as the subgroup variable was missing. 95% CI, 95% confidence interval; MACE, major adverse cardiovascular event; MI, myocardial infarction.
Kidney Outcomes Stratified by Kidney Disease Improving Global Outcomes Risk Status at Baseline
As observed with cardiovascular outcomes, the incidence of kidney outcome events was higher with higher KDIGO risk categories for both the empagliflozin and placebo groups (Figure 3). However, for each of the three kidney outcomes (incident or worsening nephropathy; progression to UACR>300 mg/g; and the composite of hard kidney end points [doubling of serum creatinine, initiation of KRT, or death from kidney disease]), empagliflozin was associated with a consistent and lower relative risk versus placebo across the KDIGO risk categories (the P values for treatment by subgroup interactions across all kidney outcomes ranged from 0.16 to 0.60) (Figure 3).
Figure 3.
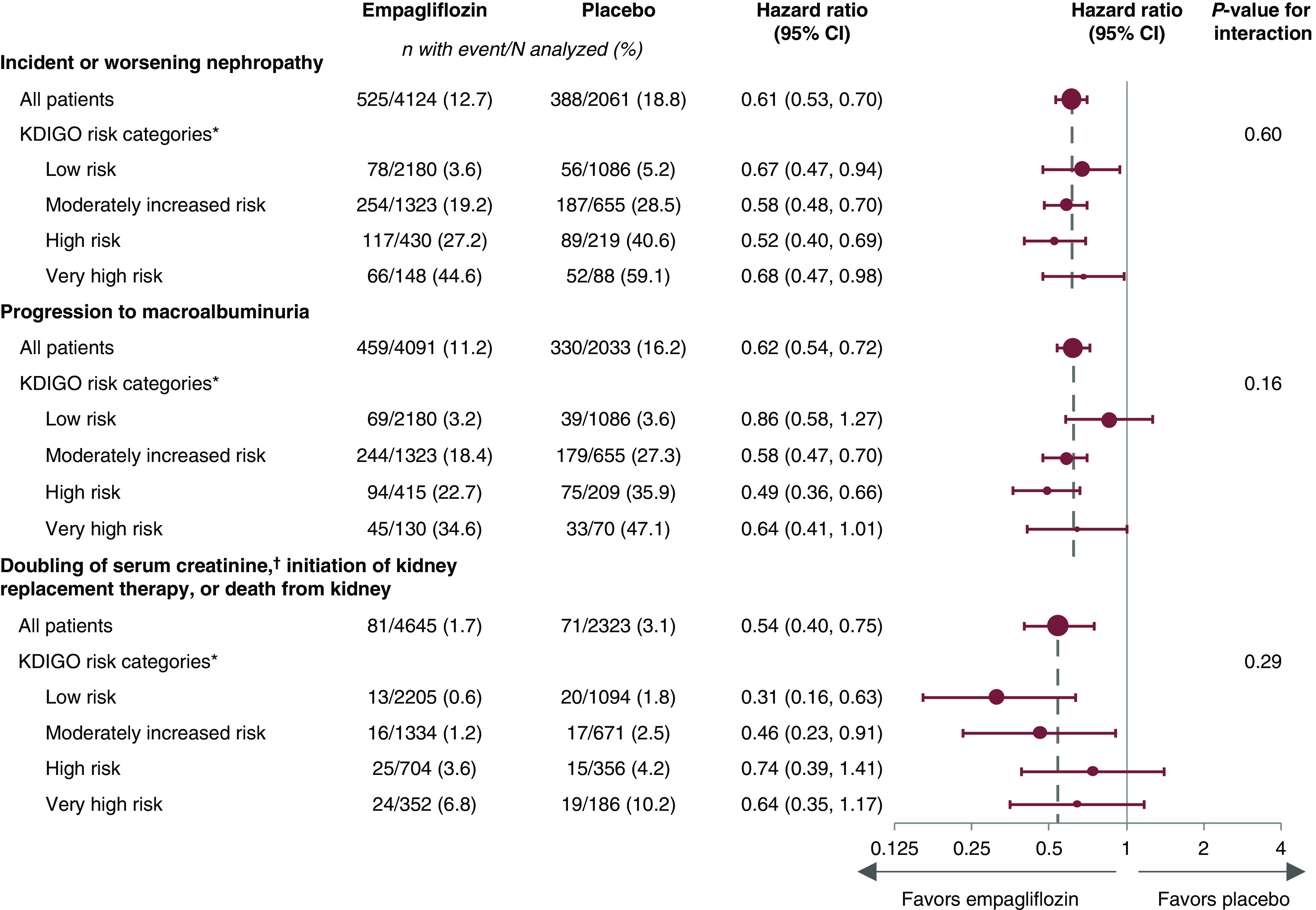
Forest plot showing that the risk reduction of kidney outcomes with empagliflozin versus placebo is consistent across KDIGO risk categories. Cox regression analysis in patients treated with one or more doses of study drug. *Sixty-eight patients were excluded as the subgroup variable was missing. †Accompanied by eGFR≤45 ml/min per 1.73 m2. Macroalbuminuria: urine albumin-creatinine ratio >300 mg/g.
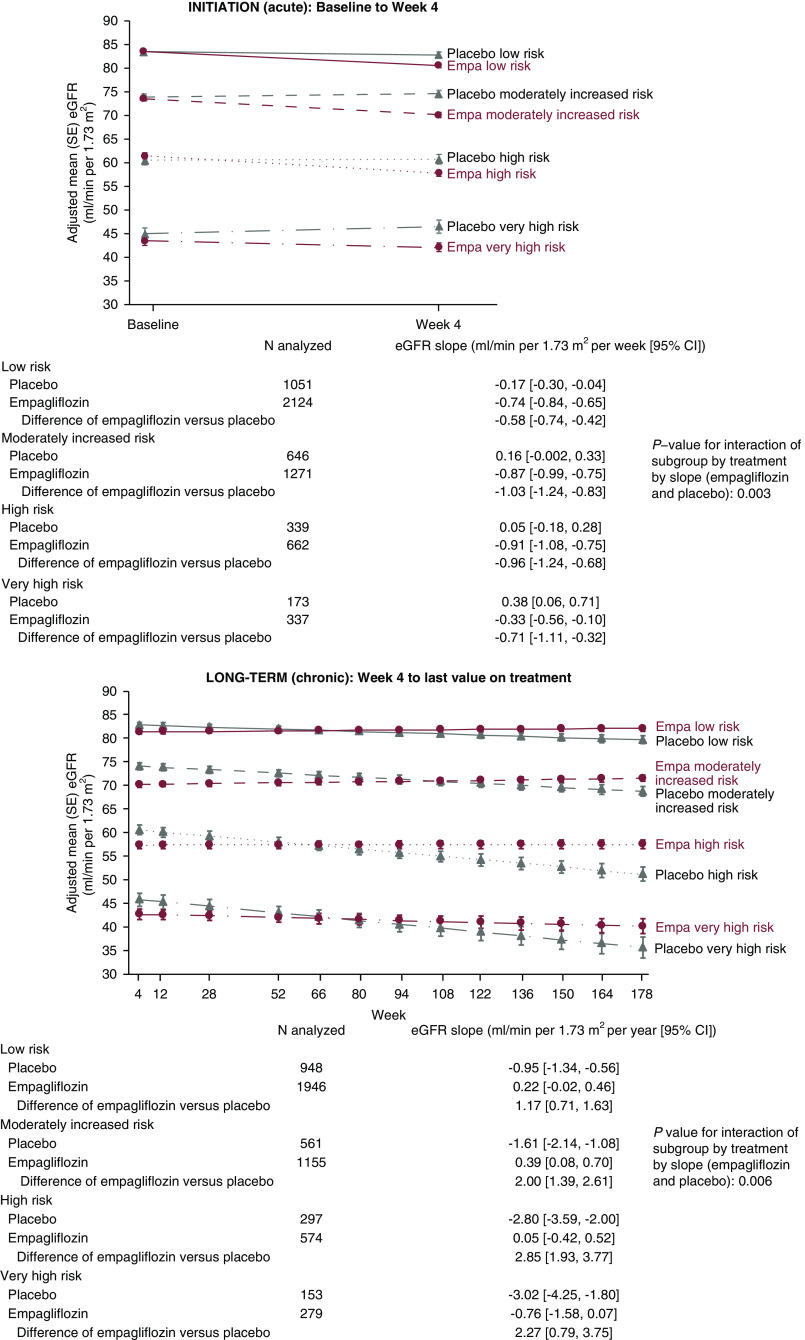
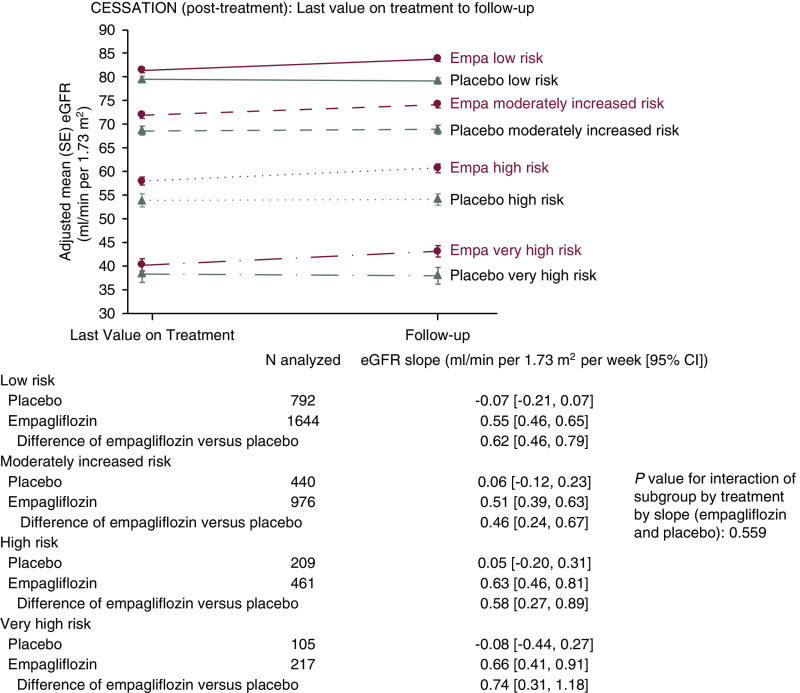
Estimated Glomerular Filtration Rate Slopes
The adjusted mean eGFR slopes for the three prespecified study periods are shown in Figure 4. Over the initial 4 weeks of treatment, the weekly mean adjusted eGFR decrease was numerically greater in the empagliflozin versus placebo groups for all KDIGO risk subgroups. During the chronic maintenance treatment period, however, the annual adjusted change in mean eGFR was stable in all empagliflozin subgroups but declined in the placebo subgroups. Finally, during the post-treatment follow-up, the adjusted mean eGFR in the empagliflozin subgroups increased, whereas little change was observed in eGFR levels in the placebo groups.
Figure 4.
Empagliflozin consistently slowed the long-term annual decline in eGFR across all patient subgroups regardless of KDIGO risk category, as assessed by mean eGFR (Modification of Diet in Renal Disease [MDRD]) slopes on the basis of random intercept/random coefficient models. Adjusted mean eGFR across subgroups of KDIGO risk category. Empa, empagliflozin.
Safety
The effect of empagliflozin versus placebo on adverse events by baseline KDIGO risk category, as incidence rate ratios, is shown in Figure 5. The incidence rate ratios were similar for empagliflozin versus placebo across the adverse events assessed, with interaction P values of >0.05 for all except for the incidence of any adverse event and hyperkalemia. Except for genital infections, all incidence rates were similar or lower with empagliflozin versus placebo, indicated by the 95% confidence intervals of the incidence rate ratios below or including unity. As reported in other trials of empagliflozin and in trials of other SGLT2 inhibitors, the rates of adverse events consistent with genital infection were greater with empagliflozin than with placebo; this was seen across KDIGO risk categories (Figure 5).
Figure 5.
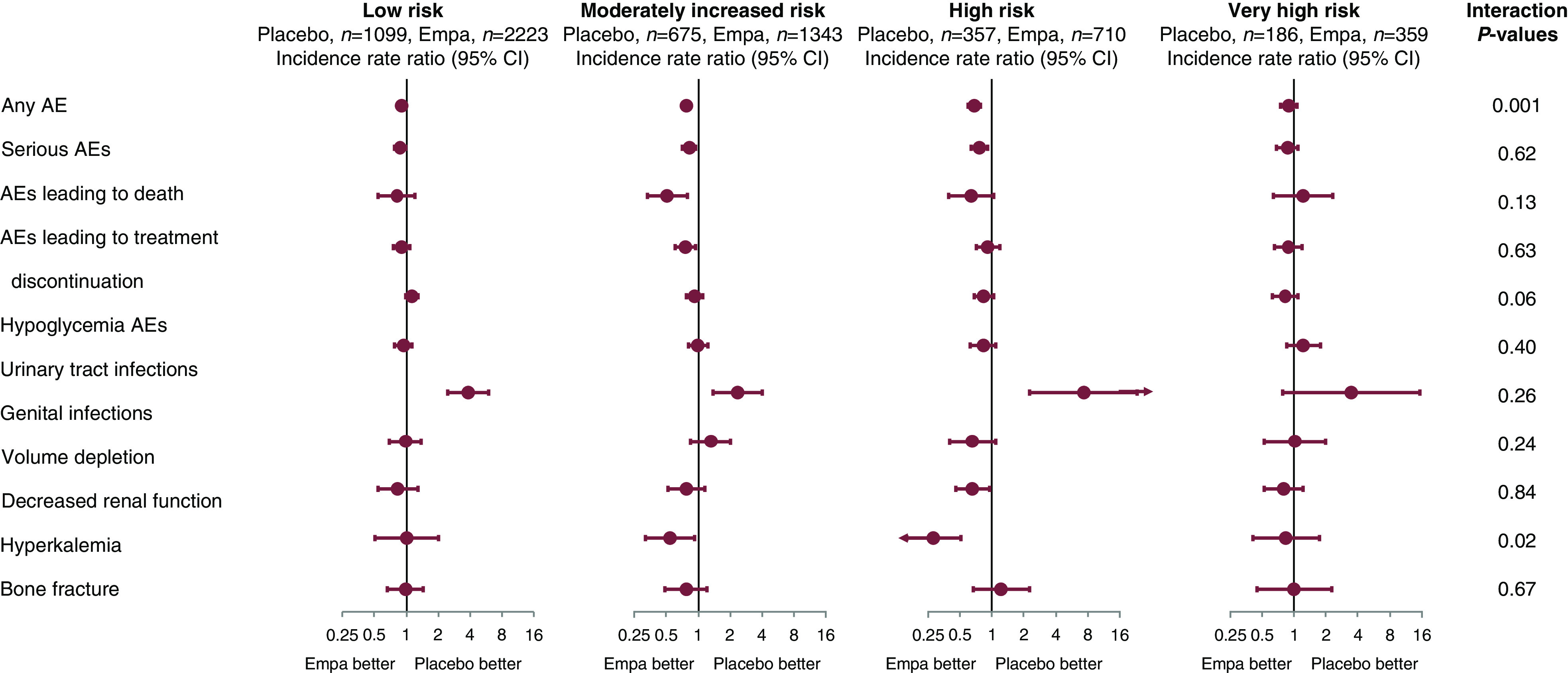
Adverse event (AE) incidence rate ratios were similar or lower with empagliflozin compared with placebo except for genital infections. Data are from patients treated with one or more doses of study drug, including all events that occurred within 7 days after the last receipt of the study drug. Medical Dictionary for Drug Regulatory Activities version used for reporting: 18.0.
Discussion
In this post hoc analysis of EMPA-REG OUTCOME, the overall numbers of cardiovascular and kidney events were higher with the degree of KDIGO risk categories in both empagliflozin and placebo groups, as reported previously in both diabetic and nondiabetic populations (15). Randomization to empagliflozin versus placebo (both given in addition to standard of care) resulted in a reduction in risk of cardiovascular outcomes (three-point MACE, cardiovascular death, hospitalization for heart failure, and all-cause mortality). This reduction in risk associated with active treatment was similar in relative terms, irrespective of baseline KDIGO risk category, and consistent with what was previously observed in the overall trial population and across patients with or without prevalent kidney disease at baseline (10,16).
In addition, empagliflozin versus placebo also lowered the risk of incident or worsening nephropathy, progression to UACR>300 mg/g, and the composite of hard kidney end points (doubling of serum creatinine, initiation of KRT, or death from kidney disease). These findings, which were seen across all baseline KDIGO risk categories, support previously reported kidney effects in the overall trial population, as well as across eGFR and albuminuria subgroups (11). The treatment effect of SGLT2 inhibitors on eGFR slopes has been shown to be a viable surrogate for clinical end points in CKD trials (17,18). The acute and chronic eGFR slopes in the EMPA-REG OUTCOME trial have previously been published (14), with similar analyses reported from the Canagliflozin Cardiovascular Assessment Study (CANVAS) and the Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) study (19,20). Given the acute hemodynamic effect of SGLT2 inhibitors, the treatment effect of empagliflozin on eGFR slope by baseline KDIGO risk categories was investigated. We showed that, over the initial 4 weeks of treatment, the weekly mean adjusted eGFR decrease was numerically greater in the empagliflozin versus placebo groups across all risk subgroups; however, during chronic maintenance treatment, the adjusted mean eGFR stabilized with empagliflozin but declined with placebo. In the post-treatment follow-up phase, the adjusted mean eGFR with empagliflozin returned toward mean baseline eGFR levels, whereas little change was seen with placebo.
The cardiovascular benefits in this study are also in line with more recently reported outcomes from SGLT2 inhibitor trials (CANVAS, Multicenter Trial to Evaluate the Effect of Dapagliflozin on the Incidence of Cardiovascular Events) that have shown reduction in the risk of cardiovascular outcomes in patients with high risk of cardiovascular events (19,21). Kidney benefits of canagliflozin were suggested in CANVAS and confirmed in CREDENCE (20). In CREDENCE, improvement in a specified kidney outcome—ESKD, doubling of serum creatinine, or death from kidney disease—was consistent across eGFR and UACR subgroups with canagliflozin versus placebo (20). Furthermore, the positive effects of SGLT2 inhibition are seen in addition to the benefits of background therapy with angiotensin-converting enzyme inhibitors and angiotensin receptor blockers and so, are particularly important.
In this analysis, the risk reductions seen with empagliflozin versus placebo were similar across the four risk category groups for each of the cardiovascular and kidney outcomes, with no attenuation of effect with higher KDIGO risk categories. The proposed mechanisms by which SGLT2 inhibition may lower the risk of cardiovascular and kidney outcomes are most likely multifactorial and may include improvements in BP control, reduction in total body sodium and water, and weight loss, all of which are associated with improved outcomes in patients with type 2 diabetes. The restoration of tubuloglomerular feedback is likely to be an important contributor to the mechanism of action of the kidney-protective effect of SGLT2 inhibitors, although this is not yet fully understood (22). Additional kidney mechanisms (e.g., tubular protection, reduced hypoxia and inflammation, and long-term effects of natriuresis) may also contribute to these kidney-protective effects (23).
Furthermore, it has been reported that reduction in HbA1c from baseline with empagliflozin was smaller in patients with versus without CKD (24). Similar data have been reported for canagliflozin (25) and dapagliflozin (26). However, the effects of empagliflozin on other cardiovascular parameters, such as systolic BP, were similar regardless of kidney function (24). Attenuation of HbA1c lowering with empagliflozin in patients with CKD is not surprising given its mechanism of action in the kidney (27). A similar finding was reported with canagliflozin (28). Additional research is required to explore the effects of SGLT2 inhibitors on cardiovascular and kidney outcomes in a broader population of patients with CKD, beyond type 2 diabetes. To this end, clinical outcomes trials investigating these agents are underway, including the Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure trial of patients with heart failure and reduced ejection fraction with or without type 2 diabetes. The study included a kidney composite secondary end point, for which no difference between dapagliflozin and placebo was reported (29); this finding was encouraging, although the trial was relatively short (median follow-up 18.2 months). More recently, the Dapagliflozin And Prevention of Adverse outcomes in Chronic Kidney Disease (DAPA-CKD) (NCT03036150) has investigated the effect of dapagliflozin on kidney and cardiovascular events in a broad range of patients with CKD, importantly including those with and without type 2 diabetes (30). In this regard, although DAPA-CKD and CREDENCE both included patients with albuminuria, DAPA-CKD differs from CREDENCE as the latter included only patients with type 2 diabetes (20). DAPA-CKD has been stopped early as the treatment benefits of dapagliflozin occurred earlier than anticipated (31). A large clinical outcomes trial investigating empagliflozin for heart and kidney protection in patients with CKD with or without type 2 diabetes, EMPA-KIDNEY, is underway, with plans to enroll approximately 6000 people, including those with and without albuminuria (NCT03594110) (32). The results of these studies will help to further define the role of new treatment therapies in the management of patients with CKD, including the effects on cardiovascular disease and premature death.
The adverse event profile of empagliflozin versus placebo was similar across KDIGO risk categories, with interaction P values for incidence rate ratios of >0.05 except for the incidence of any adverse event and hyperkalemia. Except for genital infections, rates of adverse events were similar or lower with empagliflozin versus placebo across all KDIGO risk groups. Rates of adverse events consistent with genital infections, as reported in previous trials of empagliflozin and other SGLT2 inhibitors, were greater with empagliflozin versus placebo across risk categories, with the 95% confidence interval for very high risk crossing unity (interaction P value =0.26).
The limitations of our data include the post hoc exploratory nature of the analyses and the relatively low number of patients with advanced CKD: only 8.0% (n=186) and 7.7% (n=359) of patients on placebo and patients on empagliflozin, respectively, were in the very high KDIGO risk category at baseline. Indeed, this analysis may be underpowered to detect differences in treatment effect across subgroups by virtue of the small proportions of patients in high and very high risk categories. In addition, EMPA-REG OUTCOME was not powered or designed to robustly assess kidney outcomes, and these were not adjudicated. However, the consistency of effect size across various definitions of kidney outcomes, and across SGLT2 trials, suggests that this limitation may be inconsequential (33,34).
Early detection of CKD and appropriate interventions are key to slowing disease progression and reducing the risk of adverse cardiovascular and kidney outcomes. For the small proportion of people with CKD and kidney failure who require dialysis and/or kidney transplantation, the economic effect of these interventions on health care budgets can be disproportionately high (3). Hence, identifying individuals at highest risk early in the disease course would enable earlier referral of those patients who will most likely gain benefit from specialist kidney services. This could lead to greater clinical and economic benefits (3). Furthermore, as CKD is a risk factor for cardiovascular disease, earlier intervention will also reduce the risk of cardiovascular and all-cause mortality. Evidence shows that the clinical presentation of CKD among adults with diabetes in the United States has evolved: low eGFR (<60 ml/min per 1.73 m2) in the absence of albuminuria (UACR<30 mg/g) is becoming the most common phenotype, with an associated higher mortality (35). Therefore, any treatment strategies will also need to address the high mortality rates associated with this trend (35).
In conclusion, the overall number of cardiovascular and kidney events was higher numerically with higher KDIGO risk categories in the empagliflozin and placebo groups. However, the observed cardiovascular and kidney benefits of empagliflozin versus placebo were consistent across KDIGO risk categories, indicating that the treatment benefit of empagliflozin was unaffected by baseline CKD status.
Disclosures
J. George reports medical writing support from Boehringer Ingelheim during the conduct of the study. He was an employee of Boehringer Ingelheim at the time of the study. S. Hantel is an employee of Boehringer Ingelheim Pharma GmbH & Co. KG. A. Koitka-Weber reports medical writing support from Boehringer Ingelheim during the conduct of the study. She is an employee of Boehringer Ingelheim International GmbH. A. Levin reports grants, nonfinancial support, and other from AstraZeneca; grants, nonfinancial support, and other from Boehringer Ingelheim International GmbH; and grants and other from Janssen during the conduct of the study. She has also received research support from Amgen, AstraZeneca, the Canadian Institute for Health Research, the Heart and Stroke Foundation of Canada, Janssen, the Kidney Foundation of Canada, Merck, the Michael Smith Health Research Foundation, and Otsuka. V. Perkovic is currently employed by UNSW Sydney, the Royal North Shore Hospital; reports consultancy agreements with AbbVie, Bayer, Boehringer Ingelheim, Chinook, GlaxoSmithKline, Janssen, and Pfizer; Astellas, AstraZeneca, Bayer, Baxter, Bristol-Myers Squibb, Durect, Eli Lilly, Gilead, GlaxoSmithKline, Janssen, Merck, Mitsubishi Tanabe, Mundipharma, Novartis, Novo Nordisk, Pharmalink, Relypsa, Retrophin, Roche, Sanofi, Servier, and Vitae; reports research funding from Pfizer (supplied drug and seed funding for TESTING trial) and GlaxoSmithKline; reports honoraria from AbbVie, Bayer, Boehringer Ingelheim, GlaxoSmithKline, Janssen, Pfizer; Astellas, AstraZeneca, Bayer, Baxter, Bristol-Myers Squibb, Chinook, Durect, Eli Lilly, Gilead, GlaxoSmithKline, Janssen, Merck, Mitsubishi Tanabe, Mundipharma, Novartis, Novo Nordisk, Pharmalink, Relypsa, Retrophin, Roche, Sanofi, Servier, and Vitae; reports serving or has served on steering committees for trials funded by AbbVie, AstraZeneca, Bayer, Boehringer Ingelheim, Chinook, Eli Lilly, Gilead, GlaxoSmithKline, Janssen, Novartis, Novo Nordisk, and Retrophin; and reports serving as a board director for George Clinical, George Institute, Garvan Institute, Mindgardens Network, Childrens Cancer Institute, and Victor Chang Cardiac Research Institute. M. von Eynatten reports medical writing support from Boehringer Ingelheim during the conduct of the study. He was an employee of Boehringer Ingelheim at the time of the study. C. Wanner reports medical writing support from Boehringer Ingelheim during the conduct of the study. He also reports receiving honoraria from Boehringer Ingelheim and Janssen, outside the submitted work. D. Wheeler reports personal fees and nonfinancial support from AstraZeneca; and personal fees from Amgen, Boehringer Ingelheim, Bayer, GlaxoSmithKline, Janssen, MSD, Napp, Mundipharma, Pharmacosmos Reata, and Vifor Fresanius, outside the submitted work. He was a past cochair of KDIGO.
Funding
The EMPA-REG OUTCOME trial was sponsored by the Boehringer Ingelheim and Eli Lilly and Company Diabetes Alliance.
Data Sharing Statement
The sponsor of the EMPA-REG OUTCOME trial (Boehringer Ingelheim) is committed to responsible sharing of clinical study reports, related clinical documents, and patient-level clinical study data. Researchers are invited to submit inquiries via the following website: https://trials.boehringer-ingelheim.com.
Supplementary Material
Acknowledgments
The authors thank the patients who participated in this trial and Ms. Michaela Mattheus from Boehringer Ingelheim for her contribution to the statistical analyses. Medical writing assistance, supported financially by Boehringer Ingelheim, was provided by Mr. Charlie Bellinger and Miss Sally Neath of Elevate Scientific Solutions, Horsham, United Kingdom, during the preparation of this article.
Data were presented at the International Society of Nephrology’s World Congress of Nephrology held April 21–25, 2017 in Mexico City, Mexico.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “SGLT2 Inhibitors across the Spectrum of Severity of CKD,” on pages 1386–1388.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.14901219/-/DCSupplemental.
Supplemental Material. List of EMPA-REG OUTCOME investigators.
References
- 1.American Diabetes Association : Standards of medical care in diabetes—2014. Diabetes Care 37[Suppl 1]: S14–S80, 2014. [DOI] [PubMed] [Google Scholar]
- 2.de Boer IH, Rue TC, Hall YN, Heagerty PJ, Weiss NS, Himmelfarb J: Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA 305: 2532–2539, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kidney Disease Improving Global Outcomes (KDIGO) CKD Work Group : KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl 3: 1–150, 2013 [Google Scholar]
- 4.Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, McCullough PA, Kasiske BL, Kelepouris E, Klag MJ, Parfrey P, Pfeffer M, Raij L, Spinosa DJ, Wilson PW; American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention : Kidney disease as a risk factor for development of cardiovascular disease: A statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 108: 2154–2169, 2003. [DOI] [PubMed] [Google Scholar]
- 5.Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, Jafar TH, Heerspink HJ, Mann JF, Matsushita K, Wen CP: Chronic kidney disease and cardiovascular risk: Epidemiology, mechanisms, and prevention. Lancet 382: 339–352, 2013. [DOI] [PubMed] [Google Scholar]
- 6.Collins AJ, Foley RN, Herzog C, Chavers B, Gilbertson D, Herzog C, Ishani A, Johansen K, Kasiske B, Kutner N, Liu J, St Peter W, Ding S, Guo H, Kats A, Lamb K, Li S, Li S, Roberts T, Skeans M, Snyder J, Solid C, Thompson B, Weinhandl E, Xiong H, Yusuf A, Zaun D, Arko C, Chen SC, Daniels F, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L: US Renal Data System 2012. Annual Data Report. Available at: https://www.ajkd.org/article/S0272-6386(12)01404-7/fulltext. Accessed September 9, 2020 [DOI] [PubMed]
- 7.Kerr M, Bray B, Medcalf J, O’Donoghue DJ, Matthews B: Estimating the financial cost of chronic kidney disease to the NHS in England. Nephrol Dial Transplant 27[Suppl 3]: iii73-iii80, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perkovic V, Agarwal R, Fioretto P, Hemmelgarn BR, Levin A, Thomas MC, Wanner C, Kasiske BL, Wheeler DC, Groop PH; Conference Participants : Management of patients with diabetes and CKD: Conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) Controversies Conference. Kidney Int 90: 1175–1183, 2016. [DOI] [PubMed] [Google Scholar]
- 9.Ingelfinger JR, Rosen CJ: Cardiac and renovascular complications in type 2 diabetes—Is there hope? N Engl J Med 375: 380–382, 2016. [DOI] [PubMed] [Google Scholar]
- 10.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE; EMPA-REG OUTCOME Investigators : Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373: 2117–2128, 2015. [DOI] [PubMed] [Google Scholar]
- 11.Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, Johansen OE, Woerle HJ, Broedl UC, Zinman B; EMPA-REG OUTCOME Investigators : Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 375: 323–334, 2016. [DOI] [PubMed] [Google Scholar]
- 12.Cherney DZI, Zinman B, Inzucchi SE, Koitka-Weber A, Mattheus M, von Eynatten M, Wanner C: Effects of empagliflozin on the urinary albumin-to-creatinine ratio in patients with type 2 diabetes and established cardiovascular disease: An exploratory analysis from the EMPA-REG OUTCOME randomised, placebo-controlled trial. Lancet Diabetes Endocrinol 5: 610–621, 2017. [DOI] [PubMed] [Google Scholar]
- 13.Zinman B, Inzucchi SE, Lachin JM, Wanner C, Ferrari R, Fitchett D, Bluhmki E, Hantel S, Kempthorne-Rawson J, Newman J, Johansen OE, Woerle HJ, Broedl UC: Rationale, design, and baseline characteristics of a randomized, placebo-controlled cardiovascular outcome trial of empagliflozin (EMPA-REG OUTCOMETM). Cardiovasc Diabetol 13: 102, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wanner C, Heerspink HJL, Zinman B, Inzucchi SE, Koitka-Weber A, Mattheus M, Hantel S, Woerle HJ, Broedl UC, von Eynatten M, Groop PH; EMPA-REG OUTCOME Investigators : Empagliflozin and kidney function decline in patients with type 2 diabetes: A slope analysis from the EMPA-REG OUTCOME trial. J Am Soc Nephrol 29: 2755–2769, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, Gansevoort RT, Kasiske BL, Eckardt KU: The definition, classification, and prognosis of chronic kidney disease: A KDIGO Controversies Conference report [published correction appears in Kidney Int 80: 1000, 2011 10.1038/ki.2011.310]. Kidney Int 80: 17–28, 2011. [DOI] [PubMed] [Google Scholar]
- 16.Wanner C, Lachin JM, Inzucchi SE, Fitchett D, Mattheus M, George J, Woerle HJ, Broedl UC, von Eynatten M, Zinman B; EMPA-REG OUTCOME Investigators : Empagliflozin and clinical outcomes in patients with type 2 diabetes mellitus, established cardiovascular disease, and chronic kidney disease. Circulation 137: 119–129, 2018. [DOI] [PubMed] [Google Scholar]
- 17.Inker LA, Heerspink HJL, Tighiouart H, Levey AS, Coresh J, Gansevoort RT, Simon AL, Ying J, Beck GJ, Wanner C, Floege J, Li PK-T, Perkovic V, Vonesh EF, Greene T: GFR slope as a surrogate end point for kidney disease progression in clinical trials: A meta-analysis of treatment effects of randomized controlled trials. J Am Soc Nephrol 30: 1735–1745, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levey AS, Gansevoort RT, Coresh J, Inker LA, Heerspink HL, Grams ME, Greene T, Tighiouart H, Matsushita K, Ballew SH, Sang Y, Vonesh E, Ying J, Manley T, de Zeeuw D, Eckardt K-U, Levin A, Perkovic V, Zhang L, Willis K: Change in albuminuria and GFR as end points for clinical trials in early stages of CKD: A scientific workshop sponsored by the National Kidney Foundation in collaboration with the US Food and Drug Administration and European Medicines Agency. Am J Kidney Dis 75: 84–104, 2020. [DOI] [PubMed] [Google Scholar]
- 19.Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR; CANVAS Program Collaborative Group : Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377: 644–657, 2017. [DOI] [PubMed] [Google Scholar]
- 20.Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, Edwards R, Agarwal R, Bakris G, Bull S, Cannon CP, Capuano G, Chu PL, de Zeeuw D, Greene T, Levin A, Pollock C, Wheeler DC, Yavin Y, Zhang H, Zinman B, Meininger G, Brenner BM, Mahaffey KW; CREDENCE Trial Investigators : Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med 380: 2295–2306, 2019. [DOI] [PubMed] [Google Scholar]
- 21.Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Ruff CT, Gause-Nilsson IAM, Fredriksson M, Johansson PA, Langkilde AM, Sabatine MS; DECLARE–TIMI 58 Investigators : Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380: 347–357, 2019. [DOI] [PubMed] [Google Scholar]
- 22.van Bommel EJM, Muskiet MHA, van Baar MJB, Tonneijck L, Smits MM, Emanuel AL, Bozovic A, Danser AHJ, Geurts F, Hoorn EJ, Touw DJ, Larsen EL, Poulsen HE, Kramer MHH, Nieuwdorp M, Joles JA, van Raalte DH: The renal hemodynamic effects of the SGLT2 inhibitor dapagliflozin are caused by post-glomerular vasodilatation rather than pre-glomerular vasoconstriction in metformin-treated patients with type 2 diabetes in the randomized, double-blind RED trial. Kidney Int 97: 202–212, 2020. [DOI] [PubMed] [Google Scholar]
- 23.Heerspink HJ, Perkins BA, Fitchett DH, Husain M, Cherney DZ: Sodium glucose cotransporter 2 inhibitors in the treatment of diabetes mellitus: Cardiovascular and kidney effects, potential mechanisms, and clinical applications. Circulation 134: 752–772, 2016. [DOI] [PubMed] [Google Scholar]
- 24.Cherney DZI, Cooper ME, Tikkanen I, Pfarr E, Johansen OE, Woerle HJ, Broedl UC, Lund SS: Pooled analysis of phase III trials indicate contrasting influences of renal function on blood pressure, body weight, and HbA1c reductions with empagliflozin. Kidney Int 93: 231–244, 2018. [DOI] [PubMed] [Google Scholar]
- 25.Neuen BL, Ohkuma T, Neal B, Matthews DR, de Zeeuw D, Mahaffey KW, Fulcher G, Desai M, Li Q, Deng H, Rosenthal N, Jardine MJ, Bakris G, Perkovic V: Cardiovascular and renal outcomes with canagliflozin according to baseline kidney function. Circulation 138: 1537–1550, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dekkers CCJ, Wheeler DC, Sjöström CD, Stefansson BV, Cain V, Heerspink HJL: Effects of the sodium-glucose co-transporter 2 inhibitor dapagliflozin in patients with type 2 diabetes and stages 3b-4 chronic kidney disease. Nephrol Dial Transplant 33: 2005–2011, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cooper ME, Inzucchi SE, Zinman B, Hantel S, von Eynatten M, Wanner C, Koitka-Weber A: Glucose control and the effect of empagliflozin on kidney outcomes in type 2 diabetes: An analysis from the EMPA-REG OUTCOME trial. Am J Kidney Dis 74: 713–715, 2019. [DOI] [PubMed] [Google Scholar]
- 28.Heerspink HJ, Desai M, Jardine M, Balis D, Meininger G, Perkovic V: Canagliflozin slows progression of renal function decline independently of glycemic effects. J Am Soc Nephrol 28: 368–375, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, Ponikowski P, Sabatine MS, Anand IS, Bělohlávek J, Böhm M, Chiang CE, Chopra VK, de Boer RA, Desai AS, Diez M, Drozdz J, Dukát A, Ge J, Howlett JG, Katova T, Kitakaze M, Ljungman CEA, Merkely B, Nicolau JC, O’Meara E, Petrie MC, Vinh PN, Schou M, Tereshchenko S, Verma S, Held C, DeMets DL, Docherty KF, Jhund PS, Bengtsson O, Sjöstrand M, Langkilde AM; DAPA-HF Trial Committees and Investigators : Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 381: 1995–2008, 2019. [DOI] [PubMed] [Google Scholar]
- 30.Heerspink HJL, Stefansson BV, Chertow GM, Correa-Rotter R, Greene T, Hou FF, Lindberg M, McMurray J, Rossing P, Toto R, Langkilde AM, Wheeler DC; DAPA-CKD Investigators : Rationale and protocol of the Dapagliflozin And Prevention of Adverse outcomes in Chronic Kidney Disease (DAPA-CKD) randomized controlled trial. Nephrol Dial Transplant 35: 274–282, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.AstraZeneca: Farxiga Phase III DAPA-CKD trial will be stopped early after overwhelming efficacy in patients with chronic kidney disease, 2020. Available at: https://www.astrazeneca.com/media-centre/press-releases/2020/farxiga-phase-iii-dapa-ckd-trial-will-be-stopped-early-after-overwhelming-efficacy-in-patients-with-chronic-kidney-disease.html. Accessed April 25, 2020
- 32.Herrington WG, Preiss D, Haynes R, von Eynatten M, Staplin N, Hauske SJ, George JT, Green JB, Landray MJ, Baigent C, Wanner C: The potential for improving cardio-renal outcomes by sodium-glucose co-transporter-2 inhibition in people with chronic kidney disease: A rationale for the EMPA-KIDNEY study. Clin Kidney J 11: 749–761, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Neuen BL, Young T, Heerspink HJL, Neal B, Perkovic V, Billot L, Mahaffey KW, Charytan DM, Wheeler DC, Arnott C, Bompoint S, Levin A, Jardine MJ: SGLT2 inhibitors for the prevention of kidney failure in patients with type 2 diabetes: A systematic review and meta-analysis. Lancet Diabetes Endocrinol 7: 845–854, 2019. [DOI] [PubMed] [Google Scholar]
- 34.Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Furtado RHM, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Sabatine MS: SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: A systematic review and meta-analysis of cardiovascular outcome trials. Lancet 393: 31–39, 2019. [DOI] [PubMed] [Google Scholar]
- 35.Kramer H, Boucher RE, Leehey D, Fried L, Wei G, Greene T, Rosas SE, Cooper R, Cao G, Beddhu S: Increasing mortality in adults with diabetes and low estimated glomerular filtration rate in the absence of albuminuria. Diabetes Care 41: 775–781, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.