Abstract
Background
Post‐COVID‐19 symptoms and diseases appeared on many survivors from COVID‐19 which are similar to that of the post‐severe acute respiratory syndrome (SARS) fatigue. Hence, the study aims to investigate and characterise the manifestations which appear after eradication of the coronavirus infection and its relation to disease severity.
Method
About 287 survivors from COVID‐19 were included in the study, each received a questionnaire divided into three main parts starting from subjects’ demographic data, data about the COVID‐19 status and other comorbidities of the subject, and finally data about post‐COVID‐19 manifestations. Response surface plots were produced to visualise the link between several factors.
Results
Only 10.8% of all subjects have no manifestation after recovery from the disease while a large percentage of subjects suffered from several symptoms and diseases. The most common symptom reported was fatigue (72.8%), more critical manifestations like stroke, renal failure, myocarditis and pulmonary fibrosis were reported by a few percent of the subjects. There was a relationship between the presence of other comorbidities and severity of the disease. Also, the severity of COVID‐19 was related to the severity of post‐COVID‐19 manifestations.
Conclusion
The post‐COVID‐19 manifestation is largely similar to the post‐SARS syndrome. All subjects recovered from COVID‐19 should undergo long‐term monitoring for evaluation and treatment of symptoms and conditions that might be precipitated with the new coronavirus infection.
Keywords: COVID‐19, fatigue, post‐COVID‐19 manifestations, pulmonary fibrosis
1. INTRODUCTION
Coronavirus disease 2019 (COVID‐19) is a serious respiratory disease that resulted from infection with a new coronavirus (SARS‐CoV‐2). One of the most critical issues related to the COVID‐19 is the high spread rate, millions of people have been infected around the world, and hundreds of thousands of deaths till now had been recorded. Patients suffered from different symptoms like fever, dry cough and fatigue which is mild in about 80% of cases, but the severity of the case may progress to develop a respiratory distress or respiratory failure, and hence, the need for intensive care unit (ICU) will be increased. 1 The severity of the disease is related to age and comorbidities of the infected subjects; the elderly are severely affected with the need for ICU. 2 The severity of symptoms is also related to its duration, for mild cases, symptoms may last for 2 weeks while for the severe cases it ranges from 3 to 6 weeks. 3 Direct contact to confirmed cases is the main way by which the disease transfer among people because the SARS‐CoV‐2 is transmitted through exhaled air and aerosol. 4 Diagnosis of COVID‐19 is done through polymer chain reaction (PCR), computed tomography (CT) scan and blood test. 5 For mild cases, supportive treatment is the only choice including antibiotics, vitamins, trace elements and antipyretics, while those with respiratory distress, the oxygen therapy with or without mechanical ventilation should be introduced and individualised according to each case. 6 A lot of medications were included in clinical trials to act as antiviral but there are no clear results to indicate the confirmed effect for any of the investigated medications. 7 , 8 , 9 In addition to symptomatic therapy, corticosteroids as an anti‐inflammatory could play a vital role in severe cases. 10 Most of the infected patients have recovered from the disease, this recovery could be confirmed by another PCR or by the absence of the symptoms for several days. However, many cases have suffered from different symptoms after recovery from the disease which are different from COVID‐19 symptoms. 11 Post‐recovery manifestations were also studied after the severe acute respiratory syndrome (SARS) attack in 2003 reflecting many symptoms experienced by studied subjects such as fatigue, myalgia, depression and weakness. 12 Some of these manifestations were chronic and lasted for a long time which required long‐term monitoring. 12 In addition to the previously mentioned mild symptoms, a mild hypoactivation of the hypothalamic‐pituitary‐adrenal axis was reported by Leow et al 13 Hence, the current study aims to investigate the post‐COVID‐19 manifestation to demonstrate the different symptoms or signs that appeared on subjects after recovery from the disease, also to link these symptoms with several factors (age, weight, disease severity or other comorbidities).
2. METHOD
Recovered Egyptian subjects from COVID‐19 received a questionnaire aimed to collect data related to their post‐COVID‐19 manifestations. This questionnaire was divided into several parts starting from subjects’ demographic data (age, gender, height, smoking and weight), then, data about the COVID‐19 status and other comorbidities of the subject (Severity of the disease, use of vitamins and presence of other diseases) finally data about post‐COVID‐19 manifestations (Symptoms, extra investigations of the symptoms, need for using medications for post‐COVID‐19 symptoms and recovery of post‐COVID‐19 symptoms).
Each item's responses were analysed first to indicate the rate of its occurrence, then, to be linked with the occurrence of post‐COVID‐19 manifestations.
Response surface plots were produced using design expert software version 11 (Stat‐Ease Inc, Minneapolis, MN, USA). Factors expressed on response surface plot have been coded as following; Age (1 = 20‐30 years, 2 = 31‐40 years and 3 ≥ 40 years), Comorbidity (1 = no comorbidity and 2 = presences of other diseases), severity of post‐COVID‐19 manifestations (1 = mild and 2 = severe) and Severity of COVID‐19 (Figure 1 (1 = mild, 2 = moderate and 3 = severe) and Figure 2 (0.1 = mild, 0.2 = moderate, 0.3 = severe)).
FIGURE 1.
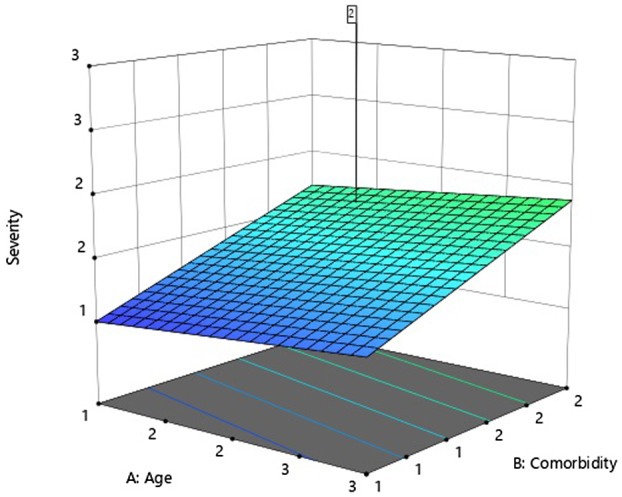
Response surface plot showing the relationship between age, comorbidities and severity of COVID‐19
FIGURE 2.
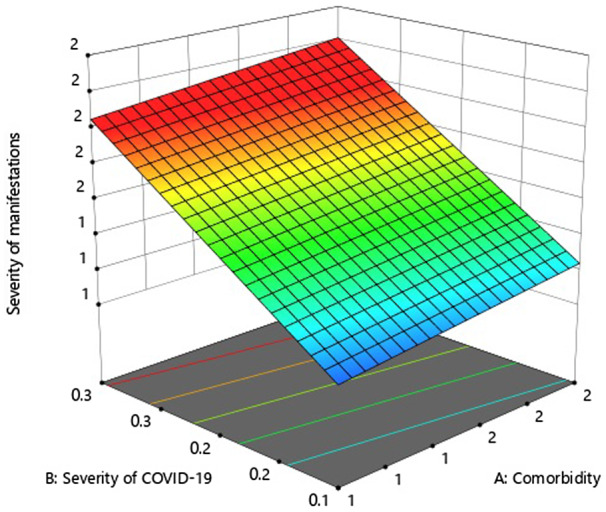
Response surface plot showing the relation between comorbidities, the severity of COVID‐19 and severity of manifestations post‐COVID‐19
3. RESULTS
Demographic data and COVID‐19 course of involved subjects are expressed in Table 1. Relation between several factors and severity of the disease is shown in Figures 1 and 2. Post‐COVID‐19 manifestations are expressed in Table 2 and Figure 3.
TABLE 1.
Demographic data of COVID‐19 subjects
| Element | Percent |
|---|---|
| Age | |
| 20‐30 y | 33.8% |
| 31‐40 y | 49.1% |
| >40 y | 17.1% |
| Gender | |
| Male | 35.9% |
| Female | 64.1% |
| Body mass index | |
| Normal (18.5‐24.9) | 26.5% |
| Overweight (25‐29.9) | 38% |
| Obese (>30) | 35.5% |
| Smoking | |
| Smoker | 9.8% |
| Non‐smoker | 90.2% |
| Severity of disease | |
| Mild | 80.2% |
| Moderate (Oxygen therapy) | 14.9% |
| Severe (ICU) | 4.9% |
| Pregnancy | |
| Pregnant | 1.4% |
| Not pregnant | 98.6% |
| Other diseases | |
| No other conditions | 70.7% |
| Hypertension | 7.7% |
| Diabetes | 5.2% |
| Rheumatoid arthritis | 1.4% |
| Dyslipidaemia | 1.4% |
| Hypothyroidism | 1% |
| Asthma | 1% |
| Peptic ulcer | 0.7% |
| Arrhythmia | 0.7% |
| Other conditions | 10.2% |
| Receiving vitamins during disease | |
| Yes | 90.6% |
| No | 9.4% |
TABLE 2.
Characterisation of post‐COVID‐19 manifestations
| Item | Percent |
|---|---|
| Manifestations | |
| Fatigue | 72.8% |
| Anxiety | 38% |
| Joints pain | 31.4% |
| Continuous headache | 28.9% |
| Chest pain | 28.9% |
| Dementia | 28.6% |
| Depression | 28.6% |
| Dyspnoea | 28.2% |
| Blurred vision | 17.1% |
| Tinnitus | 16.7% |
| Intermittent fever | 11.1% |
| Obsessive‐compulsive disorder | 4.9% |
| Pulmonary fibrosis | 4.9% |
| Diabetes mellitus | 4.2% |
| Migraine | 2.8% |
| Stroke | 2.8% |
| Renal failure | 1.4% |
| Myocarditis | 1.4% |
| Arrhythmia | 0.3% |
| Extra investigations for post‐COVID‐19 manifestations | |
| Yes | 13.2% |
| No | 86.8% |
| Received medications for post‐COVID‐19 manifestations | |
| Yes | 85% |
| No | 15% |
| Condition improved on treatment | |
| Yes | 67.2 |
| No | 32.8% |
FIGURE 3.
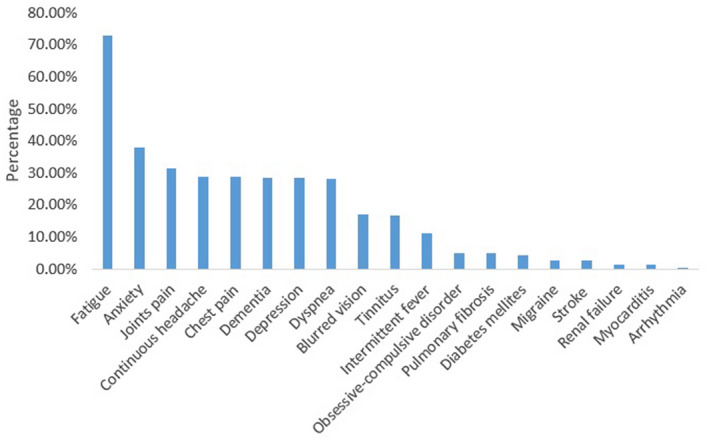
Percentage of different post‐COVID‐19 manifestations that appeared on recovered COVID‐19 subjects
The study involved 287 recovered COVID‐19 subjects, 103 of them were males and 184 females. Age of involved subjects expressed as Mean ± SD was 32.3 ± 8.5 and ages ranged from 20 to 60 years old. Mean ± SD weight, height and body mass index (BMI) were 77 ± 16.4, 162.9 ± 15.3 and 28.5 ± 5.2, respectively. Percent of smokers among male subjects was 27.2%, while all females were non‐smokers. Regarding other diseases, 70.7% of all subjects have no known history of other illnesses, while 7.7% have hypertension and 5.2% were diabetic. The severity of COVID‐19 symptoms was divided into three categories, first is the mild cases that were isolated at home and they expressed 80.2%, the second category was the moderate cases that received oxygen therapy and they represent 14.9%, the third category was the severe cases that required ICU admission and this category represent a small percent (4.9%). Analysis of post‐COVID manifestations revealed that only 10.8% of all subjects have no manifestation after recovery from the disease while a large percentage of subjects suffered from several symptoms. Most subjects suffered from fatigue (72.8%), anxiety (38%), joints pain (31.4%), continuous headache (28.9%), chest pain (28.9%), dementia (28.6%), depression (28.6%) and dyspnoea (28.2%). A few percent of recovered subjects have newly diagnosed with diabetes (2.4%) (Table 2). A large percent of the subjects was recovered from post‐COVID‐19 manifestations (67.6%), while 32.4% of subjects have persistent manifestations. Regarding nutritional support, 90.6% of all subjects were receiving multivitamins (natural or pharmaceutical products) during the disease.
Most (83.3%) of the moderate‐severe cases were related to those with comorbidities (diabetic, asthmatic and hypertensive subjects) and pregnant subjects.
The severity of COVID‐19 was related to age and comorbidities as shown in Figure 1. Also, the severity of post‐COVID‐19 manifestations was related to the severity of COVID‐19 (Figure 2).
4. DISCUSSION
Post‐COVID‐19 manifestations were recorded for about 90% of the recovered subjects, with a wide range of symptoms and conditions that varied from a low‐critical symptom like a headache to more critical conditions such as stroke, renal failure and pulmonary fibrosis. Post‐viral infection syndrome was previously reported after SARS. 12 , 13 Follow‐up for 4 years showed that chronic fatigue and psychiatric conditions continued to be clinically significant among subjects survived from SARS infection. 14 Hence, mental health morbidities management should be optimised through a multidisciplinary approach combined with long‐term rehabilitation. Regarding COVID‐19 survivors, each subject reported one or more manifestations, those manifestations persisted with all subjects for more than 20 days from the last negative PCR. The severity of COVID‐19 was classified into three categories as follow; mild cases that had controllable symptoms and have been treated at home without the need for oxygen therapy, moderate cases which suffered from difficult breathing and needed oxygen therapy at home and severe cases that had been hospitalised and needed ICU. The relation between age, comorbidities and severity of COVID‐19 showed a strong link between the presence of other comorbidities and the severity of COVID‐19. 15 Also increasing age was related to increased severity of the disease course. 16 Most of the reported manifestations were mild reversible symptoms that could be relieved without medical interventions such as fatigue and headache which could be related to COVID‐19 symptoms. Other mild symptoms like joint and muscle pain were also reported by many subjects and it could be classified as mild manifestations. It was noted that many manifestations are related to the central nervous system such as continuous headache, migraine, depression, anxiety and obsessive‐compulsive disorder. Few percent of subjects have suffered from critical complications such as stroke, myocarditis, renal failure and pulmonary fibrosis which could be reversible and required extra investigation. Regarding obesity as a factor affecting disease severity or post disease symptoms, it was shown that the majority of subjects were overweight or obese but there is no significant effect on the severity grade or type of post‐COVID‐19 symptoms. The manifestation of post‐COVID‐19 that have been recorded during this study could be classified as mild or critical, the critical manifestations are those affecting organ functions such as pulmonary fibrosis, renal failure, myocarditis, arrhythmia and stroke. There was a relationship between the severity of post‐COVID‐19 manifestations and the severity of the disease, the severe cases expressed high severity manifestations compared with those suffering from mild condition. 11 Hence, the severity of manifestations is also related to the age and comorbidities of the involved subjects. All cases with severe manifestations have confirmed their diagnosis through laboratory investigations and imaging procedures such as CT scan for diagnosis of pulmonary fibrosis. The most reported manifestation for this study was fatigue which also reported by Tansey et al after SARS in 2003. 17 Fatigue persisted with recovered subjects from SARS for several months, as subjects were monitored every 3 months, more than 50% of subjects were suffering from fatigue each time. 17 Another study followed up SARS subjects for 4 years to evaluate the percent of chronic fatigue in those subjects and they found that about 40.3% suffered from chronic fatigue. 14 In addition to fatigue, neuropsychiatric symptoms were documented for a large percent of COVID‐19 subjects, also this finding could be consistent with Lara et al finding after monitoring neuropsychiatric symptoms of Alzheimer's and mild cognitive impaired subjects whose were infected with the new coronavirus. 18 Lara et al fund that symptoms of those subjects were worsened significantly during 5 weeks from the infection. 18 Obsessive‐compulsive disorder (OCD) was diagnosed for a few percent of subjects and it was mainly reported by female subjects. Effect of COVID‐19 on symptoms exacerbations for subjects suffering from OCD was evaluated by Chakraborty et al and findings of the study indicated that a few percent (6%) of COVID‐19 subjects had a worsened symptoms. 19
A previously reported case (80 years female subject) by Schwensen et al that had recovered from COVID‐19 and she had no history of pulmonary illness, however, she was suffering from bilateral lung fibrosis as a result of COVID‐19 which leads to her death. 20 Regarding cardiac involvement, it was reported that some COVID‐19 subjects suffered from myocarditis as a complication of COVID‐19 which was consistent with the finding of this study. 21 Some of the mild manifestations might be related to the administration of hydroxychloroquine like the blurred vision which was reported from subjects receiving the drug as a part of the treatment course especially the hydroxychloroquine was a part of the treatment protocol for COVID‐19 subjects. 22
For subjects recovered from COVID‐19, negative PCR is not the end of patient monitoring, continuous and long‐term monitoring of the subjects is recommended for evaluation of post‐COVID‐19 manifestation, and early intervention with the critical signs. Also, the need for continuous counselling with the subjects is very important not only for maintaining good adherence to the medications, but also for detection of early warning signs of developing serious manifestations. Adherence to medications has a beneficial effect on patient's outcomes. 23
5. CONCLUSION
Most of the subjects recovered from COVID‐19 experienced several manifestations after the last negative PCR which could be mild symptoms such as fatigue, headache or more critical manifestations like pulmonary fibrosis, stroke and myocarditis. The most reported symptoms were fatigue, anxiety, joint pain and headache. The severity of post‐COVID‐19 manifestations was correlated to the severity of the infection which also was related to the presence of comorbidities. The post‐COVID‐19 manifestation is largely similar to the post‐SARS syndrome. All subjects recovered from COVID‐19 should undergo long‐term monitoring for evaluation and treatment of symptoms and conditions that might be precipitated after recovery from the new coronavirus infection.
DISCLOSURES
None declared.
Kamal M, Abo Omirah M, Hussein A, Saeed H. Assessment and characterisation of post‐COVID‐19 manifestations. Int J Clin Pract. 2021;75:e13746. 10.1111/ijcp.13746
REFERENCES
- 1. Wu Z, McGoogan JMJJ. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. 2020. [DOI] [PubMed]
- 2. COVID, C . Severe outcomes among patients with coronavirus disease 2019 (COVID‐19)—United States. February 12–March 16, 2020. [DOI] [PMC free article] [PubMed]
- 3. Wang D, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;23(11):1061‐1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mez J, Daneshvar DH, Kiernan PT, et al. Clinicopathological evaluation of chronic traumatic encephalopathy in players of American football. JAMA. 2017;318(4):360‐370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Udugama B, Kadhiresan P, Kozlowski HN, et al. Diagnosing COVID‐19: the disease and tools for detection. ACS Nano. 2020;14(4):3822‐3835. [DOI] [PubMed] [Google Scholar]
- 6. Li T, Lu H, Zhang W. Clinical observation and management of COVID‐19 patients. Emerg Microbes Infect. 2020;9(1):687‐690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gao J, Tian Z, Yang XJBT. Breakthrough Chloroquine phosphate has shown apparent efficacy in treatment of COVID‐19 associated pneumonia in clinical studies. Biosci Trends. 2020;14(1):72‐73. [DOI] [PubMed] [Google Scholar]
- 8. Elfiky AA. Anti‐HCV, nucleotide inhibitors, repurposing against COVID‐19. Life Sci. 2020;248:117477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen C, Huang J, Cheng Z, et al. Favipiravir versus arbidol for COVID‐19: a randomized clinical trial. MedRxiv. 2020. 10.1101/2020.03.17.20037432 [DOI] [Google Scholar]
- 10. Fadel R, Morrison A, Vahia A, et al. Short course corticosteroids in hospitalized patients with COVID‐19. Clin Infect Dis. 2020. 10.1093/cid/ciaa601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Islam MF, Cotler J, Jason LA. Post‐viral fatigue and COVID‐19: lessons from past epidemics. Fatigue: Biomedicine, Health & Behavior. 2020:8(2):61‐69. [Google Scholar]
- 12. Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post‐SARS syndrome; a case‐controlled study. BMC Neurology. 2011;11(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Leow MKS, Kwek DS, Ng AW, et al. Hypocortisolism in survivors of severe acute respiratory syndrome (SARS). Clinical Endocrinology. 63(2):197‐202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lam MH, Wing YK, Yu MW, et al. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long‐term follow‐up. Archives of Internal Medicine. 2009;169(22):2142‐2147. [DOI] [PubMed] [Google Scholar]
- 15. Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID‐19) infection: a systematic review and meta‐analysis. International Journal of Infectious Diseases. 2020;94:91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Li X, Xu S, Yu M, et al. Risk factors for severity and mortality in adult COVID‐19 inpatients in Wuhan. Journal of Allergy and Clinical Immunology. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tansey CM, Louie M, Loeb M, et al. One‐year outcomes and health care utilization in survivors of severe acute respiratory syndrome. Archives of Internal Medicine. 2007;167(12):1312‐1320. [DOI] [PubMed] [Google Scholar]
- 18. Lara BB, Carnes A, Dakterzada F, et al. Neuropsychiatric symptoms and quality of life in Spanish Alzheimer’s disease patients during COVID‐19 lockdown. European Journal of Neurology. 2020;27:1744–1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chakraborty A, Karmakar S Impact of COVID‐19 on obsessive compulsive disorder (OCD). Iranian Journal of Psychiatry. 2020;15(3):256‐259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schwensen HF, Borreschmidt LK, Storgaard M, et al. Fatal pulmonary fibrosis: a post‐COVID‐19 autopsy case. Journal of Clinical Pathology. 2020. 10.1136/jclinpath-2020-206879 [DOI] [PubMed] [Google Scholar]
- 21. Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID‐19). JAMA Cardiology. 2020;5:819–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sarma P, Kaur H, Kumar H, et al. Virological and clinical cure in COVID‐19 patients treated with hydroxychloroquine: a systematic review and meta‐analysis. Journal of Medical Virology. 2020;92:776–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Saeed H, Abdelrahim ME, Rabea H, et al. Impact of advanced patient counseling using a training device and smartphone application on asthma control. Respiratory Care. 2020;65(3):326‐332. [DOI] [PubMed] [Google Scholar]


