Abstract
Background
At the end of 2019, a novel coronavirus (COVID‐19) was identified in China. The high potential of human‐to‐human transmission led to subsequent COVID‐19 global pandemic. Public health strategies including reduced social contact and lockdown have been adopted in many countries.
Nonetheless, social distancing and isolation could also represent risk factors for mental disorders, resulting in loneliness, reduced social support and under‐detection of mental health needs.
Along with this, social distancing determines a relevant obstacle for direct access to psychiatric care services. The pandemic generates the urgent need for integrating technology into innovative models of mental healthcare.
Aims
In this paper, we discuss the potential role of telepsychiatry (TP) and other cutting‐edge technologies in the management of mental health assistance. We narratively review the literature to examine the advantages and risks related to the extensive application of these new therapeutic settings, along with the possible limitations and ethical concerns.
Results
Telemental health services may be particularly feasible and appropriate for the support of patients, family members and healthcare providers during this COVID‐19 pandemic. The integration of TP with other technological innovations (eg, mobile apps, virtual reality, big data and artificial intelligence (AI)) opens up interesting future perspectives for the improvement of mental health assistance.
Conclusion
Telepsychiatry is a promising and growing way to deliver mental health services but is still underused. The COVID‐19 pandemic may serve as an opportunity to introduce and promote, among numerous mental health professionals, the knowledge of the possibilities offered by the digital era.
What's known
A PubMed search for peer‐reviewed studies was performed with date limits ranging from 1 January 1990 to 15 March 2020.
The terms used included: telepsychiatry, telemental health, telehealth, telemedicine, videoconferencing, internet‐based, online and digital.
The articles were selected for inclusion by the authors on the basis of relevance.
What's new
Telemental health services may be particularly feasible and appropriate for the support of patients, family members and healthcare providers, particularly during the COVID‐19 pandemic.
There is an urgent need for a feasible integration of technology with innovative models of mental healthcare. The newest frontiers include mobile apps, virtual reality, big data and artificial intelligence.
Mental health professionals have a strategic role to help ensure that these technologies respect the therapeutic relationship and remain rigorous in their scientific foundation.
1. INTRODUCTION
Initially identified in December 2019 in China, the 2019 Coronavirus disease (COVID‐19) is now affecting more than 200 countries and territories around the world. Given the current unavailability of an effective cure or vaccine for COVID‐19, a public health strategy of reduced social contact and distancing has been adopted worldwide to slow the spread of the virus. This strategy may on the one hand achieve its goals, but on the other hand, it may undermine normal social support systems, yielding to loneliness and reduced support from family and friends. These conditions may be risk factors for the development of anxiety, stress and depressive symptoms 1 , 2 , 3 , 4 in the general population, they may worsen previously diagnosed diseases, 5 as well as they may favour the onset of new problematic behaviours (eg, internet misuse 6 , 7 ). During the pandemic, Ni et al 2 found that almost one‐fifth of respondents to their online survey, targeting Chinese adults, reported probable anxiety and depression. Another survey, carried out in the same time among Italian people, registered high/very high levels of depression, anxiety and stress in a large part of the sample. 1 Because of the contagiousness of COVID‐19, 8 physical access to the mental healthcare system could increase the risk of infection. Fear of contracting the disease in a healthcare setting, transportation restrictions and isolation at home have become important barriers to treatment for many people. 9 Zhou et al 9 reported that the decrease of hospital visits led to a reduction of routine psychiatric care for many patients with mental disorders in China, during the COVID‐19 outbreak. Consequently, 18.1% of their sample self‐reduced drug dosages and 17.2% stopped taking their psychiatric drugs because they could not have a prescription from their doctor. They also found out that 24.5% of new patients with anxiety disorders, insomnia, psychosis or depression could not receive timely diagnoses and treatment during this period. These data globally underline the urgency of quickly adapting to current situation, in order to guarantee continuity of care for at‐risk populations, such as that of psychiatric patients. In this respect, the global concern about the psychosocial consequences of COVID‐19 pandemic has led governments to call for suggestions to deal with these effects. The use of digital health technology has been proposed as an important strategy to reinforce heath systems. 10
According to the World Health Organization, telemedicine is “the delivery of healthcare services, where distance is a critical factor, by all healthcare professionals, using information and communication technologies”. 11 When applied in the field of psychiatry, these methods are known as telepsychiatry (TP).
Telemental health services can be particularly useful and appropriate for the support of both patients and healthcare workers during this pandemic, allowing providing assistance and care to those who need it by reducing the risk of infection. Illustrative of that is the case of a Californian psychiatric clinic in which all patients with existing appointments received care via TP, allowing to provide uninterrupted care while minimising potential COVID‐19 exposure to patients and clinicians. 12
Technology‐based tools offer telemedicine visits for patients, as well as support for institutions, by facilitating the provision of information and data sharing, while creating virtual spaces for meetings and clinical briefings. 13
It is interesting to underline that psychiatric care is relatively unique; with only rare exceptions, psychiatrists are not expected to physically touch their patients to provide the best services. Verbal and visual assessments, which can easily occur via telemedicine, are all that is needed to engage with patients appropriately to obtain full diagnostic accuracy and provide most types of treatments. For these reasons, a 2‐way tele‐videoconferencing for clinical assessments and treatment delivery is a reasonable method to provide psychiatric care. 14
The aim of this narrative review is to evaluate TP utility and feasibility, updating and summarising the most important findings about its use in the modern psychiatric practice, in order to inform the potential use of TP during the pandemic.
2. METHODS
A PubMed search for peer‐reviewed original research studies was performed with date limits ranging from 1 January 1990 to 15 March 2020, in order to capture studies carried out in mobile phone and internet era. The terms used included: telepsychiatry, telemental health, telehealth, telemedicine, videoconferencing, internet‐based, online and digital. Study types considered for inclusion were original research papers, systematic reviews and meta‐analyses on the given topic. The decision to include review has been made to rapidly update and summarise the knowledge about TP given the unfolding pandemic. Only English‐written papers were considered for inclusion. Resources were filtered using abstracts (where available), before evaluating full texts, and the included studies were selected based on their relevance to the aim of this review. The reference section of each examined article was also reviewed to identify other potential studies.
3. RESULTS
A total of 426 records were found from bibliographic search. Of these, 214 record were excluded after abstract evaluation (n = 9 because were not English written, n = 12 because were other study types and n = 193 because were not relevant to the aim of this review). Of the 212 records assessed for eligibility, 45 articles were selected for inclusion in the narrative synthesis (Figure 1).
FIGURE 1.
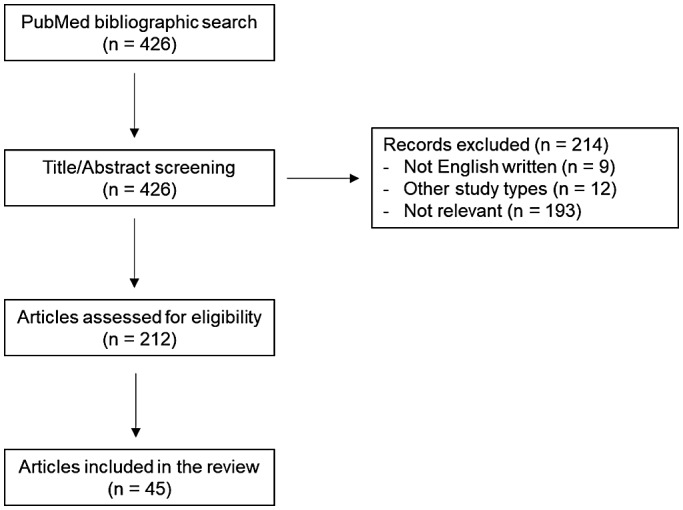
Flowchart
Five core themes were identified: advantages of TP, concerns about TP, privacy and legal issues, TP in the treatment of psychiatric disorders and psychotherapy via TP. A perspective section about new technologies in mental healthcare was also added, to inform about newest possibilities other than TP offered by the digital era.
3.1. Advantages of telepsychiatry
For patients, TP improves access to care, reduces appointments’ waiting time and decreases travel time and costs. 15 Some patients report feeling more comfortable, and can be more open and honest, when discussing difficult subjects from their devices, because the virtual space of the session instills a feeling of “protection”. Another important advantage of TP in terms of rapport building is the possibility for patients (especially immigrants, refugees and asylum seekers) to receive psychiatric assistance in their native language without the assistance of an interpreter. 16
In their review, Cowan et al 17 reported several advantages to TP, both from the patient's and the clinician's points of view. By working in different settings (schools, prisons, homes and hospitals) and with different populations (prisoners, students, employees, hospital patients and outpatients), clinicians can have flexibility in scheduling appointments and an increased diversity of practice. They may also feel safer when evaluating patients without any risk of physical aggression. Furthermore, the use of TP allows clinicians to remotely consult other colleagues.
Given a reasonable initial apprehension, discomfort and fear, patients generally report an increase in comfort and satisfaction after having used TP a few times. Comparably to patients, after a few trials, clinicians reveal an improved attitude towards TP as well, suggesting that increased exposure for clinicians may be important to alleviate their concerns about rapport. 16
With regard to efficacy, in a recent narrative review by Hilty et al, 18 TP was found to be effective in terms of patient acceptance, ability to increase access to care and provision of good educational outcomes. Moreover, TP was found to be valid and reliable when compared with in‐person services. Telemental health effectiveness compared with face‐to‐face treatment has been proven in various randomised controlled trials (RCTs). This has been proved to be valid also for psychotherapy. 19 , 20 , 21
3.2. Concerns about telepsychiatry
Both users and, particularly, non‐users of telemedicine reported disliking the loss of personal contact with patients. The decreased ability to detect non‐verbal cues during videoconferencing may limit the building of the relationship, since clinicians report some difficulties in picking up nuances and emotions. 22 Some clinicians may feel and look clumsy and uncomfortable or may have a hard time engaging with patients; eye contact can feel artificial across the screen as well. Clinicians have also expressed discomfort in being unable to take physical actions to reassure or assist their patients. 18 When randomly assigned to evaluate in‐person versus videoconference therapy sessions, psychiatrists reported lower therapeutic alliance in telemental health settings; they also persisted on being hesitant to use videoconference for their therapy sessions because they believed that the therapeutic alliance was at risk. 22 Concerns have been voiced about certain patients possibly being non‐suitable for TP, including individuals with psychotic symptoms, acute crisis or at risk of self‐harm. 17 Patients with auditive, visual or cognitive impairments appear not to be eligible for telemental health services. 17 Furthermore, it has been proposed to carefully consider the role of substance abuse and past episodes of self‐injurious or violent behaviour before selecting a patient for a TP intervention. 23 Technical difficulties, such as transmission unable to start, spontaneous disconnections, poor audio/visual quality and audio/visual delay, may seriously affect the TP session. Sound quality may affect more substantially the interaction; although audio quality may be prioritised, poor visual transmission, resulting in decreased ability to detect non‐verbal cues, remains a concern. 24
Clinicians are often reluctant to try TP because it is not something they are accustomed to. 25 New approaches to professional techniques require deliberate conscious efforts. There are deep‐rooted cultural traditions in medicine that impede the diffusion of TP. Physical proximity has an important part in clinical practice, with an enormous cultural significance. Over the course of 2000 years, a doctor's physical presence has been regarded as necessary for clinical practice and patients’ healing.
Telemental health is not equally distributed among professional categories other than psychiatrists. For example, more than two‐thirds of psychologists in the United States have never used videoconferencing to deliver their therapeutic services in 2018. 26
Finally, despite easier and cheaper access to the internet, the so called “digital divide” remains often reported in the literature and can impede TP diffusion. 27 These reports still reveal that the elderly people, racial/ethnic minorities and individuals from lower socio‐economic classes continue to trail behind in access to the internet and thus in taking advantage of TP opportunities. 28 To address this limitation, the Lancet Commission on Global Mental Health recommended adoption of digital interventions alongside traditional in‐person treatments, rather than as replacements. 29
3.3. Privacy and legal issues
A relevant concern about using TP is privacy. It is important to ensure conversations’ confidentiality and to protect health information and sensitive data. Another confidentiality issue is of technological nature, concerning network security and encryption 17 ; in fact, videoconferencing occurs through the internet connection, it is therefore essential to guarantee that the meeting will not be easily hacked into, or viewed by others. 14 Clinicians and organisations who are supplying telemental health services must adapt their connection pathways and equipment to the health information protection laws, such as the USA’s Health Insurance Portability and Accountability Act (HIPAA). In recent years, a variety of platforms (like Zoom, Bluejeans, SimplePractice and others) have been developed with opportune security and confidentiality, 30 but privacy cannot be guaranteed in its entirety. In fact, the FBI warned about the weakness of such platforms after some unidentified users invaded several school sessions, a phenomenon called “zoombombing”. Because of the COVID‐19 pandemic, some governments have issued an emergency waiver suspending the requirement to comply with information protection laws, as it happened in the USA for HIPPA, in order to facilitate access to telemedicine services. 30 However, the privacy issue remains a compelling one.
Similar with in‐person interventions, clinicians are legally obligated to seek informed consent and review possible risks and benefits of the treatment. 31 Nittari et al 32 recently reviewed legal issues related to informed consent, data protection, confidentiality, physician's malpractice and liability in telemedicine. The main issue reported by the authors is the global uncertainty of the legislation in the field. It has been suggested that clinicians need to update their knowledge and adapt to the newest regulations related to online interventions. 31
3.4. Telepsychiatry in the treatment of psychiatric disorders
TP has been proven to be valid and reliable in a variety of psychiatric disorders. Depression is one of the most studied, and the evidence supporting the treatment of depressive disorders via TP is robust. 33 A large number of systematic reviews and meta‐analyses have examined technology‐based interventions for depression, but only few of those have attempted to synthesise the data with the purpose of determining the admissibility and influencing factors of the implementation of TP. 34
There are different forms of internet‐delivered treatments for depression. One approach, based on bibliotherapy and the therapist's guidance via email or phone, uses primarily text‐based materials. There are also short treatments that are not generally delivered with guidance and do not usually target people with clinical depression; although they can reach more people at a lower cost, they do so with a presumably diminished effect. 35 Globally, it seems that computerised treatments, administered with the support of a therapist, are much more effective than the unsupported ones, and that is confirmed in many open studies. 36
Patients with depressive disorders have been shown to benefit from TP, as reported by several studies in which patients’ symptoms improved more in the telemental health group than in the traditional setting ones. A 2015 study evidenced how patients taking antidepressant in a high‐intensity telemedicine‐based collaborative care model reported less drug‐related side effects than the low‐intensity practice‐based collaborative care patients. 37
Evidence from several studies has underlined that the use of TP for delivering mental healthcare services can improve symptoms of depression among older adults. The effects are the reduction of depression symptoms and the improvement of comorbid health conditions. A 2013 review analysed the combination of TP with mobile apps targeting depression, anxiety disorders and substance abuse, reporting similar results. 38 Stanmore et al, in a meta‐analytic review, showed that TP improves not only the patient's global cognition score, but also his/her cognitive functioning, which is often affected in depressive disorders. 39
In 2019, Pruitt and colleagues assessed patients’ satisfaction in a group of military personnel with depression, who were included in a randomised clinical trial that utilised a type of psychotherapy known as Behavioural Activation Therapy for Depression (BATD); this was delivered in‐office and at home by videoconferencing. 40 They discovered that patients’ satisfaction was very high, with no significant difference between the two modalities, which is indicative of a comparable quality of care, and a satisfying level of therapeutic alliance between the patients and the clinicians. The two treatment modalities have diverse strengths and weaknesses: in‐person treatments offer a richer communication environment, both verbal and non‐verbal, when compared with the other; yet, the in‐home treatments may grant greater comfort because of the subjects’ ability to relax in a familiar setting. This balance between positive and negative aspects of the two modalities may explain the analogy of patients’ satisfaction observed in Pruitt's study. Contrary to popular belief, higher levels of end‐of‐treatment satisfaction for in‐person care were detected to be mostly associated with younger age patients. Conversely, the satisfaction for in‐home care was more frequently associated with older and symptomatic individuals. Plausible explanations for such results include stigma, symptom severity and convenience. Younger patients, or those with less debilitating symptoms, may be more satisfied with traditional care treatments, while the elderly patients, or more symptomatic patients, may prefer a home‐based care setting. 40
It has been proposed that telemental health strategies could be a useful resource in the treatment of patients with obsessive compulsive disorder (OCD). With this kind of patients, several barriers to treatment, such as logistic and financial barriers, as well as shame and fear of stigmatisation or discrimination, 41 could lead to the customary long delay from the onset of the disorder to the first treatment delivery 42 ; telemental health therapies have the potential to overcome these barriers. 43 In their extensive review, 44 Herbst et al highlighted that a lot of telemental health treatments have been used for OCD: computer programs, Computer‐Aided Vicarious Exposure (CAVE), Behaviour Therapy‐Steps (BT‐Steps), metacognitive training, meridian tapping, online Cognitive Behavioural Therapy (CBT)‐based group interventions, telephone‐administered CBT, videoconference‐based CBT. All these approaches were based on the CBT principles. Therapists’ level of involvement ranged from direct contact through video or phone, to completely automated computer programs with no direct involvement. All telemental health interventions resulted in a decrease in OCD symptoms for active participants. They observed that the most efficient studies included contact with the therapist (higher effect size and lower dropout rate), although approaches that did not include visual or auditory therapist's contact could reduce the inhibitory effect of shame and self‐stigmatisation, hence improving the treatment adherence for some patients, such as the ones with aggressive or sexual obsessions. It has been suggested that telemental health treatments for OCD could be useful in the context of a diversified care approach offering all patients a low‐threshold self‐treatment at first, to then move up to the face‐to‐face treatment, only when necessary. 45 , 46
Bolton and Dorstyn 47 analysed the role of tele‐psychological services in the management of post‐traumatic stress disorder (PTSD), a complex syndrome characterised by the re‐experiencing of a traumatic event, persistent avoidance and hyperarousal. 48 In their meta‐analysis, the authors evaluated studies using either a videoconferencing model only, or a hybrid design, which included the internet as the primary treatment modality in combination with real‐time or asynchronous communication with a therapist. All interventions were based on a cognitive behavioural framework and were time limited, with an average duration of 3 months. They determined that there was a short‐term effectiveness of the therapist‐assisted internet programs, with a large reduction in the severity of depression, anxiety symptoms and fear reactions, and an immediate improvement in suicidal ideation, social functioning and insomnia. Video‐based interventions produced short‐term improvements on affective symptoms, even though peers who received face‐to‐face therapy showed greater treatment progress. A 1 to 6 months follow‐up among those who accessed internet programs revealed an increased risk of alcohol consumption over time, but also a decline in cognitive and behavioural symptoms of PTSD and depression. The downside was in the difficulty with online cognitive restructuring tasks and the preference for other media tools (ie, mobile application) as a supplement to internet‐based guided self‐help. In a recent RCT, Haghnia et al 49 directly compared the efficacy of TP and face‐to‐face consultation in PTSD treatments in a population of 60 Iranian War veterans. Patients were divided into an experimental group and a control group; both groups were treated through face‐to‐face consultations for the first three sessions. Six follow‐up sessions were held remotely, using the Imo mobile application and Skype with the experimental group, and face‐to‐face with the control group. The researchers observed that, compared with the face‐to‐face method, TP increased access to psychiatric care, reduced follow‐up treatment costs and patients’ waiting time and increased patients’ satisfaction and physician‐patient communication.
The use of TP has been tested in patients with schizophrenia as well. In their review, Kasckow et al 50 summarised many studies involving telephone‐based, internet‐based and videoconference‐based interventions and concluded that TP approaches were feasible with this kind of patients and that they could improve treatment outcomes. TP may help to engage these patients, to improve their medication adherence rates, to detect the exacerbation of psychotic symptoms and to prevent hospitalisations; nonetheless, only a strong patient‐clinician engagement seems to guarantee an improvement in clinical and social functioning and an adequate relapse prevention. 51 Patients with schizophrenia exhibited high satisfaction levels when using TP approaches; in fact, many patients reported feeling more comfortable using TP methods to connect with their psychiatrist and, additionally, anonymous web‐based interventions may help them reduce stigmatisation feelings.
Gire et al systematically reviewed the literature on mobile device remote interventions for the treatment and assessment of psychosis (mHealth). The strongest evidence found was related to mHealth technologies for medication adherence, showing them feasible and acceptable. Other proposed applications of mHealth in psychosis are SMS‐based prompts related to follow‐up appointments, hygiene, physical exercise, symptom management and supporting messages. 52
3.5. Psychotherapy via telepsychiatry
Psychotherapy is now the front line, gold standard treatment for common mental health disorders in evidence‐based medicine. 53 Yet, because of the barriers including access, cost and stigma, estimates suggest that up to two‐thirds of individuals do not access or receive evidence‐based care. 54 TP could help overcome those barriers.
Herbst et al 43 showed how, in a population of 34 patients, an internet‐based, therapist‐guided CBT with exposure and response prevention led to significant reductions in the main symptoms of OCD; they also observed that this improvement remained stable throughout the 6‐month follow‐up period after treatment. The i‐CBT did not inhibit a solid patient‐therapist working alliance; in fact, a strong and stable patient‐therapist relation was established. 55 Matsumoto et al 56 examined the feasibility of videoconference‐delivered CBT in 30 adult patients with mild to severe OCD, panic disorder (PD) and social anxiety disorder (SAD). They determined that there was a significant reduction in symptoms for each group, with a remission rate of 40% for OCD, 50% for PD and 22% for SAD. The therapeutic alliance significantly improved throughout the treatment and its scores were comparable to those of in‐person CBT. The dropout rate was very low (3%), since 97% of patients completed the videoconference‐delivered CBT treatment. Interestingly, 83% of the participants affirmed to prefer videoconference‐delivered CBT to face‐to‐face CBT.
3.6. New technologies in mental healthcare
Additionally to telehealth services, in recent years, digital technologies have found other numerous and relevant declinations. Firstly, the growing mediatic attention towards psychiatric disorders and mental health problems has led to the development of specifically dedicated smartphone applications. Through a search on dedicated platforms conducted in 2019, 1435 mobile apps were identified, 449 of which addressing anxiety problems, 450 addressing depression, 282 addressing schizophrenia, 124 addressing self‐harm and 140 addressing substance use disorders. 57 This global mobile‐Health apps market, which is dominated by Apple's App Store and Google Play Store, is characterised by an annual growth rate of circa 38.3% starting in 2019 and generating an estimated US 111.1 billion by 2025. Examples of mobile apps’ potentialities are the capacity to monitor and track health parameters, tobacco smoke and alcohol consumption, as well as the trend of symptoms, sleep and stress levels. They can also provide electronic reminders for the correct management of pharmacotherapy and can help patients to keep in touch with healthcare providers.
Secondly, the applications of Virtual Reality (VR) are very promising for the mental health field. VR is defined as a computer‐generated simulation, a set of computer‐generated images and sounds, representing a place or situation with which the person can interact utilising special electronic equipment. 58 Immersion in VR allows the patient to savour emotions he has already experienced in the real world, yet also to face dysfunctional behaviours and traumatic situations in a safe setting. It allows each individual to act as the protagonist and to regain control of his actions, to feel as the active builder of his own experience and, over time, of the changes he brings into his own life. 59 The best applications of VR are found in PTSD, specific phobias, body‐image disorders, such as nervous anorexia, and autism spectrum disorders.
Finally, today, psychiatrists have the unprecedented opportunity to benefit from the use of artificial intelligence (AI) and, more specifically, of Machine Learning. This technique allows the clinicians to analyse huge amounts of data with the aim of producing a biologically founded re‐classification of major psychiatric disorders. Increasing evidence suggests that the sub‐classifications obtained from Machine Learning data analysis have better predictive power of treatment outcome than the traditional DSM/ICD models. In a new era of evidence‐based psychiatry, these objectively measurable transdiagnostic endophenotypes will allow the clinicians to make an early diagnosis, to individualise treatment and to make therapeutic adjustments to reduce disease relapses that are tailored for each individual. This has been called computational psychiatry. 60
4. DISCUSSION
COVID‐19 pandemic brought to reduced social contact and impeded face‐to‐face interactions, also in delivering psychiatric assistance. The purpose of this paper was to review our knowledge about TP to inform its use during this pandemic, still lacking original studies addressing this topic. As shown, many are the advantages of TP, such as an improved access to care, the possibility for patients to receive psychiatric assistance in their native language, a reduction of travel time and costs and a comparable effectiveness to in‐person care. 17 However, is also important to consider some limitations of telehealth. First of all, more studies are needed to ensure a broader and more reliable validation of TP, in terms of diagnostic reliability and therapeutic efficiency in the short and long term. Secondly, it is necessary to consider that TP is not suitable for all patients. Moreover, some concerns remain about TP use during acute crisis: important cues, such as facial expressions, tone and posture, can be missed in the TP consultation. For this reason, there must be regular screenings for adverse events and a procedure for crisis intervention must be readily available. 43 An important recommendation is to connect with on‐site staff who may intervene if necessary. 16
The privacy issue is also not to be underestimated; patients should be educated about personal privacy problems rising from using TP services outside the traditional clinical setting, such as when speaking in rooms where family members can hear the conversation, or in public places where anyone might listen. 14 The clinician himself must maintain privacy rules and ensure that no one will interrupt the session. 22
Despite the advantages and the technological progress, TP is globally underused; in 2009, only about 2% of psychiatrists in the United States had used TP. 12 A recent article examining a large population of subjects from 2005 to 2017 concluded that, although telemedicine care had substantially increased during that time, its use was still not widespread in 2017. 61 In addition, in 2014, the same 100 clinicians accounted for more than half of all telemental health visits that year, 62 suggesting that TP practice had been undertaken by very few, selected clinicians.
During this pandemic period, several authors all over the world underlined the need to promote online mental healthcare services and encourage their use. 13 , 63 , 64 In fact, TP can capably respond to the mental health needs of people in isolation or quarantine, reducing infection risk. TP observes social distancing, avoids care interruptions and increases public health outcomes. 65 Considering that psychiatric population is more vulnerable to stress than general population, a disruption in care is concerning as it may increase the risk of symptom exacerbation and relapse. TP is precious to ensure continuity of care for these populations at higher risk of decompensation. 63 In this regard, recently, the US Centers for Medicare and Medicaid Services waived restrictions on originating sites for telehealth 66 and the ability of healthcare professionals to prescribe remotely has been expanded to cover controlled substances. 67 In China, in addition, AI programs have been used as interventions for psychological crises during the pandemic. Furthermore, online psychological counselling services have been widely established as 24‐hours services on all days of the week. 68 Considering the experiences from past serious virus pandemics, improvement of mental healthcare is needed. 69 The increasing demand for psychiatric services in the overburdened mental healthcare system presents a risk of creating a global public mental health crisis throughout the world. 70 Despite initial difficulties to adapt the system to TP requirements, this crisis can be an opportunity to improve the healthcare system and to expand its accessibility for patients also for the future. 63
The review presented here has some limitations. Mainly, it has been conducted in a narrative way and using only one electronic database to search for articles. This decision has been undertaken in order to rapidly review the literature to inform the unfolding pandemic situation, but possibly limited the number of references obtained. There is the need for future research to investigate the topic in a systematic way, in order to rigorously assess the contribution of TP in COVID‐19 pandemic.
Focused and continuous trainings of clinicians are required to increase the awareness of the benefits and risks of TP. In relation to this, and considering the present pandemic, formally teaching TP in medical schools, residency trainings and continuing medical education programs should be encouraged. Among other benefits, this may be a way to help cultural acceptance of TP both among patients and medical staff.
In conclusion, TP is destined to expand in the future and mental health professionals have a strategic role to help ensure that these technologies respect the therapeutic relationship and remain rigorous in their scientific foundation.
DISCLOSURE
All the authors declare no conflict of interest.
Di Carlo F, Sociali A, Picutti E, et al. Telepsychiatry and other cutting‐edge technologies in COVID‐19 pandemic: Bridging the distance in mental health assistance. Int J Clin Pract 2020;75:e13716. 10.1111/ijcp.13716
REFERENCES
- 1. Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among italian people during the covid‐19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health. 2020;17:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ni MY, Yang L, Leung CMC, et al. Mental health, risk factors, and social media use during the COVID‐19 epidemic and Cordon Sanitaire among the community and health professionals in Wuhan, China: cross‐sectional survey. JMIR Ment Heal. 2020;7:e19009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. González‐Sanguino C, Ausín B, Castellanos MÁ, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID‐19) in Spain. Brain Behav Immun. 2020;87:172‐176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ahmed MZ, Ahmed O, Aibao Z, et al. Epidemic of COVID‐19 in China and associated psychological problems. Asian J Psychiatr. 2020;51:102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID‐19 epidemic. Lancet Psychiatry. 2020;7:e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Király O, Potenza MN, Stein DJ, et al. Preventing problematic internet use during the COVID‐19 pandemic: consensus guidance. Compr Psychiatry. 2020;100:152180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pettorruso M, Valle S, Cavic E, et al. Problematic Internet use (PIU), personality profiles and emotion dysregulation in a cohort of young adults: trajectories from risky behaviors to addiction. Psychiatry Res. 2020;289:113036. [DOI] [PubMed] [Google Scholar]
- 8. Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS‐CoV‐2). Science. 2020;368:489‐493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhou J, Liu L, Xue P, et al. Mental health response to the COVID‐19 outbreak in China. Am J Psychiatry. 2020;177:574‐575. [DOI] [PubMed] [Google Scholar]
- 10. Kola L. Global mental health and COVID‐19. Lancet Psychiatry. 2020;0366:19‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. WHO . A health telematics policy in support of WHO’s Health‐For‐All strategy for global health development: report of the WHO group consultation on health telematics. 1997.
- 12. Yellowlees P, Nafiz N. The psychiatrist‐patient relationship of the future: anytime, anywhere? Harv Rev Psychiatry. 2010;18:96‐102. [DOI] [PubMed] [Google Scholar]
- 13. Corruble E. A viewpoint from Paris on the COVID‐19 pandemic: a necessary turn to telepsychiatry. J Clin Psychiatry. 2020;81. 10.4088/JCP.20com13361. [DOI] [PubMed] [Google Scholar]
- 14. Hilt RJ. Telemedicine for child collaborative or integrated care. Child Adolesc Psychiatr Clin N Am. 2017;26:637‐645. [DOI] [PubMed] [Google Scholar]
- 15. Richardson LK, Frueh BC, Grubaugh AL, et al. Current directions in videoconferencing tele‐mental health research. Clin Psychol (New York). 2009;16:323‐338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Simpson SG, Reid CL. Therapeutic alliance in videoconferencing psychotherapy : a review. Aust J Rural Heal. 2014;22:280‐299. [DOI] [PubMed] [Google Scholar]
- 17. Cowan KE, McKean AJ, Gentry MT, et al. Barriers to use of telepsychiatry: clinicians as gatekeepers. Mayo Clin Proc. 2019;94:2510‐2523. [DOI] [PubMed] [Google Scholar]
- 18. Hilty DM, Sunderji N, Suo S, et al. Telepsychiatry and other technologies for integrated care: evidence base, best practice models and competencies. Int Rev Psychiatry. 2018;30 292‐309. [DOI] [PubMed] [Google Scholar]
- 19. Egede LE, Acierno R, Knapp RG, et al. Psychotherapy for depression in older veterans via telemedicine: a randomised, open‐label, non‐inferiority trial. Lancet Psychiatry. 2015;2:693‐701. [DOI] [PubMed] [Google Scholar]
- 20. O’Reilly R, Bishop J, Maddox K, et al. Is telepsychiatry equivalent to face‐to‐face psychiatry? Results from a randomized controlled equivalence trial. Psychiatr Serv. 2007;58:836‐843. [DOI] [PubMed] [Google Scholar]
- 21. De Las CC, Arredondo MT, Cabrera MF, et al. Randomized clinical trial of telepsychiatry through videoconference versus face‐to‐face conventional psychiatric treatment. Telemed J e‐Health. 2006;12:341‐350. [DOI] [PubMed] [Google Scholar]
- 22. May C, Gask L, Atkinson T, et al. Resisting and promoting new technologies in clinical practice: the case of telepsychiatry. Soc Sci Med. 2001;52:1889‐1901. [DOI] [PubMed] [Google Scholar]
- 23. Abrams J, Sossong S, Schwamm LH, et al. Practical issues in delivery of clinician‐to‐patient telemental health in an academic medical center. Harv Rev Psychiatry. 2017;25:135‐145. [DOI] [PubMed] [Google Scholar]
- 24. Mclaren P, Baht CJ, Summerfield AB, et al. An evaluation of the use of interactive television in an acute psychiatric service. J Telemed Telecare. 1995;1:79‐85. [DOI] [PubMed] [Google Scholar]
- 25. Barton PL, Brega AG, Devore PA, et al. Specialist physicians’ knowledge and beliefs about telemedicine: a comparison of users and nonusers of the technology. Telemed e‐Health. 2007;13:487‐499. [DOI] [PubMed] [Google Scholar]
- 26. Glueckauf RL, Maheu MM, Drude KP, et al. Survey of psychologists’ telebehavioral health practices: technology use, ethical issues, and training needs. Prof Psychol Res. 2018;49:205‐219. [Google Scholar]
- 27. Choi NG, Dinitto DM. The digital divide among low‐income homebound older adults : internet use patterns, eHealth literacy, and attitudes toward computer/internet use. J Med Internet Res. 2013;15:1‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chesser A, Burke A, Reyes J, et al. Navigating the digital divide: a systematic review of eHealth literacy in underserved populations in the United States. Inform Health Soc Care. 2016;41:1‐19. [DOI] [PubMed] [Google Scholar]
- 29. Patel V, Saxena S, Lund C, et al. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392:1553‐1598. [DOI] [PubMed] [Google Scholar]
- 30. Wright JH, Caudill R. Remote treatment delivery in response to the COVID‐19 pandemic. Psychother Psychosom. 2020;40202:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Liem A, Sit HF, Arjadi R, et al. Ethical standards for telemental health must be maintained during the COVID‐19 pandemic. Asian J Psychiatr. 2020;53:102218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nittari G, Khuman R, Baldoni S, et al. Telemedicine practice: review of the current ethical and legal challenges. Telemed J e‐Health. 2020;26:1427‐1437. 10.1089/tmj.2019.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Andersson G, Cuijpers P. Internet‐based and other computerized psychological treatments for adult depression: a meta‐analysis. Cogn Behav Ther. 2009;38:196‐205. [DOI] [PubMed] [Google Scholar]
- 34. Harerimana B, Forchuk C, Regan TO. The use of technology for mental healthcare delivery among older adults with depressive symptoms: a systematic literature review. Int J Ment Health Nurs. 2019;28:657‐670. [DOI] [PubMed] [Google Scholar]
- 35. Mayo‐Wilson E. Internet‐based cognitive behaviour therapy for symptoms of depression and anxiety: a meta‐analysis. Psychol Med. 2007;37:1211‐1212. [DOI] [PubMed] [Google Scholar]
- 36. Christensen H, Griffiths K, Groves C, et al. Free range users and one hit wonders: community users of an Internet‐based cognitive behaviour therapy program. Aust N Z J Psychiatry. 2006;40:59‐62. [DOI] [PubMed] [Google Scholar]
- 37. Chan S, Parish M, Yellowlees P, et al. Telepsychiatry today. Curr Psychiatry Rep. 2015;17):89. [DOI] [PubMed] [Google Scholar]
- 38. Donker T, Petrie K, Proudfoot J, et al. Smartphones for smarter delivery of mental health programs: a systematic review. J Med Internet Res. 2013;15:e247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Stanmore E, Stubbs B, Vancampfort D, et al. The effect of active video games on cognitive functioning in clinical and non‐clinical populations: a meta‐analysis of randomized controlled trials. Neurosci Biobehav Rev. 2017;78:34‐43. [DOI] [PubMed] [Google Scholar]
- 40. Pruitt LD, Vuletic S, Smolenski DJ, et al. Predicting post treatment client satisfaction between behavioural activation for depression delivered either in‐person or via home‐based telehealth. J Telemed Telecare. 2019;25:460‐467. [DOI] [PubMed] [Google Scholar]
- 41. Marques L, LeBlanc NJ, Wegarden HM, et al. Barriers to treatment and service utilization in an internet sample of individuals with obsessive‐compulsive symptoms. Depress Anxiety. 2010;27:470‐475. [DOI] [PubMed] [Google Scholar]
- 42. Pinto A, Mancebo MC, Eisen JL, et al. The Brown Longitudinal Obsessive Compulsive Study: clinical features and symptoms of the sample at intake. J Clin Psychiatry. 2006;67:703‐711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Herbst N, Voderholzer U, Thiel N, et al. No talking, just writing! efficacy of an internet‐based cognitive behavioral therapy with exposure and response prevention in obsessive compulsive disorder. Psychother Psychosom. 2014;83:165‐175. [DOI] [PubMed] [Google Scholar]
- 44. Herbst N, Voderholzer U, Stelzer N, et al. The potential of telemental health applications for obsessive‐compulsive disorder. Clin Psychol Rev. 2012;32:454‐466. [DOI] [PubMed] [Google Scholar]
- 45. Mataix‐Cols D, Marks IM. Self‐help with minimal therapist contact for obsessive‐compulsive disorder: a review. Eur Psychiatry. 2006;21:75‐80. [DOI] [PubMed] [Google Scholar]
- 46. Tolin DF, Diefenbach GJ, Gilliam CM. Stepped care versus standard cognitive‐behavioral therapy for obsessive‐compulsive disorder: a preliminary study of efficacy and costs. Depress Anxiety. 2011;28:314‐323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Bolton AJ, Dorstyn DS. Telepsychology for posttraumatic stress disorder: a systematic review. J Telemed Telecare. 2015;21:254‐267. [DOI] [PubMed] [Google Scholar]
- 48. Martinotti G, Sepede G, Brunetti M, et al. BDNF concentration and impulsiveness level in post‐traumatic stress disorder. Psychiatry Res. 2015;229:814‐818. [DOI] [PubMed] [Google Scholar]
- 49. Haghnia Y, Samad‐Soltani T, Yousefi M, et al. Telepsychiatry‐ based care for the treatment follow‐up of Iranian war veterans with post‐ traumatic stress disorder: a randomized controlled trial. Iran J Med Sci. 2019;44:291‐298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kasckow J, Felmet K, Appelt C, et al. Telepsychiatry in the assessment and treatment of schizophrenia. Clin Schizophr Relat Psychoses. 2014;8:21‐27A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Krzystanek M, Krysta K, Ska K. Treatment compliance in the long‐term paranoid schizophrenia telemedicine study. J Technol Behav Sci. 2017;2:84‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gire N, Farooq S, Naeem F, et al. mHealth based interventions for the assessment and treatment of psychotic disorders: a systematic review. mHealth. 2017;3:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. NICE . Depression in adults. Treatment and management. 2019. [PubMed]
- 54. Lake J. Urgent need for improved mental health care and a more collaborative model of care. Perm J. 2017;21:17‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Herbst N, Franzen G, Voderholzer U, et al. Working alliance in internet‐based cognitive‐behavioral therapy for obsessive‐compulsive disorder. Psychother Psychosom. 2016;85:117‐118. [DOI] [PubMed] [Google Scholar]
- 56. Matsumoto K, Sutoh C, Asano K, et al. Internet‐based cognitive behavioral therapy with real‐time therapist support via videoconference for patients with obsessive‐compulsive disorder, panic disorder, and social anxiety disorder: pilot single‐arm trial. J Med Internet Res. 2018;20:e12091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Larsen ME, Huckvale K, Nicholas J, et al. Using science to sell apps: evaluation of mental health app store quality claims. Digit Med. 2019;2:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Park MJ, Kim DJ, Lee U, et al. A literature overview of Virtual Reality (VR) in treatment of psychiatric disorders: recent advances and limitations. Front Psychiatry. 2019;10:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Riva G. Transforming experience: the potential of augmented reality and virtual reality for enhancing personal and clinical change. Front Psychiatry. 2016;7:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Bzdok D, Meyer‐lindenberg A. Review machine learning for precision psychiatry: opportunities and challenges. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3:223‐230. [DOI] [PubMed] [Google Scholar]
- 61. Barnett ML, Ray KN, Souza J, et al. Trends in telemedicine use in a large commercially insured population, 2005–2017. JAMA. 2018;320:2147‐2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Mehrotra A, Huskamp HA, Souza J, et al. Rapid growth in mental health telemedicine use among rural Medicare beneficiaries, wide variation across states. Health Aff. 2017;36:909‐917. [DOI] [PubMed] [Google Scholar]
- 63. Kannarkat JT, Smith NN, McLeod‐Bryant SA. Mobilization of telepsychiatry in response to COVID‐19—moving toward 21st century access to care. Adm Policy Ment Heal Ment Heal Serv Res. 2020;47:489‐491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Zhou X, Snoswell CL, Harding LE, et al. The role of telehealth in reducing the mental health burden from COVID‐19. Telemed J e‐Health. 2020;26:26‐28. [DOI] [PubMed] [Google Scholar]
- 65. Whaibeh E, Mahmoud H, Naal H. Telemental health in the context of a pandemic: the COVID‐19 experience. Curr Treat Options Psychiatry. 2020;7:198‐202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. CMS Approves First State Request for 1135 Medicaid Waiver in Florida | CMS [Internet]. https://www.cms.gov/newsroom/press‐releases/cms‐approves‐first‐state‐request‐1135‐medicaid‐waiver‐florida. Accessed June 27, 2020.
- 67. DEA Okays Telehealth to Prescribe Opioids Amid COVID‐19 Emergency [Internet]. https://mhealthintelligence.com/news/dea-okays-telehealth-to-prescribe-opioids-amid-covid-19-emergency?. Accessed June 27, 2020.
- 68. Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID‐19 outbreak. Lancet. Psychiatry. 2020;7:e17‐e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Xiang YT, Yang Y, Li W, et al. novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2019;2020:228‐229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ćosić K, Popović S, Šarlija M, et al. Impact of human disasters and Covid‐19 pandemic on mental health: potential of digital psychiatry. Psychiatr Danub. 2020;32:25‐31. [DOI] [PubMed] [Google Scholar]


