Abstract
Objectives
The COVID‐19 pandemic has led to unprecedented levels of unemployment and financial strain for many Americans. Among the individuals impacted by financial strain are pregnant women, for whom added financial stress may be particularly impactful due to the costs associated with prenatal care and providing for a newborn. Financial stress has been previously associated with elevated depression symptoms among pregnant women, which could have significant impacts on birth outcomes and long‐term offspring health. However, the impacts of COVID‐19‐associated financial stress on maternal depression in pregnancy has not been investigated.
Methods
Here, we evaluated whether COVID‐19‐associated financial stress was associated with increased likelihood of a clinically significant depression score (Edinburgh Postnatal Depression Score ≥ 15) among pregnant women living in the United States during the COVID‐19 pandemic. Data come from an online survey administered to a convenience sample in April 2020 (N = 2099).
Results
Forty‐three percent of participants reported experiencing financial stress as a result of the pandemic, while 24% of participants had a clinically significant depression score. COVID‐19‐related financial stress was significantly associated with increased likelihood of a clinically significant depression score, even after adjustment for covariates including participant education and income (adjusted Odds Ratio: 2.23, 95% CI = 1.80, 2.77, P < .001).
Conclusions
Financial stress caused by the COVID‐19 pandemic is associated with more than two times the likelihood of depression during pregnancy, which could impact birth outcomes and long‐term offspring health.
1. INTRODUCTION
The COVID‐19 pandemic has had severe financial impacts globally, including in the United States. During April 2020 a record 23.1 million individuals filed for unemployment, corresponding to 14.7% of Americans, a prevalence not seen since the Great Depression (Bureau of Labor Statistics, 2020). These unprecedented financial losses could be especially impactful for those expecting a child. Financial insecurity due to job loss could result in lost health insurance coverage and an inability to pay for added expenses associated with a newborn.
Prior research has found that lower income and financial struggles are associated with increased risk of poor mental health in pregnancy (Pooler, Perry, & Ghandour, 2013). According to the Developmental Origins of Health and Disease hypothesis, maternal stress increases risk of adverse birth outcomes and poor later health in offspring (Gluckman, Buklijas, & Hanson, 2016). Consistent with this hypothesis, prenatal depression is associated with preterm birth and low birth weight (Grote et al., 2010), as well as poorer offspring mental and physical health in later life (Davalos, Yadon, & Tregellas, 2012). These effects could occur through a combination of prenatal and postnatal biological and behavioral factors, such as in utero exposure to stress hormones and differences in behavioral responsiveness to offspring (eg, differences in breastfeeding or caregiving behavior; Conching & Thayer, 2019). It is possible that COVID‐19‐associated impacts on stress, including financial stress, could contribute to elevated depression among pregnant women, and potentially also to adverse developmental programming in offspring. However, the extent to which financial stress may impact maternal mental health, including depression risk, during the COVID‐19 pandemic has yet to be determined.
As a first step toward determining whether financial stress resulting from the pandemic could potentially affect maternal and offspring health via impacts on maternal depression, here we assess whether financial worries related to the COVID‐19 pandemic is associated with depression symptoms among pregnant women living in the United States.
2. METHODS
Data come from the COVID‐19 and Reproductive Effects (CARE) study, an online survey that was administered to a convenience sample recruited using informational flyers shared through social media (Facebook, Twitter, Reddit) and to U.S.‐based contacts working in maternal health. Zip code data were collected to assess participant distribution. Data reported here were collected from April 16 to 30 (N = 2099). This study received ethical approval from Dartmouth College (STUDY00032045).
2.1. Financial stress
Participants were asked to rate whether they agreed or disagreed (Likert question; five options ranging from strongly disagree to strongly agree) with the statement “I am worried about my financial situation due to the COVID‐19 crisis.” Participants who stated that they agreed or strongly agreed with the statement were classified as having experienced COVID‐19‐related financial stress.
2.2. Depression symptoms
Depression symptoms were screened using the Edinburgh Postnatal Depression Survey (EPDS). Depression symptoms were analyzed according to clinically significant depression criteria for pregnant women (cut‐point ≥15; Matthey, Henshaw, Elliott, & Barnett, 2006).
2.3. Covariates
Participant age (years), education (less than a bachelor's degree, a bachelor's degree, or a degree beyond a bachelor's degree), household income (USD; <$49 999, $50 000‐$99 999, or $100000+), household size (number of people), household composition (living with partner; living with parents/in‐laws), previous birth (yes/no), current gestational week during survey, and self‐reported health (poor or fair/good or excellent) were analyzed as potential covariates. Race/ethnicity was also analyzed as a potential covariate and measured via self‐report according to the Office of Management and Budget Standards (https://www.govinfo.gov/content/pkg/FR‐1997‐10‐30/pdf/97‐28653.pdf). Native Hawaiian/Pacific Islander participants were re‐classified as “Other” due to a small sample size (N = 3). Gestational week and household size were not significantly associated with COVID‐19‐related financial stress or depression and so were not included in the regression model.
2.4. Statistical analysis
Data analyses were conducted using Stata 15.1. All continuous variables exhibited normal distributions, with skewness values within approximately ±0.5 and kurtosis values within approximately ±3. Sample descriptive statistics were calculated and bivariate analyses were conducted to evaluate significant differences in study covariates according to COVID‐19‐related financial worries. A multivariate logistic regression model was used to evaluate whether financial stress was associated with increased likelihood of a clinically significant depression score, adjusting for maternal age, previous birth, self‐rated health, race/ethnicity, education, household income, and household composition. Multicollinearity was not detected; all VIF values were in an acceptable range of 1.02 to 1.43. Hosmer and Lemeshow's goodness of fit test indicated the model fit the data well (Prob > chi2 = 0.73).
3. RESULTS
Participants were distributed across all 50 U.S. states, and one participant lived in the U.S. territory of Puerto Rico (Figure S1). Twenty‐four percent of the sample had a clinically significant depression score, while 43% of the sample were worried about their financial situation due to COVID‐19 (Table 1). Age, previous birth, race/ethnicity, self‐rated health, household income, education, living with partner, living with parents or in‐laws all significantly varied according to COVID‐19‐related financial worries.
TABLE 1.
Summary statistics of study sample
| Entire sample (N = 2099) | Expressed COVID‐19‐related financial worries (N = 896) | Did not express COVID‐19‐related financial worries (N = 1203) | P value | |
|---|---|---|---|---|
| Age (years) | 31.3 (4.4) | 31.0 (4.5) | 31.5 (4.3) | .01 |
| Weeks pregnant | 26.4 (9.0) | 26.4 (8.9) | 26.4 (9.2) | .99 |
| Previous birth | .02 | |||
| Yes | 1038 (49.5%) | 417 (46.5%) | 621 (51.6%) | |
| No | 1061 (50.6%) | 479 (53.5%) | 582 (48.4%) | |
| Race/ethnicity | ||||
| White | 1814 (86.4%) | 749 (83.6%) | 1065 (88.5%) | .03 |
| Hispanic/Latino | 133 (6.3%) | 74 (8.3%) | 59 (4.9%) | |
| African American | 31 (1.5%) | 15 (1.7%) | 16 (1.3%) | |
| Asian | 70 (3.3%) | 32 (3.6%) | 38 (3.2%) | |
| American Indian/Alaska | 12 (0.6%) | 6 (0.7%) | 6 (0.5%) | |
|
Native Other |
39 (1.9%) |
20 (2.2%) |
19 (1.6%) | |
| Self‐rated health | .006 | |||
| Poor/fair | 150 (7.2%) | 80 (8.9%) | 70 (5.8%) | |
| Good/excellent | 1926 (92.9%) | 816 (91.1%) | 1133 (94.2%) | |
| Household income | ||||
| $ < 49 999 | 256 (12.2%) | 175 (19.5%) | 81 (6.7%) | |
| $50‐99 000 | 695 (33.1%) | 317 (35.4%) | 378 (31.4%) | |
| $100 000+ | 1148 (54.7%) | 404 (45.1%) | 744 (61.9%) | <.001 |
| Education | ||||
| Less than bachelor's degree | 492 (23.4%) | 279 (31.2%) | 213 (17.7%) | <.001 |
| Bachelor's degree | 730 (34.8%) | 280 (31.3%) | 450 (37.4%) | |
| Degree beyond bachelor's | 877 (41.8%) | 337 (37.6%) | 540 (44.9%) | |
| Household size | 2.9 (1.1) | 2.9 (1.2) | 2.8 (1.0) | .40 |
| Living with partner | .004 | |||
| Yes | 2010 (95.8%) | 848 (94.7%) | 1162 (96.6%) | |
| No | 89 (4.2%) | 48 (5.4%) | 41 (3.4%) | |
| Live with parents/in‐laws | .003 | |||
| Yes | 120 (5.7%) | 67 (7.5%) | 53 (4.4%) | |
| No | 1979 (94.3%) | 829 (92.5%) | 1150 (95.6%) | |
| Clinically significant depression (EPDS ≥ 15) | ||||
| Yes | 496 (23.6%) | 295 (32.9%) | 201 (16.7%) | <.001 |
| No | 1603 (76.4%) | 601 (67.1%) | 1002 (83.3%) |
Note: P values report significant differences in sample characteristics by whether or not participants expressed financial worries due to the COVID‐19 pandemic (yes/no) in chi‐squared tests (categorical variables) and t tests (continuous variables). Bold values = P < .05.
Women who were concerned about their financial situation were more than twice as likely to have a clinically significant depression score (adjusted Odds Ratio [aOR]: 2.23, 95% CI = 1.80, 2.77, P < .001, adjusted model R 2 = 0.06; Figure 1). Better self‐rated health was associated with significantly lower likelihood of depression (aOR: 0.37, 95% CI 0.26, 0.52, P < .001), while living with parents or in‐laws was associated with higher likelihood of depression (aOR: 1.58, 95% CI 1.023, 2.42, P = .037).
FIGURE 1.
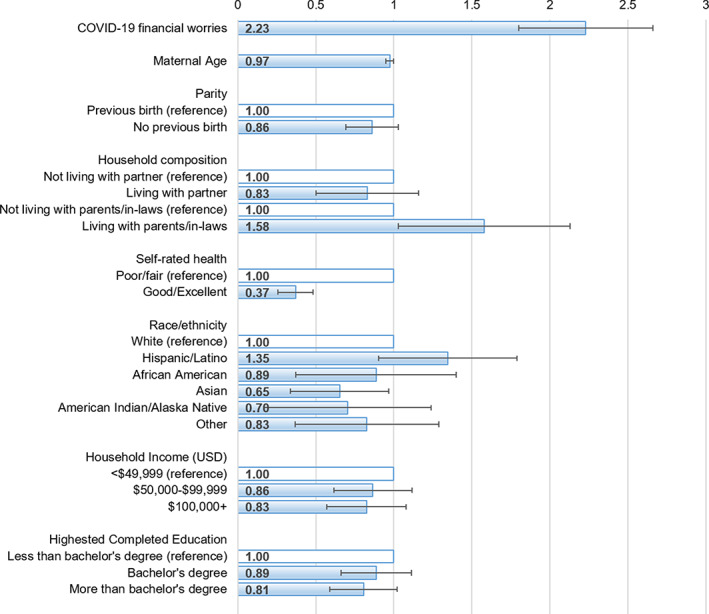
Adjusted odds ratios and 95% confidence intervals from logistic regression model predicting clinically significant depression symptoms in pregnancy (EPDS ≥ 15; N = 2099)
4. DISCUSSION
Over 40% of the sample reported that the COVID‐19 crisis had caused them to worry about their financial situation. Financial stress caused by the COVID‐19 pandemic was significantly associated with twice the likelihood of having clinically significant depression. These effects were independent of other common predictors of depression in pregnancy, including household income. Living with parents or in‐laws, which was significantly more common among lower income participants (lowest income category: 45 (14.7%), middle income category: 44 (5.6%), highest income category: 51 (4.0%), χ2 (2) = 50.3, P < .001), and among those who reported COVID‐19‐related financial stress (Table 1), was also associated with increased likelihood of depression. While COVID‐19 financial stress was more common among lower‐income participants (Table 1), the fact that this variable was associated with depression even after adjusting for income suggest that even higher‐income individuals who experience COVID‐19‐associated financial stress are at risk of developing depression.
High childcare costs, a lack of federally mandated paid maternity leave, and high maternity care costs exert an economic toll on American families. During the COVID‐19 pandemic these financial stressors have only increased, with record unemployment. Moreover, shifts to telehealth and associated barriers to effective patient‐provider communication can increase the chance that maternal depression may go undetected and untreated (Thayer & Gildner, In review). Maternal depression as a result of financial stress could potentially impact perinatal birth outcomes, thereby having long‐term impacts on offspring health (Bogin & Varea, 2020). Studies evaluating the impacts of the pandemic on children born during this time should focus on phenotypes known to be affected by prenatal stress, including birth size, changes in stress physiology functioning, cellular aging, and social and cognitive development (Suarez et al., 2018; Thayer, Wilson, Kim, & Jaeggi, 2018).
While there are many strengths to this analysis, including a large sample size, limitations exist. This analysis is cross‐sectional, meaning that this association cannot be interpreted as causal. This convenience sample is also not nationally representative, particularly with respect to socioeconomic and ethnic diversity (Martin, Hamilton, Osterman, & Driscoll, 2019). Additional research with more diverse samples is needed.
In sum, our findings suggest that the severe financial impacts of the COVID‐19 pandemic have affected mental health for pregnant women living in the U.S. Human biologists should consider the long‐term impacts of COVID‐19‐related stressors—including financial stress—on maternal and offspring health (Gildner & Thayer, 2020).
AUTHOR CONTRIBUTIONS
Zaneta Thayer: Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; visualization; writing‐original draft. Theresa Gildner: Conceptualization; data curation; funding acquisition; investigation; methodology; project administration; writing‐review and editing.
Supporting information
FIGURE S1: Supporting information
ACKNOWLEDGMENTS
Nadia Clement assisted with building the online survey and designing the recruitment flyers. Margaret Sherin, Gloriuese Uwizeye, and Chlöe Sweetman, provided feedback on the questionnaire during development. Elise Laugier generated the map of participant distribution across the United States. Thayer was supported by Wenner‐Gren Hunt Award #9687. Participant compensation was provided through the Claire Garber Goodman Fund for Anthropological Research.
Thayer ZM, Gildner TE. COVID‐19‐related financial stress associated with higher likelihood of depression among pregnant women living in the United States. Am J Hum Biol. 2021;33:e23508. 10.1002/ajhb.23508
Funding information Claire Garber Goodman Fund for Anthropological Research; Wenner‐Gren Foundation, Grant/Award Number: 9687
REFERENCES
- Bogin, B. , & Varea, C. (2020). COVID‐19, crisis, and emotional stress: A biocultural perspective of their impact on growth and development for the next generation. Am J Hum Biol, e23474. https://onlinelibrary.wiley.com/action/showCitFormats?doi=10.1002%2Fajhb.23474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics . (2020). The Employment Situation: April 2020. Department of Labor, USA. USDL‐20‐0815
- Conching, A. K. S. , & Thayer, Z. (2019). Biological pathways for historical trauma to affect health: A conceptual model focusing on epigenetic modifications. Social Science & Medicine, 230, 74–82. [DOI] [PubMed] [Google Scholar]
- Davalos, D. B. , Yadon, C. A. , & Tregellas, H. C. (2012). Untreated prenatal maternal depression and the potential risks to offspring: A review. Archives of Women's Mental Health, 15(1), 1–14. [DOI] [PubMed] [Google Scholar]
- Gildner, T. , & Thayer, Z. (2020). Maternal and child health during the COVID‐19 pandemic: Contributions in the field of human biology. Am J Hum Biol, e23494. https://onlinelibrary.wiley.com/action/showCitFormats?doi=10.1002%2Fajhb.23494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluckman, P. D. , Buklijas, T. , & Hanson, M. A. (2016). The developmental origins of health and disease (DOHaD) concept: Past, present, and future. The epigenome and developmental origins of health and disease (pp. 1–15). London: Elsevier. [DOI] [PubMed] [Google Scholar]
- Grote, N. K. , Bridge, J. A. , Gavin, A. R. , Melville, J. L. , Iyengar, S. , & Katon, W. J. (2010). A meta‐analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Archives of General Psychiatry, 67(10), 1012–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin, J. , Hamilton, B. , Osterman, M. , & Driscoll, A. (2019). Births: Final data for 2018. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Matthey, S. , Henshaw, C. , Elliott, S. , & Barnett, B. (2006). Variability in use of cut‐off scores and formats on the Edinburgh Postnatal Depression Scale: Implications for clinical and research practice. Archives of Women's Mental Health, 9(6), 309–315. [DOI] [PubMed] [Google Scholar]
- Pooler, J. , Perry, D. F. , & Ghandour, R. M. (2013). Prevalence and risk factors for postpartum depressive symptoms among women enrolled in WIC. Maternal and Child Health Journal, 17(10), 1969–1980. [DOI] [PubMed] [Google Scholar]
- Suarez, A. , Lahti, J. , Czamara, D. , Lahti‐Pulkkinen, M. , Knight, A. K. , Girchenko, P. , … Räikkönen, K. (2018). The epigenetic clock at birth: Associations with maternal antenatal depression and child psychiatric problems. J Am Acad Child Adolesc Psychiatry, 57(5), 321–328.e322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thayer, Z. , & Gildner, T. (In review). Reported information sharing and satisfaction with maternity care providers during the COVID‐19 pandemic: Associations with socioeconomic status and shifts to telehealth. Birth. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thayer, Z. M. , Wilson, M. A. , Kim, A. W. , & Jaeggi, A. V. (2018). Impact of prenatal stress on offspring glucocorticoid levels: A phylogenetic meta‐analysis across 14 vertebrate species. Scientific Reports, 8(1), 4942. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FIGURE S1: Supporting information


