Abstract
Purpose/objectives
The current coronavirus disease 19 (COVID‐19) pandemic has affected most countries. Infection, Prevention, and Control training is important in mitigating the spread of COVID‐19. The closure of universities by the Nigerian government has hampered academic activities of dental students. Our objectives were to assess the knowledge, perception, and attitude of undergraduate dental students in Nigeria to the COVID‐19 pandemic and infection control practices.
Methods
This was a cross‐sectional study of undergraduate clinical dental students from the dental schools in Nigeria. Self‐administered questionnaires were distributed to participants using an online data collection platform. Correct responses to the 45‐item questionnaire on COVID‐19 knowledge were scored to determine their knowledge level. A Likert scale of 1‐5 was used to assess the 13‐item perception and attitude questions. The level of significance was set at P values ≤ 0.05.
Results
A total of 102 undergraduate clinical dental students participated in the study. Males represented 54.9%, and mean age was 25.3 ± 2.4 years. Fifty percent of the students had adequate knowledge of COVID‐19. Final‐year students (58.1%) demonstrated more adequate knowledge of COVID‐19 than penultimate‐year students (28.6%, P = 0.008). Most (95.1%) respondents had positive attitudes towards infection control practices against COVID‐19.
Conclusion
Although the clinical dental students had a positive attitude to infection control practices against COVID‐19, the overall knowledge of COVID‐19 was barely adequate. Guidelines on COVID‐19 from reputable health authorities should be reviewed by dental school authorities and disseminated to the students to suit their clinical practice.
Keywords: attitude, COVID‐19, knowledge, Nigeria, undergraduate dental students
1. INTRODUCTION
The new coronavirus infection was first identified in a cluster of patients admitted into hospitals for suspected pneumonia of an unknown cause, later linked to a seafood and wet animal market in Wuhan city, Hubei Province, China, in December 2019. 1 This coronavirus has been identified as the severe acute respiratory syndrome coronavirus (SARS‐CoV‐2). 2 This infection was named the novel coronavirus disease 19 (COVID‐19) on February 11, 2020 by the WHO. 3 As the disease began to spread rapidly across several countries, the COVID‐19 outbreak was declared a global pandemic by the WHO on March 11, 2020. 4 Since the initial cases, COVID‐19 has affected more than 27 million people globally with over 880,000 deaths in about 216 countries and territories 3 as of September 7, 2020, thus posing a serious and alarming public health concern.
Since the index confirmed case in Nigeria on February 27th, 2020, the number of confirmed cases have risen to 55,160 with 1061 COVID‐19 related deaths, as of September 8, 2020. 5 The increase in the number of confirmed cases led the federal government of Nigeria (FGN) in March 2020 to effect the immediate closure of all educational institutions including universities, airports, land borders, and religious and recreational centers, amongst others, as major efforts to curb the spread of the infection. 5 The Nigeria Centre for Disease Control (NCDC) in partnership with the Ministry of Health and State governments has been actively involved in contact tracing, testing, isolation, and treatment of COVID‐19 cases in Nigeria. 5 Numerous campaigns have been embarked upon through the media for preventive measures such as hand hygiene, respiratory etiquette, social/physical distancing, noncontact temperature screening, and facemask wearing in public places to limit the spread of the disease.
The COVID‐19 pandemic has also affected dental training schools and dental clinics all over the world, with initial restrictions to emergency and urgent dental care. 6 , 7 , 8 The Nigerian Dental Association also issued some guidelines on COVID‐19 protocol for dental clinics in Nigeria to postpone elective procedures in April, 2020. 9 This is due to the reported high risk of infection amongst dental professionals as a result of the large amounts of aerosols generating procedures and their close proximity to patients in confined treatment offices/clinic. The coronavirus has also been found in the saliva of infected persons, 10 and shown to survive in aerosols for hours and on surfaces for days. 11
The closure of universities by the FGN in a bid to limit the spread of COVID‐19, has hampered the academic activities of dental schools and clinical training of dental students in Nigeria. The pandemic also affected the training activities of dental students in countries such as China 12 and Canada. 13 Dental students in China had to continue learning online after the Chinese Spring Festival and were told not to return to school until further notification at the onset of the pandemic. 12 Also in Canada, many third‐ and fourth‐year undergraduate dental students within a dental geriatric module in the University of British Columbia, Vancouver, were unable to participate in the clinical geriatric care activities due to the COVID‐19 pandemic. 13 The ongoing industrial strike action embarked by the Academic Staff Union of Universities in Nigeria has further worsened the situation as all forms of training in federal universities have been grossly affected. The impact on the effective training of dental students in Nigerian universities is likely to be severe, further worsened by the highly contagious nature of the COVID‐19 infection in clinic settings by the time dental schools in Nigeria reopen.
Previous studies among Nigerian dental students had highlighted the importance of feedbacks from students on the factors that affecting their training and how these could be overcome. 14 , 15 , 16 The COVID‐19 pandemic presents with a new range of challenges for undergraduate dental training, not only in Nigeria, but worldwide which include infection control practices in the clinic. Understanding these challenges will assist and guide dental faculties in assisting dental students through these very difficult times. The aim of this study was therefore to assess the knowledge, perception and attitude to the COVID‐19 pandemic and infection control practices among undergraduate clinical dental students in Nigeria.
2. MATERIALS AND METHODS
Ethical approval for this study was obtained from the Health Research Ethics Committee of the Lagos University Teaching Hospital. The Ethical approval number for the study is LUTHHREC/EREV/0420/12. This was a descriptive cross‐sectional study in which the study population was made up of undergraduate clinical dental students in their penultimate (Year 5) and final years (Year 6) from 9 out of the 12 accredited dental schools in Nigeria. The estimated population of undergraduate clinical dental students in Nigeria is 400, as they constitute a smaller segment of all undergraduate dental students in the country. The sample size of the participants for the study was determined to be 102 using a confidence level of 98% within a 10% margin of error. Informed consent was obtained from all respondents in the study. Self‐administered questionnaires were distributed and sent out repeatedly to participants using an online data collection platform (Google forms), between April 30 and June 6, 2020 using a purposive sampling technique. The respondents were accessed through their WhatsApp general dental students’ platform and direct WhatsApp messages. The questionnaire had 3 sections. Section 1 documented the participants’ sociodemographic characteristics while section 2 recorded participants’ knowledge of COVID‐19. Correct responses were assigned 1 point while incorrect answers were assigned 0. Forty‐five (n = 45) questions were used to assess the students’ knowledge of COVID‐19. The total knowledge score was derived based on the total sum of correct responses and converted to percentage scores. The level of knowledge of COVID‐19 was categorized into 2: adequate and inadequate, using a cut off value of 60% considering the fact that COVID‐19 is still a novel disease. The third section appraised their perception and attitude towards infection control practices in the dental clinic using 13 questions. Participants’ attitudes were assessed using a 5‐point Likert scale (1 = Strongly disagree; 2 = Disagree; 3 = Indifferent; 4 = Agree; 5 = Strongly Agree). All the scores were summed up and converted to percentages. The average percentage perception score was then computed. Scores ≥60% were graded as positive attitude towards infection control.
Data analysis was carried out using the Statistical Package for Social Sciences version 20. Descriptive statistics was used for categorical variables that were expressed as frequencies and percentages, while student's t test was used to compute the means and standard deviation of continuous variables such as the age. The 5 Likert scales were collapsed into 3 categories: Disagree (Scales 1,2), Neutral (Scale 3), and Agree (Scales 3,4) for purpose of the statistical analysis. Differences between categorical variables were compared using the chi‐square or Fisher's exact where indicated. The level of statistical significance was set at P ≤ 0.05.
3. RESULTS
A total of 102 undergraduate clinical dental students participated in the study. Males were slightly more (54.9%) than females (45.1%). The mean age of the respondents was 25.3 ± 2.4 years (range of 21–31 years). Majority (72.6%) of the respondents were in their final year. Students in 9 out of the 12 dental schools participated in the study and distribution is as follows: University of Lagos—35 (34.3%); Obafemi Awolowo University—20 (19.6%); University of Maiduguri—15 (14.7%); University of Nigeria Nsukka, Enugu—12 (11.7%); University of Benin—6 (5.9%); Lagos State University—5 (4.9%); University of Ibadan—5 (4.9%); University of Medical Sciences, Ondo—2 (2%); and Bayero University of Kano—2 (2%).
The mean overall knowledge score was 70.17 ± 10.0. Overall, 51(50%) demonstrated adequate knowledge of COVID‐19. A significant proportion of the respondents (78.4%) reported that they were up to date on the case definition for COVID‐19. Figure 1 shows the source of information about COVID‐19, which is the primary data collected among the respondents during the present study. Their source was mostly from the social media (99%), television (81.4%), friends/family (45.1%), colleagues (42.2%), and text message (39.2%), while the least source of information came from academic training courses (8.8%). The social media in this study included Twitter, Facebook, Instagram, YouTube, etc., while the text message was the short message service (SMS) through phone which was utilized mainly by the Nigerian Center for Disease Control (NCDC) to disseminate COVID‐19 related information. Academic training courses on COVID‐19 that were freely organized by health organizations/bodies, locally and internationally, were accessible to the respondents in this study through different online platforms.
FIGURE 1.
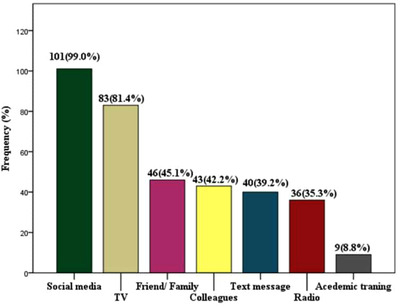
Sources of information about COVID‐19 among the respondents in the present study
Table 1 shows the responses of the respondents to the questions on COVID‐19. Nearly 60% of the students correctly identified SARS‐COV 2 virus as the cause of COVID‐19 while majority (95.1%) knew the average incubation period as 1–14 days. Only 30.4% of the respondents knew that mild to moderate symptoms occurred in 80% of those infected with COVID‐19, while 96.1% knew that asymptomatic people could spread the coronavirus. Transmission routes of COVID‐19 were reported as respiratory droplets from coughing, sneezing, and talking (99%), and airborne (52.9%). Some of the symptoms of COVID‐19 known by the respondents included shortness of breath (100%), cough (99%), fever (97.1%), loss of smell or taste (49%), joint/muscle pain (44.1%), chills (42.2%) and diarrhea (25.5%).
TABLE 1.
Responses to questions on the knowledge of COVID‐19
| Questions | Correct responses N (%) | Incorrect responses N (%) |
|---|---|---|
| Cause of COVID‐19 a virus called SARS‐COV 2 | 61 (59.8) | 41 (40.2) |
| Average incubation of COVID‐19 1–14 days | 97 (95.1) | 5 (4.9) |
| Proportion of people infected with mild‐moderate disease 80% | 31 (30.4) | 71 (69.6) |
| If asymptomatic people can spread the coronavirus Yes | 98 (96.1) | 4 (3.9) |
| Transmission routes of COVID‐19 | ||
| Respiratory droplets from coughing, sneezing, talking | 101 (99.0) | 1 (1.0) |
| Touching contaminated surfaces | 97 (95.1) | 5 (4.9) |
| Handshaking | 74 (72.5) | 28 (27.5) |
| Saliva | 62 (60.8) | 40 (39.2) |
| Airborne | 54 (52.9) | 48 (47.1) |
| Symptoms of COVD‐19 | ||
| Shortness of breath | 102 (100.0) | 0 (0.0) |
| Cough | 101 (99.0) | 1 (1.0) |
| Fever | 99 (97.1) | 3 (2.9) |
| Sore throat | 81 (79.4) | 21 (2.6) |
| Headache | 66 (64.7) | 36 (35.3) |
| Loss of smell or taste | 50 (49.0) | 52 (51.0) |
| Joint/muscle pain | 45 (44.1) | 57 (55.9) |
| Chills | 43 (42.2) | 59 (57.8) |
| Diarrhea | 26 (25.5) | 76 (74.5) |
| Sample collection methods of diagnosing COVID‐19 | ||
| Real‐time PCR with nasopharyngeal swab/sputum | 87 (85.3) | 15 (14.7) |
| Real‐time PCR with oropharyngeal swab/sputum | 60 (58.8) | 42 (41.2) |
| Real time PCR with endotracheal aspirate | 29 (28.4) | 73 (71.6) |
| Real time PCR with bronchoalveolar aspirate | 24 (23.5) | 78 (76.5) |
| Confirmed case definition for COVID‐19 | ||
| Laboratory confirmation of SARS‐COV‐2 virus | 17 (16.7) | 85 (83.3) |
| Treatments being investigated | ||
| Hydrochloroquine/chloroquine with azithromycin | 79 (77.5) | 23 (22.5) |
| Remdesivir | 70 (68.6) | 32 (31.4) |
| Ivermectin | 6 (5.9) | 96 (94.1) |
| Pluristem | 2 (2.0) | 100 (98.0) |
| Current availability of vaccine for COVID‐19 | 88 (86.3) | 14 (13.7) |
| People at higher risk of COVID‐19 | ||
| Healthcare workers | 98 (96.1) | 4 (3.9) |
| Elderly | 95 (93.1) | 7 (6.9) |
| Individual with underlying medical condition | 98 (96.1) | 4 (3.9) |
| Close relatives of COVID‐19 patients | 89 (87.3) | 13 (12.7) |
| Caregivers of COVID‐19 patients | 84 (82.4) | 18 (17.6) |
| Travelers | 79 (77.5) | 23 (22.5) |
| Smokers | 59 (57.8) | 43 (42.2) |
| Preventive strategies for COVID‐19 | ||
| Frequent use of alcohol‐based hand rub/sanitizer | 101 (99.0) | 0 (0.0) |
| Avoid touching of eyes, nose, and mouth | 101 (99.0) | 0 (0.0) |
| Frequent washing of hand with soap and water | 100 (98.0) | 2 (2.0) |
| Wearing of personal protective equipment by health worker | 100 (98.0) | 2 (2.0) |
| Wearing of facemask by all patients in dental clinic | 99 (97.1) | 3 (2.9 |
| Routine cleaning and disinfecting of surfaces | 98 (96.1) | 4 (3.9) |
| Social or Physical distance | 92 (90.2) | 10 (9.8) |
| Practice proper respiratory hygiene | 82 (80.4) | 20 (19.6) |
| Placing confirmed or suspected patients in adequately ventilated room | 76 (74.5) | 26 (25.5) |
| Minimum social distancing by WHO 1 m | 20 (19.6) | 82 (80.4) |
The sample collection methods to diagnose COVID‐19 was reported by 85.3% as real‐time PCR with nasopharyngeal swab/sputum and 23.5% as real time PCR with endotracheal aspirate. Only 16.7% of the respondents knew the confirmed case definition for COVID‐19. Hydroxychloroquine/chloroquine with azithromycin (77.5%) followed by remdesivir (68.6%) were the 2 most commonly known treatment options being investigated for treating COVID‐19. Over 86% knew there was currently no available vaccine for COVID‐19 while healthcare workers (96.1%) and individuals with underlying medical conditions (96.1%) were among those identified with a higher risk for COVID‐19. Preventive strategies for COVID‐19 such as the frequent use of alcohol‐based hand rub/sanitizer were reported by 99% of the respondents. The minimum social distance of 1 meter advocated by the WHO was known by only 19.6%.
The average perception/attitude score was 85.6 ± 10.4. Generally, most respondents (95.1%) had good perception/positive attitudes to infection control practices in preventing the spread of COVID‐19 in their clinics and training schools (Figure 2). Table 2 shows their perception/attitude towards infection control. Their responses included the perception that the current standard of infection control measures in their dental schools were effective in preventing the spread of COVID‐19 (24.5%). Majority (95.1%) agreed that aerosol‐generating procedures in dentistry carried a high risk of spreading COVID‐19. Regarding their attitude, 92.2% were willing to undergo an infection control training in dentistry for COVID‐19 while only 39.2% were willing to personally procure extra personal protective equipment (PPE) for use in the dental clinic to prevent the spread of COVID‐19.
FIGURE 2.
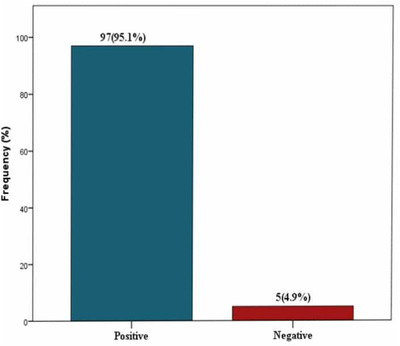
Overall attitude towards infection control practices against COVID‐19
TABLE 2.
Perception/attitude towards infection control practices against COVID‐19
| Perception | Disagree | Neutral | Agree |
|---|---|---|---|
| 1. Current standard of infection control measures in dental school are effective in preventing the spread of COVID‐19 | 52 (51.0) | 25 (25.5) | 25 (24.5) |
| 2. Aerosol generating procedures in dentistry carry a high risk of spreading COVID‐19 | 1 (1.0) | 4 (3.9) | 97 (95.1) |
| 3. Proper hand washing before and after seeing each patient with soap and water is very important in reducing the risk of COVID‐19 | 2 (2.0) | 3 (2.9) | 97 (95.1) |
| 4. All dental patients awaiting treatment should wear face covering/masks to reduce the risk of transmitting COVID‐19 to others | 2 (2.0) | 5 (4.9) | 95 (93.1) |
| 5. Changing face masks before and after treating each dental patient is more protective than wearing the same mask for different patients | 3 (2.9) | 5 (4.9) | 94 (92.2) |
| 6. COVID‐19 patients should be treated in a well‐ventilated room or in a negative pressure room | 5 (4.9) | 12 (11.8) | 85 (83.3) |
| Attitude | |||
| 7. Willing to undergo an infection control training in dentistry for COVID‐19 | 5 (4.9) | 3 (2.9) | 94 (92.2) |
| 8. Willing to personally procure extra PPE for use in the dental clinic to prevent the spread of COVID‐19 | 42 (41.2) | 30 (19.6) | 40 (39.2) |
| 9. Wearing my gloves, face masks, goggles, and face shield while performing dental procedure will adequately protect from contracting COVID‐19 in the clinic | 12 (11.8) | 14 (13.7) | 76 (74.5) |
| 10. Wearing clinical scrubs with protective footwear without my personal clothes when treating dental patients in the clinic gives better protection against COVID‐19 than wearing a clinical white coat on top of personal clothes | 12 (11.8) | 10 (9.8) | 80 (78.4) |
| 11. It is not advisable to wear the same cloth and footwear worn in the clinic to my home or residence | 9 (8.8) | 5 (4.9) | 88 (86.3) |
| 12. It is necessary to change and wash my clinical white coat after daily use | 3 (2.9) | 5 (4.9) | 94 (92.2) |
| 13. If patient is sneezing or coughing persistently in the dental clinic, I will stop the treatment and refer for COVID‐19 test | 4 (3.9) | 9 (8.8) | 89 (87.3) |
Table 3 shows the association between knowledge of COVID‐19 and sociodemographic characteristics, and perception/attitude towards infection control practices against COVID‐19. Only the year of study was significantly associated with the knowledge of COVID‐19, as the final‐year students (58.1%) demonstrated more adequate knowledge of COVID‐19 than the penultimate‐year students (28.6%) (P = 0.008).
TABLE 3.
Association between knowledge and socio‐demography, perception, and attitude towards infection control practices against COVID‐19
| Socio‐demography | Inadequate (n = 51) | Adequate (n = 51) | Total | X 2 | P‐value |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 24 (42.9) | 32 (57.1) | 56 (54.9) | 2.534 | 0.111 |
| Female | 27 (58.7) | 19 (41.3) | 46 (45.1) | ||
| Age group (years) | |||||
| ≤25 | 30 (52.6) | 27 (47.4) | 57 (55.9) | 0.358 | 0.550 |
| >25 | 21 (46.7) | 24 (53.3) | 45 (44.1) | ||
| Year of study | |||||
| Penultimate | 20 (71.4) | 8 (28.6) | 28 (24.5) | 7.089 | 0.008 a |
| Final | 31 (41.9) | 43 (58.1) | 74 (72.5) | ||
| Opinion on having up‐to‐date information on COVID‐19 case definition | |||||
| Yes | 39 (48.8) | 41 (51.2) | 80 (78.4) | 0.232 | 0.630 |
| No | 12 (54.5) | 10 (45.5) | 22 (21.6) | ||
| Formal training on infection control in dentistry | |||||
| Yes | 40 (47.1) | 45 (52.9) | 85 (83.3) | 1.765 | 0.184 |
| No | 11 (64.7) | 6 (35.5) | 17 (16.7) | ||
| Regular training on infection control in dentistry | |||||
| Yes | 18 (50.0) | 1 (50.0) | 13 (12.7) | 0.000 | 1.000 |
| No | 33 (50.0) | 33 (50.0) | 89 (87.3) | ||
| Formal training on infection control in dentistry for COVID‐19 | |||||
| Yes | 6 (46.2) | 7 (53.8) | 13 (12.7) | 0.088 | 0.767 |
| No | 45 (50.6) | 44 (49.4) | 89 (87.3) | ||
| Perception/attitude to infection control practices against COVID‐19 | |||||
| Positive | 49 (50.5) | 48 (49.5) | 97 (95.1) | 0.210 | 0.647 |
| Negative | 2 (40.0) | 3 (60.0) | 5 (4.9) | ||
Statistically significant.
4. DISCUSSION
The rapid surge in the number of cases during the COVID‐19 pandemic has placed enormous strain on health care systems and significantly impacted educational systems globally, including dental training institutions in health care settings of undergraduate dental students. There are currently about 12 accredited dental schools in Nigeria. Prior to the COVID‐19 pandemic, studies by Isiekwe et al. 14 , 15 , 16 among undergraduate dental students in Nigeria observed a lack of satisfaction with the quality of their clinical training. This study sought to provide an overview of dental students’ knowledge of COVID‐19 and attitude to infection control during this pandemic, which could serve as guidelines in preparation for school resumption and clinical training of the students.
The present study revealed that generally, only half of the students had adequate COVID‐19 related knowledge. On the contrary, majority had a positive attitude towards infection control practices for preventing COVID‐19 within the dental clinics. Considering the fact that majority (78.4%) of the students reported that they were up to date on the confirmed case definition of COVID‐19, it was surprising to find only 16.7% of the respondents knowing the correct confirmed case definition, while only half (50%) actually demonstrated overall good knowledge of COVID‐19. Our findings contrast with that of Yaling et al., 17 who reported a large proportion (82.3%) of university students in China with good knowledge of COVID‐19. A possible reason for the differences observed may be the fact that fewer questions were used in that survey (5 questions) 19 compared to our present survey which had many more questions on COVID‐19 (45 questions). It is thus most likely that more information was required from the students in the present study. Clinical dental students are expected to possess an in‐depth knowledge particularly due to their access to the social media and television which were their most frequent source of information in the present study. The proportion of respondents with adequate knowledge of the diagnosis, case definition, symptoms (like diarrhea, joint/muscle pain, loss of smell, chills, headache), and at‐risk persons was observed to be low. This could be ascribed to the novelty of the infection and the rapidly evolving information concerning its epidemiology.
In this study 97% of the participants knew the correct incubation period of COVID‐19, which is contrary to the findings of Khader et al., who reported that only 36.1% of dentists in Jordan knew the correct incubation period. 18 The news media in Nigeria has been flooded with regular and continuous information from the NCDC (Nigerian Centre for Disease Control) on the need for self‐isolation for a period of 14 days for people who developed specific symptoms such as cough, fever, and breathing difficulties. This would no doubt have increased the respondents’ awareness about these common symptoms, as the news media was bombarded by campaigns to identify these symptoms. Besides, the Jordanian study 18 was conducted at an earlier stage of the pandemic, which might have accounted for the disparity in knowledge level of the correct incubation period.
The majority of the dental students knew the early and common features of the infection; this finding is crucial as students should be able to easily identify a suspected case and take the necessary immediate action and respond appropriately. This was also the case in a Jordanian study amongst dentists. 18 The respondents in the present study indicated good knowledge of the preventive strategies for COVID‐19. However, it was surprising to observe that the minimum social/physical distance of 1 m (equivalent to 3 feet) recommended by the WHO 19 was unknown by the majority in the present study. A distance of at least 2 m (about 2 arms’ length) between people has also been advocated by other health authorities such as the U.S. Centers for Disease Control and Prevention. 20 It is important to maintain the recommended distance to prevent a person from inhaling droplets from someone with COVID‐19 who may be either asymptomatic or with symptoms of coughing, sneezing, or speaking.
Knowledge of bronchoalveolar and endotracheal aspirate for diagnosis was poor, however. This finding may be attributed to the most frequently used methods in this environment, which are oropharyngeal and nasopharyngeal swabs. Although nasopharyngeal swabs have typically been used to confirm clinical diagnosis of COVID‐19, a Chinese study found bronchoalveolar fluid to have the highest positivity (93%), followed by sputum (72%), nasal swabs (63%), pharyngeal swabs (32%). 21 The respondents’ knowledge of hydrochloroquine/azithromycin and remdisivir was particularly impressive compared to that of pluristem and ivermectin. This may be due to the several controversies that have been generated regarding the effectiveness of these drugs, especially the antimalarial drug chloroquine and its derivative hydroxychloroquine, which the WHO is testing in some clinical (solidarity) trials 22 in which Nigeria is participating.
The higher knowledge demonstrated by the final‐year compared to the penultimate‐year students could stem from a greater urge to learn more about the coronavirus and a deeper concern, eagerness, and anticipation amongst the final‐year students to complete their clinical procedures upon school resumption in order to write the qualifying exams. It would therefore not be unexpected by them to want to learn more about COVID‐19. These findings highlight the need to improve the knowledge span of undergraduate clinical dental students about COVID‐19 in order to mitigate its spread. This should be included in the curriculum for dental students all over the world.
The greater percentage (83.3%) of the students claimed to have had formal training on infection control while only 12.7% have had formal training on infection control in COVID‐19. This finding is not farfetched, as the lock down period might have prevented a more organized or structured training/teaching. The majority of the students (94.1%) in the present study had a good perception and positive attitude towards infection control practices, similar to Yaling et al.’s findings in China, where 73.8% of their subjects demonstrated positive attitudes. 17 This is crucial, as the current approach to COVID‐19 is to control the routes of infection and to conduct extensive infection prevention and control (IPC) trainings with preventive measures to lower the risk of transmission. 18 Surprisingly, knowledge did not influence the attitude of the students significantly in this study.
However, it was noted that there was a lack of will by most students to personally procure extra PPE to prevent the spread of COVID‐19, when they recommence their clinical procedures. These materials are currently scarce in the market and quite expensive too, and many students may lack the funds to procure them. Besides, there could be a notion that the school authorities are to provide these items. Undergraduate dental education in Nigeria is heavily subsidized by the government, with almost all the dental schools located in either federal or state government‐owned universities. Thus, students pay very minimal tuition, however, they are expected to purchase most of the bench items required for training. Furthermore, since the dental schools are dependent on the government for most of their funding, they often have restrictive finances due to limited funding from the government. The provision of PPE by the dental school may therefore be an additional financial burden; in this context, without additional help from the government, the dental schools may be constrained to ask the students to procure their own PPE for training.
This underscores the critical need by stakeholders to make appropriate PPE available for all undergraduate clinical dental students to curtail the spread of COVID‐19 particularly in resource restricted countries like Nigeria. Government and all stakeholders in the health and educational sectors must cooperate to fight this deadly scourge ravaging the whole world.
Majority of respondents (74.5%) agreed that wearing of face masks, gloves, goggles, and face shields while performing dental procedures will protect against COVID‐19. This observation is similar to effective infection control advocated in China by Meng et al. 12 It was encouraging to note that most of the respondents recognized that it was not advisable to wear the same clothing and footwear between the clinic and their hostels. Approximately 61% of respondents strongly agreed that wearing clinical scrubs with protective footwear without their personal clothes when treating patients or observing procedures in the clinic gives better protection against COVID‐19 than wearing clinical white coats on top of their personal home clothing. This is in keeping with standard infection protocols to avoid transmitting infections.
The role of health care worker's uniforms on the horizontal transmission of pathogens in hospital settings is controversial. 23 In the study by Munoz‐Price et al., 23 they found an association between the contamination of providers’ hands and contamination of white coats, yet they found no association between providers’ hands and scrubs although this was mainly attributed to the reduced frequency of laundering white coats than the scrubs. Prior to the pandemic, white clinical coats were worn over personal clothes by clinical dental students in Nigeria during school hours in the dental clinics. This may however not be appropriate nor sufficient particularly with the highly infectious nature of COVID‐19 and might change when the students resume to school. Advocating the wearing of clinical scrubs and foot wears was supported by most of the students in the present study. It would also equally important to emphasize the frequent laundering of the scrubs and foot wears. Of note is the significant proportion of students supporting the need to change and wash their clinical white coat after daily use.
Thus, it should be performed regularly and thoroughly as it is a simple but effective measure that dissolves the lipid coat surrounding the virus and kills or inactivates the virus if the hands have been contaminated. 12 , 19 , 24 In addition, in the present study, the perception held by many of the students was to pause the dental treatment of patients who start sneezing or coughing persistently in the dental clinic and refer them for further screening and possibly a COVID‐19 test. This is in tandem with the WHO policy that procedures which are likely to induce coughing should be avoided (if possible) or performed cautiously. 6 , 15 , 24
The importance of hand hygiene as one of the most critical factors for reducing the risk of transmission of COVID‐19 has been previously reported. 12 , 19 Thus, it should be performed regularly and thoroughly as it is a simple but effective measure that dissolves the lipid coat surrounding the virus and kills or inactivates the virus if the hands have been contaminated. 12 , 19
Concerning the dental management of COVID‐19 patients, 83.3% supported their treatment in a well‐ventilated room or in a negative pressure room. It is better and advised to encourage good air flow whilst ensuring physical distancing as much as possible. Meng et al., 12 proposed that based on their experience, relevant guidelines, and research, dentists are to take strict personal infection control measures that are effective and avoid or minimize operations that can produce droplets or aerosols. Four‐handed technique is considered beneficial for controlling infection coupled with the use of saliva ejectors with high volume to reduce the production of droplets and aerosols.
4.1. Limitations
The nonprobability sampling method employed in the study may be subject to selection bias as participants were approached via online platforms. Environmental factors in each dental school may have influenced the responses recorded as each dental school has its own peculiarities. Notwithstanding, this study has provided a national perspective on the knowledge and attitudes/perceptions of undergraduate clinical dental students towards the COVID‐19 pandemic and infection control practices in Nigeria.
5. CONCLUSION
This study determined that only half of the undergraduate clinical dental students had adequate general knowledge of COVID‐19. The students were not abreast of current updates on COVID‐19, particularly the confirmed case definition and less common symptoms. The students however had a good perception and positive attitude towards infection control practices against COVID‐19. Our recommendations are that guidelines from reputable health institutions/authorities on COVID‐19 be reviewed by the dental school authorities and included in the dental school curricula. The government should also make more PPE available for clinical dental students.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Umeizudike KA, Isiekwe IG, Fadeju AD, Akinboboye BO, Aladenika ET. Nigerian undergraduate dental students’ knowledge, perception, and attitude to COVID‐19 and infection control practices. J Dent Educ. 2021;85:187–196. 10.1002/jdd.12423
REFERENCES
- 1. Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol. 2020;92(4):401‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID‐19) outbreak. J Autoimmun. 2020;109:1024‐1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coronavirus disease (COVID‐19) Situation Report 129. World Health Organization web site. www.who.int/docs/default-source/coronaviruse/situation-reports/20200528-covid-19-sitrep-129.pdf?sfvrsn=5b154880_2. 2020. Accessed June 7, 2020.
- 4.Coronavirus disease (COVID‐19) Situation Report 51. World Health Organization web site. www.who.int/emergencies/diseases/novel-coronavirus-2019. 2020. Accessed March 11, 2020.
- 5.Updates on Coronavirus disease (COVID‐19). Nigeria Centre for Disease Control web site. www.covid19.ncdc.gov.ng/. 2020. Accessed August 19, 2020.
- 6.COVID‐19 Guidance for Dentistry. California Department of Public Health web site . https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/GuidanceforDentistry.aspx.
- 7.CDC Guidance for Providing Dental Care During COVID‐19.Centers for Disease Control and Prevention . https://www.cdc.gov/oralhealth/infectioncontrol/st
- 8.COVID‐19 latest guidance for Wales. General Dental Council web site. https://www.gdc‐uk.org/information‐standards‐guidance/covid‐19/covid‐19‐latest‐information/covid‐19‐latest‐guidance‐for‐wales. Last updates September 8, 2020. Accessed September 14, 2020.
- 9.NDA Recommendations On COVID‐19 Protocol for Dental Clinics. Nigerian Dental Association web site . https://nigdentalasso.org/about-us/. Accessed April 21, 2020.
- 10. Xu J, Li Y, Gan F, Du Y, Yao Y. Salivary glands: potential reservoirs for COVID‐19 asymptomatic infection. J Dent Res. 2020;99(8):989. [DOI] [PubMed] [Google Scholar]
- 11. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS‐CoV‐2 as compared with SARS‐CoV‐1. N Engl J Med. 2020;382(16):1564‐1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID‐19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99(5):481‐487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brondani M, Donnelly L. COVID‐19 pandemic: students’ perspectives on dental geriatric care and education. J Dent Educ. 2020:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Isiekwe GI, Umeizudike KA, Abah AA, Fadeju AD. Nigerian dental students’ perspectives about their clinical education. Unilag J Dent Sci. 2019;3(1):3‐7. [Google Scholar]
- 15. Isiekwe GI, Umeizudike KA, Abah AA, Fadeju AD. Undergraduate dental education in Nigeria: perceptions of dental students and recent dental graduates. Odontostomatol Trop. 2016;39(154):15‐23. [PubMed] [Google Scholar]
- 16. Isiekwe GI, Umeizudike KA, Abah AA, Olatosi OO. Perception of dental students and recent graduates of a Nigerian Dental School on the quality of undergraduate training received. Unilag J Med Sci Technol. 2015;3(1):34‐44. [Google Scholar]
- 17. Yaling P, Chenchen P, Yan Z, et al. Knowledge, attitude and practice associated with COVID‐19 among university students: a cross‐sectional survey in China. BMC Public Health. In review. [Google Scholar]
- 18. Khader Y, Al Nsour M, Al‐Batayneh OB, et al. Dentists' awareness, perception, and attitude regarding COVID‐19 and infection control: cross‐sectional study among Jordanian Dentists. JMIR Public Health Surveill. 2020;6(2):1e18798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Health Topics: Coronavirus [Internet]. World Health Organization (WHO) web site . https://www.who.int/health-topics/coronavirus#tab=tab_1 2020. Accessed June 2, 2020.
- 20.Coronavirus Disease 2019 (COVID‐19) Social Distancing, Quarantine, and Isolation. Centers for Disease Control and Prevention web site . www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html. 2020. Accessed May 28, 2020.
- 21. Wang W, Xu Y, Gao R, et al. Detection of SARS‐CoV‐2 in different types of clinical specimens. JAMA. 2020;323(18):1843‐1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Effectiveness of use of chloroquine/ hydroxychloroquine in COVID‐19 case management. 2020. World Health Organization web site. www.apps.who.int/iris/handle/10665/332261. 2020. Accessed May 22, 2020.
- 23. Munoz‐Price L, Arheart K, Lubarsky D, et al. Differential laundering practices of white coats and scrubs among health care professionals. Am J Infect Control. 2013;41(6):565‐567. [DOI] [PubMed] [Google Scholar]
- 24.Coronavirus disease (COVID‐19) Advice for public. www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. World Health Organization web site . Accessed June 3, 2020.


