Abstract
During the 2020 COVID‐19 pandemic, an outbreak occurred following attendance of a symptomatic index case at a weekly rehearsal on 10 March of the Skagit Valley Chorale (SVC). After that rehearsal, 53 members of the SVC among 61 in attendance were confirmed or strongly suspected to have contracted COVID‐19 and two died. Transmission by the aerosol route is likely; it appears unlikely that either fomite or ballistic droplet transmission could explain a substantial fraction of the cases. It is vital to identify features of cases such as this to better understand the factors that promote superspreading events. Based on a conditional assumption that transmission during this outbreak was dominated by inhalation of respiratory aerosol generated by one index case, we use the available evidence to infer the emission rate of aerosol infectious quanta. We explore how the risk of infection would vary with several influential factors: ventilation rate, duration of event, and deposition onto surfaces. The results indicate a best‐estimate emission rate of 970 ± 390 quanta/h. Infection risk would be reduced by a factor of two by increasing the aerosol loss rate to 5 h−1 and shortening the event duration from 2.5 to 1 h.
Keywords: aerosol transmission, infectious disease, pandemic, risk, ventilation, virus
Practical Implications.
During respiratory disease pandemics, group singing indoors should be carefully managed as singing can generate large amounts of aerosolized virus if any of the singers is infected.
Ventilation requirements for spaces that are used for singing (eg, buildings for religious services and rehearsal/performance) should be reconsidered in light of the potential for aerosol transmission of infectious diseases.
Systems that combine the functions heating and ventilation (or cooling and ventilation) should be accompanied with a disclaimer saying “do not shut this system off when people are using the room; turning off the system will also shut down outdoor air supply, which can lead to the spread of airborne infections.”
1. INTRODUCTION
SARS‐CoV‐2 was first reported in China at the end of 2019 and rapidly spread to the rest of the world over the subsequent months. Evidence from laboratory studies has shown that the SARS‐CoV‐2 virus can remain infectious while airborne for extended periods. 1 , 2 The virus has been detected by PCR in the air in several healthcare environments. 3 , 4 , 5 , 6 , 7 , 8 , 9 Researchers have reported values for the SARS‐CoV‐2 viral load in the mouth that span an extraordinarily broad range: from 102 to 1011 copies per mL of respiratory fluid. 10 , 11 , 12 Viral loads vary over the course of the disease, tending to peak near the onset of symptoms.
Aerosol transmission is now strongly suspected to play a significant role in superspreading events (SSEs) under certain conditions. SSEs occur when a large number of secondary transmissions are produced early in an outbreak and transmission is sustained in later stages. 13 Some people release respiratory aerosol at an order of magnitude greater rate than their peers and might contribute to superspreading events. 14 The very broad range of viral loads in respiratory fluids may also be an important factor influencing SSE. An infectious respiratory aerosol is a collection of pathogen‐laden particles in air emitted during respiring activities of an infected individual. 15
Conditions that promote outbreaks of COVID‐19 include large indoor gatherings and poor ventilation. An assessment of over 300 COVID‐19 outbreaks involving three or more people confirmed that all transmission could be linked to indoor environments. 16 A Japanese study based on contact tracing concluded that the odds that a primary case transmitted COVID‐19 in a closed environment was 18.7 times greater compared to an open‐air environment. 17 Another study from Japan concluded that the typical settings for superspreading events included “singing at karaoke parties, cheering at clubs, having conversations in bars, and exercising in gymnasiums.” 18 Poor ventilation has been a driving factor in other infectious disease outbreaks. Transmission of influenza from one index case to 72% of the onboard passengers occurred on an airplane that was grounded for three hours, during which the ventilation system was inoperative. 19
In this paper, we first discuss the outbreak and establish the likelihood of an important contribution from aerosol transmission. We then estimate the infectious quanta emission rate during a choir rehearsal that has been identified as a superspreading event. Quanta are used to represent infectious respiratory aerosol when the actual viral dose in the aerosol and the human dose‐response required to cause infection are unknown. 17 , 21 We then explore the sensitivity of the secondary attack rate of infection to the loss rate of aerosolized virus, whether by ventilation, deposition onto surface, or biological decay, as well as to duration of the event.
2. CASE STUDY
A SSE occurred in Skagit Valley, Washington, USA. 22 , 23 When the Skagit Valley Chorale (SVC) met on the evening of March 10, 2020, one person attending the rehearsal had cold‐like symptoms that had developed 3 days earlier; that individual subsequently tested positive for COVID‐19. This person is considered the “index case.” Within a few days of the news report, we contacted the journalist that reported on the event, the county health department, and a member of the choir. An initial questionnaire and multiple follow up questions were sent to the choir contact, and most of the choir members provided information on their activities. The responses are included in the Supplemental Information in the same form as provided to us, except for items removed due to privacy concerns. At the time of the rehearsal, the Skagit County Health Department was not recommending widespread closure of public venues or public events. They were recommending that those 60 years of age and older, or persons with underlying medical conditions, should avoid large public gatherings. Choral members were told to not attend on March 10 if they were sick with any kind of symptoms or if they had concerns.
The chorale met in the Fellowship Hall of a church in Mount Vernon, Skagit County. The day after the rehearsal on March 11, the governor of Washington recommended physical distancing and no large group meetings in three other nearby counties. At the time of the rehearsal, there were no known COVID‐19 cases in Skagit County, nor were any closures in effect. Before detecting the cluster on March 17, Skagit County had developed seven COVID‐19 cases. The likelihood of a second index case at the rehearsal can be estimated as 0.32%, from the seven other cases that had been reported in the county at the time in which the choir outbreak became known, given the population of the county, and an assumption of 50% asymptomatic cases. Asymptomatic cases were less likely than for an average population given that the choir members are more elderly than the general population; for example, 75.5% of those who became ill were 65 or more years old. 22
The SVC has 122 members, but only 61 attended rehearsal on March 10, amid concerns about COVID‐19 transmission. Precautions were taken during rehearsal, including the use of hand sanitizer, no hugging, and no handshakes. 23 All 120 chairs were arranged by 3 people who arrived early, and members sat in their usual chairs, which increased their distance compared to other well‐attended rehearsals. Lateral distance between chair centers (and thus nose/mouth distances) was ~0.75 m, while forward distance between rows was ~1.4 m.
Some members began experiencing illness from March 11 to March 22. The timing of these potential secondary infections is consistent with what is known about the temporal dynamics of virus shedding and serial interval for COVID‐19. 24 In particular three cases were identified the day after the rehearsal, according to the county report, 22 although the choir members are not aware of cases before March 12 (see Supplemental Information). Several published analyses of the incubation time of COVID‐19 include some probability of developing symptoms within 1 day of infection. 25 , 26 , 27 , 28 This would be more likely in the case of receiving a high viral dose, as would be expected in an event like this with such a high attack rate. It is also possible that there was more than one index case present at the rehearsal, and the impact of this possibility on our analyses is discussed below.
Among the 61 attendees at the rehearsal, 53 cases in total were subsequently identified including the index case, with 33 confirmed through positive COVID‐19 tests and 20 unconfirmed but probable secondary cases based on symptoms and timing. Testing was unavailable to many of the choir members (see Supplemental Information). Accounting for the one presumed index case, the secondary infection attack rate is thus in the range 32/60 to 52/60, or 53%‐87%.
The large number of infections arising from this event, compared to the low incidence in the county at the time, makes it unlikely that they were acquired at a different setting than the choir. This inference is consistent with the conclusion of the county health investigators, who interviewed all choir members and investigated other possible avenues for contact: transmission most likely occurred at the March 10th rehearsal. 22 It is also consistent with the opinion of the choir members (see Supplemental Information). Infection of many choir members at the prior March 3rd rehearsal is also very unlikely, as discussed by Hamner et al 22 Given a median incubation time of 4‐5 days, if multiple members had been infected at the March 3rd practice, 70%‐80% of them should have presented symptoms by the time of the March 10th practice. 27
A seating chart obtained through personal communication showed the layout of participants among 120 chairs plus the position of the choir director and piano accompanist. Although the chart cannot be reproduced because of privacy concerns, 22 a centrally important point for interpreting the cause of transmission is that the cases occurred throughout the room with no clear spatial pattern. Specifically, dividing the 120 seats into quadrants of 30 seats each, the occupancy levels (seats occupied/seats available) span a narrow range of 44%‐53%. The infection rate (reported infections/seats occupied) are substantial in each quadrant, with a low of 43% and being in the range 71%‐87% in the other three quadrants.
The rehearsal started at 6:30 PM The SVC rehearsed in a single group in the Fellowship Hall for 45 minutes, with the members in fixed positions in their usual seats, then split into two approximately equal‐sized groups for 45 minutes. One group, mostly male singers, went to practice in a different room of the church, where the singers sat in the church pews and the piano was off to the side. A second group stayed in the Fellowship Hall. The attack rate was higher in the group that stayed in the Fellowship Hall (see Supplemental Information), which is consistent with the presence of the index case in that room during the separate rehearsals. Transitions between the 3 phases of rehearsal were rapid (see Supplemental Information). After practicing separately, and following a 10‐minute break, the members reconvened in the Fellowship Hall for another 50 minutes, until 9 PM During the split session, those who remained in the Fellowship Hall occupied about half of the space, and thus had a similar person density as during the whole‐group rehearsal (see Supplemental Information).
Limited information is available about the heating and ventilating system; what was learned from personal communications is summarized here. The Fellowship Hall is heated and ventilated with a mechanical air heating system including an outdoor air intake and air recirculation. The air handling unit has a relatively new commercial forced‐air furnace (see Supplemental Information for the system capacity details). The furnace is installed with an outside make‐up air function and it also has a separate combustion air intake, which is standard for gas appliances. But it is not known how much outside make‐up air was supplied to the building that evening. The furnace is also outfitted with a MERV 11 filter, which has a rated single‐pass efficiency of ≥30%‐65% for aerosol particles of diameter 1 µm or larger. 29 , 30 Three supply air registers are situated 2.4 m above the floor on one wall with a single return on an adjacent wall, just above the floor (~0.15 m). Someone in the front office reportedly turned on the heating system prior to the rehearsal to warm the space, and the thermostat was set to 20°C (68 °F). It was about 7°C (45°F) outside, so the heating was on at the start of the rehearsal, but with so many people in the room, it did not need to stay on to maintain a comfortable temperature. During the entire rehearsal no exterior doors were open. It is not known whether the forced‐air furnace fan operated (only) under thermostatic control or whether it ran continuously.
3. EVIDENCE RELATED TO THE ROUTES OF TRANSMISSION
There are considered to be three primary routes of transmission for COVID‐19: (a) direct contact (eg, shaking hands) or indirect contact with contaminated objects (“fomites”), followed by touching one's eyes, nostrils, or mouth; (b) large ballistic droplets that travel directly from an infected person's nose or mouth to a susceptible person's eyes, nostrils, or mouth; (c) exhaled respiratory aerosols, which can linger in the air for minutes to hours, and may infect by inhalation.
There is no specific evidence that COVID‐19 is transmitted via the fomite route, 31 and the US CDC has stated that while possible, this route is considered less likely, 32 possibly because of rapid inactivation demonstrated for lipid‐enveloped viruses on human skin. 33 , 34 , 35 , 36 At the time of the chorale rehearsal on 10 March 2020, because of emerging concern about SARS‐CoV‐2, person‐to‐person contact and touching of surfaces was consciously limited, and hand sanitizer was used. No one reported direct physical contact between attendees to the County Public Health investigators. 22 Although some choir members helped arrange the chairs and ate snacks during the intermission, the index case did not participate in these activities, and many other members reported not eating the snacks. 22 Thus fomite transmission from the index case via chairs or snacks can be excluded. The index case used one of the bathrooms during the event and thus touched the door handle and other surfaces there, but only about six other choir members used that restroom (see Supplemental Information), and many choir members who did not use any of the restrooms were also infected. Indeed, the clustering of infected cases on the seating chart does not support transmission from a point surface contact(s) unless the people who sat together all touched the same contaminated surface. Thus, it appears highly improbable that the direct and indirect contact routes could account for a significant fraction of the transmission during this event.
There is no direct evidence of transmission by ballistic droplets for any disease in the literature. 37 The risk of widespread transmission owing to large ballistic droplets during close proximity situations would seem to be low in this event, considering that it is likely to have been only one index case, who was seated in close proximity to only a small proportion of the other chorale members. One half of the chairs were unoccupied, increasing the distance between members. No one was located within 3 meters in front of the index case (where respiratory droplets from the index case would be expected to have landed (see Supplemental Information) during either of the rehearsal periods. Two other members where located within 1 m to each side of the index case during parts of the rehearsal, while four other members were located within 2 m behind (and one 2 m to the side) of the index case during parts of the rehearsal. Ballistic droplets, propelled forward by exhaled breath, could not have traveled backwards in this low ventilation situation.
There was a single 10‐minute break (see Supplemental Information), during which the participants talked with each other, mostly in groups of 3‐4 people, while the index case conversed minimally with others throughout the rehearsal and the break (see Supplemental Information). Many members arrived shortly before and left immediately after the practice (see Ref. 19 and Supplemental Information). However, about 15 minutes of close proximity is thought to be needed for transmission. 32 Thus, it is physically not possible for the index case (or even several index cases) to have conversed with and impacted ballistic droplets onto 53 other members in such a short time.
Literature evidence suggests that singing could have been a contributing factor to the high secondary attack rate compared to other common indoor activities. The rate of aerosol emission during vocal activities increases with voice loudness. 14 A study of respiratory emissions also found higher emission rates of respiratory droplets to be associated with more extensive vocalization. 38 Outbreaks of tuberculosis, a disease known to be transmitted via inhalation, have been linked to singing. 39 , 40 , 41 At the time this article is being written, there have been additional media reports of COVID‐19 outbreaks associated with choirs. Cases with high secondary attack rates have been reported in the Netherlands, Austria, Canada, Germany, England, South Korea, Spain, and France. 42 , 43 , 44
Loudon and Roberts 45 characterized respiratory aerosol emitted during talking, singing, and coughing. They reported that “fewer droplets were expelled during singing than during talking, but a higher proportion of them were in the smaller size range. The percentage of droplets still airborne as droplet nuclei after a 30‐minute settling period were 35.7, 6.4, and 48.9 for singing, talking, and coughing, respectively.”
If transmission by fomites and/or ballistic droplets were the dominant modes of transmission, then the secondary attack rate should have been much smaller than the observed range of 53%‐87%. We would also expect to see the secondary cases predominantly among those in closer proximity to the index case rather than distributed throughout the rehearsal room. Even in the case that a second index case had been present, the same considerations make such wide transmission by the fomite and ballistic drop routes very unlikely to explain the observed very high attack rate. Per Occam's razor, this explanation seems most probable: that inhalation of infectious respiratory aerosol from “shared air” was the leading mode of transmission.
4. MODELING AEROSOL INFECTION RISK
This distinctive superspreading event, occurring in an enclosed community facility, with indoor space shared for a specified period of time, offers a good opportunity to examine a range of physical parameters that influence the eventual outcome. Our analysis was undertaken to explore whether this outbreak could have happened due to aerosol transmission and how future outbreaks could be avoided. In assuming only aerosol transmission what follows represents a worst‐case scenario for aerosol transmission, that is, highest possible quanta generation rate from the event. If a few cases arose from fomite or ballistic droplet routes, the quanta emission rate of the aerosol route would be proportionally lower.
There is no evidence to suggest that more than one person was infected and showing symptoms at the time of the rehearsal. Asymptomatic transmission, however, is important in the spread of COVID‐19. 24 Available evidence suggests that 50% of transmission happens while asymptomatic; it is, however, estimated that only 20% of cases remain asymptomatic. 47 , 48 , 49 Thus, it is possible that individuals at the rehearsal were asymptomatic transmitters; however, as described earlier, we estimate this probability to be very small because of the low community prevalence of COVID‐19 at the time of the rehearsal. Assuming that there is only one index case to account for all transmission and that all transmission was through aerosol is a conservative approach and provides a basis that can be used to develop precautionary mitigation approaches.
Hence, on the basis of the available information about this event, a modeling effort was undertaken with two goals. The first goal was to estimate an average quanta emission rate that is consistent with the evidence, while assuming that all transmission happens through exposure to aerosol from a single index case. This calculation proceeds in two steps: determining the average aerosol quanta concentration from the reported secondary infection attack rate, and then evaluating the emission rate that would have produced the inferred average concentration. The second modeling goal was to explore how a change in the loss rates, for example owing to improved ventilation and filtration, would have altered the infection risk. In pursuing both goals, the modeling effort uses an idealization of the more complex real situation, in part because some key data are lacking. A similar approach has been used in other studies to explore aerosol infection risk in indoor environments. 20 , 50
The model of infection risk due to aerosol transmission is based on the Wells‐Riley formulation, 46 , 51 as amended by Gammaitoni and Nucci. 52 In applying this approach, these assumptions are made: (a) there is one infectious individual who emits SARS‐CoV‐2 quanta at a constant rate throughout the event, (b) there is no prior source of quanta in the space, (c) the latent period of the disease is longer than the time scale of the event, (d) the infectious respiratory aerosol quickly becomes evenly distributed throughout the room air, and (e) infectious quanta are removed by first‐order processes reflecting the sum of ventilation, filtration, deposition, and airborne inactivation. The assumption that the indoor environment can be modeled as well‐mixed is substantiated in this case by the broad spatial distribution of secondary infections among the rehearsal participants. Additional information is provided in the Supplemental Information describing supporting evidence of the well‐mixed assumption. In epidemic modeling, where the aim is to assess the disease spread in the community, it is impossible to specify geometries, ventilation efficiency, and the locations of the infectious sources in each microenvironment. Therefore, adopting the well‐mixed assumption is generally more reasonable than hypothesizing about specific patterns of emissions, airflow and removal processes. 53
The modeled probability of infection (p) is related to the number of quanta inhaled (n) according to Equation (1) 53 :
| (1) |
Equation (1) is used to estimate the average quanta concentration during the practice, given estimates of the probability of infection based on the secondary attack rate. The aerosol quanta concentration increases with time from an initial value of zero following a “one minus exponential” form, which is the standard dynamic response of a well‐mixed indoor volume to a constant input source. The time‐average quanta concentration (C avg, q/m3) is the quanta inhaled divided by the volume of air breathed. The volume of air breathed (m3) is equal to the duration of the event (D, h) multiplied by the volumetric breathing rate of rehearsal participants (Q b, m3/h).
A well‐mixed material balance model for the room (Equation 2) is applied next to relate the quanta concentration, C (quanta/m3), to the emission rate, E (quanta/h):
| (2) |
Here V = volume of the rehearsal hall (m3) and λ = first‐order loss rate coefficient for quanta (h−1) due to the summed effects of ventilation (λv ), deposition onto surfaces (λdep ), and virus decay (k). 54 Assuming the quanta concentration is 0 at the beginning of the rehearsal, Equation (2) is solved and the average concentration determined as follows (Equation 3):
| (3) |
| (4) |
Here, t = time (h). Equation (4) is rearranged to solve for the emission rate, E:
| (5) |
A Monte Carlo simulation was run (N = 1000 iterations) to estimate E for the superspreading event given a range of input values. The unknown parameters (p, Q b, λv , λdep , k) were specified as probabilistic using uniform distributions bounded by specified upper and lower limits. These parameters were assumed to be uncorrelated. A sensitivity analysis was undertaken to explore how using different parametric distributions influenced the predictions. see Supplemental Information for details and results.
The ranges of the uncertain model parameter values explored in the primary Monte Carlo simulation are summarized in Table 1. Constant values were used for the volume of the Fellowship Hall and the rehearsal duration.
Table 1.
Parametric values used in the Monte Carlo simulation for estimating E
| Parameter | Value(s) | Distribution | Reference(s) |
|---|---|---|---|
| Probability of infection, p (%) | 53‐87 | Uniform | 22 |
| Volumetric breathing rate, Q b (m3/h) | 0.65‐1.38 | Uniform | 55, 56 |
| Loss rate due to ventilation, λv (h−1) | 0.3‐1.0 | Uniform | Supplemental Information |
| Loss rate due to deposition onto surfaces, λdep (h−1) | 0.3‐1.5 | Uniform | 57, 58 |
| Loss rate due to virus inactivation, k (h−1) | 0‐0.63 | Uniform | 1, 2 |
| Volume of rehearsal hall, V (m3) | 810 | Constant | Personal Communication |
| Duration of rehearsal, D (h) | 2.5 | Constant | 22 |
The lower breathing rate used in our simulations was from Binazzi et al 56 who reported volumetric inhalation rates of singers to be in the range 0.22‐1.0 m3/h. The upper breathing rate was from Adams et al 55 for light activity (walking female and male middle age adults). 50 SARS‐CoV‐2 was found in air samples in two size ranges: 0.5‐1 µm and >2.5 µm. 7 The surface deposition loss rate range was based on data from Thatcher et al 58 and Diapouli et al. 57 The range of values for virus decay is based on two sources: Fears et al 1 showed no decay in virus‐containing aerosol for 16 hours at 53% RH, whereas van Doremalen et al 2 estimated the half‐life of aerosol SARS‐CoV‐2 is 1.1 hours, which equates to a decay rate of 0.63 h−1. The loss rate due to ventilation is likely to have been in the range from 0.3 to 1 h−1 (see Supplemental Information). We did not include filtration in our estimation of the loss rate.
5. RESULTS
The mean (± SD) inferred emission rate was E = 970 (±390) quanta/h. Additional statistics for the distribution of E from the Monte Carlo simulation are as follows: geometric mean = 900 q/h; geometric standard deviation = 1.5; 10th, 25th, 50th, 75th and 90th percentiles: 550, 680, 910, 1180, 1510 q/h.
We reiterate that the emission rate was derived based on a base case assumption of one index case and all transmission by aerosol inhalation. It is plausible that more than one person attending the rehearsal was infectious. If this was the case then the inferred emission rate would represent the sum of emission rates from each of the infectious individuals. The analysis assumes that viral transmission all occurred through aerosol inhalation. If additional transmission routes played some role in this outbreak, then our the actual quanta emission rates would have been correspondingly lower.
Quanta emission rates for influenza have been reported to be in the range 15‐128 quanta/h 20 , 59 ; for measles: 5580 q/h 60 ; and for tuberculosis: 1.25‐30 840 q/h (the high value attributed to intubation). 61 The quanta for SARS transmission in a hospital and in an elementary school was estimated to be 28 q/h. 62 A forward model was used to estimate a large range of estimated quanta emission rates for SARS‐COV‐2, depending on activity level and respiratory activity: 10.5‐1030 quanta/h. 50
To explore the influence of changing the loss rate on the probability of infection, we performed sensitivity simulations in which we varied the loss rate. In these simulations, we used the mean emission rate of E = 970 q/h and a constant volumetric breathing rate of Q b = 1.0 m3/h. If λ is systematically increased by some combination of increased ventilation, deposition, filtration, and inactivation loss rates, how would the probability of infection decrease? We also explored what would happen if the emission rate was set at the 10th and 90th percentile values from the Monte Carlo simulation. Using the model equations above with λ ranging from 0.6 to 12 h−1, the percentage of the rehearsal participants infected is determined. The results are plotted in Figure 1.
Figure 1.
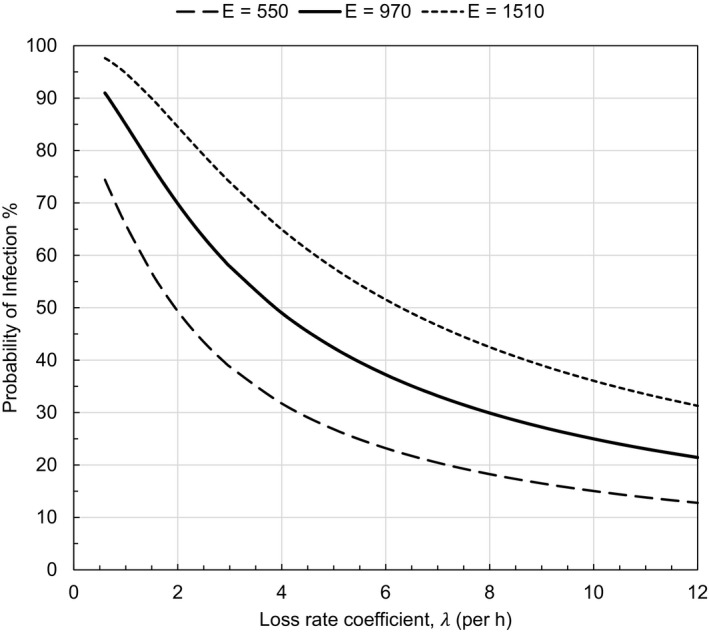
Probability of infection for each rehearsal participant as a function of loss rates for varying aerosol quanta emission rates (E, q/h). Infection probability is plotted for the predicted mean emission rate (970 q/h) and the 10th and 90th percentile emission rates (550 and 1510 q/h, respectively.) Constant values were assumed for rehearsal duration (2.5 h), indoor volume (810 m3) and volumetric breathing rate (1.0 m3/h)
A key point displayed in Figure 1 is that, for the mean value E = 970 q/h, increasing the loss rate coefficient from a nominal baseline value of 0.6 to 5 h−1 would reduce the probability of infection by a factor greater than two, from 91% to 42%. For the full range of loss rates plotted in Figure 1, the infection risks spans a factor of eight: from 98% to 13%.
We also explored how changing the duration of the event would impact the probability of infection as a function of loss rate. Again, we use the mean emission rate of 970 q/h and a volumetric breathing rate of 1.0 m3/h. For durations ranging from 0.5 to 2.5 hours, and total loss rates ranging from 0.6 to 12 h−1, the predicted percentage infected spanned a broad extent, from 4% to 91%. The results are plotted in Figure 2.
Figure 2.
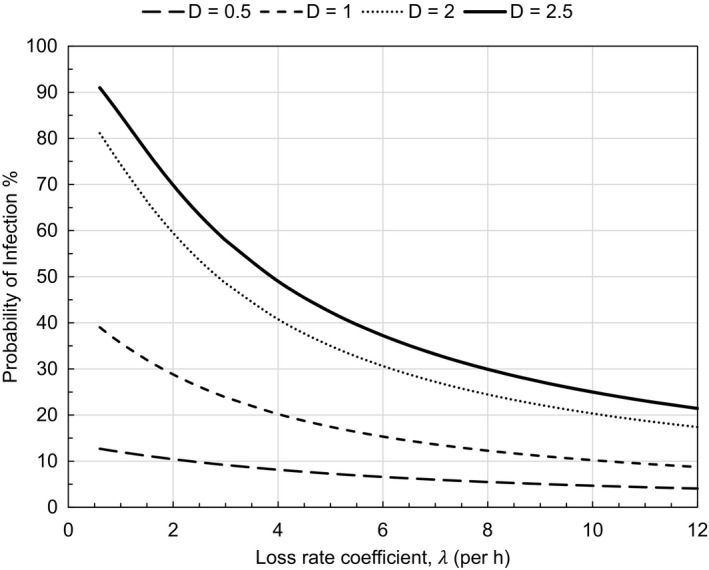
Probability of infection as a function of loss rates for varying event duration (D, h). A mean emission rate (970 q/h) and constant volumetric breathing rates of 1.0 m3/h were assumed
6. DISCUSSION
The inferred emission rate of 970 quanta/h is plausible given observations of SARS‐CoV‐2 in aerosol samples collected in hospitals and exhaled breath condensate collected from patients. Concentrations of viral RNA in patient rooms averaged 3000 ± 2700 gene copies/m3 across 18 measurements in Nebraska 9 and 2600 ± 1000 gene copies/m3 across two measurements in Singapore. 3 If the dominant removal mechanism was ventilation at an average rate of 13 h−1 in Nebraska and 12 h−1 in Singapore, then these concentrations correspond to emission rates of the order 106 gene copies/h from a patient. This emission rate matches the range measured directly in the exhaled breath condensate of patients. 63 Evidence suggests that ratio of gene copies to infectious virus is roughly 103, 64 , 65 so the emission rate of 106 gene copies/h would correspond to 103 infectious virions emitted per hour. This compares favorably to the quanta emission rate if the infectious dose is close to 1 plaque forming unit (PFU). We do not yet know the dose‐response relationship for SARS‐CoV‐2, but prior work indicates that the dose of SARS‐CoV corresponding to illness in 10% and 50% of those exposed is 43 and 280 PFU. 21 For influenza an inhaled dose as low as 0.7‐3.5 PFU is sufficient to cause seroconversion in 50% of subjects. 66
The emission rate can also be estimated by combining evidence on respiratory aerosol in exhaled breath with viral loads for SARS‐CoV‐2 in saliva. Concentrations of respiratory aerosol in exhaled breath that are smaller than 10 µm diameter are in the approximate range 1‐10 nL/m3 for vocalization activities. 38 For this concentration range, a volumetric breathing rate of 1 m3/h would produce an emission rate of 1‐10 nL/h of respiratory aerosol. In limited sampling of SARS‐CoV‐2 in saliva and other respiratory fluids, viral loads as high as 1011 gene copies/mL have been reported. 10 , 11 , 12 , 67 At 10 nL/h, a viral load in respiratory fluid of 1011 gene copies per mL (= 105 gene copies/nL) would lead to an emission rate of 106 gene copies/h, similar to the rate calculated above. Several factors contribute to substantial uncertainty in these comparisons including variability in viral shedding with type of respiratory activity, 68 , 69 viral load among infectious persons, 10 the dose‐response relationship, and other factors. However, the estimates do support the plausibility of the inferred quantum emission rate.
This modeling analysis has explored the very probable situation in which transmission by inhaling respiratory aerosol that was released during singing caused a large COVID‐19 outbreak. Accumulating evidence points to these factors being important for increasing the risk of aerosol transmission indoors: dense occupancy, long duration, loud vocalization, and poor ventilation.
In the domain of indoor environmental quality control, the first and best measure is generally to minimize indoor emissions. 70 Because it is not yet possible throughout communities to identify individuals who are highly infectious and therefore are potential superspreaders, effective source control can not be so well practiced, short of suspending large gatherings of high‐risk indoor events. Risks would be reduced if fewer people attended, if durations were shorter, and if attendees wore masks. The simulation results presented here show that the risk of secondary infections can be substantially reduced although not practically eliminated through a combination of increasing removal rates and by limiting the duration of indoor activities. The high ventilation rate in the hospital settings combined with other controls such as use of isolation rooms and effective personal protective equipment is likely to mitigate transmission from a high viral shedder in the healthcare environment. 3 , 9 In general community indoor spaces, which are not dedicated to infection prevention, controlling aerosol diseases transmission remains a great challenge during this pandemic. Ventilation rates corresponding to current standards would allow occupancy duration of only about 0.5 hours for an infection risk level below 10% for a such high emission activity as investigated here. Indoor environmental quality control measures available to improve conditions include enhanced ventilation, mechanical filtration, and germicidal ultraviolet disinfection. 71 , 72 Widespread application of effective indoor environment controls could help limit the extent of superspreading events and therefore contribute to slowing the pandemic spread.
CONFLICTS OF INTEREST
The authors of this paper certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent‐licensing arrangements), or non‐financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
AUTHOR CONTRIBUTION
Shelly L Miller: Conceptualization (equal); Data curation (equal); Formal analysis (equal); Investigation (equal); Methodology (equal); Project administration (equal); Validation (equal); Writing‐original draft (equal); Writing‐review & editing (equal). William W Nazaroff: Conceptualization (equal); Data curation (equal); Formal analysis (equal); Investigation (equal); Methodology (equal); Project administration (equal); Writing‐original draft (equal); Writing‐review & editing (equal). Jose L Jimenez: Conceptualization (equal); Data curation (equal); Investigation (equal); Methodology (equal); Writing‐original draft (equal); Writing‐review & editing (equal). Atze Boerstra: Data curation (equal); Writing‐original draft (supporting); Writing‐review & editing (supporting). Giorgio Buonanno: Conceptualization (supporting); Formal analysis (supporting); Methodology (supporting); Writing‐review & editing (equal). Stephanie Dancer: Conceptualization (supporting); Investigation (supporting); Writing‐original draft (supporting); Writing‐review & editing (supporting). Jarek Kurnitski: Conceptualization (equal); Formal analysis (supporting); Investigation (supporting); Methodology (supporting); Writing‐original draft (supporting); Writing‐review & editing (equal). Linsey Marr: Conceptualization (equal); Methodology (equal); Writing‐original draft (equal); Writing‐review & editing (equal). Lidia Morawska: Conceptualization (supporting); Methodology (supporting); Writing‐original draft (supporting); Writing‐review & editing (supporting). Catherine Noakes: Conceptualization (supporting); Methodology (supporting); Writing‐original draft (supporting); Writing‐review & editing (supporting).
Peer Review
The peer review history for this article is available at https://publons.com/publon/10.1111/ina.12751.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
We wholeheartedly thank Carolynn Comstock for acting as choir spokesperson, providing extensive information on the details of the outbreak, and answering many questions. We also thank the choir members for their extensive cooperation through the spokesperson, Richard Read of the Los Angeles Times for his rapid response to our inquiry and detailed discussions, and Lea Hamner and the rest of the Skagit County Public Health Dept for very useful information and discussions about the event.
Miller SL, Nazaroff WW, Jimenez JL, et al. Transmission of SARS‐CoV‐2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. Indoor Air.2021;31:314–323. 10.1111/ina.12751
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Fears AC, Klimstra WB, Duprex P, et al. Comparative dynamic aerosol efficiencies of three emergent coronaviruses and the unusual persistence of SARS‐CoV‐2 in aerosol suspensions. medRxiv. 2020. 10.1101/2020.04.13.20063784 [DOI] [Google Scholar]
- 2. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS‐CoV‐2 as compared with SARS‐CoV‐1. N Engl J Med. 2020;382:1564‐1567. 10.1056/NEJMc2004973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chia PY, Coleman KK, Tan YK, et al. Detection of air and surface contamination by SARS‐CoV‐2 in hospital rooms of infected patients. Nat Commun. 2020;11:2800. 10.1038/s41467-020-16670-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ding Z, Qian H, Xu B, et al. Toilets dominate environmental detection of SARS‐CoV‐2 virus in a hospital. medRxiv. 2020. 10.1101/2020.04.03.20052175 [DOI] [Google Scholar]
- 5. Guo Z‐D, Wang Z‐Y, Zhang S‐F, et al. Aerosol and surface distribution of Severe Acute Respiratory Syndrome Coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis. 2020;26:10‐3201. 10.3201/eid2607.200885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jiang Y, Wang H, Chen L, et al. Clinical data on hospital environmental hygiene monitoring and medical staffs protection during the coronavirus disease 2019 outbreak. medRxiv. 2020. 10.1101/2020.02.25.20028043 [DOI] [Google Scholar]
- 7. Liu Y, Ning Z, Chen Y, et al. Aerodynamic analysis of SARS‐CoV‐2 in two Wuhan hospitals. Nature. 2020;582(7813):557‐560. 10.1038/s41586-020-2271-3 [DOI] [PubMed] [Google Scholar]
- 8. Lednicky JA, Lauzardo M, Fan ZH, et al. Viable SARS‐CoV‐2 in the air of a hospital room with COVID‐19 patients. International Journal of Infectious Diseases. 2020:4608. 10.1016/j.ijid.2020.09.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Santarpia JL, Rivera DN, Herrera V, et al. Transmission potential of SARS‐CoV‐2 in viral shedding observed at the University of Nebraska Medical Center. medRxiv. 2020. 10.1101/2020.03.23.20039446 [DOI] [Google Scholar]
- 10. Pan Y, Zhang D, Yang P, Poon LLM, Wang Q. Viral load of SARS‐CoV‐2 in clinical samples. Lancet Infect Dis. 2020;20:411‐412. 10.1016/S1473-3099(20)30113-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. To KK‐W, Tsang OT‐Y, Leung W‐S, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS‐CoV‐2: an observational cohort study. Lancet Infect Dis. 2020;20():565‐574. 10.1016/S1473-3099(20)30196-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID‐2019. Nature. 2020;581:465–469. 10.1101/2020.03.05.20030502 [DOI] [PubMed] [Google Scholar]
- 13. Frieden TR, Lee CT. Identifying and interrupting superspreading events—implications for control of Severe Acute Respiratory Syndrome Coronavirus 2. Emerg Infect Dis. 2020;26:1061‐1066. 10.3201/eid2606.200495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Asadi S, Wexler AS, Cappa CD, Barreda S, Bouvier NM, Ristenpart WD. Aerosol emission and superemission during human speech increase with voice loudness. Sci Rep. 2019;9:2348. 10.1038/s41598-019-38808-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jones RM, Brosseau LM. Aerosol transmission of infectious disease. J Occup Environ Med. 2015;57:501‐508. 10.1097/JOM.0000000000000448 [DOI] [PubMed] [Google Scholar]
- 16. Qian H, Miao T, Liu L, Zheng X, Luo D, and Li Y. Indoor transmission of SARS‐CoV‐2. medRxiv. 2020. 10.1101/2020.04.04.20053058 [DOI] [PubMed] [Google Scholar]
- 17. Nishiura H, Oshitani H, Kobayashi T, et al. Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID‐19). medRxiv. 2020. 10.1101/2020.02.28.20029272 [DOI] [Google Scholar]
- 18. Furuse Y, Sando E, Tsuchiya N, et al. Clusters of coronavirus disease in communities, Japan, January–April 2020. Emerg Infect Dis. 2020;26:2176‐2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Moser MR, Bender TR, Margolis HS, Noble GR, Kendal AP, Ritter DG. An outbreak of influenza aboard a commercial airliner. Am J Epidemiol. 1979;110(1):1‐6. 10.1093/oxfordjournals.aje.a112781 [DOI] [PubMed] [Google Scholar]
- 20. Rudnick SN, Milton DK. Risk of indoor airborne infection transmission estimated from carbon dioxide concentration. Indoor Air. 2003;13:237‐245. 10.1034/j.1600-0668.2003.00189.x [DOI] [PubMed] [Google Scholar]
- 21. Watanabe T, Bartrand TA, Weir MH, Omura T, Haas CN. Development of a dose‐response model for SARS coronavirus. Risk Anal. 2010;30:1129‐1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hamner L, Dubbel P, Capron I, et al. High SARS‐CoV‐2 attack rate following exposure at a choir practice — Skagit County, Washington, March 2020. Morbidity and Mortality Weekly Report. 2020;69. 10.15585/mmwr.mm6919e6 [DOI] [PubMed]
- 23. Read R. A choir decided to go ahead with rehearsal. Now dozens of members have COVID‐19 and two are dead. Los Angeles Times, 29 March 2020. https://www.latimes.com/world‐nation/story/2020‐03‐29/coronavirus‐choir‐outbreak. Accessed May 7, 2020. [Google Scholar]
- 24. He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID‐19. Nat Med. 2020;26:672‐675. [DOI] [PubMed] [Google Scholar]
- 25. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID‐19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577‐582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhao Q, Ju N, Bacallado S, Shah RD.BETS: the dangers of selection bias in early analyses of the coronavirus disease (COVID‐19) pandemic. arXiv:2004.07743 2020.
- 27. Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019‐nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Euro Surveill. 2020;25(5):2000062. 10.2807/1560-7917.ES.2020.25.5.2000062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus‐infected pneumonia. N Engl J Med. 2020;382:1199‐1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. ASHRAE . ANSI/ASHRAE Standard 52.2‐2017 Method of Testing General Ventilation Air‐Cleaning Devices for Removal Efficiency by Particle Size. Atlanta, GA: American Society of Heating, Refrigerating and Air Conditioning Engineers Inc.; 2017. [Google Scholar]
- 30. Fazli T, Zeng Y, Stephens B. Fine and ultrafine particle removal efficiency of new residential HVAC filters. Indoor Air. 2019;29:656‐669. [DOI] [PubMed] [Google Scholar]
- 31. WHO . Scientific Brief. Transmission of SARS‐CoV‐2: implications for infection prevention precautions. 2020. https://www.who.int/publications/i/item/modes‐of‐transmission‐of‐virus‐causing‐covid‐19‐implications‐for‐ipc‐precaution‐recommendations. Accessed 28 August 2020.
- 32. Centers for Disease Control and Prevention . How COVID‐19 spreads. Updated June 16, 2020. https://www.cdc.gov/coronavirus/2019‐ncov/prevent‐getting‐sick/how‐covid‐spreads.html. Accessed 28 August 2020.
- 33. Bean B, Moore BM, Sterner B, Peterson LR, Gerding DN, Balfour HH Jr. Survival of influenza viruses on environmental surfaces. J Infect Dis. 1982;146(1):47‐51. 10.1093/infdis/146.1.47 [DOI] [PubMed] [Google Scholar]
- 34. Thomas Y, Boquete‐Suter P, Koch D, Pittet D, Kaiser L. Survival of influenza virus on human fingers. Clin Microbiol Infect. 2014;20:O58‐O64. [DOI] [PubMed] [Google Scholar]
- 35. Boone SA, Gerba CP. Significance of fomites in the spread of respiratory and enteric viral disease. Appl Environ Microbiol. 2007;73:1687‐1696. 10.1128/AEM.02051-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Grayson ML, Melvani S, Druce J, et al. Efficacy of soap and water and alcohol‐based hand‐rub preparations against live H1N1 influenza virus on the hands of human volunteers. Clin Infect Dis. 2009;48:285‐291. 10.1086/595845 [DOI] [PubMed] [Google Scholar]
- 37. Chen W, Zhang N, Wei J, Yen H‐L, Li Y. Short‐range airborne route dominates exposure of respiratory infection during close contact. Build Environ. 2020;176:106859. 10.1016/j.buildenv.2020.106859 [DOI] [Google Scholar]
- 38. Morawska L, Johnson GR, Ristovski ZD, et al. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. J Aerosol Sci. 2009;40:256‐269. [Google Scholar]
- 39. Bates JH, Potts WE, Lewis M. Epidemiology of primary tuberculosis in an industrial school. N Engl J Med. 1965;272:714‐717. [DOI] [PubMed] [Google Scholar]
- 40. Mangura BT, Napolitano EC, Passannante MR, McDonald RJ, Reichman LB Mycobacterium tuberculosis miniepidemic in a church gospel choir. Chest. 1998;113:234‐237. [DOI] [PubMed] [Google Scholar]
- 41. Washko R, Robinson E, Fehrs LJ, Frieden TR. Tuberculosis transmission in a high school choir. J Sch Health. 1998;6:256‐259. [DOI] [PubMed] [Google Scholar]
- 42. Read R. Scientists to choirs: Group singing can spread the coronavirus, despite what CDC may say. Los Angeles Times, 01 June 2020. https://www.latimes.com/world‐nation/story/2020‐06‐01/coronavirus‐choir‐singing‐cdc‐warning. Accessed 08 June 2020. [Google Scholar]
- 43. Peinado F, Ferrero B. El virus se ceba con las voces del coro de la Zarzuela. El Pais, 01 June 2020. https://elpais.com/espana/madrid/2020‐06‐02/el‐virus‐se‐ceba‐con‐las‐voces‐del‐coro‐de‐la‐zarzuela.html. Accessed 06 June 2020. [Google Scholar]
- 44. Charlotte N. High rate of SARS‐CoV‐2 transmission due to choir practice in France at the beginning of the COVID‐19 pandemic. medRxiv. 2020. 10.1101/2020.07.19.20145326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Loudon RG, Roberts RM. Singing and the dissemination of tuberculosis. Am Rev Respir Dis. 1968;98:297‐300. [DOI] [PubMed] [Google Scholar]
- 46. Noakes CJ, Sleigh PA. Mathematical models for assessing the role of airflow on the risk of airborne infection in hospital wards. J R Soc Interface. 2009;6:S791‐S800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lee S, Kim T, Lee E, et al. Clinical course and molecular viral shedding among asymptomatic and symptomatic patients with SARS‐CoV‐2 infection in a Community Treatment Center in the Republic of Korea. JAMA Intern Med.aaa 2020. 10.1001/jamainternmed.2020.3862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Buitrago‐Garcia DC, Egli‐Gany D, Counotte MJ, et al. Occurrence and transmission potential of asymptomatic and presymptomatic SARS‐CoV‐2 infections: A living systematic review and meta‐analysis. PLoS Med.. 2020;17(9):e1003346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS‐CoV‐2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382:2081‐2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Buonanno G, Stabile L, Morawska L. Estimation of airborne viral emission: quanta emission rate of SARS‐CoV‐2 for infection risk assessment. Environ Int. 2020;141:105794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Nicas M, Nazaroff WW, Hubbard A. Toward understanding the risk of secondary airborne infection: emission of respirable pathogens. J Occup Environ Hyg. 2005;2:143‐154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gammaitoni L, Nucci MC. Using a mathematical model to evaluate the efficacy of TB control measures. Emerg Infect Dis. 1997;3:335‐342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sze To GN, Chao CYH. Review and comparison between the Wells‐Riley and dose‐response approaches to risk assessment of infectious respiratory diseases. Indoor Air. 2010;20:2‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Yang W, Marr LC. Dynamics of airborne influenza A viruses indoors and dependence on humidity. PLoS One. 2011;6:e21481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Adams WC.Measurement of breathing rate and volume in routinely performed daily activities. Final Report, Contract No. A033–205. California Air Resources Board, Sacramento, CA. 1993. [Google Scholar]
- 56. Binazzi B, Lanini B, Bianchi R, et al. Breathing pattern and kinematics in normal subjects during speech, singing and loud whispering. Acta Physiol. 2006;186:233‐246. [DOI] [PubMed] [Google Scholar]
- 57. Diapouli E, Chaloulakou A, Koutrakis P. Estimating the concentration of indoor particles of outdoor origin: a review. J Air Waste Manag Assoc. 2013;63:1113‐1129. [DOI] [PubMed] [Google Scholar]
- 58. Thatcher TL, Lai ACK, Moreno‐Jackson R, Sextro RG, Nazaroff WW. Effects of room furnishings and air speed on particle deposition rates indoors. Atmos Environ. 2002;36:1811‐1819. [Google Scholar]
- 59. Knibbs LD, Morawska L, Bell SC. The risk of airborne influenza transmission in passenger cars. Epidemiol Infect. 2012;140:474‐478. [DOI] [PubMed] [Google Scholar]
- 60. Riley EC, Murphy G, Riley RL. Airborne spread of measles in a suburban elementary school. Am J Epidemiol. 1978;107:421‐432. [DOI] [PubMed] [Google Scholar]
- 61. Beggs CB, Noakes CJ, Sleigh PA, Fletcher LA, Siddiqi K. The transmission of tuberculosis in confined spaces: an analytical review of alternative epidemiological models. Int J Tuberc Lung Dis. 2003;7(11):1015‐1026. [PubMed] [Google Scholar]
- 62. Liao C‐M, Chang C‐F, Liang H‐M. A probabilistic transmission dynamic model to assess indoor airborne infection risks. Risk Anal. 2005;25:1097‐1107. [DOI] [PubMed] [Google Scholar]
- 63. Ma J, Qi X, Chen H, et al. Exhaled breath is a significant source of SARS‐CoV‐2 emission. medRxiv. 2020. 10.1101/2020.05.31.20115154 [DOI] [Google Scholar]
- 64. Bordi L, Piralla A, Lalle E, et al. Rapid and sensitive detection of SARS‐CoV‐2 RNA using the Simplexa™ COVID‐19 direct assay. J Clin Virol. 2020;128:104416. 10.1016/j.jcv.2020.104416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Corman VM, Eckerle I, Bleicker T, et al. Detection of a novel human coronavirus by real‐time reverse‐transcription polymerase chain reaction. Euro Surveill. 2012;17(39):20285. 10.2807/ese.17.39.20285-en [DOI] [PubMed] [Google Scholar]
- 66. Alford RH, Kasel JA, Gerone PJ, Knight V. Human influenza resulting from aerosol inhalation. Exp Biol Med. 1966;122(3):800‐804. 10.3181/00379727-122-31255 [DOI] [PubMed] [Google Scholar]
- 67. Jones TC, Mühlemann B, Veith T, et al. An analysis of SARS‐CoV‐2 viral load by patient age. medRxiv. 2020. 10.1101/2020.06.08.20125484 [DOI] [Google Scholar]
- 68. Yan J, Grantham M, Pantelic J, et al. Infectious virus in exhaled breath of symptomatic seasonal influenza cases from a college community. Proc Natl Acad Sci USA. 2018;115:1081‐1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Lindsley WG, Blachere FM, Beezhold DH, et al. Viable influenza A virus in airborne particles expelled during coughs versus exhalations. Influenza Other Respir Viruses. 2016;10:404‐413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Nazaroff WW. Four principles for achieving good indoor air quality. Indoor Air. 2013;23:353‐356. [DOI] [PubMed] [Google Scholar]
- 71. Nardell EA, Nathavitharana RR. Airborne spread of SARS‐CoV‐2 and a potential role for air disinfection. JAMA. 2020;324(2):141–142. 10.1001/jama.2020.7603 [DOI] [PubMed] [Google Scholar]
- 72. Morawska L, Tang JW, Bahnfleth W, et al. How can airborne transmission of COVID‐19 indoors be minimised? Environ Int. 2020;142:105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


