Abstract
Increased use of azithromycin (AZ) in treating infections associated with coronavirus disease 2019 (COVID‐19) and reports of increased incidence of prolonged corrected QT (QTc) interval associated with AZ used with hydroxychloroquine prompted us to review the latest evidence in the literature, present additional analyses of human cardiovascular (CV) electrophysiology studies, and to describe sequential steps in research and development that were undertaken to characterize the benefit‐risk profile of AZ. Combined QTc findings from electrocardiograms taken during oral and i.v. pharmacokinetic‐pharmacodynamic studies of AZ suggest that clinically meaningful QTc prolongation is unlikely. Findings from several observational studies were heterogeneous and not as consistent as results from at least two large randomized controlled trials (RCTs). The QTc findings presented and observational data from studies with large numbers of events are not consistent with either a proarrhythmic action of AZ or an increase in frequency of CV deaths. Well‐powered RCTs do not suggest a presence of increased risk of CV or sudden cardiac death after short‐term or protracted periods of AZ usage, even in patients at higher risk from pre‐existing coronary disease.
The antibiotic azithromycin (AZ) is the mainstay of a multinational program using Surgery, Antibiotics, Facial cleanliness, Environmental improvements (the SAFE strategy) to eliminate the leading cause of infectious blindness globally, blinding trachoma due to Chlamydia trachomatis. 1 A majority of Pfizer‐manufactured AZ is used therapeutically in Sub‐Saharan Africa in community treatment of adults and children for disease elimination programs or in research to study survival in younger children. 2
Based on an observational study from an administrative database linked to death certificates that contained small numbers of cardiac events, 3 increased deaths (50/million) were reported during days 1–5 of dosing in AZ recipients. The authors concluded the deaths were due to the proarrhythmic effects of AZ. Several letters responded to the paper and one 4 highlighted the paucity of data to support a proarrhythmic mechanism for AZ because of its known modest inhibitory effects on potassium channels that induce repolarization (IKr, Ito), 5 studies in animal models that did not find any proarrhythmic activity, and the findings from two large randomized clinical trials (RCTs) that demonstrated no increase in cardiovascular (CV) events in patients with coronary disease who might be predisposed to ischemia or arrhythmia.
Recently, there have been reports of the use of AZ in treating infections associated with coronavirus disease 2019 (COVID‐19), as well as reports of prolonged corrected QT (QTc) interval associated with AZ used with hydroxychloroquine (HCQ). 6 , 7 , 8 , 9 This paper reviews the latest evidence in the literature, 10 additional analyses of human CV electrophysiology studies, and highlights of expert advice obtained to provide further insights on the CV risk of AZ.
STUDIES TO INFORM THE POTENTIAL FOR QTc PROLONGATION PRIOR TO STARTING THE MALARIA PROGRAM
In vitro malaria studies with the Trager and Jensen method 11 and clinical studies were performed to assess the ability of AZ to work synergistically with other malaria therapeutics. 12 , 13 Potential safety risks were also studied in preclinical models. It is important to acknowledge the limitations of the early studies and recognize that they are a first step in understanding the arrhythmogenic potential of a molecule. In these studies, AZ was a weak inhibitor of cloned human ether‐a‐go‐go‐related gene (hERG) and lacked proarrhythmic activity when studied at supratherapeutic concentrations in animal models. 14 , 15 Next, and prior to conducting field malaria clinical studies, electrophysiology studies in humans were performed to assess the effects on QTc prolongation of chloroquine (CQ) alone as well as CQ with AZ.
A single‐center open‐label, placebo‐controlled, randomized, multiple‐dose healthy volunteer (N = 119) study randomized subjects to one of five treatment groups, as outlined in Figure S1 . In all analyses, the mean of the electrocardiogram (ECG) parameters within a triplicate was used as the observation for each subject at each nominal timepoint. The primary end point was change of QTc from baseline at each nominal time point on day 3, using Fridericia’s method (∆QTcF) to correct for heart rate effects on the QT interval. Comparisons were made between treatments vs. placebo and vs. the CQ group, using an analysis of variance (ANOVA) model. Mean ∆QTcF time profiles on day 3 are shown in Figure S2 .
In comparison to ∆QTcF values in placebo‐treated subjects, CQ increased mean time‐matched ∆QTcF, with the maximum difference generally occurring at 10 hours postdose on day 3 (Table 1 ). Maximum observed plasma CQ concentrations on day 3 were similar for all groups. AZ + CQ was also associated with increases in ∆QTcF values. Because of the differences in the time course of AZ‐associated and CQ‐associated effects on ∆QTcF, maximum changes in ∆QTcF vs. placebo were similar among all nonplacebo regimens. AZ exposure increased proportionally with increasing dose, and time to maximum concentration (Tmax) values did not change with dose.
Table 1.
Observed and predicted ∆QTcF and pharmacokinetic parameter values on day 3 following daily oral administration of CQ or CQ + AZ to healthy subjects
| Group | Vs. Placebo | Vs. CQ | CQ | AZ | Predicted maximum ∆QTcF effect due to AZ, msec | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Maximum ∆QTcF, msec | Time of maximum ∆QTcF, hours | Maximum ∆QTcF, msec | Time of maximum ∆QTcF, hours | Cmax, µg/mL | Tmax, hours | Cmax, µg/mL | Tmax, hours | Predicted effects at AZ Cmax using p.o. studya | Predicted effects at AZ Cmax using i.v. studyb | |
| (90% CI) | (90% CI) | (%CV) | (%CV) | (%CV) | (%CV) | |||||
| CQ | 35.0 | 10 | – | – | 0.314 | 7.65 | – | – | – | – |
| (29.9–40.2) | (28) | (39) | ||||||||
| CQ + 500 mg AZ | 36.2 | 10 | 5.31 | 2 | 0.356 | 6.44 | 0.53 | 1.44 | 3.78 | 0.72 |
| (31.0–41.6) | (0.19–10.4) | (35) | (47) | (33) | (38) | |||||
| CQ + 1000 mg AZ | 36.9 | 10 | 6.51 | 1 | 0.336 | 6.20 | 0.957 | 1.32 | 6.83 | 1.30 |
| (31.7–42.0) | (1.38–11.6) | (27) | (58) | (31) | (29) | |||||
| CQ + 1500 mg AZ | 35.0 | 6 | 8.88 | 2 | 0.334 | 6.27 | 1.54 | 1.35 | 11.00 | 2.09 |
| (29.7–40.4) | (3.56–14.2) | (22) | (68) | (28) | (30) | |||||
∆QTcF, Fridericia corrected QT interval; AZ, azithromycin; CI, confidence interval; Cmax, maximum plasma concentration; CQ, chloroquine; %CV, coefficient of variation in percent; Tmax, time to maximum plasma concentration.
Azithromycin plus chloroquine p.o. study analysis.
Azithromycin i.v. study analysis.
A model to examine possible effects of AZ concentration, CQ concentration, and sex on observed QTcF intervals was judged inadequate as predicted values were less than observed values at all but the earliest timepoints. Alternatively, a post hoc analysis estimated the effect of AZ on ∆QTcF in the presence of CQ (Figure 1 , left panel). The estimated effect due to AZ was a 7.14 msec (90% confidence interval (CI): 4.54, 9.74) change in QTcF per µg/mL AZ. Predicted maximum ΔQTc values are shown in Table 1 . This model assumed that differences were due directly to AZ concentration. AZ is a weak inhibitor of CYP3A4; thus, this analysis potentially overestimated AZ’s effect on QT if AZ altered a CQ metabolite that also increased QTcF.
Figure 1.
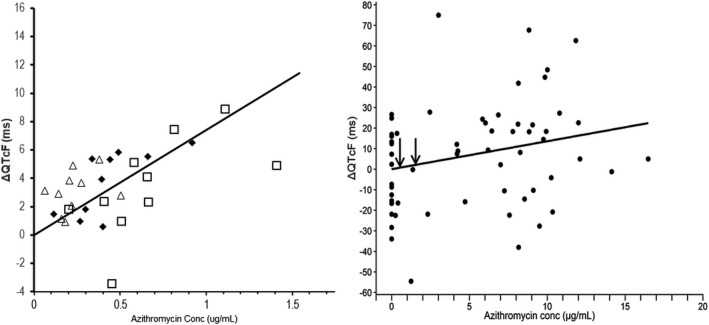
Relationship between azithromycin (AZ) concentration and Fridericia’s rate‐corrected QT interval (∆QTcF) on day 3 following oral administration of AZ and chloroquine (CQ) for 3 days (left panel) or following a single i.v. infusion of AZ (right panel). In the left panel, the mean differences in time matched changes from baseline in ∆QTcF between CQ plus AZ groups and CQ were regressed against corresponding mean AZ concentrations. In the regression model, treatment group was included as a random effect, AZ was included as a fixed effect, and there was no intercept term. (Legend: triangles: CQ + 500 mg AZ; diamonds: CQ + 1,000 mg AZ; squares: CQ + 1,500 mg AZ; solid line: regression model predictions). Right panel legend: circles represent individual subject data; solid line: regression model prediction; arrows represent corresponding mean peak plasma concentration (Cmax) values from the oral study after 500 mg and 1,500 mg dose of AZ as noted in Table 1 .
The relationship of AZ concentration vs. QTc was also investigated in an i.v. pharmacokinetic study to assess local tolerability in support of the original i.v. formulation development. This double‐blind, placebo‐controlled study involved four parallel, sequential, groups with eight healthy subjects per group (6 treated and 2 placebo). AZ was given at increasing infusate concentration (in half‐normal saline) of 1 mg/mL to 10 mg/mL as 1‐hour i.v. infusions of up to 2,000 mg, dosed daily for 10 days. Considering the absolute oral bioavailability, the i.v. dose in this study is approximately the equivalent of 6,000 mg orally, an amount roughly 12 times higher than the therapeutic dose of 500 mg. Based on observed local tolerability, the final infusate concentration ranged from 1 mg/mL to 5 mg/mL, doses of AZ ranged from 712 mg to 2,000 mg, and dosing duration was either 6 or 10 days across all 4 groups. A single 12‐lead ECG was obtained at screening (within 2 weeks prior) and at the end of infusion on treatment days 1, 6, and 10; QT values were recorded manually.
The relationship of AZ concentration at 1 hour (end of infusion) and corresponding baseline‐corrected QTcF values are presented in Figure 1 , right panel. The results estimated a 1.36 msec change from baseline in QTcF for every unit (µg/mL) change in AZ concentration. The variability in the data is apparent and can be attributed to single ECG measurements, precision of manually recording QT intervals, and the lack of an exact time‐matched baseline measurement. The observed AZ concentrations following i.v. administration in the study ranged from 0.25 µg/mL to 16.8 µg/mL. By comparison, the mean (SD) peak plasma concentration (Cmax) was 0.54 µg/mL (0.25 µg/mL) after oral administration of AZ 500 mg daily for 3 days (Table 1 ). Predicted mean ∆QTc values are shown in Table 1 ; these ∆QTc predictions are lower than that estimated from the AZ + CQ oral administration study.
CARDIOVASCULAR SAFETY EVALUATED IN RANDOMIZED CONTROLLED TRIALS
Two RCTs collected predefined cardiac end points, Weekly Intervention with Azithromycin for Atherosclerosis and its Related Disorders (WIZARD) 16 and Azithromycin and Coronary Events Study (ACES), 17 to assess the benefit and risk of AZ in a large sample of patients over a long duration of exposure. Several other small‐to‐intermediate‐sized RCTs also were carried out, but too few cardiac events occurred to reliably assess the CV effects of short‐term antibiotic treatment. 18
WIZARD 16 was a randomized, placebo‐controlled trial of adults with previous myocardial infarction (MI) and an elevated Chlamydia pneumoniae IgG titer. Patients received either AZ (600 mg/day for 3 days during week 1, then 600 mg/week during weeks 2 to 11; n = 3,866) or matching placebo (n = 3856). The primary end point was the first occurrence of death from any cause, nonfatal reinfarction, coronary revascularization, or hospitalization for angina. During the ≥ 14‐month follow‐up, 1,038 events accrued. There was no significant association between AZ treatment and the primary end point (hazard ratio 0.93; 95% CI: 0.83, 1.05). Analysis of hazard ratios at restricted time intervals indicated an early benefit of AZ on the risk of death or reinfarction during the time closest to exposure to AZ (Figure 2 ); dosing in the first week of WIZARD most closely mirrors the dosing regimens used for acute treatment of infections and in clinical studies of severe acute respiratory syndrome‐coronavirus 2 (SARS‐CoV‐2) treatment. 19 Most importantly, short‐term therapy with AZ did not increase the risk of CV death in a robust controlled trial involving large numbers of events.
Figure 2.
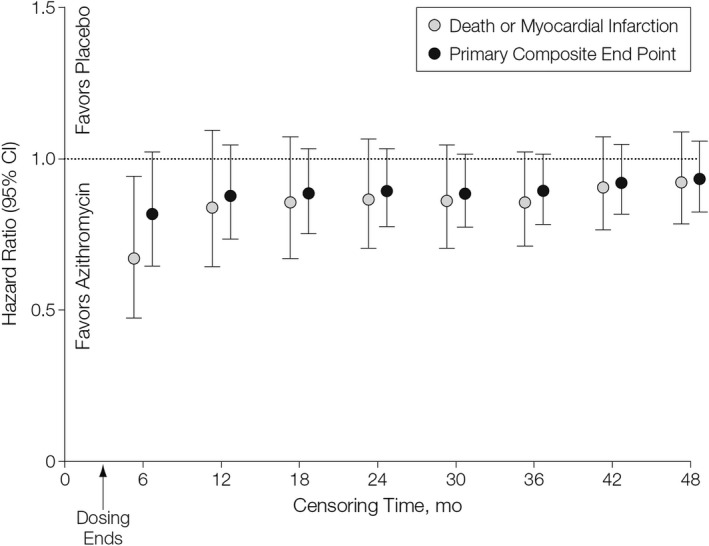
Comparison of hazard ratios at various censoring times in the Weekly Intervention with Azithromycin for Atherosclerosis and its Related Disorders (WIZARD) trial. 16 Hazard ratio (± 95% confidence interval (CI)) for treatment effect with azithromycin at various times after randomization. Reproduced with permission from JAMA 2003; 290(11):1459‐1466. ©2003 American Medical Association. All rights reserved.
The second trial was ACES, 17 a randomized, double‐blind, placebo‐controlled, multicenter study that evaluated the effect of AZ for the secondary prevention of coronary events in patients with stable coronary artery disease (defined as prior MI ≥ 3 months prior to enrollment or previous revascularization procedure). Patients were randomized to either AZ 600 mg (n = 2004) or a matching placebo + usual care (n = 2008) once weekly for 1 year. Follow‐up occurred at 3 weeks, 6 weeks, and 3, 6, 9, and 12 months after enrollment. The primary end point was a composite of any of the following: coronary heart disease death, nonfatal MI, percutaneous or surgical revascularization procedure, or hospitalization for unstable angina. There was no significant difference in the composite primary end point in the AZ group compared with the placebo group (risk reduction, 1%; 95% CI: −13%, 13%), nor in any of the individual CV event components of the primary end point. The authors concluded that a 1‐year course of weekly AZ had no effect on the risk of cardiac events among patients with stable coronary artery disease.
SAFETY PERSPECTIVE FROM OBSERVATIONAL STUDY—LITERATURE REVIEW
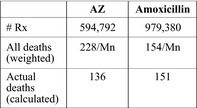
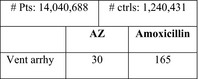
Table 2 outlines the design and key findings of seven observational studies conducted to assess the CV profile of AZ. The safety findings were heterogeneous as to whether the short‐term use of AZ carried an immediate and clinically important risk of a lethal ventricular arrhythmia. Initially, a Medicaid claims study 3 of a database (prescriptions: ~ 0.35 Mn AZ; ~ 1.3 Mn amoxicillin) highlighted in row 1 of Table 2 , reported 29 CV deaths in AZ users treated for 5 days, of which 22 were ‘sudden cardiac deaths'. These numbers were proportionately greater than after a 5‐day course of amoxicillin, wherein 42 CV deaths and 29 ‘sudden cardiac deaths' occurred. By comparison, two observational studies 20 , 21 highlighted in rows 4 and 7 of Table 2 , which involved thousands of CV deaths in each treatment group and populations with intrinsically greater CV risk, demonstrated an odds ratio for death of 0.77 and 0.74, respectively, favoring AZ, and did not suggest excess CV risk when AZ was compared with short‐term use of other antibiotics. The disparate findings might be explained by several factors, including the number and magnitude of increase in CV end points, the ability to discern different CV causes of death, and the measures taken to mitigate the impacts of confounders. One key element: death certificates are known to be an imperfect means to establish cause of death in patients with chronic lung disease; CV death is often mistakenly assumed when patients die suddenly. 22 , 23
Table 2.
Observational studies regarding CV event rates (2012–2018)
| Population | Primary comparator | Exposure window | Primary outcome(s) | Main results | Total/ CV Deaths with Rx | References |
|---|---|---|---|---|---|---|
| Medicaid | Amoxicillin | 0–5 and 6–10 days after dispensing | CV death |
CV death: HR 2.49 (95% CI: 1.38, 4.50) CV death: RD 47 (95% CI: NR) deaths per Mn Rx CV death among high baseline CV risk: RD 245 (95% CI: 63, 576) deaths per Mn Rx |
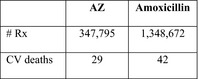
|
3 |
| Danish general population | Penicillin V | 0–5 days after dispensing | CV death |
CV death: RR 0.93 (95% CI: 0.56, 1.55) CV death among those with prior CV disease: RR 1.35 (95% CI: 0.69, 2.64) |
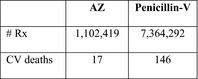
|
32 |
| US veterans (Veteran Affairs database) |
Amoxicillin |
0–5 and 6–10 days after dispensing |
All‐cause death Serious arrhythmia |
All‐cause death: HR 1.48 (95% CI: 1.05, 2.09) Serious arrhythmia: HR 1.77 (95% CI: 1.20, 2.62) |
|
33 |
| US veterans (Veteran Affairs database), hospitalized with pneumonia | Guideline concordant antibiotics | 30 and 90 days after dispensing |
30‐day mortality 90‐day mortality 90‐day MI 90‐day arrhythmia 90‐day cardiac event |
30‐day mortality: OR 0.77 (95% CI: 0.73, 0.81) 90‐day mortality: OR 0.73 (95% CI: 0.70, 0.76) 90‐day MI: OR 1.17 (95% CI: 1.08, 1.25) 90‐day arrhythmia: OR 0.99 (95% CI: 0.95, 1.02) 90‐day cardiac event: OR 1.01 (95% CI: 0.98, 1.05) |
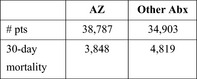
|
20 |
| Taiwanese National Health Insurance Database | Amoxicillin‐clavulanate | 7 days after dispensing |
CV death Vent arrhy |
OR 2.62 (95% CI: 1.69, 4.06) OR 4.32 (95% CI: 2.95, 6.33) |
34 | |
| 7 EU general populations | Amoxicillin | 7 days after dispensing | Ventricular arrhythmia | OR 0.90 (95% CI 0.48–1.71) |
|
35 |
| Medicare | Amoxicillin‐clavulanate | 7 days after dispensing |
Death MI Vent arrhy Atria fib or flutter |
OR 0.74 (95% CI 0.65–0.85) OR 1.10 (95% CI 0.91–1.33) OR 1.13 (95% CI 0.92–1.40) OR 1.24 (95% CI 1.11–1.38) |
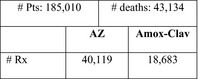
|
21 |
Abx, antibiotic; Amox‐Clav, amoxicillin‐clavulanate; CI, confidence interval; ctrl, control; CV, cardiovascular; EU, European Union; fib, fibrillation; HR, hazard ratio; MI, myocardial infarction; Mn, million; NR, not reported; OR, odds ratio; RD, risk difference; RR, relative risk; Rx, prescription; Vent arrhy, ventricular arrhythmia.
INTEGRATION OF EVIDENCE AND PERSPECTIVE
Considering QT prolongation observed with macrolide antibiotics, torsades de pointes has been raised as a class effect of concern and by association, with AZ. This has held even though AZ is an azalide, chemically different from macrolides, and different in its metabolism and drug interactions. Polymorphic ventricular tachycardia has occurred after treatment with AZ, but at a lower incidence than with either erythromycin orclarithromycin. 24 Other factors, such as concomitant proarrhythmic medications, hypokalemia or hypomagnesemia, or profound bradycardia often are significant contributors to trigger such arrhythmias and lessen the causative association to a specific drug.
Observational studies are an option for assessing the safety of a medicine; they may be especially valuable when the anticipated effect size is large (e.g., hazard ratios of several fold) or the magnitude of risk is proportional to exposure (i.e., dose or duration of treatment). However, assigning causality may have limited validity due to the potential impact of residual confounding factors even when mathematical adjustment techniques are utilized to mitigate confounders. In addition model misspecifications and missing data further limit causality assignment. 25 Furthermore, findings may depend on the source of the database and/or statistical techniques used (e.g., refs. 26, 27). When events are few, the findings should point to the need for future confirmatory studies and cite the available controlled data to contextualize the results with the weight of the evidence.
Especially with antibiotics, observational studies have difficulty matching treatment groups to eliminate imbalance, probably due to residual confounding from indication for use. Patients prescribed AZ are inherently different in severity of illness compared with those prescribed other antibiotics, especially amoxicillin. 20 AZ is preferentially prescribed for more serious lower respiratory tract infections (e.g., pneumonia or exacerbations of chronic bronchitis), where beta‐receptor agonists also are administered; the latter drugs are known to increase CV events. 28
RCTs are the gold standard for generating reliable evidence about benefits and risks of alternative treatments. Large‐scale RCTs of adequate design, power and follow‐up provide unique insights; when results are available from one or more such trials, observational studies become subordinate in the hierarchy of evidence. 25 WIZARD and ACES were characterized by prospectively defined end points, analysis methods, and other features intended to enhance data quality and minimize bias. These trials also used central adjudication of outcomes by blinded experts, with a view to reducing interobserver variability, minimizing bias, and improving data quality and integrity.
Such design features overcome some of the limitations of observational studies in terms of accurate diagnosis of events and cause of death. The WIZARD and ACES trials with AZ were conducted specifically in pre‐existing coronary heart disease to assess clinically important CV effects in patients predisposed to CV events. As discussed, AZ treatment was not associated with increased CV events nor with sudden cardiac death in these higher risk populations. The WIZARD study dosed subjects initially with 600 mg of AZ on days 1–3, which most closely mimics drug exposures in the on‐going clinical trials for SARS‐CoV‐2 treatment. Most clinical trials in patients with COVID‐19 (reported on ClinicalTrials.gov as currently active, July 10, 2020) have used AZ 500 mg on day 1 and 250 mg on days 2–5, whereas others have used doses of AZ 500 mg once daily for a duration ranging from 3–14 days; a single oral dose of AZ 1,200 mg and 250 mg daily for 5 days has been used in 1 trial each.
The benefit‐risk of AZ for mass drug administration was reviewed in the trachoma elimination program, including on‐going pharmacovigilance activities. In AZ dose‐intensification field studies to treat trachoma in Ethiopia, children under 10 years of age had a survival benefit with AZ treatment compared with a control group. 29 In a retrospective analysis, this survival benefit was also observed in adults. 30 The finding in children was confirmed in a three‐country study in Niger, Malawi, and Tanzania where overall mortality was reduced by 13.5% overall and 24.9% in a secondary end point of children 1–6 months of age. 2
Summary
Combined QTcF findings obtained during oral and i.v. pharmacokinetic‐pharmacodynamic studies of AZ suggest that the potential risk of torsade is unlikely with 500–1,500 mg oral daily doses, because the mean maximum QTc increase is less than 6–10 msec. 31 If a more conservative threshold is chosen of a placebo‐adjusted QTc with an upper bound of the 2‐sided 90% CI below 10 msec, then the 500 mg daily dose meets this criterion.
The observational studies that have assessed CV risk with antibiotics like AZ need to be interpreted cautiously because of the potential for bias due to confounders and small numbers of CV events. From studies with large numbers of CV end points, an acute illness requiring antibiotics is accompanied by an increased risk of CV death related to the severity of the underlying illness and not the antibiotic used. The increased risk of CV and non‐CV mortality during antibiotic treatment for acute illness may produce significant confounding by indication. Given data from sufficiently powered RCTs in populations at heightened risk, like the WIZARD and ACES trials, observational studies of CV risk in the same or lesser risk populations add little further insight. RCTs of AZ in patients with SARS‐CoV‐2 infection are underway and will best determine the benefit‐risk profile of the medicine in this patient population. CQ and HCQ have a known risk of proarrhythmia, however, comparative data of their effects on QTc interval prolongation are lacking. A literature search revealed no comparative studies of human ether‐a‐go‐go‐related gene effects of CQ and HCQ under the same experimental conditions. Although the effects of CQ on QTc have been evaluated in clinical studies, only case reports and observational studies are available for the effects of HCQ on QT interval. Given the termination of the HCQ alone arm of the Recovery study 19 and withdrawal of the emergency use authorization for HCQ, combination therapy with AZ and HCQ for treatment of SARS‐CoV‐2 infections should be reconsidered and reserved for study in clinical trials.
Funding
Medical writing support was funded by Pfizer Inc.
Conflict of Interest
All authors are employees of Pfizer, Inc.
Supporting information
Fig S1‐S2
Acknowledgments
The authors would like to thank Drs. Leaney, Lorenzen, and Tawadrous for their thorough scientific review.
References
- 1. Mecaskey, J.W. , Knirsch, C.A. , Kumaresan, J.A. & Cook, J.A. The possibility of eliminating blinding trachoma. Lancet Infect. Dis. 3, 728–734 (2003). [DOI] [PubMed] [Google Scholar]
- 2. Keenan, J.D. et al Azithromycin to reduce childhood mortality in Sub‐Saharan Africa. N. Engl. J. Med. 378, 1583–1592 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ray, W.A. , Murray, K.T. , Hall, K. , Arbogast, P.G. & Stein, C.M. Azithromycin and the risk of cardiovascular death. N. Engl. J. Med. 366, 1881–1890 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Knirsch, C.A. & Chandra, R. Azithromycin and the risk of cardiovascular death. N. Engl. J. Med. 367, 772–773 (2012). [DOI] [PubMed] [Google Scholar]
- 5. Crumb, W.J. Jr , Vicente, J. , Johannesen, L. & Strauss, D.G. An evaluation of 30 clinical drugs against the comprehensive in vitro proarrhythmia assay (CiPA) proposed ion channel panel. J. Pharmacol. Toxicol. Methods 81, 251–262 (2016). [DOI] [PubMed] [Google Scholar]
- 6. Saleh, M. et al Effect of chloroquine, hydroxychloroquine, and azithromycin on the corrected QT interval in patients with SARS‐CoV‐2 infection. Circ. Arrhythm. Electrophysiol. 13, e008662 (2020). 10.1161/circep.120.008662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mercuro, N.J. et al Risk of QT interval prolongation associated with use of hydroxychloroquine with or without concomitant azithromycin among hospitalized patients testing positive for coronavirus disease 2019 (COVID‐19). JAMA Cardiol. 10.1001/jamacardio.2020.1834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Geleris, J. et al Observational study of hydroxychloroquine in hospitalized patients with Covid‐19. N. Engl. J. Med. 382, 2411–2418 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rosenberg, E.S. et al Association of treatment with hydroxychloroquine or azithromycin with in‐hospital mortality in patients with COVID‐19 in New York State. JAMA 323, 2493–2502 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Damle, B. , Vourvahis, M. , Wang, E. , Leaney, J. & Corrigan, B. Clinical pharmacology perspectives on the antiviral activity of azithromycin and use in COVID‐19. Clin. Pharmacol. Ther. 108, 201–211 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ohrt, C. , Willingmyre, G.D. , Lee, P. , Knirsch, C. & Milhous, W. Assessment of azithromycin in combination with other antimalarial drugs against Plasmodium falciparum in vitro. Antimicrob. Agents Chemother 46, 2518–2524 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Noedl, H. et al Azithromycin combination therapy with artesunate or quinine for the treatment of uncomplicated Plasmodium falciparum malaria in adults: a randomized, phase 2 clinical trial in Thailand. Clin. Infect. Dis. 43, 1264–1271 (2006). [DOI] [PubMed] [Google Scholar]
- 13. Noedl, H. et al In vitro antimalarial activity of azithromycin, artesunate, and quinine in combination and correlation with clinical outcome. Antimicrob. Agents Chemother. 51, 651–656 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fossa, A.A. , Wisialowski, T. , Duncan, J.N. , Deng, S. & Dunne, M. Azithromycin/chloroquine combination does not increase cardiac instability despite an increase in monophasic action potential duration in the anesthetized guinea pig. Am. J. Trop. Med. Hyg. 77, 929–938 (2007). [PubMed] [Google Scholar]
- 15. Thomsen, M.B. et al No proarrhythmic properties of the antibiotics moxifloxacin or azithromycin in anaesthetized dogs with chronic‐AV block. Br. J. Pharmacol. 149, 1039–1048 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. O'Connor, C.M. et al Azithromycin for the secondary prevention of coronary heart disease events: the WIZARD study: a randomized controlled trial. JAMA 290, 1459–1466 (2003). [DOI] [PubMed] [Google Scholar]
- 17. Grayston, J.T. et al Azithromycin for the secondary prevention of coronary events. N. Engl. J. Med. 352, 1637–1645 (2005). [DOI] [PubMed] [Google Scholar]
- 18. Grayston, J.T. Antibiotic treatment of atherosclerotic cardiovascular disease. Circulation 107, 1228–1230 (2003). [DOI] [PubMed] [Google Scholar]
- 19. Recovery Study . <https://www.recoverytrial.net/>. Accessed July 9, 2020.
- 20. Mortensen, E.M. et al Association of azithromycin with mortality and cardiovascular events among older patients hospitalized with pneumonia. JAMA 311, 2199–2208 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Polgreen, L.A. et al Estimated cardiac risk associated with macrolides and fluoroquinolones decreases substantially when adjusting for patient characteristics and comorbidities. J. Am. Heart Assoc. 7, e008074 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Myerburg, R.J. Cardiac and noncardiac causes of apparent sudden arrhythmic deaths: shadows in a spectrum. Circulation 137, 2701–2704 (2018). [DOI] [PubMed] [Google Scholar]
- 23. Wise, R.A. et al Discordance in investigator‐reported and adjudicated sudden death in TIOSPIR. ERJ Open Res. 3, 00073‐2016 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hancox, J.C. , Hasnain, M. , Vieweg, W.V. , Crouse, E.L. & Baranchuk, A. Azithromycin, cardiovascular risks, QTc interval prolongation, torsade de pointes, and regulatory issues: a narrative review based on the study of case reports. Ther. Adv. Infect. Dis. 1, 155–165 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. MacMahon, S. & Collins, R. Reliable assessment of the effects of treatment on mortality and major morbidity, II: observational studies. Lancet (London, England) 357, 455–462 (2001). [DOI] [PubMed] [Google Scholar]
- 26. Hartz, A. , He, T. , Wallace, R. & Powers, J. Comparing hormone therapy effects in two RCTs and two large observational studies that used similar methods for comprehensive data collection and outcome assessment. BMJ Open 3, e002556 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Madigan, D. et al Evaluating the impact of database heterogeneity on observational study results. Am. J. Epidemiol. 178, 645–651 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Salpeter, S.R. , Ormiston, T.M. & Salpeter, E.E. Cardiovascular effects of beta‐agonists in patients with asthma and COPD: a meta‐analysis. Chest 125, 2309–2321 (2004). [DOI] [PubMed] [Google Scholar]
- 29. Porco, T.C. et al Effect of mass distribution of azithromycin for trachoma control on overall mortality in Ethiopian children: a randomized trial. JAMA 302, 962–968 (2009). [DOI] [PubMed] [Google Scholar]
- 30. Keenan, J.D. , Emerson, P.M. , Gaynor, B.D. , Porco, T.C. & Lietman, T.M. Adult mortality in a randomized trial of mass azithromycin for trachoma. JAMA Intern. Med. 173, 821–823 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shah, R.R. The significance of QT interval in drug development. Br. J. Clin. Pharmacol. 54, 188–202 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Svanstrom, H. , Pasternak, B. & Hviid, A. Use of azithromycin and death from cardiovascular causes. N. Engl. J. Med. 368, 1704–1712 (2013). [DOI] [PubMed] [Google Scholar]
- 33. Rao, G.A. et al Azithromycin and levofloxacin use and increased risk of cardiac arrhythmia and death. Ann. Family Med. 12, 121–127 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chou, H.W. , Wang, J.L. , Chang, C.H. , Lai, C.L. , Lai, M.S. & Chan, K.A. Risks of cardiac arrhythmia and mortality among patients using new‐generation macrolides, fluoroquinolones, and beta‐lactam/beta‐lactamase inhibitors: a Taiwanese nationwide study. Clin. Infect. Dis. 60, 566–577 (2015). [DOI] [PubMed] [Google Scholar]
- 35. Trifiro, G. et al Use of azithromycin and risk of ventricular arrhythmia. CMAJ 189, E560–E568 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1‐S2