Abstract
Confinement during the COVID‐19 pandemic is expected to have a serious and complex impact on the mental health of patients with an eating disorder (ED) and of patients with obesity. The present manuscript has the following aims: (1) to analyse the psychometric properties of the COVID Isolation Eating Scale (CIES), (2) to explore changes that occurred due to confinement in eating symptomatology; and (3) to explore the general acceptation of the use of telemedicine during confinement. The sample comprised 121 participants (87 ED patients and 34 patients with obesity) recruited from six different centres. Confirmatory Factor Analyses (CFA) tested the rational‐theoretical structure of the CIES. Adequate goodness‐of‐fit was obtained for the confirmatory factor analysis, and Cronbach alpha values ranged from good to excellent. Regarding the effects of confinement, positive and negative impacts of the confinement depends of the eating disorder subtype. Patients with anorexia nervosa (AN) and with obesity endorsed a positive response to treatment during confinement, no significant changes were found in bulimia nervosa (BN) patients, whereas Other Specified Feeding or Eating Disorder (OSFED) patients endorsed an increase in eating symptomatology and in psychopathology. Furthermore, AN patients expressed the greatest dissatisfaction and accommodation difficulty with remote therapy when compared with the previously provided face‐to‐face therapy. The present study provides empirical evidence on the psychometric robustness of the CIES tool and shows that a negative confinement impact was associated with ED subtype, whereas OSFED patients showed the highest impairment in eating symptomatology and in psychopathology.
Keywords: COVID Isolation Eating Scale, COVID‐19, eating disorders, obesity
1. BACKGROUND
In just a few months, COVID‐19 has become a global pandemic that has brought numerous challenges to health professionals and their patients. To stop the speed of the spread of the virus, most governments have chosen to place their populations under confinement, which has implied radical changes in social interactions and the way work was conducted. The final repercussions of confinement are still under investigation, though it is expected to have a significant impact on mental health for many.
Considering other health and humanitarian crises, such as the Ebola and H1N1 influenza epidemics, depression (Hewlett & Hewlett, 2005; Kinsman, 2012), isolation, fear of being infected, posttraumatic stress (Li et al., 2018; Raven, Wurie, & Witter, 2018; Main, 2011) and health anxiety (McDonnell, Nelson, & Schunk, 2012; Mihashi, 2009) have been some of the negative effects on mental health reported by the general population, health workers and survivors of past epidemics (Wu, 2009). Confinement has been found to increase the incidence of negative states such as irritability, insomnia, anger, depression symptoms, amongst others (Mihashi, 2009).
In response to the COVID‐19 pandemic, several studies have already been carried out to explore the psychological effects of the pandemic and confinement. In the general population, anxiety, depression, stress, worry about being infected, worry about family members being infected, worry about financial stress stability, post‐traumatic stress (Cao et al., 2020; Wang, Pan, et al., 2020; Wang, Di et al., 2020), but also mental health deterioration (Pierce, Hope, Ford, et al., 2020) and nutritional and activity patterns changes (Papandreou, Tsilidis, Arija, Aretouli, & Bulló, 2020), have been reported. Healthcare workers have emerged as a specific population in danger of suffering from psychological distress, depression, anxiety and insomnia (Inchausti, García‐Poveda, Prado‐Abril, & Sánchez‐Reales, 2020; Lai et al., 2020; Rossi et al., 2020) and populations with a prior mental health condition may experience an increase in their symptomatology related to changes in the delivery of their usual treatment (De Girolamo et al., 2020; Fernández‐Aranda et al., 2020).
It is important to consider that stay‐at‐home and social‐distancing mandates have increased the frequency of several risk behaviours. The time available for engaging in potentially addictive behaviours, such as online gambling, gaming, and pornography (Håkansson, Fernández‐Aranda, Menchón, Potenza, & Jiménez‐Murcia, 2020; Király et al., 2020; Mestre‐Bach, Blycker, & Potenza, 2020) has increased and these behaviours, along with the use of alcohol or other substances, may be used as coping strategies to avoid negative emotional states (Håkansson et al., 2020; King, Delfabbro, Billieux, & Potenza, 2020; Király et al., 2020; Sun et al., 2020). Although these behaviours do not constitute a risk for all individuals, the current situation may increase the risk for onset, maintenance, and relapse, especially for the most vulnerable individuals (Columb, Hussain, & O'Gara, 2020; Marsden et al., 2020), such as patients with an eating disorders and patients with obesity (Baenas et al., 2020; Graell et al., 2020; Cornejo‐Pareja et al., 2020), as well as patients with less favourable family environments (Vintró‐Alcaraz et al., 2018).
It has been hypothesised that the COVID‐19 pandemic may exacerbate the risk factors for overeating and unhealthy weight gain, especially in vulnerable populations such as children and individuals with an eating disorder (ED) and obesity (Rundle, Park, Herbstman, Kinsey, & Wang, 2020, Graell et al., 2020). ED patients have already reported increased worries about the risk of being infected with COVID‐19, disruptions in their work and treatment, the worsening of their ED symptoms, as well as heightened anxiety and stress (Fernández‐Aranda et al., 2020). ED patients and individuals with obesity constitute vulnerable populations who require targeted approaches (Cornejo‐Pareja et al., 2020). As an immediate emergency measure to address this situation, different telemedicine tools during the pandemic have been described within this population (Cooper et al., 2020; Smith, Ostinelli, Macdonald, & Cipriani, 2020), however there is a lack of studies looking at their effectiveness and acceptability by users.
New psychometric instruments have been developed to measure different features related to the Covid‐19 pandemic, such as the contextual situation lived during the confinement, the changes occurring in the individuals' life and the impact on their health state. Some of these new scales are: the Fear of COVID‐19 Scale (FCV‐19S; (Ahorsu et al., 2020; Sakib et al., 2020; Soraci et al., 2020), the COVID‐19 Anxiety Scale (CAS; (Chandu, Pachava, Vadapalli, & Marella, 2020), the COVID‐19‐PTSD (Forte, Favieri, Tambelli, & Casagrande, 2020), the CoViD‐19 Peritraumatic Distress Index (CPDI; (Costantini & Mazzotti, 2020), the Coronavirus Impact Scale (CIS; Kaufman & Stoddard, 2020) and the COVID Stress Scales (CSS; (Taylor et al., 2020), including COVID danger and contamination fears, COVID fears about economic consequences, COVID xenophobia, COVID compulsive checking and reassurance seeking, and COVID traumatic stress symptoms. However, to the best of our knowledge, no tool has yet been developed and validated to assess eating disorder symptomatology and treatment‐related aspects in patients with an ED and obesity.
1.1. Goals
The aims of this exploratory study were threefold: (1) to analyse the psychometric properties of the COVID Isolation Eating Scale (CIES), a newly created scale for measuring the impact of confinement; (2) to explore changes that occurred due to confinement (eating symptomatology and weight, attitudes and dysfunctional emotions, worries and concerns, anxiety and depressive symptomatology and addictive behaviours); (3) to explore the potential difficulties for participants in using telemedicine during confinement when usual health care was interrupted. Based on previous literature (Baenas et al., 2020; Fernández‐Aranda et al., 2020; Temorshuizen et al., 2020; Mallorqui‐Bague, 2018), we hypothetised that eating disorder subtype and obesity would achieve a moderator/interaction role in the changes occurred during the confinement: behavioural and emotional reactions, eating patterns‐weight, anxiety and affective symptoms should be different depending on the ED subtype previous to the COVID‐19 pandemic.
2. METHODS
The data collection of this study was conducted between June and July 2020. Our study sample comprised 121 participants (87 ED patients and 34 patients with obesity), recruited from six different child‐adolescent and adult units from the Barcelona (Spain) region. These centres are representative of the public and private sectors of ED treatment services in Barcelona. Participants were involved in ED treatment before the outbreak of COVID‐19 and were asked by therapists from each centre if they were willing to voluntarily complete the study questionnaire. The ED sample was diagnosed according to DSM‐5 criteria (American Psychiatric Association, 2013) by means of a semi‐structured interview. Obese participants were bariatric surgery candidates who were recruited at the Endocrinological Unit at the Clinic Hospital of Barcelona.
The sex distribution was 104 women (86.0%) and 17 men (14.0%). The age range was broad (mean = 33.7, SD = 15.8), ranging from 13 to 77. The distribution of the ED diagnoses was as follows: 55 cases met criteria for anorexia nervosa (AN), 18 for bulimia nervosa (BN), 14 were diagnosed with an Other Specified Feeding or Eating Disorder (OSFED). Table S1 (supplementary material) contains the distribution of sex and age within the groups defined by diagnosis. No statistical differences by gender were obtained (χ 2 = 4.06, df = 3, p = .256). However, chronological age was not equally distributed between groups (F = 30.08, df = 3/117, p < .001): obese patients were the oldest (mean = 48.8, SD = 12.9), followed by OSFED (mean = 36.9, SD = 16.4), BN (mean = 31.5, SD = 10.1) and AN (mean = 24.2, SD = 10.7) patients.
2.1. Assessment
The COVID Isolation Eating Scale (CIES) is a self‐report questionnaire that assesses the impact of confinement in patients with an eating disorder and/or obesity. This measure has been designed to be answered both with paper and pencil or online. The scale was generated by experts in the ED area through a theoretical‐rationale procedure based on the next steps: (a) identification of the domains (constructs/areas) endeavouring to measure; (b) deciding the number of factors/dimensions and their position into a meaningful order and format into the questionnaire; and (c) generating the items, as well as their distribution within each factor/dimension. After the development of the item pool, independent expert judges assessed whether the items adequately represented the domains of interest. The final CIES, besides exploring patient sociodemographic information, the scale was divided into four sections: (I) Circumstances during confinement (eight items characterising the circumstances of confinement). (II) Effects of confinement on eating disorder symptoms (13 items relating to the eating symptomatology of anorexia nervosa, bulimia nervosa, binge eating disorder and other specified feeding or eating disorder, according to the DSM‐5 and comorbid physical and psychiatric disorders. (III) Behavioural and psychopathological impact of confinement (34 items covering the effects of confinement on eating patterns, attitudes and habits, anxiety‐depression symptomatology, emotion dysregulation, and other symptomatology associated with substance use disorders and non‐substance related addictive behaviours. (IV) Evaluation of remote interventions (13 items assessing the feasibility, acceptance and satisfaction). The three last scales are answered on a five‐point Likert scale. Sections 2 and 3 consider two moments of time: before confinement and now, the present (for the English version of CIES Scale and translation in 18 additional languages see Supplementary information online).
2.2. Additional information
Socio‐demographic/clinical information, including age, affiliation to the patient with an ED, and marital status, but also variables related to COVID and duration and type of the confinement was obtained along with the CIES questionnaire.
2.3. Procedure
The present study was approved by the Clinical Research Ethics Committee of Bellvitge University Hospital (PR239/20). Written and signed informed consent was obtained from all participants before taking part in the study.
2.4. Statistical analysis
Statistical analyses were carried out with Stata16 for Windows (Stata Press, 2019). Based on the theoretical‐rational method used to develop the CIES, confirmatory factor analyses (CFA) was used to verify the factor structure of the questionnaire. CFA was implemented through structural equation modelling, defining the maximum likelihood, and considering adequate goodness of fit for Root Mean squared Error of Approximation RMSEA < 0.08, Comparative Fit Index CFI > 0.90, Tucker‐Lewis Index TLI > 0.90 and Standardised Root Mean Squared Residuals SRMR<0.10 (Barrett, 2007).
An initial CFA assumed the existence of five latent theoretical factors: Factor 1 was defined by 10 items measuring eating related symptoms (such as concerns about weight, attempts to reduce eating quantities and meals, presence of bingeing/purging, use of laxatives/diuretics, and exercise or other activities to control weight); Factor 2 was defined by 10 items measuring the effects of confinement on the eating related style (such as being unable to stop eating during the day, or between meals or certain foods); Factor 3 was defined by 11 items assessing anxiety and depressive symptoms (sleep problems, upsetting thoughts, loneliness, limited social contact, health concerns related to COVID‐19, or sexual problems); Factor 4 was defined by five items related to emotion regulation (emotional control/awareness, anger/shame, aggressive behaviours and irritability); and Factor 5 was defined by 10 items to evaluate telemedicine (adequacy, motivation, satisfaction and usefulness). Factors F1, F2, F3 and F4 were also developed to allow for assessment prior and following COVID‐19 confinement. However, it was not possible to test the initial single CFA for the five‐dimension model, because the sample size was too small to verify this complex structure (fit was not obtained). According to the sample size, separate models were tested for each dimension, programming within the same model the measures for the pre‐ and the post‐confinement to account for the expected correlations between both periods. Figure S1 (supplementary material) contains the path diagrams for the individual constructs tested in this manuscript.
The pre‐post changes in the quantitative variables of the study were based on paired‐sample t‐tests for interval scaled variables, and on the McNemar test for categorical measures. The comparison between groups defined by the diagnosis (AN, BN, OSFED and obese) was based on analysis of variance analyses (ANOVAs), with post‐hoc pairwise comparisons estimated via Bonferroni's procedure. For all these analyses, significant tests were complemented with the estimation of the effect size through Cohen's‐d coefficient, considering null effect for |d| < 0.20, low‐poor for |d| > 0.20, mild‐medium for |d| > 0.50 and large‐high for |d| > 0.80) (Cohen, 1988; Kelley & Preacher, 2012; Granero, 2020).
3. RESULTS
3.1. Characteristics of the participants during the COVID‐19 confinement
During the lockdown period, 30 (24.8%) participants lived alone, and 32 (26.4%) lived with one or two people at home, 29 (24.0%) lived with three people, and the remaining 30 participants (24.8%) lived with more than three people. Most participants were not infected by COVID‐19 (n = 115, 95.0%) and most had no infections amongst people close to them (n = 94, 77.7%). Most participants did not report a caring role during the confinement (n = 84, 69.4%). 58% (70 participants) continued to work and 69% (83 participants) had no financial loss. No statistical differences between groups were observed for these contextual variables during lockdown (Table S1, supplementary material, contains the frequency distribution within the groups).
3.2. Psychometric properties of the CIES
The factorial analyses confirmed the rational‐theoretical structure for the CIES. All the items obtained significant factor loadings for their specific factor (Table S2, supplementary material, includes the standardised coefficients, standard errors, p‐values and 95% confidence intervals). The upper block of Table 1 includes the fit indices of the CFAs and the internal consistency coefficients of the factors/scales: adequate goodness‐of‐fit was obtained, and Cronbach alpha coefficients ranged from good (α = 0.81, for the factor F1‐impacts at pre‐confinement) to excellent (α = 0.92, for F2‐changes in eating at pre‐confinement). The bottom block of Table 1 contains the correlation matrix for the factor scores. Relevant positive correlations (with |R| coefficients above 0.24) were obtained for the factors F1, F2, F3 and F4, for both at pre‐confinement and after the confinement, with the only exception of F1‐post which did not correlate with F3‐pre and F4‐pre. However, no relevant correlations emerged between F5 (evaluation of telemedicine) and the other factors.
TABLE 1.
Internal consistency, fitting indexes in the CFA and correlation‐matrix for CIES scores
| Cronbach‐alpha | Fitting indices | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | RMSEA | CFI | TLI | SRMR | ||||
| F1. | Impact on ED symptoms | .805 | .806 | .061 | .937 | .917 | .088 | ||
| F2. | Changes ‐ eating | .922 | .910 | .072 | .941 | .924 | .080 | ||
| F3. | Changes‐ anxiety/depression | .865 | .857 | .093 | .961 | .950 | .089 | ||
| F4. | Changes‐ emotion regulation | .826 | .836 | .012 | .999 | .998 | .042 | ||
| F5. | Evaluation telemedicine | .939 | .033 | .983 | .964 | .036 | |||
| Correlation‐matrix | F2pre | F3pre | F4pre | F1post | F2post | F3post | F4post | F5 | |
| F1. | Pre‐impact on ED symptoms | .675 | .368 | .401 | .547 | .480 | .278 | .256 | .006 |
| F2. | Pre‐changes—eating | — | .489 | .498 | .451 | .657 | .341 | .338 | .160 |
| F3. | Pre‐changes—anxiety/depression | — | .736 | .144 | .345 | .729 | .549 | −.032 | |
| F4. | Pre‐changes—emotional regulation | — | .154 | .281 | .553 | .765 | −.145 | ||
| F1. | Post‐impact on ED symptoms | — | .656 | .365 | .331 | −.120 | |||
| F2. | Post‐changes—eating | — | .528 | .444 | −.008 | ||||
| F3. | Post‐changes—anxiety/depression | — | .746 | −.208 | |||||
| F4. | Post‐changes—emotion regulation | — | −.183 | ||||||
| F5. | Evaluation telemedicine | ||||||||
Abbreviations: CFI, comparative fit index; RMSEA, root mean squared error of approximation; SRMR, standardised root mean squared residual; TLI, Tucker‐Lewis Index.
Note: Bold values indicate correlation coefficient with an effect size in the moderate (|R| > 0.24) to high (|R| > 0.37) range.
3.3. Impact of the COVID‐19 on eating related behaviours
Table 2 contains the main changes in weight, BMI, CIES factors F1 to F4, the consumption of substances and the presence of other addictive behaviours. Separate analyses were performed according to the diagnostic subtype, since it was hypothesised that the diagnosis could influence pre‐post differences. Within AN patients, significant decreases after the confinement due to COVID‐19 were found for the factors F1 (impact on eating symptoms), F2 (changes in eating style) and F4 (changes in emotion regulation). Obese patients also reported a significant decrease in weight, BMI and changes in the eating style. However, no significant changes emerged for the BN and OSFED patients.
TABLE 2.
Changes during confinement stratified by diagnostic subtype
| Pre | Post | |||||
|---|---|---|---|---|---|---|
| Anorexia (n = 55) | Mean | SD | Mean | SD | p | |d| |
| Weight (kg) | 49.16 | 6.91 | 50.27 | 6.52 | .056 | 0.17 |
| BMI (kg/m2) | 18.25 | 2.25 | 18.67 | 2.14 | .058 | 0.19 |
| CIES‐F1 impact ED symptoms | 11.87 | 6.79 | 9.40 | 5.61 | .015 | 0.40 |
| CIES‐F2 changes—eating | 8.76 | 9.61 | 6.11 | 6.94 | .023 | 0.32 |
| CIES‐F3 changes—anxiety‐depression | 18.29 | 9.69 | 17.80 | 9.64 | .662 | 0.05 |
| CIES‐F4 changes—emotion regulation | 9.47 | 4.63 | 8.33 | 4.86 | .046 | 0.24 |
| n | % | n | % | P | |d| | |
| Tobacco | 15 | 27.3% | 15 | 27.3% | 1.00 | 0.00 |
| Alcohol | 6 | 10.9% | 5 | 9.1% | 1.00 | 0.06 |
| Other illegal drugs | 4 | 7.3% | 3 | 5.5% | 1.00 | 0.07 |
| Addictive behaviours | 25 | 45.5% | 31 | 56.4% | .180 | 0.22 |
| Bulimia (n = 18) | Mean | SD | Mean | SD | p | |d| |
| Weight (kg) | 65.26 | 10.93 | 66.22 | 11.81 | .230 | 0.08 |
| BMI (kg/m2) | 24.13 | 3.75 | 24.47 | 4.02 | .243 | 0.09 |
| CIES‐F1 impact ED symptoms | 15.72 | 6.31 | 14.94 | 6.04 | .617 | 0.13 |
| CIES‐F2 changes—eating | 19.50 | 9.75 | 17.72 | 7.51 | .306 | 0.20 |
| CIES‐F3 changes—anxiety‐depression | 18.61 | 8.89 | 20.22 | 7.12 | .125 | 0.20 |
| CIES‐F4 changes—emotion regulation | 9.33 | 4.19 | 9.56 | 4.26 | .521 | 0.05 |
| n | % | n | % | p | |d| | |
| Tobacco | 5 | 27.8% | 5 | 27.8% | 1.00 | 0.00 |
| Alcohol | 6 | 33.3% | 6 | 33.3% | 1.00 | 0.00 |
| Other illegal drugs | 1 | 5.6% | 1 | 5.6% | 1.00 | 0.00 |
| Addictive behaviours | 12 | 66.7% | 13 | 72.2% | 1.00 | 0.12 |
| OSFED (n = 14) | Mean | SD | Mean | SD | p | |d| |
| Weight (kg) | 63.07 | 8.99 | 62.91 | 8.48 | .926 | 0.02 |
| BMI (kg/m2) | 23.40 | 3.38 | 23.30 | 2.84 | .886 | 0.03 |
| CIES‐F1 impact ED symptoms | 12.29 | 6.60 | 13.14 | 8.37 | .602 | 0.11 |
| CIES‐F2 changes—eating | 11.57 | 10.80 | 13.36 | 12.68 | .140 | 0.15 |
| CIES‐F3 changes—anxiety‐depression | 14.07 | 10.23 | 18.21 | 10.54 | .071 | 0.40 |
| CIES‐F4 changes—emotion regulation | 5.14 | 4.28 | 6.36 | 4.80 | .066 | 0.27 |
| n | % | n | % | p | |d| | |
| Tobacco | 6 | 42.9% | 6 | 42.9% | 1.00 | 0.00 |
| Alcohol | 3 | 21.4% | 4 | 28.6% | 1.00 | 0.17 |
| Other illegal drugs | 0 | 0.0% | 0 | 0.0% | 1.00 | 0.00 |
| Addictive behaviours | 7 | 50.0% | 9 | 64.3% | .500 | 0.29 |
| OBESE (n = 34) | Mean | SD | Mean | SD | p | |d| |
| Weight (kg) | 109.62 | 20.51 | 106.46 | 19.61 | .035 | 0.16 |
| BMI (kg/m2) | 41.15 | 7.37 | 39.94 | 6.86 | .037 | 0.17 |
| CIES‐F1 impact ED symptoms | 13.29 | 6.06 | 13.56 | 6.21 | .645 | 0.04 |
| CIES‐F2 changes—eating | 14.00 | 10.40 | 9.82 | 9.40 | .017 | 0.42 |
| CIES‐F3 changes—anxiety‐depression | 14.29 | 9.80 | 14.00 | 10.33 | .765 | 0.03 |
| CIES‐F4 changes—emotion regulation | 4.65 | 4.69 | 4.06 | 4.36 | .280 | 0.13 |
| n | % | n | % | p | |d| | |
| Tobacco | 5 | 14.7% | 4 | 11.8% | 1.00 | 0.09 |
| Alcohol | 6 | 17.6% | 4 | 11.8% | .500 | 0.17 |
| Other illegal drugs | 1 | 2.9% | 0 | 0.0% | 1.00 | 0.34 |
| Addictive behaviours | 23 | 67.6% | 23 | 67.6% | 1.00 | 0.00 |
Abbreviations: OSFED, other specified feeding eating disorders.
Note: Bold values indicate significant comparison.
Figure 1 displays the means of the pre‐post changes in the main variables of the study: weight, BMI, and CIES factors F1 to F4 (Table 3 contains the ANOVA comparing the changes between the groups). The obese patients were characterised by the highest change in weight (with a significant decrease of 3.2 kg, compared to an increase of nearly 1 kg for AN and BN patients and 0 kg for OSFED patients). Patients with AN also improved on other CIES factors. Although for the OSFED patients there were no pre‐post changes in weight and BMI, all other CIES factors deteriorated.
FIGURE 1.
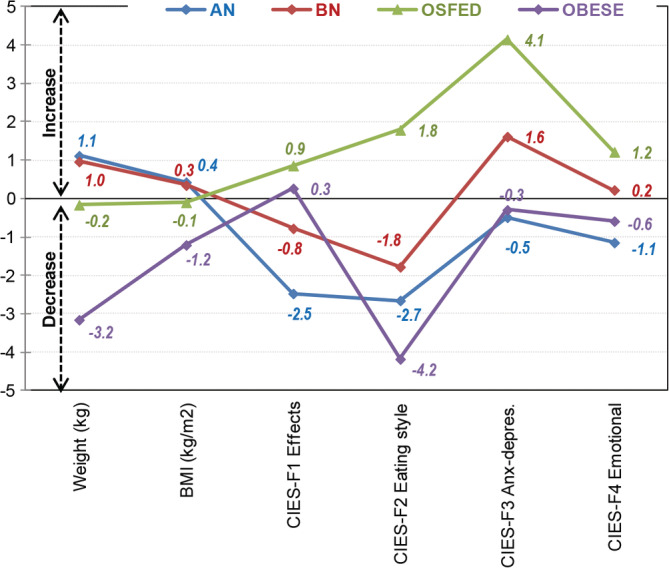
Differences (post‐pre changes) in weight, BMI and CIES factors amongst the groups [Colour figure can be viewed at wileyonlinelibrary.com]
TABLE 3.
Comparison of the differences (post‐pre changes) for the weight and the CIES factor scores
| Anorexia (AN) | Bulimia (BN) | OSFED | Obesity (OBES) | Significant | |||||
|---|---|---|---|---|---|---|---|---|---|
| N = 55 | N = 18 | N = 14 | N = 34 | Pairwise | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Comparisons | |
| Weight (kg) | 1.11 | 4.23 | 0.96 | 3.27 | −0.16 | 6.48 | −3.16 | 8.38 | OBES ≠ (AN=BN=OSFED) |
| BMI (kg/m2) | 0.43 | 1.63 | 0.35 | 1.22 | −0.10 | 2.51 | −1.21 | 3.24 | OBES ≠ (AN=BN=OSFED) |
| CIES‐F1 impact ED symptoms | −2.47 | 7.31 | −0.78 | 6.48 | 0.86 | 6.00 | 0.26 | 3.31 | AN ≠ (BN=OSFED = OBES) |
| CIES‐F2 changes—eating | −2.65 | 8.38 | −1.78 | 7.14 | 1.79 | 4.25 | −4.18 | 9.70 | OSFED ≠ (AN=BN) ≠ OBES |
| CIES‐F3 changes—anx‐dep. | −0.49 | 8.29 | 1.61 | 4.23 | 4.14 | 7.89 | −0.29 | 5.70 | OSFED ≠ (AN=BN=OBES) |
| CIES‐F4 changes—emotion | −1.15 | 4.15 | 0.22 | 1.44 | 1.21 | 2.26 | −0.59 | 3.12 | OSFED ≠ (AN=BN=OBES) |
Abbreviations: OSFED, other specified feeding eating disorder.
3.4. Evaluation of telemedicine
Table 4 contains information about the evaluation of alternatives to face to face therapy. Patients with AN, found these alternatives the least acceptable whereas people with obesity and OSFED patients were more satisfied with these alternatives.
TABLE 4.
Comparison of the CIES F5 evaluation of telemedicine between the groups
| Anorexia (AN) | Bulimia (BN) | OSFED | Obesity | ||||
|---|---|---|---|---|---|---|---|
| n = 55 | n = 18 | n = 14 | n = 34 | ||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| 25.58 | 10.40 | 28.61 | 6.46 | 29.50 | 9.53 | 28.97 | 7.25 |
| Pairwise comparisons | p | |d| | |||||
| Anorexia vs bulimia | .218 | 0.35 | |||||
| Anorexia vs OSFED | .148 | 0.39 | |||||
| Anorexia vs obesity | .047* | 0.38 | |||||
| Bulimia vs OSFED | .782 | 0.11 | |||||
| Bulimia vs obesity | .891 | 0.05 | |||||
| OSFED vs obesity | .853 | 0.06 | |||||
Abbreviation: OSFED, other specified feeding eating disorder.
4. DISCUSSION
This study was prompted by the need to assess the effects of confinement due to the COVID‐19 pandemic in vulnerable patients with ED and obesity (Cornejo‐Pareja et al., 2020; Fernández‐Aranda et al., 2020; Todisco & Donini, 2020). The three main aims were to first establish the psychometric properties of the specifically developed assessment measure (CIES), second to measure the changes in eating and general symptomatology, and thirdly to establish the acceptability of remote interventions.
The CFA confirmed the rational‐theoretical structure of CIES into five‐factors (impact on eating symptoms, changes in eating style, changes in anxiety/depression symptoms, changes in emotion regulation and evaluation of telemedicine), obtaining adequate goodness‐of‐fit. Other attributes of validity of this tool should be analysed in future research (such as the convergent, discriminant and predictive validity, assessing the relationship between the CIES scores with other external measures related with eating behaviours).
The impact of confinement was mixed and varied by diagnosis. In contrast to other studies (Rodgers et al., 2020), the disordered eating improved during the COVID‐19 pandemic. Patients with obesity had a significant decrease both in weight/BMI and in eating psychopathology. This may be due to the fact that candidates for bariatric surgery were receiving ongoing nutritional management, and were selected based on minimal psychopathology. Also the findings from AN and BN patients do not align with previous studies which found a worsening in dietary restriction (Temorshuizen et al., 2020) and heightened psychological distress (Clark Bryan et al., 2020; Pierce et al., 2020). In the present study, AN and BN participants, did not present significant changes in weight/BMI. In this study people with AN, reported a significant decrease in ED symptomatology and in emotion dysregulation after confinement. Factors such as younger age and how participants were dealing with external control environments, might be associated (Darrow, Accurso, Nauman, Goldschmidt, & Le Grange, 2017; Treasure, Gavan, Todd, & Schmidt, 2003). Interestingly, OSFED patients reported most adverse effects on eating behaviours and anxiety‐depressive symptoms after confinement. As reported previously in the literature (Riesco et al., 2018), clinicians may need to pay special attention to subthreshold cases, who may be more sensitive to adverse environments (Claes, Boekaerts, Verschueren, Boukaert, & Luyckx, 2019; Strand, von Hausswolff‐Juhlin, Fredlund, & Lager, 2019; Vanzhula, Calebs, Fewell, & Levinson, 2019)
Finally, although most patients reported being satisfied with the remote treatment used during the pandemic, in concordance with previous studies (Linardon, Shatte, Tepper, & Fuller‐Tyszkiewicz, 2020), patients with AN were the least comfortable with the change. Other studies have reported on the distress caused by premature discharge from inpatient care with a lack of preparation (Clark Bryan et al., 2020). This sensitivity to change may be related with specific temperamental traits, such as managing uncertainty and may be specific therapy targets in future interventions (Baenas et al., 2020; Brown et al., 2017; Kannarkat, Smith, & McLeod‐Bryant, 2020).
4.1. Limitations
Despite the novelty of this study, several limitations should be considered in the present study: memory bias due to the retrospective nature of the assessment, limited sample size and heterogeneity of the patient groups analysed.
5. CONCLUSIONS
The present study provides empirical evidence on the psychometric robustness of the CIES tool. The effects of confinement, varied by ED subtype. Patients with AN and those with obesity endorsed a positive response whereas OSFED patients showed the highest deterioration in eating symptomatology and in psychopathology. Furthermore, AN patients expressed the greatest dissatisfaction with adjustment to remote therapy.
The administration of the CIES in populations with ED and obesity may inform clinicians about how to prepare for adjustments to future environmental challenges. Further studies may need to be conducted in different countries with larger samples in order to be able to generalise these results.
Supporting information
Figure S1 Scheme of the CFA in the study
Table S1 and Table S2 Description of the sample and Standardised coefficients obtained in the CFA
CIES Scale v.1.0 (Translation in 19 Languages: English‐Spanish‐Catalan‐French‐Portuguese‐Italian‐German‐Swedish‐Czech‐Lithuanian‐Dutch‐Russian‐Hungarian‐Georgian‐Hebrew‐Japanese‐Korean‐Chinese‐Ukrainian).
ACKNOWLEDGEMENTS
We thank CERCA Programme/Generalitat de Catalunya for institutional support. This manuscript and research was supported by grants from the Ministerio de Economía y Competitividad (PSI2015‐68701‐R), Instituto de Salud Carlos III (ISCIII) ( INT19/00046 and PI17/01167) and co‐funded by FEDER funds /European Regional Development Fund (ERDF), a way to build Europe. CIBERobn, CIBERsam and CIBERDEM are all initiatives of ISCIII. GMB is supported by a postdoctoral grant from FUNCIVA. This initiative is supported by Generalitat de Catalunya. LM is supported by a postdoctoral grant of the Mexican institution Consejo Nacional de Ciencia y Tecnología (CONACYT). PPM was supported, in part, by a Portuguese Foundation for Science and Technology grant (POCI‐01‐0145‐FEDER‐028145). IB was partially supported by a Post‐Residency Grant from Research Committee of the University Hospital of Bellvitge (HUB; Barcelona, Spain) 2019‐2020. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Fernández‐Aranda F, Munguía L, Mestre‐Bach G, et al. COVID Isolation Eating Scale (CIES): Analysis of the impact of confinement in eating disorders and obesity—A collaborative international study. Eur Eat Disorders Rev. 2020;28:871–883. 10.1002/erv.2784
Funding information Fondo Investigación Sanitario‐ FIS, Grant/Award Numbers: FIS, INT19/00046, PI17/01167; Ministerio de Economía y Competitividad, Grant/Award Number: PSI2015‐68701‐R; Portuguese Foundation for Science and Technology grant, Grant/Award Number: POCI‐01‐0145‐FEDER‐028145; Consejo Nacional de Ciencia y Tecnología; Generalitat de Catalunya; European Regional Development Fund
REFERENCES
- Ahorsu, D. K. , Lin, C. Y. , Imani, V. , Saffari, M. , Griffiths, M. D. , & Pakpour, A. H. (2020). The fear of COVID‐19 scale: Development and initial validation. International Journal of Mental Health and Addiction, 27, 1–9. 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association, (2013). Diagnostic and statistical manual of mental disorders (5th ed.), Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Baenas, I. , Caravaca‐Sanz, E. , Granero, R. , Sánchéz, I. , Riesco, N. , Testa, G. , … Fernández‐Aranda, F. (2020). COVID‐19 and eating disorders during confinement: Analysis of factors associated with resilience and aggravation of symptoms (2020). European Eating Disorders Review. 10.1002/erv.2771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett, P. (2007). Structural equation modelling: Adjudging model fit. Personality and Individual Differences, 42(5), 815–824. 10.1016/j.paid.2006.09.018 [DOI] [Google Scholar]
- Brown, M. , Robinson, L. , Campione, G. C. , Wuensch, K. , Hildebrandt, T. , & Micali, N. (2017). Intolerance of uncertainty in eating disorders: A systematic review and meta‐analysis. European Eating Disorders Review, 25, 329–343. 10.1002/erv.2523 [DOI] [PubMed] [Google Scholar]
- Cao, W. , Fang, Z. , Hou, G. , Han, M. , Xu, X. , Dong, J. , & Zheng, J. (2020). The psychological impact of the COVID‐19 epidemic on college students in China. Psychiatry Research, 287, 112934. 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandu, V. C. , Pachava, S. , Vadapalli, V. , & Marella, Y. (2020). Development and initial validation of the COVID‐19 anxiety scale. Indian Journal of Public Health, 64, S201–S204. 10.4103/ijph.IJPH_492_20 [DOI] [PubMed] [Google Scholar]
- Claes, L. , Boekaerts, E. , Verschueren, M. , Boukaert, W. , & Luyckx, K. (2019). Identity statuses in prebariatric patients with obesity: Associations with eating disorder symptoms, psychological complaints, and coping behaviour? European Eating Disorders Review, 27, 410–420. 10.1002/erv.2681 [DOI] [PubMed] [Google Scholar]
- Clark Bryan, D. , Macdonald, P. , Ambwani, S. , Cardi, V. , Rowlands, K. , Willmott, D. , & Treasure, J. (2020). Exploring the ways in which COVID‐19 and lockdown has affected the lives of adult patients with anorexia nervosa and their carers. European Eating Disorders Review. 10.1002/erv.2762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power for the behavioral sciences (2nd ed.). Hillsdale, NJ: Laurence Erlbaum and Associates. [Google Scholar]
- Columb, D. , Hussain, R. , & O'Gara, C. (2020). Addiction psychiatry and COVID‐19‐impact on patients and service provision. Irish Journal of Psychological Medicine, 21, 1–5. 10.1017/ipm.2020.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, M. , Reilly, E. E. , Siegel, J. A. , Coniglio, K. , Sadeh‐Sharvit, S. , Pisetsky, E. M. , & Anderson, L. M. (2020). Eating disorders during the COVID‐19 pandemic and quarantine: An overview of risks and recommendations for treatment and early intervention. Eating Disorders., 9, 1–23. 10.1080/10640266.2020.1790271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornejo‐Pareja, I.M. , Gómez‐Pérez, A.M. , Fernández‐García, J.C. , Barahona San Millan, R. , Aguilera Luque, A. , de Hollanda, A. , Jiménez, A. , Jimenez‐Murcia, S. , Munguia, L. , Ortega, E. , Fernandez‐Aranda, F. , Fernández Real, J.M. and Tinahones, F. (2020). Coronavirus disease 2019 (COVID‐19) and obesity. Impact of obesity and its main comorbidities in the evolution of the disease. European Eating Disorders Review, 28; https://wiley.eproofing.in/Proof.aspx?token=2c87f8bf8630444d9e53479a04fd6632001224623 [DOI] [PubMed] [Google Scholar]
- Costantini, A. , & Mazzotti, E. (2020). Italian validation of CoViD‐19 Peritraumatic distress index and preliminary data in a sample of general population. Rivista di Psichiatria, 55(3), 145–151. 10.1708/3382.33570 [DOI] [PubMed] [Google Scholar]
- Darrow, S. M. , Accurso, E. C. , Nauman, E. R. , Goldschmidt, A. B. , & Le Grange, D. (2017). Exploring types of family environments in youth with eating disorders. European Eating Disorders Review, 25, 389–396. 10.1002/erv.2531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Girolamo, G. , Cerveri, G. , Clerici, M. , Monzani, E. , Spinogatti, F. , Starace, F. , … Vita, A. (2020). Mental health in the coronavirus disease 2019 emergency – the Italian response. JAMA Psychiatry. 10.1001/jamapsychiatry.2020.1276 [DOI] [PubMed] [Google Scholar]
- Fernández‐Aranda, F. , Casas, M. , Claes, L. , Bryan, D. C. , Favaro, A. , Granero, R. , … Treasure, J. (2020). COVID −19 and implications for eating disorders. European Eating Disorders Review, 28(3), 239–245. 10.1002/erv.2738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forte, G. , Favieri, F. , Tambelli, R. , & Casagrande, M. (2020). COVID‐19 pandemic in the Italian population: Validation of a post‐traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. International Journal of Environmental Research and Public Health, 17(11), 4151. 10.3390/ijerph17114151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granero, R. , Treasure, J., Claes, L., Favaro, A., Jiménez‐Murcia, S., Karwautz, A., … Fernández‐Aranda, F. (2020). Null hypothesis significance tests, a misleading approach to scientific knowledge: Some implications for eating disorders research. European Eating Disorders Review, 28(5), 483–491. http://dx.doi.org/10.1002/erv.2782. [DOI] [PubMed] [Google Scholar]
- Graell, M. , Morón‐Nozaleda, M. G. , Camarneiro, R. , Villaseñor, Á. , Yáñez, S. , Muñoz, … Faya, M. (2020). Children and adolescents with eating disorders during COVID‐19 confinement: Difficulties and future challenges. European Eating Disorders Review, 10.1002/erv.2763. [DOI] [PubMed] [Google Scholar]
- Håkansson, A. , Fernández‐Aranda, F. , Menchón, J. M. , Potenza, M. N. , & Jiménez‐Murcia, S. (2020). Gambling during the COVID‐19 crisis ‐ a cause for concern? Journal of Addiction Medicine, Publish Ahead of Print, 14, e10–e12. 10.1097/adm.0000000000000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewlett, B. L. , & Hewlett, B. S. (2005). Providing care and facing death: Nursing during Ebola outbreaks in Central Africa. Journal of Transcultural Nursing, 16(4), 289–297. 10.1177/1043659605278935 [DOI] [PubMed] [Google Scholar]
- Inchausti, F. , García‐Poveda, N. V. , Prado‐Abril, J. , & Sánchez‐Reales, S. (2020). La Psicología Clínica ante la Pandemia COVID‐19 en España. Clínica y Salud., 31, 105–107. 10.5093/clysa2020a11 [DOI] [Google Scholar]
- Kannarkat, J. T. , Smith, N. N. , & McLeod‐Bryant, S. A. (2020). Mobilization of Telepsychiatry in response to COVID‐19—Moving toward 21st century access to care. Administration and Policy in Mental Health and Mental Health Services Research, 47(4), 489–491. 10.1007/s10488-020-01044-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Stoddard J. (2020). The Coronavirus Impact Scale. Retreived from https://disasterinfo.nlm.nih.gov/search/?source=2587.
- Kelley, K. , & Preacher, K. (2012). On effect size. Psychological Methods, 17(2), 137–152. 10.1037/a0028086 [DOI] [PubMed] [Google Scholar]
- King, D. L. , Delfabbro, P. H. , Billieux, J. , & Potenza, M. N. (2020). Problematic online gaming and the COVID‐19 pandemic. Journal of Behavioral Addictions, 9, 184–186. 10.1556/2006.2020.00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsman, J. (2012). “A time of fear”: Local, national, and international responses to a large Ebola outbreak in Uganda. Globalization and Health, 8, 1–12. 10.1186/1744-8603-8-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Király, O. , Potenza, M. N. , Stein, D. J. , King, D. L. , Hodgins, D. C. , Saunders, J. B. , … Demetrovics, Z. (2020). Preventing problematic internet use during the COVID‐19 pandemic: Consensus guidance. Comprehensive Psychiatry, 100, 152180. 10.1016/j.comppsych.2020.152180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, J. , Ma, S. , Wang, Y. , Cai, Z. , Hu, J. , Wei, N. , … Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y. , Wang, H. , Jin, X. R. , Li, X. , Pender, M. , Song, C. P. , … Wang, Y. G. (2018). Experiences and challenges in the health protection of medical teams in the Chinese Ebola treatment center, Liberia: A qualitative study. Infectious Diseases of Poverty, 7, 1–12. 10.1186/s40249-018-0468-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linardon, J. , Shatte, A. , Tepper, H. , & Fuller‐Tyszkiewicz, M. (2020). A survey study of attitudes toward, and preferences for, e‐therapy interventions for eating disorder psychopathology. International Journal of Eating Disorders, 53(6), 907–916. 10.1002/eat.23268 [DOI] [PubMed] [Google Scholar]
- Main, A. , Zhou, Q. , Ma, Y. , Luecken, L. J. , & Liu, X. (2011). Relations of sars‐related stressors and coping to chinese college students' psychological adjustment during the 2003 Beijing sars epidemic. Journal of Counseling Psychology, 58(3), 410–423. 10.1037/a0023632 [DOI] [PubMed] [Google Scholar]
- Mallorquí‐Bagué, N. , Vintró‐Alcaraz, C. , Sánchez, I. , Riesco, N. , Agüera, Z. , Granero, R. , … Fernández‐Aranda, F. (2018). Emotion regulation as a Transdiagnostic feature among eating disorders: Cross‐sectional and longitudinal approach. European Eating Disorders Review, 26(1), 53–61. 10.1002/erv.2570 [DOI] [PubMed] [Google Scholar]
- Marsden, J. , Darke, S. , Hall, W. , Hickman, M. , Holmes, J. , Humphreys, K. , … West, R. (2020). Mitigating and learning from the impact of COVID‐19 infection on addictive disorders. Addiction, 115(6), 1007–1010. 10.1111/add.15080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonnell, W. M. , Nelson, D. S. , & Schunk, J. E. (2012). Should we fear “flu fear” itself? Effects of H1N1 influenza fear on ED use. American Journal of Emergency Medicine, 30(2), 275–282. 10.1016/j.ajem.2010.11.027 [DOI] [PubMed] [Google Scholar]
- Mestre‐Bach, G. , Blycker, G. R. , & Potenza, M. N. (2020). Pornography use in the setting of the COVID‐19 pandemic. Journal of Behavioral Addictions, 9, 181–183. 10.1556/2006.2020.00015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihashi, M. , Otsubo, Y. , Yinjuan, X. , Nagatomi, K. , Hoshiko, M. , & Ishitake, T. (2009). Predictive factors of psychological disorder development during recovery following SARS outbreak. Health Psychology, 28(1), 91–100. 10.1037/a0013674 [DOI] [PubMed] [Google Scholar]
- Papandreou, C. , Tsilidis, K. K. , Arija, V. , Aretouli, E. , & Bulló, M. (2020). Comparing eating behaviours, and symptoms of depression and anxiety between Spain and Greece during the COVID‐19 outbreak: Cross‐sectional analysis of two different confinement strategies. European Eating Disorders Review. 10.1002/erv.2772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce, M. ,, Hope, H., Ford, T., Hatch, S., Hotopf, M., John, A., … Abel, K. M. (2020). Mental health before and during the COVID‐19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 10.1016/s2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raven, J. , Wurie, H. , & Witter, S. (2018). Health workers' experiences of coping with the Ebola epidemic in Sierra Leone's health system: A qualitative study. BMC Health Services Research, 18, 1–9. 10.1186/s12913-018-3072-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riesco N., Agüera, Z., Granero, R., Jiménez‐Murcia, S., Menchón, J.M., Fernández‐Aranda, F. (2018). Other Specified Feeding or Eating Disorders (OSFED): Clinical heterogeneity and cognitive‐behavioral therapy outcome. European Psychiatry, 54, 109–116. http://dx.doi.org/10.1016/j.eurpsy.2018.08.001. [DOI] [PubMed] [Google Scholar]
- Rodgers, R. F. , Lombardo, C. , Cerolini, S. , Franko, D. L. , Omori, M. , Fuller‐Tyszkiewicz, M. , … Guillaume, S. (2020). The impact of the COVID‐19 pandemic on eating disorder risk and symptoms. International Journal of Eating Disorders, 53(7), 1166–1170. 10.1002/eat.23318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi, R. , Socci, V. , Pacitti, F. , Di Lorenzo, G. , Di Marco, A. , Siracusano, A. , & Rossi, A. (2020). Mental health outcomes among frontline and second‐line health care workers during the coronavirus disease 2019 (COVID‐19) pandemic in Italy. JAMA Network Open, 3(5), e2010185. 10.1001/jamanetworkopen.2020.10185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rundle, A. G. , Park, Y. , Herbstman, J. B. , Kinsey, E. W. , & Wang, Y. C. (2020). COVID‐19‐related school closings and risk of weight gain among children. In Obesity (Vol. 28, Issue 6, pp. 1008–1009). Blackwell Publishing Inc. 10.1002/oby.22813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakib, N. , Bhuiyan, A. K. M. I. , Hossain, S. , Al Mamun, F. , Hosen, I. , Abdullah, A. H. , … Mamun, M. A. (2020). Psychometric validation of the Bangla fear of COVID‐19 scale: Confirmatory factor analysis and Rasch analysis. International Journal of Mental Health and Addiction. 10.1007/s11469-020-00289-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, K. , Ostinelli, E. , Macdonald, O. , & Cipriani, A. (2020). COVID‐19 and telepsychiatry: An evidence‐based guidance for clinicians. JMIR Mental Health. 10.2196/21108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soraci, P. , Ferrari, A. , Abbiati, F. A. , Del Fante, E. , De Pace, R. , Urso, A. , & Griffiths, M. D. (2020). Validation and psychometric evaluation of the Italian version of the fear of COVID‐19 scale. International Journal of Mental Health and Addiction, 1–10. 10.1007/s11469-020-00277-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stata Press . (2019). Stata statistical software: Release 16. Texas: StataCorp LLC. [Google Scholar]
- Strand, M. , von Hausswolff‐Juhlin, Y. , Fredlund, P. , & Lager, A. (2019). Symptoms of disordered eating among adult international adoptees: A population‐based cohort study. European Eating Disorders Review, 27, 236–246. 10.1002/erv.2653 [DOI] [PubMed] [Google Scholar]
- Sun, Y. , Li, Y. , Bao, Y. , Meng, S. , Sun, Y. , Schumann, G. , … Shi, J. (2020). Brief report: Increased addictive internet and substance use behavior during the COVID‐19 pandemic in China. The American Journal on Addictions, 29(4), 268–270. 10.1111/ajad.13066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, S. , Landry, C. A. , Paluszek, M. M. , Fergus, T. A. , McKay, D. , & Asmundson, G. J. G. (2020). Development and initial validation of the COVID stress scales. Journal of Anxiety Disorders, 72, 102232. 10.1016/j.janxdis.2020.102232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Termorshuizen, J. D. , Watson, H. J., Thornton, L. M., Borg, S., Flatt, R. E., MacDermod, C. M., … Bulik, C. M. (2020). Early impact of COVID ‐19 on individuals with self‐reported eating disorders: A survey of ~1,000 individuals in the United States and the Netherlands. International Journal of Eating Disorders, http://dx.doi.org/10.1002/eat.23353. [DOI] [PubMed] [Google Scholar]
- Todisco, P. , & Donini, L. M. (2020). Eating disorders and obesity (ED&O) in the COVID‐19 storm. Eating and Weight Disorders. 10.1007/s40519-020-00938-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treasure, J. , Gavan, K. , Todd, G. , & Schmidt, U. (2003). Changing the environment in eating disorders: Working with carers/families to improve motivation and facilitate change. European Eating Disorders Review, 11, 25–37. 10.1002/erv.485 [DOI] [Google Scholar]
- Vanzhula, I. A. , Calebs, B. , Fewell, L. , & Levinson, C. A. (2019). Illness pathways between eating disorder and post‐traumatic stress disorder symptoms: Understanding comorbidity with network analysis. European Eating Disorders Review, 27, 147–160. 10.1002/erv.2634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vintró‐Alcaraz, C. , Mestre‐Bach, G. , Steward, T. , Lozano‐Madrid, M. , Agüera, Z. , Jiménez‐Murcia, S. , … Fernández‐Aranda, F. (2018). Validation of the Caregiver Skills (CASK ) scale in Catalonia: Concordance between caregivers in attitudes and behaviours. European Eating Disorders Review, 26, 329–336. 10.1002/erv.2604 [DOI] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C. S. , & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Y. , Di, Y. , Ye, J. , & Wei, W. (2020). Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID‐19) in some regions of China. Psychology, Health and Medicine, 1–10. 10.1080/13548506.2020.1746817 [DOI] [PubMed] [Google Scholar]
- Wu, P. , Fang, Y. , Guan, Z. , Fan, B. , Kong, J. , Yao, Z. , … Hoven, C. (2009). The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk NIH public access. Canadian Journal of Psychiatry, 54(5), 302–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Scheme of the CFA in the study
Table S1 and Table S2 Description of the sample and Standardised coefficients obtained in the CFA
CIES Scale v.1.0 (Translation in 19 Languages: English‐Spanish‐Catalan‐French‐Portuguese‐Italian‐German‐Swedish‐Czech‐Lithuanian‐Dutch‐Russian‐Hungarian‐Georgian‐Hebrew‐Japanese‐Korean‐Chinese‐Ukrainian).


