Dear Editor,
Coronavirus disease 2019 also known as COVID‐19 (caused by the new coronavirus known as SARS‐CoV‐2) has established itself as a global pandemic with significant debilitating effects primarily targeting the respiratory system. 1 COVID‐19 pneumonia is characterized by a general inflammation in endothelial cells affecting multiple organ systems predisposing to vascular thrombosis. 1
Age and obesity are the biggest COVID‐19 risk factors. 2 There is also accumulating evidence that Black, Asian, and Minority Ethnic (BAME) groups in the UK are at increased risk of complications from COVID‐19. 3
Pregnancy further increases the risks of COVID‐19 complications particularly thrombotic complications. 4
The ABO blood group system was established by Karl Landsteiner, who classified blood groups according to the existence of A and B antigens on the surface of red blood cells. 5 An individual with A antigen has blood group A; B antigen blood group B; A and B antigens blood group AB, whilst individuals with blood group O have neither antigen. Blood group A individuals have antibodies against B antigen (anti‐B); blood group B have anti‐A; blood group AB have neither anti‐A nor anti‐B, and blood group O have both anti‐A and anti‐B antibodies. Since the discovery of the ABO blood group system, numerous studies have been undertaken to study the link between the ABO blood group system and diseases. 5 It had been identified that there is an association between ABO blood group and the risk of developing the severe acute respiratory syndrome (also known as SARS caused by SARS‐CoV‐1 infection) and the severity of associated complictions. 6
Consequently, we looked at the relative frequency of blood groups A, B, AB and O in pregnancy in two multiethnic UK cities (Leicester and Birmingham).
The maternity units at University Hospitals of Leicester (UHL) and University Hospitals of Birmingham (UHB) are both tertiary referral centres, each delivering approximately 10,000 births per year. At UHL (16th March to 23rd April 2020) and UHB (20th March to 5th May 2020), nose and throat swabs were performed on women presenting with symptoms suggestive of COVID‐19. From 24th April 2020 and 6th May 2020, respectively, all women admitted to both maternity units were swabbed to test for asymptomatic COVID‐19. As part of service evaluation at both UHL and UHB, data [age, body mass index (BMI), ethnicity, ABO blood group and COVID‐19 swab result] were collected anonymously in real time. ICE and E3 maternity system were used to obtain the data at UHL, whilst UltraAgenda and BadgerNet maternity system were used to obtain the data at UHB.
The ABO blood group in 185 COVID‐19 negative pregnant women in Leicester showed a frequency distribution of 35%, 16%, 8% and 42% for A, B, AB and O, respectively (Figure 1A and Table 1). On the other hand, the ABO blood group in 44 COVID‐19 positive pregnant women in Leicester showed a frequency distribution of 39%, 20%, 16% and 25% for A, B, AB and O, respectively (Figure 1A and Table 1).
FIGURE 1.

A, Relative frequency, expressed as a percentage, for blood groups A, B, AB and O, separated into women who were COVID‐19 positive (n = 44) and COVID‐19 negative (n = 185) in Leicester. B, Relative frequency, expressed as a percentage, for blood groups A, B AB and O, separated into women who were COVID‐19 positive (n = 42) and COVID‐19 negative (n = 84) in Birmingham. C, Relative frequency, expressed as a percentage, for blood groups A, B, AB and O (combined Leicester and Birmingham) separated into women who were COVID‐19 positive (n = 86) and COVID‐19 negative (n = 269)
Table 1.
ABO blood group and COVID‐19 status—Leicester (L) and Birmingham (B)
| COVID‐19 status | Region | ABO blood group frequency (%) | Total | |||
|---|---|---|---|---|---|---|
| A (n, [%]) | B (n, [%]) | AB (n, [%]) | O (n, [%]) | |||
| COVID‐19 positive | Leicester | 17 (39%) | 9 (20%) | 7 (16%) | 11 (25%) | 44 (100%) |
| COVID‐19 negative | Leicester | 64 (35%) | 29 (16%) | 14 (8%) | 78 (42%) | 185 (101% rounded) |
| COVID‐19 positive | Birmingham | 17 (40%) | 10 (24%) | 5 (12%) | 10 (24%) | 42 (100%) |
| COVID‐19 negative | Birmingham | 28 (33%) | 19 (23%) | 3 (4%) | 34 (40%) | 84 (100%) |
| COVID‐19 positive | All (Leicester and Birmingham) | 34 (40%) | 19 (22%) | 12 (14%) | 21 (24%) | 86 (100%) |
| COVID‐19 negative | All (Leicester and Birmingham) | 92 (34%) | 48 (18%) | 17 (6%) | 112 (42%) | 269 (100%) |
The ABO blood group in 84 COVID‐19 negative pregnant women in Birmingham displayed a frequency distribution of 33%, 23%, 4% and 40% for A, B, AB and O, respectively (Figure 1B and Table 1). Conversely, the ABO blood group in 42 COVID‐19 positive pregnant women in Birmingham revealed a frequency distribution of 40%, 24%, 12% and 24%for A, B, AB and O, respectively (Figure 1B and Table 1).
Leicester and Birmingham combined the ABO blood group in 269 COVID‐19 negative pregnant women exhibited a frequency distribution of 34%, 18%, 6% and 42% for A, B, AB and O, respectively (Figure 1C and Table 1). In contrast, the ABO blood group in 86 COVID‐19 positive pregnant women combined showed a frequency distribution of 40%, 22%, 14% and 24% for A, B, AB and O, respectively (Figure 1C and Table 1).
The chi‐square test of independence was performed to determine the statistical significance of the relationship between ABO blood group and COVID‐19 status. ABO blood group was found to be significantly associated with COVID‐19 status (P = .012), and the AO blood groups were even more strongly associated (P < .001). Although pregnant women in our cohort were more likely to be blood group O, blood group A women had a significantly higher relative risk of developing COVID‐19 infection (RR 1.71 [95% Confidence Interval: 1.05‐2.78]).
Taken together, our data suggest that the risk for COVID‐19 is higher with blood group A and lower with blood group O. In line with this hypothesis, it has been reported that blood group O individuals were less susceptible to SARS (caused by SARS‐CoV‐1 infection). 6
SARS‐CoV‐2 can replicate in epithelial cells that express A and B antigens in the lungs 7 ; individuals with blood group O have both anti‐A and anti‐B antibodies, which could target SARS‐CoV‐2 infected lung epithelial cells, thus, offering protection to these individuals.
Further, as mentioned above, pregnancy increases the risks of thrombotic complications associated with COVID‐19 infection. 4 Individuals with blood group O have lower biologic activity and circulating concentrations of vWF (von Willebrand factor), a carrier protein for coagulation factor VIII critical to blood coagulation, leading to lower risks of thromboembolic diseases. 5
The percentage distribution of ethnicity in the COVID‐19 negative pregnant women group was 47% White European and 53% BAME (Black, Asian and Minority Ethnic) whereas in the COVID‐19 positive pregnant women group was 22% White European and 78% BAME; this is in keeping with the higher risk of COVID‐19 in BAME groups. 3 Notably, the pattern of higher blood group A and lower blood group O frequency distributions in COVID‐19 positive pregnant women, according to ethnic group (Figure 2A and Table 1), was similar to Figure 1A‐C; this pattern was most accentuated in the BAME group (Figure 2B and Table 1). The average age of COVID‐19 negative women was 31 years and 30 years in the COVID‐19 positive group, and the average BMI for the COVID‐19 negative group was 26 and for the COVID‐19 positive group was 27, which was not significantly different.
FIGURE 2.
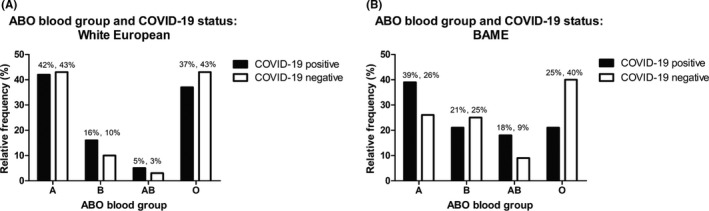
A, Relative frequency, expressed as a percentage, for blood groups A, B, AB and O, in White European women separated into COVID‐19 positive (n = 19) and COVID‐19 negative (n = 127). B, Relative frequency, expressed as a percentage, for blood groups A, B, AB and O, in BAME (Black, Asian and Minority Ethnic) women separated into COVID‐19 positive (n = 66) and COVID‐19 negative (n = 142)
In summary, we present novel data specifically in pregnant women who are an important cohort to consider, given the increased risk of COVID‐19 infection in pregnant women. Our findings imply that pregnant women with blood group A would require extra vigilance from clinicians and carers and may warrant more personal protection to lower the risks of COVID‐19 infection.
CONFLICT OF INTEREST
The authors have no competing interests.
AUTHOR CONTRIBUTIONS
IA and LQ collected the data for the manuscript. BKT wrote the manuscript. All authors reviewed, edited and approved submission of the manuscript.
ACKNOWLEDGEMENTS
We would like to acknowledge Stevie Comery‐Lang and Rebecca Crook for assisting with the data collection at University Hospitals Leicester.
Lauren Quinn and Bee K. Tan are joint senior authors.
REFERENCES
- 1. Price LC, McCabe C, Garfield B, Wort SJ. Thrombosis and COVID‐19 pneumonia: the clot thickens!. Eur Respir J. 2020;56:2001608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid‐19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Townsend MJ, Kyle TK, Stanford FC. Outcomes of COVID‐19: disparities in obesity and by ethnicity/race. Int J Obes (Lond). 2020;44(9):1807‐1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ahmed I, Azhar A, Eltaweel N, Tan BK. First COVID‐19 maternal mortality in the UK associated with thrombotic complications. Br J Haematol. 2020;190(1):e37‐e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Groot HE, Villegas Sierra LE, Said MA, Lipsic E, Karper JC, van der Harst P. Genetically determined ABO blood group and its associations with health and disease. Arterioscler Thromb Vasc Biol. 2020;40(3):830‐838. [DOI] [PubMed] [Google Scholar]
- 6. Cheng Y, Cheng G, Chui CH, et al. ABO blood group and susceptibility to severe acute respiratory syndrome. JAMA. 2005;293(12):1450‐1451. [DOI] [PubMed] [Google Scholar]
- 7. Sano R, Nakajima T, Takahashi Y, et al. Epithelial expression of human ABO blood group genes is dependent upon a downstream regulatory element functioning through an epithelial cell‐specific transcription factor, Elf5. J Biol Chem. 2016;291(43):22594‐22606. [DOI] [PMC free article] [PubMed] [Google Scholar]


