1.
As the COVID‐19 pandemic continues to expand throughout the world, innovative methods are required to involve residents in the care of critically ill COVID‐19 patients. The disease is caused by highly infectious novel corona virus (SARS‐CoV‐2) transmitted via respiratory droplets and direct contact (1). Health care providers in intensive care units (ICUs) are on the frontline to take care of increasing numbers of critically ill COVID‐19 patients. Residents who are rotating in the ICU are at high risk of acquiring the virus while treating COVID‐19 patients. The main objectives are to provide optimal care to patients and adequate clinical training while minimising the risk of acquiring the infection and ensuring safety and well‐being of the residents.
Tele‐Medicine is a practice of medicine in which health care providers utilise the telecommunication technologies to deliver health care, diagnoses and treatments, to patients remotely (2). In this context, the providers conduct communication with patients, families and/or the bedside caring team from a geographically distant location by using variety of technologies to provide and promote care to patients in a different site. Telecommunication systems may range from highly advanced audiovisual systems with cameras installed in patient’s rooms to using portable computers, phones and other mobile devices to conduct required clinical activities, clinical consultations and follow‐ups, and patient and family conferences. As intensive care specialists in our institution, in this paper we reflect on our experiences of using a tele‐ICU model during the pandemic.
In the United States, the Accreditation Council for Graduate Medical Education (ACGME) has recognised that institutions and training programs are deploying telemedicine to assist trainees in taking care of patients with COVID‐19 remotely. ACGME permitted residents and fellows to participate in the use of telemedicine to care for patients who are affected by the pandemic to decrease the risk of exposure and promote residents and fellows’ safety (3).
Tele‐Medicine models in the ICU, tele‐ICU, have historically been used to provide care to seriously ill patients by offsite health care providers. These models have been associated with the improved clinical outcomes of ICU patients and effective supervision and education of trainees. Studies have shown that tele‐ICU have a significant positive impact on education and improved patient safety and quality of care among residents (4, 5). In order to offer adequate care to an overwhelmingly high number of critically ill COVID‐19 patients in conjunction with the demand of ensuring residents safety and well‐being, tele‐ICU can be a valuable solution during the current pandemic.
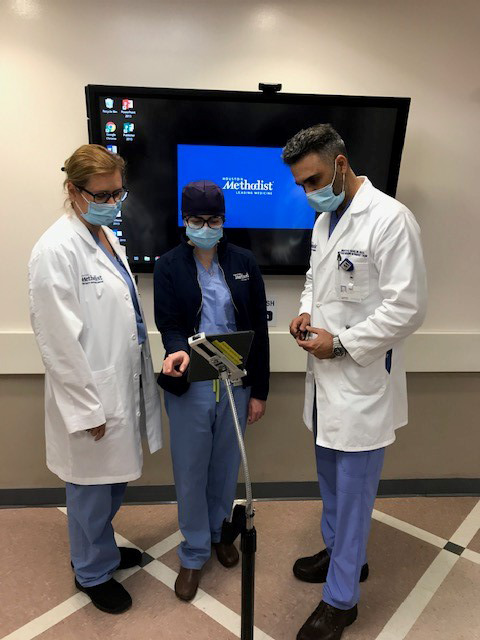
Intensive care unit specialists in our institution started to utilise tele‐ICU during COVID‐19 pandemic. Tele‐ICU was deployed throughout the day in the medical ICU, a 24‐bed unit dedicated to care for COVID‐19 critically ill patients. The tele‐ICU system includes adjustable high‐resolution cameras throughout the room, a two‐way audio system and direct digital connection to the monitoring system, allowing the team to view the patient, vital signs monitors, mechanical ventilation settings, intravenous infusions and rates, and other organs supportive devices, and to communicate with the caring nursing staff from a distant location. The residents and faculty members can manage patients without being in direct contact or inside the room. Direct care is limited to trained faculty members, while residents communicate with the nursing staff, patients and families via the audiovisual tele‐ICU system. Although the residents are still in the ICU conducting regular daily tasks and interacting with the multidisciplinary teams, they are not in direct contact with COVID‐19 patients. This approach in provision of care can achieve many goals, specifically, adequate education to trainees, effective communication with the nursing staff, patients and their families, and enhanced safety and well‐being of residents. The disadvantages of this model are the lack of hands‐on experience and involvement in ICU bedside procedures. Another obstacle in implementing tele‐ICU model is the high cost of the infrastructure to set such an advanced system. One of the solutions that can be adopted by ICU specialists who do not have tele‐ICU system available in the hospital is to use alternative tools to achieve the same objectives. Such tools may include phones, portable computers or other mobile and wireless communication devices. In evaluating the benefits and limitations of tele‐ICU models in caring for COVID‐19 patients, ICU specialists in our hospital consider the use of tele‐ICU model in treating highly infectious COVID‐19 ICU patients is superior for residents as it offers adequate education, higher safety and sense of well‐being. It can be applied as a substitute method for residents who are caring for seriously ill patients infected with novel corona virus in the ICU. Several telecommunication technologies can be utilised to serve the purpose such as portable computers, phones, and other mobile and wireless communication devices.
Tele‐ICU is a unit equipped with audiovisual telecommunication capabilities to enable health care providers to deliver care to patients remotely.
Utilising tele‐ICU in caring for critically ill COVID‐19 patients can provide adequate education and higher safety for residents.
References
- 1. Otter Ja, Donskey C, Yezli S, Douthwaite S, Goldenberg Sd, Weber Dj, et al. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. J Hosp Infect. 2016;92(3):235–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. NEJM catalyst . What Is Telehealth? Catalyst.nejm.org. 2020; https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0268 [Google Scholar]
- 3. ACGME response to the Coronavirus (COVID‐19). https://acgme.org/Newsroom/Newsroom‐Details/ArticleID/10111/ACGME‐Response‐to‐the‐Coronavirus‐COVID‐19
- 4. Coletti C, Elliott D, Zubrow M. Resident perceptions of a tele‐intensive care unit implementation. Telemed J E Health. 2010;16(8):894–897. [DOI] [PubMed] [Google Scholar]
- 5. Mora A, Faiz S, Kelly T, Castriotta R, Patel B. Resident perception of the educational and patient care value from remote telemonitoring in a medical intensive care unit. Chest. 2007;132(4):443A. [Google Scholar]


