Abstract
Background
The COVID‐19 pandemic posed a great challenge to paediatric dentistry, which confronted with the restriction of service and resource shortage.
Aim
To retrospectively analyse the information of children's dental online health consultation during the COVID‐19 pandemic in China, and to provide methods to distinguish between dental emergencies and non‐emergencies as well as their management.
Design
We collected all the online consultation information in Dept. of Paediatric dentistry, School & Hospital of Stomatology, Wuhan University, from 2 February to 31 March 2020, and extracted the information of age, gender, reason for consultation, description of symptom, and preliminary diagnosis of the children.
Results
A total of 474 online consultations of paediatric dentistry were included within 59 days during lockdown, and 190 (40.1%) were dental emergencies and 284 (59.9%) non‐emergencies. Of 190 emergency consultations, 186 (97.9%) showed swelling, pain, and trauma with or without systemic symptoms. Among 284 non‐emergency consultations, retained primary teeth (n = 126) and orthodontic consultation (n = 53) were the most common reasons for consultation.
Conclusion
The paediatric emergency and non‐emergency problems should be clearly distinguished and sufficient instructions provided in the special period of COVID‐19. Priorities also should be set to deal with urgent conditions after the release of lockdown.
Keywords: COVID‐19, emergency management, online consultation, paediatric dentistry
1. INTRODUCTION
COVID‐19 pandemic has caused more than 7.0 million cases worldwide as of 9 June 2020, according to World Health Organization. 1 In China, in order to control the spread of the pandemic, Wuhan adopted a strict lockdown from 23 January until 8 April. 2 , 3 During the 76‐day blockade period, more than 1.3 million children in Wuhan were staying at home. 4 At the same time, all dental clinics, as well as paediatric departments, closed down. 5 , 6 The COVID‐19 has been exposing challenges to basic medical service, especially the dental service.
Compared to adults, children are more prone to injury, 7 poor oral hygiene, and high frequency of intake of desserts because of a lively nature and irregular living habits. The need to spend the whole day in a home setting under pandemic can stimulate more unhealthy eating habits and active play modes in the children, with an increased risk of caries and traumatic events. 8 , 9 , 10 , 11 In addition, retained primary teeth and malocclusion are also common in children. 12 There has been an increasing contradiction between the huge paediatric demands and the limited medical resources with the outbreak of the pandemic.
It is precisely during the COVID‐19 pandemic period that a specific classification of dental emergencies and dental non‐emergencies becomes of crucial importance. 7 , 13 Some potentially life‐threatening real dental emergencies such as uncontrolled bleeding, diffuse soft‐tissue bacterial infection and maxillofacial fractures occur by accident. 14 , 15 However, the most common reason for dental‐related emergency department visits was not a matter of life‐and‐death such as dental caries and trauma. 9 , 16 Dental non‐emergencies that do not require immediate intervention can take palliative measures to reduce the occupation of emergency visit and minimize infection risk of COVID‐19. 7 , 14
Attention has been aroused by various dental organizations due to the complexity of paediatric emergency during COVID‐19 lockdown. 14 , 17 However, there has been no relative studies available related to this issue yet. We retrospectively analysed the situation of children's dental health during COVID‐19 based on the information of dental network consultation. The main distinguishing methods and the principle of treatment priority for children's dental emergencies were put forward, and the management of children's dental emergencies was provided.
2. METHODS
2.1. Study design
This retrospective study was carried out at the paediatric department of Wuhan University Stomatology Hospital, the main centre for the routine treatment and care of children dental diseases related to both emergencies and non‐emergencies in the city of Wuhan. In lockdown, the department was closed and all the staffs were trained to provide online consultation between 8:00 to 17:00 on duty in turn every day. All the online consultation information of 474 consultants (≤18 years old) from the personal computer terminal of the paediatric department of Wuhan University Stomatology Hospital from 2 February to 31 March 2020 were included.
This online doctor consultation system, as a model of telemedicine, was distributed in order to minimize unnecessary emergency visits, where dentists instructed parents remotely to take preventive measures and daily oral health care for children. All the online consulting services were free of charge during the pandemic. Two types of online consultation methods were available: graphic consultation and video consultation. The consulting parents followed the instruction of the WeChat's official blog of Wuhan University Stomatology Hospital and clicked ‘Online Inquiry’ to enter the interface. Parents could enter the reservation interface by following the steps to fill in the name, ID number and mobile phone number for real‐name authentication. After selecting the department, they could initiate a ‘video consultation’ or ‘graphic consultation’, and describe the condition of their children.
During the consultation process, the consultants would submit the main symptoms of children and provide a series of photos of the face, teeth, and soft tissue in the complaint area. After going through the information, the dentists on duty would further inquiry about the symptoms, including the nature, duration, and inducement of the pain. Other information that would be helpful for diagnoses could also be supplemented, for example, photos of previous medical records and drugs taken, or videos of abnormal pronunciation and bad oral habits of the children. Therefore, the dentists could get relatively sufficient information and give corresponding suggestions.
According to the chief complaint and the description of the condition of the consultants, the consultations were divided into real emergencies, abscess or swelling, pain (due to caries, periapical inflammation or ulcer), trauma (deciduous teeth, permanent teeth or soft tissue), non‐emergency consultation. The age of the consulting children was divided into four groups: 0‐3 years old, 3‐6 years old, 6‐12 years old and above 12 years old. The consultation distribution of children in different age groups was compared to determine the proportion of children's dental emergencies and non‐emergency conditions. This study was approved by the Medical Ethics Committee of Wuhan University Stomatology Hospital (2020‐B28). Because we could not contact the subjects, there was no informed consent. The two examiners (FY and LY) confirmed the consultation classification and possible clinical diagnosis (Appendix S1).
2.2. Definitions
2.2.1. Dental emergency
Real dental emergency is potentially life‐threatening and requires immediate treatment to stop the deterioration of health condition, for example, uncontrolled bleeding and airway obstruction. 13 , 14
Urgent dental care focuses on the management of conditions that require immediate attention to relieve pain and/or reduce the risk of infection and to alleviate the burden on hospital emergency departments. 14
2.2.2. Dental non‐emergency
Dental non‐emergency is defined as routine or non‐urgent dental procedures such as aesthetic dental procedures. 14
2.3. Data collection
The original information of each online consulting child was extracted by two researchers (FY and LY) who had been trained in data collection independently and in duplicate. Then, they cross‐checked the accuracy of the original data. All disagreements were resolved by discussion until an excellent agreement was reached (Kappa >80%). All the personal information was removed. The extracted information included age, gender, the reason for consultation, symptom description, initial diagnosis, times of consultations, consultation duration, and online consultation method. For the missing data in the records, we tried to extract the image and video information in the original record for the supplement. Then, all data were verified by another researcher (GS).
2.4. Statistical analysis
The Statistical package for Social Sciences (SPSS, version 23.0) was used to encode and analyse the data. A descriptive analysis of all variables was performed. Categorical variables were presented as frequency (percentage). The Pearson chi‐square test followed by pairwise comparisons adjusted by Bonferroni correction was used to analyse categorical variables among children of different age groups. Two‐sided P < .05 was considered statistically significant.
3. RESULTS
A total of 474 online consultations of paediatric dentistry were included within 59 days. The average number of consultations per day was 8.25, and each consultation took about 28 minutes on average. The characteristics of online consultation are shown in Table 1. Due to the imperfectness of the online consultation system in the early stage, some age and gender data were missing. Consultation method was mainly graphic consultation (85.7%). The incidence of paediatric emergencies (40.1%) was slightly lower than non‐emergencies (59.9%). Sixteen cases of special urgent conditions were reported, including children with fever (2.1%), children with facial swelling (3.2%) and children with systemic diseases (0.2%). Forty children (8.4%) had already taken medicine, such as cephalosporin, amoxicillin and ibuprofen to control the inflammation before the consultation. There were also 123 parents (25.9%) expressing concern about missing the optimal time for treatment because some children were in the treatment period like root canal treatment, orthodontic treatment.
TABLE 1.
Descriptive characteristics of online consultation in paediatric dentistry department (N = 474)
| Variables | N (%) |
|---|---|
| Gender a | |
| Male | 129 (27.2) |
| Female | 172 (36.3) |
| Age a | |
| 0‐3 y | 54 (11.4) |
| 3‐6 y | 155 (32.7) |
| 6‐12 y | 139 (29.3) |
| 12‐18 y | 0 (0.0) |
| Consultation type | |
| Graphic | 406 (85.7) |
| Video | 68 (14.3) |
| Dental emergency | |
| Emergency | 190 (40.1) |
| Non‐emergency | 284 (59.9) |
| Special condition | |
| Fever | 10 (2.1) |
| Facial swelling | 15 (3.2) |
| Systemic disease | 1 (0.2) |
| Postponement of return visit | 123 (25.9) |
| Medicine taking | 40 (8.4) |
Data were partially missing.
As shown in Figure 1, the majority (97.9%) of 190 consultations of dental emergencies showed swelling, pain, trauma with or without systemic symptoms. Only one case of all online consultations was classified as real dental emergency, uncontrolled bleeding, which was reported by a 6 years old child suffering from deciduous tooth trauma with haemophilia A. As for urgent dental care, there were mainly three kinds of chief complaints: abscess/swelling, pain and dental trauma. First, pure gingival abscess caused by localized bacterial infection was the most common, 65 consultations in total, accounting for 13.7%. Meanwhile, facial swelling with or without systemic symptom, such as fever and malaise, accounted for 15 times. Second, 60 consultations (12.6%) reported severe dental pain caused by deep caries or pulpitis. Ten consultations (2.1%) during or after root canal therapy presented with mastication or occlusive pain without swelling. Pain with fever, headache, sore throat or enlarged lymph nodes caused by herpetic gingivostomatitis was reported four times. Among dental trauma, consultants with primary tooth trauma were 17 children (3.6%), which were slightly more than children with permanent tooth trauma (2.1%). In addition, four consultations reported soft‐tissue trauma, including tongue injury, lip laceration, and a stab wound in the gingiva. Other problems for consultation including one recurrent parotitis, one non‐oral emergency (fishbone stuck in the throat), and two cases of unclear injury were also recorded in the online consultation.
FIGURE 1.
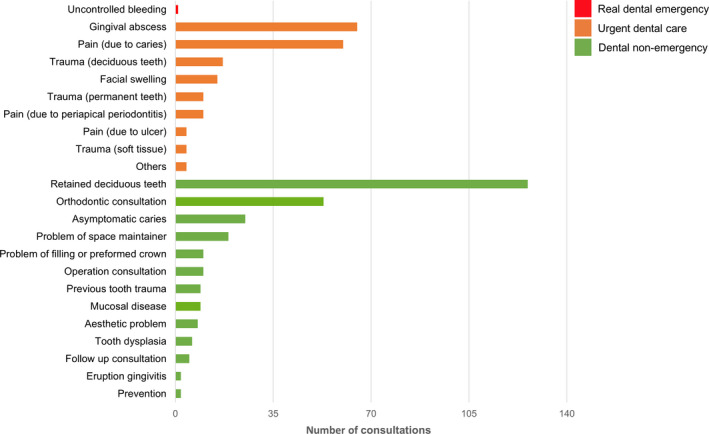
Distribution of number of real dental emergency, urgent dental care, and dental non‐emergency (N = 474)[Colour figure can be viewed at wileyonlinelibrary.com]
Among the 284 times of dental non‐emergencies, most consultations reported retained deciduous teeth (26.6%) and orthodontic consultations (11.2%), with 126 times and 53 times respectively. Asymptomatic caries (5.3%) were consulted 25 times. Nineteen consultations concerned about the problems associated with the space maintainer whereas ten consultations were related to the trouble of fillings or preformed metal crowns. Other non‐emergencies including surgery consultation, previous tooth trauma, mucosal disease, aesthetic problems were reported 51 times in total.
Table 2 shows the age‐related characteristics. There were 348 times of consultation reporting clear ages among all the 474 consultations, and no one had been reported in the group of over 12 years old. Most of the consultations were in the groups of 3‐6 and 6‐12 years old, 155 times (44.5%) and 139 times (40.0%) respectively. Consultations of pain were significantly more in the group of 3‐6 years old than the other two groups (P < .001). The proportion of dental emergency in the 3‐6 age group was significantly higher than the 6‐12 group (P = .007). The most frequently reported traumatic injuries were in the group of 0‐3 years old (P < .001). There was no significant difference in medicine taking between age groups (P = .276).
TABLE 2.
Characteristics of online consultation for children of different age groups
| Variables | Sub‐group | Number of consultations (%) | P value | |||
|---|---|---|---|---|---|---|
|
0‐3 y (n = 54) |
3‐6 y (n = 155) |
6‐12 y (n = 139) |
Total (n = 348) |
|||
| Consultations | Abscess/swelling | 5 (9.3)a | 34 (21.9)a | 17 (12.2)a | 56 (16.1) | .026* |
| Pain | 2 (3.7)a | 40 (25.8)b | 15 (10.8)a | 57 (16.4) | <.001* | |
| Trauma | 16 (29.6)a | 3 (1.9)b | 10 (7.2)b | 29 (8.3) | <.001* | |
| Non‐urgent consultation | 31 (57.4)a,b | 78 (50.3)b | 95 (68.3)a | 204 (58.6) | .007* | |
| Dental emergency | Emergency | 23 (42.6)a,b | 77 (49.7)b | 44 (31.7)a | 144 (41.3) | .007* |
| Medicine taking | Yes | 3 (5.6) | 19 (12.2) | 11 (7.9) | 33 (9.5) | .276 |
a,bGroups with the same letters in the same row are not statistically different (P > .05) according to post hoc tests.
P < .05
4. DISCUSSION
During the pandemic of COVID‐19, children's dental diseases cannot be diagnosed and treated in time as usual, because of not only the lockdown but also the fear of the high risk of infection of SARS‐CoV‐2, which transmitted through droplets and aerosols when using some dental instruments such as high‐speed turbines. 7 , 17 , 18 Fever, the initial symptom of COVID‐19 infection, was also reported, stimulating the nerves of parents. Most cases of fever in this study were related to herpes gingivostomatitis and acute periapical periodontitis. Parents were instructed to keep close contact with local communities to get medical care for their children underlying this complex medical condition. 19 Another prominent issue attracting our attention was that one‐quarter of the parents expressed concerns about the postponement of the next follow‐up. Considering the potential consequences of treatment interruption, paediatric dentists should move actively to keep close eyes on those children who had to delay their treatment unexpectedly and complete the therapy step by step once the lockdown ends. Furthermore, accesses of telemedicine, telephone or online counselling service also should be provided by professional dental clinics. 20
To decide what is real emergent, urgent, or neither even through the prism of professional guidance is a challenge but of great significance. 6 Effectively grading severity of the dental diseases can greatly save medical resources and minimize the risk of wider population exposure while medical resources are straining under such circumstances. 6 The category of dental emergency is not fixed and unchangeable. Dentists should use their professional judgment in determining a patient's need for urgent or emergency care. 14 In our study, a case of uncontrolled bleeding caused by the trauma of primary teeth was reported by a 6‐year‐old child. The parents were informed that our emergency department was still open and they could get help there. Some other real emergencies that may potentially compromise the patient's airway caused by cellulitis or trauma involving facial bones should be treated immediately although parents are afraid of getting exposed to COVID‐19 when visiting the healthcare setting. 14 , 19 Paediatric departments have the responsibility to cope with real emergencies if they have the capacity to provide high‐quality treatment meanwhile protecting themselves, their staffs, and their environment. 6
Urgent dental care focuses on managing conditions that require immediate attention to relieve severe pain and the risk of infection. Dental pain and abscess or swelling were the most common oral health‐related concerns for parents to contact us. These signs and symptoms are associated with pulpal and periapical conditions, which usually results from caries. 21 The previous study confirms that the most common reasons for hospital‐based emergency visits are dental caries and pulpal or periapical lesions. 22 Pain associated with herpes gingivostomatitis is also frequent in children and should be paid highly attention when associated with fever. 23 Our results show that dental trauma occurred commonly in children, which was in agreement with previous studies, 10 , 24 , 25 , 26 and all the three kinds of trauma involving primary teeth, permanent teeth or soft tissue had been reported. Cases of tooth fracture and avulsion/luxation require treatments instantly to release pain and improve a favourable outcome. 14 Online advice by a professional could provide an approach for the immediate or urgent care of dental traumatic injuries to prevent further injury by immediate replantation or storing it in the mouth. 26 Additionally, careful attention should be made to preserve pulpal vitality in the immature permanent tooth to ensure continuous root development. 26
During the pandemic, dental treatments referring to pulpotomy, pulpectomy, or nonsurgical root canal treatment were not priorities for urgent dental care. Guidelines suggest that the first choice is to take medicine as one of the control measures at home. 21 , 27 A couple of children had taken some tablets without professional advice to release dental pain or control local inflammation, but our study indicates that their medication was scarcely standard. 28 American Dental Association (ADA) confirmed that up to 85% of dental antibiotic prescriptions were ‘suboptimal or not indicated’ in 2019. 21 Oral analgesics are common medication choices for the treatment of dental pain in children. 21 , 29 Nonsteroidal anti‐inflammatory drugs and acetaminophen specifically ibuprofen and acetaminophen are alternated or staggered as first‐line pharmacologic therapy for dental pain and/or swelling without systemic involvement but no antibiotics. 21 , 27 Antibiotics are effective when pulp‐ and periapical‐related dental pain and swelling are associated with systemic involvement. 21 Oral amoxicillin is the first choice for children who have no penicillin allergy, or penicillin V potassium as an alternative if the former isn't feasible. 21 , 30 But when first‐line treatment fails, the only choice turns to the broader antibiotic with a supplement for oral metronidazole. 21 Meanwhile, children with allergies may consider oral azithromycin, clindamycin, or cephalexin. 21 , 30 Moreover, antibiotic use remains at the discretion of the clinicians when dental traumas are accompanied by an avulsed tooth, soft tissue, and other associated injuries. 30 There is limited evidence for the use of systemic antibiotics in the management of other traumatic dental injuries. 10 , 25 Therefore, parents should instruct their children to take medicines with the guidance of professional paediatric dentists especially in this special blockade period.
Routine or non‐urgent dental procedures that do not require immediate intervention were another major aspect of counselling. Retained deciduous teeth, with the simultaneous eruption of the permanent successors, were the most common occurrences. Chewing hard consistency foods, such as fruits and beef, can facilitate the normal replacement of teeth through mechanical stimulation. 7 Palliative measures are strongly recommended during COVID‐19 to cope with the problems of orthodontic consultations (overjet, overbite, crowded dentition and so on), asymptomatic caries, space maintainers, fillings and preformed crowns. The treatment of non‐emergencies could be postponed until the release of lockdown. Non‐aerosol generating procedures such as interim therapeutic restoration (ITR), Hall crowns and non‐restoration treatments like fluoride varnish could be alternative approaches. 6 In the context of the pandemic, it is of great significance for paediatric dentists to disseminate oral health education through adequate remote consultation. 7 Dentists could use the digital platforms on which they could comfort parents and offer the information of prevention methods against oral diseases for children including effective oral hygiene management and regular dietary habits. 7 , 20
The results of this study indicate that the proportion of children who develop dental emergencies varies in different ages. Kindergarteners between 3‐6 years old, with the highest incidence of emergencies, should be highly valued by dentists and parents by assisting children to take an active part in prevention and protection. The high caries prevalence rate in kindergarteners leads to a high incidence of related sequelae (pulp or periapical lesions). 21 Moreover, this study confirmed the available literature of dental traumatic injuries for one specific age group (0‐3 years old). The possible reasons for injury are that the first 3 years of childhood is the period of motor development, which brings the danger of accidental injury. While the children between 6‐12 years old tend to engage in hazardous activities, which may also increase the risk of traumatic injury. 13
This study had some limitations. First of all, lack of accurate history and other important information especially in the absence of clinical and X‐ray examination would have resulted in the wrong diagnosis and classification of cases as dental emergencies or non‐emergencies. Second, these findings are only from the Paediatric Department in Stomatology of Wuhan University, and cannot be generalized. However, the city of Wuhan, as the first one to take strict lockdown measure, is likely to show similar characteristics to other cities which were in lockdown. Despite these limitations, this study is the first to retrospectively analyse the oral problems reported by children during the period of the strict blockade and give corresponding suggestions. The results of this study provide evidence and implications of how to manage and treat paediatric diseases during and after COVID‐19 pandemic for other parts of the world that are experiencing or about to end the blockade.
In conclusion, paediatric dentists all over the world are facing great challenges in avoiding infection and developing paediatric emergency services in the current context of COVID‐19 with uncertainty and frequent change. Effective dental emergency triage with children can minimize the tension of medical resources and ensure the safety of healthcare professionals, children, and parents.
Why this paper is important to paediatric dentists.
It shows that dental emergencies of children were most related to swelling, pain, and trauma with or without systemic symptoms during the pandemic of COVID‐19.
It highlights the need for effective dental emergency triage with children to greatly save medical resources and minimize the risk of wider population exposure under COVID‐19 blockade.
Telemedicine service including medication instruction and oral health instruction could be helpful for dentists to provide home management approaches for children.
CONFLICT OF INTEREST
All authors declare no competing interests.
AUTHOR CONTRIBUTIONS
FY and LY conceived the ideas; FY and LY collected the data; FH and DQ analysed the data; and GS led the writing.
Supporting information
App S1
ACKNOWLEDGEMENTS
The authors are indebted to all the dentists in Department of Paediatric Dentistry, Wuhan University Stomatology Hospital for their efforts in free online consultations for children.
Yang F, Yu L, Qin D, Hua F, Song G. Online consultation and emergency management in paediatric dentistry during the COVID‐19 epidemic in Wuhan: A retrospective study. Int. J. Paediatr. Dent. 2021;31:5–11. 10.1111/ipd.12722
Yang and Yu should be considered joint first author.
Funding information
This work was supported by Hubei Provincial Natural Science Foundation of China, Grant/Award Number: 2015CFB258. The funding sources had no involvement in the study design, collection, analysis and interpretation of data, preparation of the manuscript, or in the decision to publish.
REFERENCES
- 1. Coronavirus disease(COVID‐19) situation report‐141 . World Health Organization. https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200609‐covid‐19‐sitrep‐141.pdf?sfvrsn=72fa1b16_2. Accessed June 9, 2020.
- 2. Notice of the prevention and control headquarters of pneumonia in new coronavirus infection. Wuhan Municipal Health Commission. http://www.wh.gov.cn/sy/whyw/202003/t20200316_960171.shtml. Accessed January 23, 2020.
- 3. Notice of Hubei Province new coronavirus infection pneumonia prevention and control headquarters. Wuhan Municipal Health Commission. http://wjw.wuhan.gov.cn/ztzl_28/fk/tzgg/202004/t20200430_1198401.shtml. Accessed April 7, 2020.
- 4. Population grouped by age. Hubei Provincial bureau of statsitics. http://tjj.hubei.gov.cn/tjsj/sjkscx/tjnj/gsztj/whs/201911/P020191104653356795480.pdf. Accessed June 6, 2019.
- 5. Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID‐19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99(5):481‐487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Casamassimo PS, Townsend JA, Litch CS. Pediatric dentistry during and after COVID‐19. Pediatr Dent. 2020;42(2):87‐90. [PubMed] [Google Scholar]
- 7. Luzzi V, Ierardo G, Bossù M, Polimeni A.COVID‐19: pediatric oral health during and after the pandemics. 2020. [DOI] [PMC free article] [PubMed]
- 8. Caries‐risk assessment and management for infants, children, and adolescents. Pediatr Dent. 2017;39(6):197‐204. [PubMed] [Google Scholar]
- 9. Ferraz dos Santos B, Dabbagh B. A 10‐year retrospective study of paediatric emergency department visits for dental conditions in Montreal, Canada. International Journal of Paediatric Dentistry. 2020. 10.1111/ipd.12651 [DOI] [PubMed] [Google Scholar]
- 10. Malmgren B, Andreasen JO, Flores MT, et al. International association of dental traumatology guidelines for the management of traumatic dental injuries: 3. Injuries in the primary dentition. Dent Traumatol. 2012;28(3):174‐182. [DOI] [PubMed] [Google Scholar]
- 11. AbdelAziz WE, Dowidar KM, El Tantawi MM. Association of healthy eating, juice consumption, and bacterial counts with early childhood caries. Pediatric dentistry. 2015;37(5):462‐467. [PubMed] [Google Scholar]
- 12. Management of the developing dentition and occlusion in pediatric dentistry. Pediatr Dent. 2018;40(6):352‐365. [PubMed] [Google Scholar]
- 13. Martens LC, Rajasekharan S, Jacquet W, Vandenbulcke JD, Van Acker JWG, Cauwels R. Paediatric dental emergencies: a retrospective study and a proposal for definition and guidelines including pain management. Eur Arch Paediatr Dent. 2018;19(4):245‐253. [DOI] [PubMed] [Google Scholar]
- 14. What constitutes a dental emergency? American dental association. https://www.ada.org/en/publications/ada‐news/2020‐archive/march/ada‐develops‐guidance‐on‐dental‐emergency‐nonemergency‐care. Accessed March 18, 2020.
- 15. Anegundi RT, Patil SB, Shubha M, Havale R. Pediatric dental trauma: wide horizon of ignored etiological factors. Int J Clin Pediatr Dent. 2011;4(2):101‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Alsharif AT, Kruger E, Tennant M. Dental hospitalization trends in Western Australian children under the age of 15 years: a decade of population‐based study. Int J Paediatr Dent. 2015;25(1):35‐42. [DOI] [PubMed] [Google Scholar]
- 17. Singh V, Lehl GK, Talwar M, Luthra A. The novel coronavirus and challenges for general and paediatric dentists. Occup Med (Lond). 2020;70(5):320‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang Y, Zhou CC, Shu R, Zou J. Oral health management of children during the epidemic period of coronavirus disease 2019. Sichuan Da Xue Xue Bao Yi Xue Ban. 2020;51(2):151‐154. [DOI] [PubMed] [Google Scholar]
- 19. Children and youth with special healthcare needs. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019‐ncov/faq.html#Children‐and‐Youth‐with‐Special‐Healthcare‐Needs. Accessed June 2, 2020.
- 20. Georgakopoulou EA. Digitally aided telemedicine during the SARS‐CoV‐2 pandemic to screen oral medicine emergencies. Oral Diseases. 2020. 10.1111/odi.13383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lockhart PB, Tampi MP, Abt E, et al. Evidence‐based clinical practice guideline on antibiotic use for the urgent management of pulpal‐ and periapical‐related dental pain and intraoral swelling: a report from the American dental association. J Am Dent Assoc. 2019;150(11):906‐921.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Allareddy V, Nalliah RP, Haque M, Johnson H, Rampa SB, Lee MK. Hospital‐based emergency department visits with dental conditions among children in the United States: nationwide epidemiological data. Pediatr Dent. 2014;36(5):393‐399. [PubMed] [Google Scholar]
- 23. Petti S, Lodi G. The controversial natural history of oral herpes simplex virus type 1 infection. Oral Dis. 2019;25(8):1850‐1865. [DOI] [PubMed] [Google Scholar]
- 24. Abbott P. Traumatic dental injuries are now the 5th most prevalent disease/injury in the world‐But they are being neglected!! Dent Traumatol. 2018;34(6):383. [DOI] [PubMed] [Google Scholar]
- 25. DiAngelis AJ, Andreasen JO, Ebeleseder KA, et al. International association of dental traumatology guidelines for the management of traumatic dental injuries: 1. fractures and luxations of permanent teeth. Dent Traumatol. 2012;28(1):2‐12. [DOI] [PubMed] [Google Scholar]
- 26. Andersson L, Andreasen JO, Day P, et al. International association of dental traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dental Traumatol. 2012;28(2):88‐96. [DOI] [PubMed] [Google Scholar]
- 27. Pain Management in Infants . Children, adolescents and individuals with special health care needs. Pediatr Dent. 2018;40(6):321‐329. [PubMed] [Google Scholar]
- 28. Use of antibiotic therapy for pediatric dental patients. Pediatr Dent. 2018;40(6):383‐385. [PubMed] [Google Scholar]
- 29. Hammel JM, Fischel J. Dental emergencies. Emerg Med Clin North Am. 2019;37(1):81‐93. [DOI] [PubMed] [Google Scholar]
- 30. Segura‐Egea JJ, Gould K, Şen BH, et al. European Society of endodontology position statement: the use of antibiotics in endodontics. Int Endod J. 2018;51(1):20‐25. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
App S1


