Two months have already passed since the World Health Organization declared COVID‐19 a global pandemic. Italy was the first European country to record an outbreak of COVID‐19, and lockdown and social distancing strategies were adopted to prevent the spread of the virus. Several countries have examined the “Italian phase‐one strategy model” for outbreak containment and adopted similar procedures: all levels of school closures, extended workplace closures, and social isolation.
The Dermatological Clinic of the United Hospitals of Ancona City is a medium‐sized departmental organizational structure (SOD) belonging to the Department of Clinical and Surgical Sciences of a level II hospital with a catchment area of 800,000 inhabitants. More than 15,000 day services are recorded annually in our SOD. At the beginning of March, when the pandemic was widespread in Italy as in the rest of the world, the clinic's activities underwent a major reorganization, with a temporary suspension of all nonurgent clinical activities. The majority of the healthcare personnel, including physicians and nurses, were moved to COVID‐19 wards to deal with health emergencies. 1
Since the beginning of May in Italy, thanks to the decrease in the number of contagions (Fig. 1), the “Italian phase‐two strategy model" has been in effect, which consists of maintaining social distance and the partial resumption of productive and commercial activities.
Figure 1.
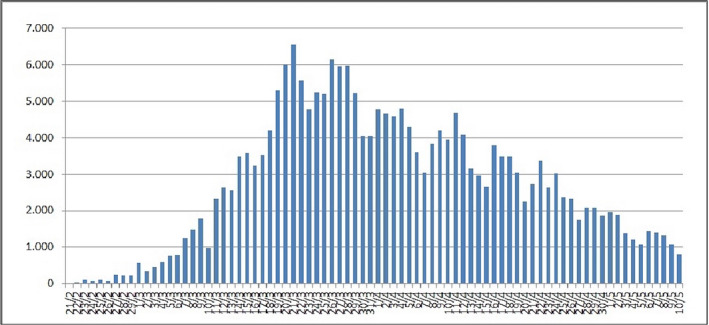
Absolute increase in COVID‐19 cases. The graph illustrates the new daily cases of SARS‐CoV‐2 in Italy from February 21 to May 10 2
A well‐known and generally accepted index for evaluating the pandemic trend in Italy, beyond the total contagions, is the number of patients admitted to intensive care departments.
The number of hospitalizations in intensive care for COVID‐19 in Italy fell from 1,168 to 1,034, that is by 134 units, on April 14, 2020. On that same day, there was a decrease in the total number of admissions from 14,636 to 13,834, a drop of 802 units (3,000 less than 5 days earlier). 2 These instructive data led the Italian task force for outbreak containment strategies to partially resume daily routines, even in the hospital environment.
This national lockdown loosening program was turned to the regional level and caused us to partially resume our activities, both inpatient and outpatient services. The protocol adopted by our clinic is described below.
Following the release of nursing staff from a closed COVID‐19 unit, the inpatient ward was reopened on May 10, 2020, and it has been possible to carry out ordinary hospitalization (according to clinical priority), although access has been reduced to allocate only one patient to a hospital room. Before admission, a telephone or outpatient triage is performed to assess the symptoms of possible SARS‐CoV‐2 infection (fever >37.5 °C, and/or respiratory symptoms, and/or personal history of previous contacts with subjects infected by SARS‐CoV‐2).
If the infection is suspected, the patient is automatically transferred to the emergency room for assessment; otherwise, the patient is regularly admitted, and a diagnostic swab for SARS‐CoV‐2 RNA extraction is performed. During triage operations, a comprehensive clinical evaluation, focusing not only on specific dermatological symptoms and signs of hospitalization but also on skin symptoms related to COVID‐19 (chilblains and skin rash), is generally performed. 3 , 4
Every week, the following inpatient activities are generally scheduled: three ordinary hospitalizations (variable length of hospital stay according to clinical conditions) and six daily accesses for photodynamic treatment. At present, major surgical activities are suspended, since operating rooms previously occupied by COVID‐19 patients are in the reconverting phase; reopening is scheduled for the end of May, with 2‐hour long surgical sessions twice weekly (only skin cancer surgery admitted), and shared with plastic surgeons.
All patients are encouraged to wear a surgical mask when dealing with ward personnel and must perform periodic hand hygiene, regardless of their SARS‐CoV‐2 status.
Similarly, all ward personnel have to wear personal protective equipment (PPE) during all diagnostic or therapeutic procedures on the patient or when dealing with colleagues.
With regards to outpatient activities, since May 10, 2020, the following outpatient services have been activated: clinical consultations for general dermatology (10 medical examinations per week), pediatric dermatology (two per week), digital dermoscopy (eight per week), inflammatory and immunomediated skin diseases (five per week), surgical and nonsurgical wound dressings (20 per week), and cryotherapy/diathermy (10 per week). Outpatient services that remained active during “phase 1” of the pandemic have been empowered: oncological dermatology, dermatological follow‐up for transplanted patients, melanoma and nonmelanoma skin cancer screening visits, and outpatient surgery for melanoma and nonmelanoma skin cancer. For each outpatient service, specific clinical‐assistance pathways have been traced to protect the health of both patients and healthcare personnel.
The following services are still not active: allergological dermatology, trichology, capillaroscopy, sexually transmitted infections care, and dermatology–rheumatology–gastroenterology multidisciplinary integrated activities. 1 The amount of activity has been reduced by 1/5 compared to the pre‐COVID‐19 era, which reduces the number of patients in the waiting room (20 patients in a time span of 8 hours).
All programmed or deferred visits, coded as P (within 90 days) and D (within 30 days) priorities, not performed in the previous 2 months have been canceled by a regional decree, and the necessity of the visit is reassessed by the general practitioner. Only first visits and checks with urgent (U, within 72 hours) and brief (B, within 10 days) priorities are allowed in May. In any case, information technology is being improved to optimally activate telemedicine, especially for patients already under treatment, who need nonurgent assistance or therapeutic adjustments.
As for outpatients, specific itineraries have been traced. The day before the visit, the patient is contacted, and a phone triage is conducted asking for information on any symptoms attributable to COVID‐19 or previous contacts with SARS‐CoV‐2 positive individuals. The patient is also reminded to come to the clinic by him/herself, only one caregiver is allowed for underage or disabled patients, and punctuality with respect to the agreed visiting time is recommended. 5 , 6 , 7 Before entering the dermatological polyclinic area, the patient's body temperature is measured and if it exceeds 37.5 °C, access is prevented. Otherwise, the patient is provided with standard single‐use PPE (surgical mask and nitrile gloves) before entering. Moreover, the patient must fill out a self‐certification form attesting current health status and any potentially at‐risk contact with SARS‐CoV‐2 positive persons. Waiting rooms of the outpatient services have been arranged to avoid crowding, guaranteeing an interpersonal distance of 2 square meters. In addition, disinfectant gels are mounted on the walls, and all spaces are sanitized three times a day. All the healthcare operators wear filtering facepiece 2 (FFP2) masks without a filter or other types of PPEs according to the procedures to be performed on the patient.
In our opinion, such a complex reorganization of services is mandatory to ensure the safety of both healthcare staff and patients during the so‐called phase 2, to control virus circulation in the healthcare environment, and to prevent the hospital itself from becoming a source of an outbreak of the infection.
Conflict of interest: None.
Funding source: None.
F.D, G.R., and A.C. equally contributed to the manuscript.
References
- 1. Radi G, Diotallevi F, Campanati A, et al. Global coronavirus pandemic (2019‐nCOV): Implication for an Italian medium size dermatological clinic of a II level hospital. J Eur Acad Dermatol Venereol 2020; 34: e213–e214. [DOI] [PubMed] [Google Scholar]
- 2. Integrated surveillance of COVID‐19 in Italy (Ordinanza n. 640 del 27/02/2020). 2020. Available at: https://www.epicentro.iss.it/.
- 3. Campanati A, Brisigotti V, Diotallevi F, et al. Active implications for dermatologists in “SARS‐CoV‐2 era”: personal experience and review of the literature. J Eur Acad Dermatol Venereol 2020; 34: 1626–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Diotallevi F, Campanati A, Bianchelli T, et al. Skin involvement in SARS‐CoV‐2 infection: case series [published online ahead of print, 2020 May 15]. J Med Virol 2020. 10.1002/jmv.26012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Radi G, Simonetti O, Diotallevi F, et al. How can I take care of you? The dermatologist meets patients' needs during the COVID‐19 pandemic [published online ahead of print, 2020 Jun 1]. Dermatol Ther 2020; 33(4): e13740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marasca C, Ruggiero A, Annunziata MC, et al. Face the COVID‐19 emergency: measures applied in an Italian Dermatologic Clinic [published online ahead of print, 2020 Apr 15]. J Eur Acad Dermatol Venereol 2020; 34(6): e249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Patrizi A, Bardazzi F, Filippi F, Abbenante D, Piraccini BM. The covid‐19 outbreak in Italy: preventive and protective measures adopted by the dermatology unit of Bologna University Hospital [published online ahead of print, 2020 Apr 29]. Dermatol Ther 2020; 33(4): e13469. [DOI] [PMC free article] [PubMed] [Google Scholar]


