Abstract
The novel coronavirus disease (COVID‐19) pandemic has created major challenges and disruptions to hospitals throughout the world, with profound implications for cardiac surgery and cardiac surgeons. In this review, we highlight the hospital and cardiac surgical experience at Baylor St. Luke's Medical Center in the Texas Medical Center in Houston, Texas as of mid‐July 2020. Our local experience has consisted of a spring surge (early March to early May), followed by a relative flattening and then a summer surge (early June to present day), similar to a sine wave. Throughout the entire pandemic, our simultaneous medical priorities have been treating the growing number of patients with COVID‐19 while continuing to provide needed care for those without COVID‐19. The current situation will be the “new normal” until a vaccine becomes available. It will be vital to stay attuned to epidemiologists, public health officials, and infection control experts, because what they see today, the intensive care units will see tomorrow. The lessons we have learned are outlined in this review but can be summarized most succinctly: preparation. We must prepare in advance, stockpile supplies and personal protective equipment, have rapid and vigorous testing protocols in place, utilize technology (eg, online meetings, videoconference “office visits”), and encourage hospital‐wide and community protective efforts (social distancing, mask wearing, hand hygiene). Hopefully, the lessons learned through this challenging experience will prepare us for the next time.
Keywords: cardiovascular surgery, COVID‐19, Houston, pandemic
1. THE GLOBAL CHALLENGE
The novel coronavirus disease (COVID‐19) pandemic created by the severe acute respiratory syndrome coronavirus (SARS‐CoV‐2) has resulted in major public health challenges and economic disruption on a global scale. The World Health Organization declared a global pandemic on March 11, 2020, and the United States declared a national emergency 2 days later. As of this writing (late July 2020), more than 16.8 million cases have been confirmed worldwide, along with more than 662 000 deaths; the United States confirms 4.4 million cases and more than 150 000 deaths. 1
The regional incidence and impact of the COVID‐19 pandemic in the United States has varied substantially over time, with a disproportionate share of the initial impact in New York City and the northeast and, at first, comparably less impact in the southern states, with fewer cases and fatalities. Individual states and localities issued varying degrees of stay‐at‐home orders in an effort to “flatten the curve,” in an attempt to prevent an acute surge in hospitalizations that would overwhelm intensive care units (ICUs) and the hospitals’ capacity to care for all patients. These variations in burden and response are underscored in a pithy observation by an unknown author: “We are in the same storm, but not in the same boat.”
The complications of COVID‐19 also vary widely and extend beyond respiratory failure to life‐threatening cardiac, renal, and immunological dysfunction, to name only a few. The implications for cardiac surgery and cardiac surgeons have been profound. Although not typically involved as front‐line providers, cardiac surgeons have been called on to provide leadership and direction for local health care providers navigating the intense and widespread challenges posed by COVID‐19. Their expertise has been essential and will continue to be in the months and years ahead.
In this report, we highlight the hospital and cardiac surgical experience in Houston, Texas as of mid‐July 2020, with a particular focus on hospitals in the Texas Medical Center, the largest medical city in the world.
2. THE LOCAL CHALLENGE
In Texas, the COVID‐19 pandemic could be thought of as occurring in two surges with respect to infected patients: a spring surge (early March to early May) followed by a relative flattening, and then a summer surge (early June to present day). In numbers and, perhaps most importantly, in the attitude of the public, the COVID‐19 experience resembles a sine wave.
Texas Governor Abbott initially declared a state of disaster on March 13, 2020, after 30 COVID‐19 cases had been confirmed. 2 In response, Harris County (comprising the greater Houston metropolitan area) issued a county‐wide stay‐at‐home order on March 24 that included social distancing, travel restrictions, shelter‐in‐place directives, and closure of nonessential business. As of July 29, statewide data indicated that more than 3.5 million tests had been administered in Texas, resulting in more than 403 000 cases (11.4% test positivity); in addition, 6190 fatalities had been recorded. 3 In Harris County, home to 4.7 million people and the third‐most‐populated county in the United States, 67 660 COVID‐19 cases had been identified. Within seven major institutions in the Texas Medical Center (TMC) in Houston, 16 818 patients have been hospitalized with COVID‐19; of these, 12% were currently hospitalized as of late July, 8% had died, and 80% had been discharged. The sine wave appearance of COVID‐19 patients in the ICU showed a rise and then fall in the spring followed by another rise in June (Figure 1). 4
Figure 1.
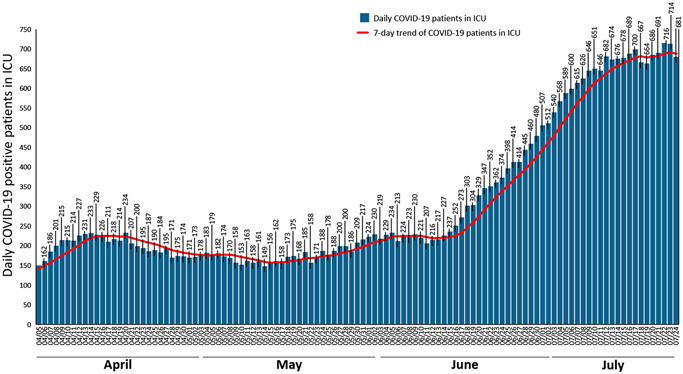
Texas Medical Center COVID‐19‐positive patients in ICU beds through July 24, 2020. A sine wave appearance is evidenced by a rise in April, a dip in May, and another rise in June. 4 COVID‐19, novel coronavirus disease; ICU, intensive care unit
Baylor St. Luke's Medical Center in the TMC is the flagship hospital of the Catholic Health Initiative (CHI) nationwide network. The hospital opened in 1954 and added the Texas Heart Institute with Dr. Denton Cooley in 1962; it has been affiliated with the Baylor College of Medicine since 2004. Its 884‐bed capacity makes it a hub in the CHI network for complex tertiary and quaternary care in southeast Texas. Its normal ICU capacity is 145 beds in 12 discrete ICU locations spread across five floors. The initial preparation for the expected surge in COVID‐19 patients was an escalation to 190 beds; a secondary “doomsday scenario” planned for emergency preparation of up to 250 beds by conversion of operating rooms to ICUs and hospital‐wide mobilization, as outlined by others on the basis of the New York City experience. 5
In addition, in February 2020, senior hospital administration entered into daily close communication with public health authorities, infection control experts, and critical care leaders across the TMC to review the capacity of the system and the availability of mechanical ventilation resources, personal protective equipment (PPE), and ICU beds. The contributions of those experienced in disaster management and adaptation of the military medicine principles of preparedness, team‐based care, and effective triage were vital to a sustained effort, which in its 6th month continues at the highest level of intensity. 6 The TMC tracks and publishes various case count, mortality, and occupancy metrics, updated daily. 4
Two simultaneous medical priorities required our focus: treating the growing number of patients with COVID‐19, while continuing to provide needed care for those without COVID‐19.
3. THE CRITICAL CARE CHALLENGE
Our guiding principles were to attempt to anticipate what was coming with respect to the needs of the COVID‐19 patients and then to stay ahead as much as possible. Leaders across multiple fields were in close communication with colleagues throughout the world and in parts of the country that were most affected in late February and early March. Failing to anticipate a substantial influx of patients would risk having a hospital paralyzed in the middle of a crisis, overwhelmed in its capacity to provide care for COVID‐19 patients while ignoring the vital needs of its non–COVID‐19 patients.
Specifically, we aimed to: (a) conserve, protect, and support staff by providing adequate PPE; (b) eliminate nonurgent strains on the system by postponing elective outpatient procedures, such as screening colonoscopies; (c) moderate the local transmission of COVID‐19 by restricting the number of people entering the hospital, screening those entering the facility, and limiting the hospital workforce to essential personnel (which limited our ability to enroll and conduct clinical trials); (d) promote transparency by providing daily text and email messages to all hospital workers regarding the capacity of ICUs, PPE, and other relevant information from the Chief Medical Officer and other senior leaders from both the hospital and the Department of Surgery 7 ; and (e) have the leadership maintain a visible presence in the ICUs to encourage resilience among the doctors, nurses, and ancillary staff; effective leadership requires constant feedback from frontline providers on both the COVID‐19 and non‐COVID‐19 fronts.
In the ICUs, we initiated a tiered escalation strategy (yellow/orange/red) involving the repurposing of ICUs, staff intensivists, advanced practice providers, allied health care workers, and house staff. The yellow tier would be entered once we surpassed 19 beds needed for COVID‐19 patients, and additional ICUs would be repurposed as dedicated COVID‐19 ICUs; after 59 beds we would enter the orange tier and after 152 beds the red tier. Initially, two 12‐bed ICUs were repurposed as dedicated COVID‐19 ICUs. In addition, other ICUs were consolidated: four units with 68 ICU beds normally dedicated to cardiovascular care—including the care of patients after coronary bypass grafting, valvular or aortic surgical procedures, thoracic and abdominal transplantation, and mechanical circulatory support devices (including extracorporeal membrane oxygenation [ECMO] and durable and temporary ventricular assist devices)—were consolidated into three units, with concomitant reduction in scheduled cardiac surgeries that allowed for adequate capacity. Special attention was given to ensure that COVID‐19 patients were not mixed into units housing the most vulnerable, immunosuppressed patients (eg, transplant recipients). Emergency contingencies included redeploying surgical attending physicians, although this was never implemented or necessary.
In the spring surge we peaked at approximately 36 COVID‐19 ICU beds on April 13 (yellow tier), followed by a gradual decline to 9 COVID‐19 ICU beds on May 25; once the summer surge began, we climbed to 60 COVID‐19 ICU beds on July 12 (orange tier). As of July 29, we are at 38 COVID‐19 ICU beds (yellow tier) and are cautiously optimistic that the downward trend will continue.
Furthermore, administrative leaders involved in the daily TMC collaborative monitoring of ICU capacity 8 ensured that if any one hospital were pushed to the brink, other hospitals would provide help if needed and accept patients. It was known that there would be strains on various health care resources, including ICU capacity, PPE, and advanced therapeutics such as mechanical ventilation, ECMO, and renal replacement therapy. In the event that the hospital were in a triage scenario requiring the rationing of scarce resources, formal multidisciplinary committees would discuss the ethical considerations for just allocation; fortunately, this has not been required. 9 , 10
4. THE CARDIAC SURGERY CHALLENGE
Despite serious concerns about surgical mortality (with reports as high as 20% for cases in Wuhan, China), it was important to continue conducting cardiac operations in as responsible a manner as possible, given the pandemic. 11 Baylor St. Luke's moved to the three‐tier system described by national societies to determine which cases would proceed and which would be placed on hold: (a) tier 1, emergency or high‐acuity cases; (b) tier 2, urgent or intermediate‐acuity cases (should be done within 30 days); and (c) tier 3, elective or low‐acuity cases that could be safely delayed for at least 30 days. Tier 1 and 2 procedures were conducted without delay, whereas tier 3 cases were reviewed on a case‐by‐case basis by a multispecialty group of surgeons, anesthesiologists, and administrators to determine appropriateness, given the patient's clinical need, the hospital's capacity, and risks and benefits of proceeding with surgery. 12 Consistent with Society of Thoracic Surgeons guidance, 13 our goals were to protect the cardiac surgical patient from risk for nosocomial infection, protect the hospital and our local community by preserving ICU beds and PPE, and protect the members of the health care team.
Procedures in the surgical offices were modified to handle changes in the way we interacted with outpatients. It was important to identify patients at higher risk from COVID‐19 exposure who would most benefit from avoiding coming to the clinic. Given the lifting of Medicare telehealth restrictions, we expanded our capacity to conduct telemedicine office visits for both postoperative follow‐ups and new patient consultations, although consultations across state lines were not possible. Moreover, we established mechanisms to facilitate periodic check‐ins with tier 3 patients (for example, a patient with a 5.0‐cm ascending aortic aneurysm or severe mitral regurgitation but with minimal symptoms) to ensure that they were not becoming symptomatic during this waiting period. Meanwhile, we implemented a robust screening protocol that began right at the front desk, with mask wearing, face shielding, limited and separated seating, and other distancing measures.
Finally, it was necessary to downscale the in‐person office staff to avoid interemployee COVID‐19 transmission. This was accomplished by allowing employees to work from home whenever possible. We took into account the fact that some employees were more vulnerable to serious COVID‐19 infection, due to older age or pre‐existing conditions, and should work exclusively from home, whereas others were more able to share time between the clinic and home; tasks were assigned accordingly. This also required a supportive information technology infrastructure platform with efficient remote desktop access to preserve productivity. It was important to engage the office staff in this process, instead of having it arbitrarily imposed by department administration: Achieving maximal buy‐in from everyone fostered a higher likelihood of sustained acceptance and resilience among the staff.
4.1. Considerations for transplantation
One of the challenges the institution faced was the need to balance the risk for COVID‐19 infection in transplant patients against the risk for increased waitlist mortality. Reports described a 75% increase in waitlist inactivations and a 37% reduction in waitlist additions during the COVID surge, with major regional variations indicating more significant reductions in the northeast and less effect in the southern states. 14 Moreover, initial reports from New York City indicated a 25% mortality rate for heart transplant recipients infected with COVID‐19. 15 Furthermore, the availability of donor organs in the United States during the course of the pandemic had decreased by approximately 50%. 16 In response, we developed institutional protocols that combined the patient's clinical history, consultation with a transplant infectious disease specialist, COVID‐19 rapid polymerase chain reaction testing, and chest computed tomography scanning to screen potential recipients. 17
During the spring surge, more than 70% of heart transplant offers and more than 90% of lung transplant offers were accepted at our center, including one heart‐lung and one heart‐kidney. 17 It is notable that our heart and lung transplant volume (20 cases) was actually greater in the 3‐month period from March through May 2020 than it was during the same 3‐month period in 2019 (13 cases).
4.2. Considerations for patients on mechanical ventilation with tracheostomy and ECMO
COVID‐19‐related respiratory failure resulted in many patients needing longer‐term ventilator support. As part of the tracheostomy team treating COVID‐19‐positive patients, our thoracic surgery colleagues were involved with bedside percutaneous tracheostomy with full PPE precautions and nonpowered, air‐purifying respirators. Separate COVID‐19 ECMO units were established for patients who needed ECMO for severe respiratory failure, with no overlap permitted between the COVID‐19 and non‐COVID‐19 ECMO units. We provided a dedicated 24/7 inhouse ECMO staff intensivist, and an in‐house perfusionist was present 24/7 for every four ECMOs running. Cannulation was performed predominantly by interventional cardiologists, consistent with institutional practice, with ongoing management overseen by dedicated ECMO intensivists. Cardiovascular surgeons performed decannulation procedures and advised or performed alternative cannulation configurations as needed. We also maintained close collaboration with two other TMC hospitals (Memorial Hermann and Houston Methodist Hospital) during this time to expand our access to ECMO facilities if needed, as each of these programs performs more than 100 ECMO runs annually.
During the spring surge, 62 patients with COVID‐19 required mechanical ventilation; mortality for this group was 30%, and the mean age of nonsurvivors was 69 years. This compares favorably against the 40% mortality rate in New York City. 18 Our intubated patients were twice as likely to be male and were considerably older (65 years) than our female patients (56 years). The mean duration of mechanical ventilation in these intubated patients was 23 days (20 days for nonsurvivors and 26 days for survivors). This threatened to outstrip ICU capacity, because once patients were mechanically ventilated, they were in the ICU for at least 3 weeks. Meanwhile, multiple other management challenges, including systemic thrombosis, were encountered. This vexing dilemma caused continuous renal replacement filters and intravascular catheters to clot easily. Cardiac and critical care surgeons were instrumental in modifying institutional guidelines for systemic anticoagulation using thromboelastography, for example. 19 Practical management considerations in the COVID‐19 ECMO units included keeping machines outside the patient's room to reduce the number of times providers needed to enter the room (Figure 2).
Figure 2.
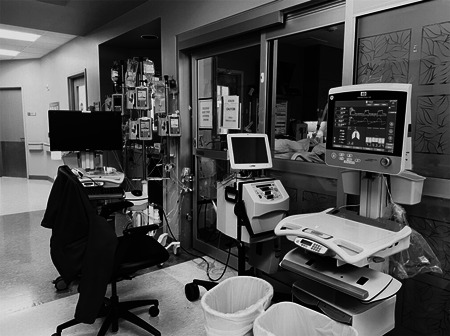
COVID‐19 ECMO unit with mechanical ventilator, continuous renal replacement therapy machine, and IV manifolds, all located outside the patient room to minimize the need to enter the room. ECMO, extracorporeal membrane oxygenation
Typically, our annual ECMO volume is about 125 cases, of which 80% are venoarterial (for cardiogenic shock) and 20% are venovenous (for respiratory failure). During the spring surge, ECMO was used almost exclusively to combat respiratory failure in 12 of the 62 patients on mechanical ventilation (19%), as described in our preliminary report. 20 At our maximum, we ran 12 patients on ECMO (seven with COVID‐19) simultaneously; by mid‐July, we had placed 20 COVID‐19–positive patients on ECMO. We increased our capacity to provide ECMO during the summer surge by hiring additional perfusionists, acquiring or renting additional ECMO circuits, and training more nurses in ECMO care.
4.3. Cardiac surgery during COVID‐19
Elective cardiac surgery was stopped consistent with recommendations from the US Centers for Disease Control and Prevention and the American College of Surgeons. 21 A panel of senior clinicians and administrative leaders had a daily afternoon conference call to determine which surgical cases would go forward. These decisions reflected a deliberate effort to avoid excess blood product use and depletion of mechanical ventilators and PPE, in anticipation of an overwhelming influx of COVID‐19‐positive patients. Complex elective aortic surgical procedures, for example, could place a strain on our blood bank resources, reflecting the global shortage in blood bank products. 22 In fact, given the unprecedented reduction in blood bank donations as a result of social distancing and fears of COVID‐19 transmission, the US Food and Drug Administration (FDA) liberalized the donor pool in an effort to increase the blood product supply. 23
In comparing our 2019 and 2020 cardiac surgical volumes for the 3‐month period from March through May, we noted a 40% drop overall. This reduction was seen across almost all cardiac surgical procedures, including coronary artery bypass grafting (CABG; 41% decrease), valve ±CABG (49%), aortic surgery (34%), and ventricular assist device implantation (25%). This is consistent with a recent report from Maryland that showed a 54% drop in cardiac surgery 24 and a global survey of 60 centers across five continents that revealed a 50% to 75% reduction in cardiac surgery cases. 25
Interestingly, the proportion of urgent and emergency surgeries in 2019 (52% of all cardiac operations) was essentially unchanged in 2020 (50%) during the March through May time period. It is important to note that the distinction between “urgent” and “elective” is not necessarily reflective of clinical need but is differentiated by a patient coming from home for surgery instead of waiting a few days in the hospital for surgery. 26 Indeed, to the lay public, elective surgery implies esthetic cosmetic surgery, not cardiovascular surgery: few would consider a 5‐cm aortic aneurysm with an annual aortic event rate (dissection, rupture, or death) of 3% to 5% to be a truly elective procedure, even if the patient came from home on the day of surgery. Our goal was to triage cases on the basis of patient condition and hospital capacity. Surgical procedures with an expected short length of stay (eg, transcatheter aortic valve replacement) largely continued.
4.4. COVID‐19 impact on cardiovascular emergencies
Multiple reports have shown that patients appear to be avoiding the emergency department, which has resulted in increased morbidity and mortality in acute cardiovascular emergencies. New York City saw a 77% reduction in the monthly volume of type A aortic dissection repairs, 27 a 38% reduction in cardiac catheterization laboratories activated for ST elevation myocardial infarctions, 28 a 43% reduction in hospitalizations for acute cardiovascular causes, 29 and a threefold increase in out‐of‐hospital cardiac arrests during the COVID period compared with the year before, along with a much higher mortality rate. 30 Nationwide, visits to the emergency department were down 40% for January through May 2020, compared with the same time period a year earlier. 31 At our own center, whereas we averaged 17 type A aortic dissection surgeries in the 3‐month period from March through May in each of 2018 and 2019, we performed only 7 during the same period in 2020—a nearly 60% reduction. We observed a similar reduction in emergency cases.
4.5. Considerations for the cardiac surgical workforce
The overall impact of the COVID‐19 pandemic on our cardiac surgical workforce was heterogenous. Almost all surgeons were less clinically active, as expected. Those with significant research interests saw major curtailments in their ability to conduct laboratory research and enroll patients in clinical trials, as a result of institutional social distancing guidelines. The larger goal of surgical leadership, then, was to support our colleagues by making efforts to preserve morale and emphasize team spirit. We were not disappointed in our department's ability to rise to the occasion.
Although major individual financial hardships were not imposed on physicians, given that the hospital has not cut salaries as of July 2020, other hospital staff have been furloughed, and that has required a level of humility and understanding on the part of surgeons working with our ancillary staff. Also in light of objective financial realities, employer contributions to retirement accounts and continued medical education allowances were reduced. All business‐related travel was prohibited as well, to preserve employee safety. Lastly, before mandatory face mask policies were implemented in our hospital on March 31, 14 health care workers tested positive for COVID‐19; as of July 23, 192 (4.3% of the workforce) have tested positive. The data specifically for surgeons is not known.
In sum, our own institutional experience suggests that patients may have been avoiding medical care for fear of COVID‐19 transmission, consistent with reports from other centers. We did not see an increase in surgical mortality during this period. We do look forward to larger multicenter and administrative data set analyses that comprehensively assess the true impact of the breadth and far‐reaching consequences of the pandemic on cardiac surgery practice.
5. THE TRAINING AND EDUCATION CHALLENGE
Our Accreditation Council for Graduate Medical Education (ACGME)‐accredited thoracic surgical residency is the largest in the United States, with four residents matriculating into the program each year. We also have a non‐ACGME aortic surgical fellowship and selective fellowships in thoracic transplantation, mechanical circulatory support, and advanced thoracic surgery. Typically, residents train across five hospitals within the TMC (Baylor St. Luke's, the major academic hospital; Michael E. DeBakey VA Medical Center, the largest Veterans Affairs hospital in the country; Ben Taub Hospital, a county hospital that is home to one of the busiest trauma programs in the world; Texas Children's Hospital, an internationally acclaimed pediatric hospital; and the world‐renowned MD Anderson Cancer Center). 32
During the period when elective cardiothoracic surgical cases were postponed, efforts at practicing social distancing and reducing onsite personnel included modifying resident clinical coverage, to make a modest reduction in the resident footprint in the hospital. This provided an opportunity for residents to be trained and prepared for possible ICU deployment. Critical care physicians offered short courses in basic ICU management. Residents were made available to participate on the vascular access team. Similar to trainees in New York City, some of our residents with formal critical‐care training stepped up to volunteer for ICU deployment. 33
Nevertheless, the overall surgical trainee volume was reduced, compared with that in previous years. Although this may have had minimal impact on trainees in the 1st year of a 3‐year fellowship, it certainly could complicate matters for residents in 2‐year programs who were months away from graduation. The final months also provide the largest exposure to the most complex cardiac cases and offer greater autonomy to increase ease and familiarity with procedures, as these residents are ready to begin a superspecialized fellowship or become a staff surgeon. 34 The American Board of Thoracic Surgery is aware of the potential shortfall in case numbers that some finishing residents may experience and will evaluate those situations on a case‐by‐case basis. Going forward, it will be interesting to see if the COVID‐19 experience will accelerate the use of competency‐based assessments for board certification instead of relying strictly on case numbers, as has been pondered for many years. 35
Similar to students in other academic medical centers, our medical students were removed from clinical services as the pandemic surged in the spring. 36 The surgical curriculum was revamped to include more online modules, which benefitted from significant faculty participation: The reduction in the elective surgery schedule created more time for engagement by members of the surgical department.
Lastly, departmental forums (including grand rounds and the morbidity and mortality conference) and multidisciplinary clinical meetings (including our heart valve and tumor board conferences) were quickly converted to videoconference format, to both preserve the educational mission and facilitate patient care.
6. THE RAMP‐UP CHALLENGE
After seeing a reduction in COVID admissions, on May 1 we began a staged (50%) reintroduction of elective cardiac surgery cases, aiming to return to full normal activity by May 18. We recognized that these surgeries needed to be reintroduced in a deliberate and gradual fashion, and we adopted the recommendations of the Centers for Medicaid and Medicare Services to accomplish this. 37 Nonetheless, estimates suggested that cardiac surgery programs would have to operate at 216% to 263% of the normal volume to be able to clear their backlog. 24 Our projections were consistent with those estimates.
Our deliberations about fully resuming cardiac surgery were guided by the principles outlined by the Society of Thoracic Surgeons: (a) collaborate, (b) prioritize, and (c) reevaluate. 38 Multidisciplinary collaboration and responsiveness to the needs and concerns of our workforce were critical. We prioritized surgical cases by patient acuity and urgency, so as to deliver surgery first to those who needed it most. Even as we began to ramp up our case volume, we were always mindful that COVID‐19 cases could increase again at any point and that we would need to be ready for a second surge.
Ultimately, it was important to be able to reassure our patients that we were doing everything possible to protect them when they came for surgery. This involved performing adequate COVID‐19 screening no more than 72 hours before surgery, securing an adequate supply of PPE and then assuring the community that we had satisfactory stockpiles, and maintaining appropriate physical distancing throughout the hospital so that anyone entering could see that all possible measures were being taken.
One challenge was whether or not to allow families to visit. This became a trust issue for both patients and families, because many people are legitimately concerned that a hospital may not be safe. Having visitors is less important when the length of stay is only 1 or 2 days—for example, after laparoscopic cholecystectomy. With complex aortic surgical procedures that may require a 7‐ to 14‐day stay, the need for family visitation for support is important. We determined that allowing for one family member to be with the patient and visit each day was important for patients to feel comfortable moving ahead with surgery.
Overall, the most vital strategies for mitigating the spread of COVID‐19 that we identified included safe and reliable patient screening, the graded increase of surgical volumes based on our own institutional and TMC COVID‐19 admission projections and our own ICU capacity, along with continued team training in the operating room and ICU for best practices to reduce the risk for transmission. 39
7. LESSONS LEARNED FOR THE NEXT PANDEMIC
It is important to recognize that the current situation is now the “new normal” until a vaccine becomes available. There is every reason to expect COVID‐19 to be here into 2021, and so these lessons will continue to be applicable. The single most important lesson is to stay in tune with the epidemiologists, public health officials, and infection control experts, for what they see today, the ICUs will see tomorrow. We must prepare in advance and stockpile PPE for the rest of 2020.
At a leadership level, it is essential to identify the concerns of the workforce. In surveys, only one‐third of health care workers feel confident that following their organization's guidelines will keep them safe. The lessons for leadership are to: (a) broadcast the organization's safety plan regarding COVID‐19, (b) keep managers accountable and aligned, and (c) use ongoing dialogue and rounding to address safety. 40
Displays of leadership and empathy must be genuine. One of our surgical ICUs was transformed into a COVID‐19 ICU, and it was heartening to see surgical attendings providing meals for the surgical ICU teams, recognizing the sacrifices they were making. The pandemic calls for visible leaders spending time in the ICUs, the wards, and the clinics (ie, “boots on the ground”), visiting the staff to boost morale and to see the real issues for themselves. No amount of Zoom calls, graphs, and PowerPoint presentations can substitute for visibility.
Telemedicine now offers a chance to educate and engage with patients in a different way. The desire to avoid readmission and to facilitate sustained follow‐up will be important going forward. The rapid development of videoconferencing technology ensures that telemedicine will remain a viable way to engage with patients, especially when evaluating referrals from a distance. We have to recognize that our particular patients (advanced age, more comorbidities) are the most vulnerable segment of society and will want to avoid being in crowded waiting rooms, elevators, etcetera, as much as possible and only when necessary.
Lastly, enhanced recovery pathways that are designed to shorten length of stay and promote process efficiencies will become more valuable. 41 , 42 Given that patients will want to spend as little time as possible in the hospital in the COVID‐19 and post–COVID‐19 era, strategies to achieve those goals are likely to be met with patient satisfaction. 43 Moreover, opportunities to harness technology in a patient‐centric manner will preserve the doctor‐patient relationship, although in a different way.
8. “AMERICA IS DONE WITH COVID‐19. COVID‐19 ISN'T DONE WITH AMERICA”
On June 16, 2020, the highest single‐day level of new COVID‐19 cases in the greater Houston area (>1600) was recorded. The logical conclusion was that we either had entered a second wave (a summer surge) or that the first surge had never really gone away. Indeed, after a drop in the number of new cases followed by a plateau, another surge did occur. 44 In some ways, this COVID‐19 sine wave was reflected in the attitudes of the community, which went from heightened alert to relaxation to even more heightened alert. On June 17, former FDA Commissioner Scott Gottlieb said of Texas that “This is an outbreak that's underway. It's expanding. They're at risk of tipping over.” 45 Now that we appear to have entered a second surge, all the lessons learned from the first surge have become applicable again. There are some initial reasons for optimism, however, as clinicians are better at understanding and managing the disease and, perhaps, at recognizing when futility approaches.
9. CONCLUSION
Houston was certainly not surprised that the second wave came: We are now in our 5th month of active experience with the pandemic, and COVID‐19 will be part of the “new normal” for the hospital for the next several months, at least. Rather than a tropical storm that wreaks havoc and then moves on, the COVID‐19 pandemic has been a siege that requires a slow war of attrition. Community efforts to curtail the pandemic will be critical to reduce the burden on hospitals. Although strategies such as the wearing of face masks have been credited with preventing up to 450 000 COVID‐19 cases, 46 the political will to reimpose a second round of shutdowns and social isolation may be difficult to find as the US enters the run‐up to an election—even if public health experts deem it necessary.
Even once this second surge dies down, there is no guarantee that a third surge will not arise in the winter months. We recognize that, as of this writing in late July 2020, the situation is so fluid and dynamic that weeks and certainly months from now some of our conclusions will be obsolete. That is an intrinsic risk of any report in the midst of the pandemic. Nonetheless, we hope that some of our lessons learned can provide other centers with guidance, both now and for future preparations.
CONFLICT OF INTERESTS
Dr. Coselli participates in clinical trials with and/or consults for Terumo Aortic, Medtronic, and W.L. Gore & Associates and receives royalties and grant support from Terumo Aortic. The remaining authors that there are no conflict of interests.
ACKNOWLEDGMENTS
The authors thank Jeanie F. Woodruff, BS, ELS, from the Texas Heart Institute's Scientific Publications Department for providing editorial support and Susan Y. Green, MPH, at Baylor College of Medicine for critical review.
Chatterjee S, Anton JM, Rosengart TK, Coselli JS. Cardiac surgery during the COVID‐19 sine wave: Preparation once, preparation twice. A view from Houston. J Card Surg. 2021;36:1615–1623. 10.1111/jocs.14987
[Correction added after first publication on 9 February 2021: The article title was revised.]
DATA AVAILABILITY STATEMENT
No data in this report were extracted from the medical records of specific patients. The numbers presented are either publicly available on the TMC website or aggregated from internal databases.
REFERENCES
- 1. Johns Hopkins University & Medicine . COVID‐19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Coronavirus Resource Center. Updated July 23, 2020. https://coronavirus.jhu.edu/map.html. Accessed July 30, 2020.
- 2. Abbott G. Governor Abbott declares state of disaster in Texas due to COVID‐19. Office of the Texas Governor: news. Updated March 13, 2020. https://gov.texas.gov/news/post/governor-abbott-declares-state-of-disaster-in-texas-due-to-covid-19. Accessed July 23, 2020.
- 3. Texas Health and Human Services . Texas case counts: COVID‐19 coronarvirus disease 2019. Updated July 22, 2020. https://txdshs.maps.arcgis.com/apps/opsdashboard/index.html#/ed483ecd702b4298ab01e8b9cafc8b83. Accessed July 23, 2020.
- 4. Texas Medical Center . Current COVID‐19 related patients through TMC System. Coronavirus (COVID‐19) Updates. Updated July 22, 2020. https://www.tmc.edu/coronavirus-updates/current-covid-19-related&hyphen-qj2;-patients-through-tmc-system/. Accessed July 23, 2020.
- 5. George I, Salna M, Kobsa S, et al. The rapid transformation of cardiac surgery practice in the coronavirus disease 2019 (COVID‐19) pandemic: insights and clinical strategies from a center at the epicenter. Ann Thorac Surg. 2020. 10.1016/j.athoracsur.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Katz JN, Sinha SS, Alviar CL, et al. COVID‐19 and disruptive modifications to cardiac critical care delivery: JACC Review Topic of the Week. J Am Coll Cardiol. 2020;76:72‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kuy S, Gupta R, Correa R, et al. Best practices for a COVID‐19 preparedness plan for health systems. NEJM Catalyst. 2020;30:2020. 10.1056/CAT.20.0108 [DOI] [Google Scholar]
- 8. Texas Medical Center . Total TMC COVID‐19 positive patients in ICU beds. Coronavirus (COVID‐19) Updates. Updated July 22, 2020. https://www.tmc.edu/coronavirus-updates/total-tmc-covid-19-positive-patients-in-icu-beds/. Accessed July 23, 2020.
- 9. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid‐19. N Engl J Med. 2020;382:2049‐2055. [DOI] [PubMed] [Google Scholar]
- 10. Wood DA, Mahmud E, Thourani VH, et al. Safe reintroduction of cardiovascular services during the COVID‐19 pandemic: from the North American society leadership. J Am Coll Cardiol. 2020;75:3177‐3183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID‐19 infection. EClinicalMedicine. 2020;21:100331. 10.1016/j.eclinm.2020.100331:100331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Patel V, Jimenez E, Cornwell L, et al. Cardiac surgery during the coronavirus disease 2019 pandemic: perioperative considerations and triage recommendations. J Am Heart Assoc. 2020;9:e017042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Haft JW, Atluri P, Ailawadi G, et al. Adult cardiac surgery during the COVID‐19 pandemic: a tiered patient triage guidance statement. Ann Thorac Surg. 2020;110:697‐700. 10.1016/j.athoracsur.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. DeFilippis EM, Sinnenberg L, Reza N, et al. Trends in US heart transplant waitlist activity and volume during the coronavirus disease 2019 (COVID‐19) pandemic. JAMA Cardiol. 2020. 10.1001/jamacardio.2020.2696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Latif F, Farr MA, Clerkin KJ, et al. Characteristics and outcomes of recipients of heart transplant with coronavirus disease 2019. JAMA Cardiol. 2020:e202159. 10.1001/jamacardio.2020.2159:e202159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Loupy A, Aubert O, Reese PP, Bastien O, Bayer F, Jacquelinet C. Organ procurement and transplantation during the COVID‐19 pandemic. Lancet. 2020;395:e95‐e96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Galvan NTN, Moreno NF, Garza JE, et al. Donor and transplant candidate selection for solid organ transplantation during the COVID‐19 pandemic. Am J Transplant. 2020. 10.1111/ajt.16138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cummings MJ, Baldwin MR, Abrams D, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID‐19 in New York City: a prospective cohort study. Lancet. 2020;395:1763‐1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mortus JR, Manek SE, Brubaker LS, et al. Thromboelastographic results and hypercoagulability syndrome in patients with coronavirus disease 2019 who are critically ill. JAMA Netw Open. 2020;3:e2011192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yang Y, Rali AS, Inchaustegui C, et al. Extracorporeal membrane oxygenation in coronavirus disease 2019‐associated acute respiratory distress syndrome: an initial US experience at a high‐volume centre. Card Fail Rev. 2020;6:e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. American College of Surgeons . COVID‐19 guidelines for triage of cardiac surgery patients. ACS: COVID‐19 and Surgery. Updated March 24, 2020. https://www.facs.org/covid-19/clinical-guidance/elective-case/cardiac-surgery. Accessed July 30, 2020.
- 22. Stanworth SJ, New HV, Apelseth TO, et al. Effects of the COVID‐19 pandemic on supply and use of blood for transfusion. Lancet Haematol. 2020. 10.1016/S2352-3026(20)30186-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. US Food and Drug Administration . Coronavirus (COVID‐19) update: FDA provides updated guidance to address the urgent need for blood during the pandemic. Updated April 2, 2020. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-provides-updated-guidance-address-urgent-need-blood-during-pandemic. Accessed July 23, 2020.
- 24. Salenger R, Etchill EW, Ad N, et al. The surge after the surge: cardiac surgery post‐COVID‐19. Ann Thorac Surg. 2020. 10.1016/j.athoracsur.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gaudino M, Chikwe J, Hameed I, Robinson NB, Fremes SE, Ruel M. Response of cardiac surgery units to COVID‐19: an internationally‐based quantitative survey. Circulation. 2020;142:300‐302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bakaeen FG, Gillinov AM, Roselli EE, et al. Cardiac surgery and the coronavirus disease 2019 pandemic: what we know, what we do not know, and what we need to do. J Thorac Cardiovasc Surg. 2020;160:722‐726. 10.1016/j.jtcvs.2020.04.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. El‐Hamamsy I, Brinster DR, DeRose JJ, et al. The COVID‐19 pandemic and acute aortic dissections in New York: a matter of public health. J Am Coll Cardiol. 2020;76:227‐229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST‐segment elevation cardiac catheterization laboratory activations in the United States during COVID‐19 pandemic. J Am Coll Cardiol. 2020;75:2871‐2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bhatt AS, Moscone A, McElrath EE, et al. Fewer hospitalizations for acute cardiovascular conditions during the COVID‐19 pandemic. J Am Coll Cardiol. 2020;76:280‐288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lai PH, Lancet EA, Weiden MD, et al. Characteristics associated with out‐of‐hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020:e202488. 10.1001/jamacardio.2020.2488:e202488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hartnett KP, Kite‐Powell A, DeVies J, et al. Impact of the COVID‐19 pandemic on emergency department visits—United States. MMWR Morb Mortal Wkly Rep. 2020;69:699‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Coselli JS. History and highlights of cardiothoracic surgery at Baylor College of Medicine. Semin Thorac Cardiovasc Surg. 2016;28:611‐620. [DOI] [PubMed] [Google Scholar]
- 33. Mitzman B, Yang S, Brownlee A, et al. The effect of COVID‐19 on cardiothoracic surgery education. Updated April 30, 2020. Accessed July 23, 2020. 10.25373/ctsnet.12214331.v1 [DOI]
- 34. Fuller S, Vaporciyan A, Dearani JA, Stulak JM, Romano JC. COVID‐19 disruption in cardiothoracic surgical training: an opportunity to enhance education. Ann Thorac Surg. 2020. 10.1016/j.athoracsur.2020.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can Covid catalyze an educational transformation? Competency‐based advancement in a crisis. N Engl J Med. 2020. 10.1056/NEJMp2018570 [DOI] [PubMed] [Google Scholar]
- 36. Calhoun KE, Yale LA, Whipple ME, Allen SM, Wood DE, Tatum RP. The impact of COVID‐19 on medical student surgical education: implementing extreme pandemic response measures in a widely distributed surgical clerkship experience. Am J Surg. 2020;220:44‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Center for Medicare & Medicaid Services . CMS adult elective surgery and procedures recommendations: limit all non‐essential planned surgeries and procedureds, including dental, until further notice. April 7, 2020. https://www.cms.gov/files/document/covid-elective-surgery-recommendations.pdf. Accessed July 23, 2020.
- 38. Engelman DT, Lother S, George I, et al. Ramping up delivery of cardiac surgery during the COVID‐19 pandemic: a guidance statement from The Society of Thoracic Surgeons COVID‐19 Task Force. Ann Thorac Surg. 2020;110:712‐717. 10.1016/j.athoracsur.2020.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Engelman DT, Lother S, George I, et al. Adult cardiac surgery and the COVID‐19 pandemic: aggressive infection mitigation strategies are necessary in the operating room and surgical recovery. J Thorac Cardiovasc Surg. 2020;160:447‐451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Foy D, Mallory L. Healthcare leaders: 3 steps to a better safety culture. Updated June 18, 2020. https://www.gallup.com/workplace/312521/steps-healthcare-leaders-during-coronavirus.aspx. Accessed July 23, 2020.
- 41. Engelman DT, Ben Ali W, Williams JB, et al. Guidelines for perioperative care in cardiac surgery: enhanced Recovery After Surgery Society recommendations. JAMA Surg. 2019;154:755‐766. [DOI] [PubMed] [Google Scholar]
- 42. Gregory AJ, Grant MC, Boyle E, et al. Cardiac surgery enhanced recovery programs modified for COVID‐19: key steps to preserve resources, manage caseload backlog, and improve patient outcomes [published online ahead of print August 10, 2020]. J Cardiothorac Vasc Anesth. 2020. 10.1053/j.jvca.2020.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zaouter C, Oses P, Assatourian S, Labrousse L, Rémy A, Ouattara A. Reduced length of hospital stay for cardiac surgery‐implementing an optimized perioperative pathway: prospective evaluation of an enhanced recovery after surgery program designed for mini‐invasive aortic valve replacement. J Cardiothorac Vasc Anesth. 2019;33:3010‐3019. [DOI] [PubMed] [Google Scholar]
- 44. Kluger J, Wilson G. America is done with COVID‐19. COVID‐19 isn't done with America. TIME Magazine: health—COVID‐19. June 12, 2020. https://time.com/5852913/covid-second-wave/. Accessed July 30, 2020.
- 45. Hellman J. Florida, Texas and Arizona set records for daily COVID‐19 cases. The Hill. Updated June 17, 2020. https://thehill.com/policy/healthcare/503199-florida-texas-and-arizona-set-records-for-daily-covid-19-cases. Accessed July 30, 2020.
- 46. Lyu W, Wehby GL. Community use of face masks and COVID‐19: evidence from a natural experiment of state mandates in the US. Health Aff (Millwood). 2020;39:1419‐1425. 10.1377/hlthaff.2020.00818 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data in this report were extracted from the medical records of specific patients. The numbers presented are either publicly available on the TMC website or aggregated from internal databases.


