Abstract
The SARS‐CoV‐2 pandemic has caused a yet unresolved global crisis. Effective medical intervention by vaccination or therapy seems to be the only possibility to control the pandemic. In this context, animal models are an indispensable tool for basic and applied research to combat SARS‐CoV‐2 infection. Here, we established a SARS‐CoV‐2 infection model in Chinese hamsters suitable for studying pathogenesis of the disease as well as pre‐clinical testing of vaccines and therapies. This species of hamster is susceptible to SARS‐CoV‐2 infection as demonstrated by robust virus replication in the upper and lower respiratory tract accompanied by bronchitis and pneumonia as well as significant body weight loss following infection. The Chinese hamster features advantages compared to the Syrian hamster model, including more pronounced clinical symptoms, its small size, well‐characterized genome, transcriptome and translatome data and availability of molecular tools.
Keywords: coronavirus, experimental animal models, histopathology
1. INTRODUCTION
The rapid worldwide spread of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) has caused an unparalleled crisis and requires urgent testing of prophylactic and therapeutic measures. SARS‐CoV‐2 likely emerged from a yet unknown animal reservoir; its rapid spread can be attributed to efficient replication in the upper respiratory tract and robust human‐to‐human transmission. This characteristic clearly distinguishes this novel coronavirus from the related SARS‐CoV‐1 and MERS‐CoV (Andersen et al., 2020). Interestingly, SARS‐CoV‐2 human‐to‐animal transmissions have also been reported (Halfmann et al., 2020; Leroy et al., 2020). Currently, we find ourselves racing for efficacious therapies and protective vaccinations. In this context, small animal models are indispensable as pre‐clinical studies in animals are of critical importance for basic and applied research on SARS‐CoV‐2 infection. Several SARS‐CoV‐2 animal models have been investigated, including non‐human primates, ferrets, transgenic mice, cats and hamsters, (Chan et al., 2020; Dhama et al., 2020; Imai et al., 2020; Lakdawala & Menachery, 2020; Osterrieder et al., 2020; Sia et al., 2020; Trimpert et al., 2020; Yuan et al., 2020). However, in silico models with respect to potential usage of the entry receptor by the spike glycoprotein (S) of SARS‐CoV‐2 suggest susceptibility of Chinese hamsters (Cricetulus griseus) (Luan et al., 2020; Luan et al., 2020) and a previous study in Chinese hamsters demonstrated susceptibility to SARS‐CoV‐1 (Luo et al., 2007). We here determined SARS‐CoV‐2 susceptibility of Chinese hamsters and established this species as novel small animal model for SARS‐CoV‐2 research.
2. MATERIALS AND METHODS
2.1. Viruses and cells
The SARS‐CoV‐2 München isolate (BetaCoV/Germany/BavPat1/2020) (Wölfel et al., 2020) was used for virus challenge. Stocks were propagated and titrated on Vero E6 cells (ATCC CRL‐1586) in minimal essential medium (MEM; PAN Biotech, Aidenbach, Germany) supplemented with 10% foetal bovine serum (PAN Biotech), 100 IU/ml penicillin G and 100 µg/ml streptomycin (Carl Roth, Karlsruhe, Germany) and stored at −80°C prior to experimental infections.
2.2. Experimental infection of Chinese hamsters
24 five‐ to seven‐week‐old female and male Chinese hamsters (Cricetulus griseus) were obtained via the German pet trade and kept in groups of six animals in enriched, individually ventilated cages. The hamsters had ad libidum access to food and water, and were allowed acclimatization to these conditions for seven days prior to SARS‐CoV‐2 infection. Cage temperatures and relative humidities were recorded daily and ranged from 23 to 24°C and from 50% to 65%, respectively. The animals were randomly distributed into two groups: SARS‐CoV‐2‐infected (n = 12; 1 × 105 plaque‐forming units (pfu) in a volume of 30 µl) and mock‐infected (n = 12; 30 µl cell culture supernatant from uninfected Vero E6 cells). The infection was performed exactly as previously described (Osterrieder et al., 2020). Baseline body weights of all hamsters and body temperatures of at least three hamsters per group were measured before infection and then recorded daily throughout the 14‐day experiment. Moreover, clinical signs of all animals were monitored twice daily throughout the experiment. On days 2, 3, 5 and 14 post‐infection (dpi), three randomly assigned hamsters of each group were euthanized by exsanguination under general anaesthesia as described (Nakamura et al., 2017). For virus titrations and RT‐qPCR and/or histopathological examinations, blood, bucco‐laryngeal swabs and lungs (left and right) were collected.
2.3. Histopathology and in situ hybridization
For histopathology, lungs were processed as previously described (Osterrieder et al., 2020). In brief, the left lung lobe was carefully removed and immersion fixed in buffered 4% formalin, pH 7.0, for 48 hr, embedded in paraffin and cut at 2 μm thickness. Sections were stained with haematoxylin and eosin (HE) followed by blinded microscopic evaluation by board certified veterinary pathologists (K.D., A.D.G.). For in situ hybridization (ISH), the ViewRNA™ ISH Tissue Assay Kit (Invitrogen by Thermo Fisher Scientific, Darmstadt, Germany) was used following the manufacturer's instructions with minor adjustments. A probe for the detection of the N gene RNA of SARS‐CoV‐2 (NCBI database NC_045512.2, nucleotides 28,274–29,533, assay ID: VPNKRHM) was employed. Next, lung sections of 2 μm thickness were mounted on adhesive glass slides, dewaxed in xylol and dehydrated in graded ethanols. Tissues were incubated at 95°C for 10 min, and subsequently, protease digested for 20 min. Sections were fixed with 4% paraformaldehyde dissolved in phosphate‐buffered saline (PBS) and hybridized with the probes. Amplifier and label probe hybridizations were performed according to the manufacturer's instructions using fast red as chromogen. Sections were counterstained with haematoxylin for 45 s, washed in tap water for 5 min and mounted with Roti®‐Mount Fluor‐Care DAPI (4, 6‐diaminidino‐2‐phenylindole; Carl Roth). For negative and morphologically intact controls, lungs from uninfected hamsters were included. An irrelevant probe for the detection of streptococcal pneumolysin was used as a control for sequence‐specific binding. HE‐stained and ISH slides were analysed and photographs were taken using an Olympus BX41 microscope with a DP80 Microscope Digital Camera and the cellSens™ Imaging Software, Version 1.18 (Olympus Corporation, Münster, Germany). For overviews, slides were automatically digitized using the Aperio CS2 slide scanner (Leica Biosystems Imaging Inc., Vista, CA, USA) followed by image file generation using the Image Scope Software (Leica Biosystems Imaging Inc.).
2.4. Virus titrations, RNA extractions and RT‐qPCR
Virus titres from 50 mg lung tissue were assessed by serial dilution of tissue homogenates and subsequent titrations on Vero E6 cells. 3 dpi, cells were formalin‐fixed, stained with crystal violet, and plaques were counted. RNA was extracted from tissue samples, blood and tracheal swabs using the innuPREP Virus RNA kit (Analytic Jena, Jena, Germany) and quantified with a one‐step RT‐qPCR reaction (NEB Luna Universal Probe One‐Step RT‐qPCR kit; New England Biolabs, Ipswitch, MA, USA) and previously published TaqMan primers and probe (Corman et al., 2020).
2.5. Statistical analyses
Data were analysed with GraphPad PRISM. We used Mann–Whitney U tests to compare body weights and body temperatures in mock‐infected versus SARS‐CoV‐2 infected Chinese hamsters. Data were considered significant if p < .05 (*p < .05; **p < .01).
3. RESULTS AND DISCUSSION
The study, which was approved by the Landesamt für Gesundheit und Soziales in Berlin, Germany (permit # 0086/20), involved 24 female and male Chinese hamsters of 5–7 weeks of age. Hamsters were randomly assigned to two groups (SARS‐CoV‐2‐infected, n = 12; mock‐infected, n = 12) Upon intranasal infection with 1x105 plaque‐forming units (pfu) of a human SARS‐CoV‐2 isolate, we observed clinical symptoms including transient but significant body weight loss and subtle drops in body temperatures at early time points after infection, a course of disease comparable to that in Syrian hamsters (Figure 1) (Chan et al., 2020; Imai et al., 2020; Kreye et al., 2020; Osterrieder et al., 2020; Sia et al., 2020). Differences in body weights between infected and mock‐infected animals were significant at 1–3 and at 5 days post‐infection (dpi), infected hamsters did not reach pre‐infection body weights before 14 dpi when the experiment was terminated (Figure 1a). However, the largest difference in mean body temperatures of infected compared to mock‐infected animals was only −0.6°C at 3 dpi (Figure 1b), suggesting that this parameter may not be useful to assess the status of infection. We determined virus replication and virus spread by measuring RNA copy numbers in the lungs, bucco‐laryngeal swabs and whole blood samples of all hamsters (Figure 1c–e).
Figure 1.
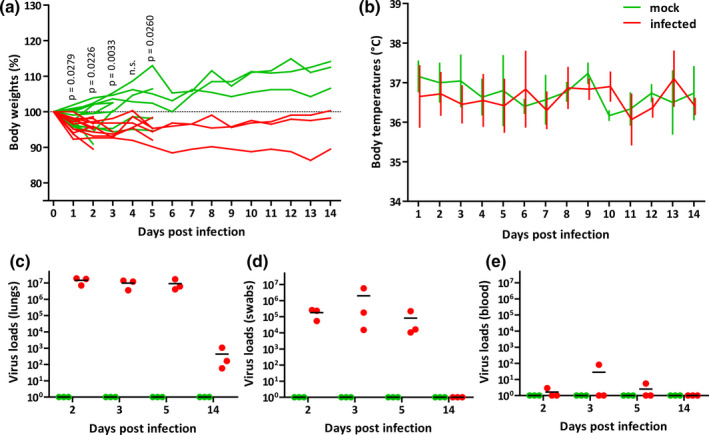
Body weight changes, body temperatures and virus loads of mock‐infected and SARS‐CoV‐2‐infected Chinese hamsters. (a) Individual relative body weights of mock‐infected (green) and SARS‐CoV‐2‐infected (red) hamsters over the course of 14 days after infection. p‐values indicate significant differences (Mann–Whitney U test). (b) Temperature changes (as means with SD). Virus loads were determined from total RNA in (c) 2.5 mg homogenized right cranial lung lobes, in (d) bucco‐laryngeal swabs and (e) 2.5 µl of whole blood samples by RT‐qPCR [Colour figure can be viewed at wileyonlinelibrary.com]
In addition, we determined viral titres in the lungs of infected animals (Figure S1). Our assays confirmed high RNA copy numbers and corresponding viral titres at early time points after infection followed by a rapid but incomplete clearance of the virus infection until 14 dpi. With titres of up to 5 × 107 pfu per 50 mg lung tissue and viral RNA copies in the range of up to 1 × 107 per 2.5 mg lung tissue at early time points after infection, we concluded that Chinese hamsters are highly susceptible to SARS‐CoV‐2. On the other hand, virus loads in blood samples were below 1 × 102 RNA copies per 2.5 µl of whole blood (15.6 ± 29.8 SD) at all time points, indicating lack of significant viremia and systemic infection (Figure 1e). These observations match findings from other animal models for emerging coronaviruses (Yuan et al., 2020).
Lung histopathology revealed tissue damage and inflammation principally similar to what has been described in Syrian hamsters (Figure 2) (Chan et al., 2020; Gruber et al., 2020; Imai et al., 2020; Kreye et al., 2020; Osterrieder et al., 2020; Sia et al., 2020). However, the course of bronchitis and pneumonia was in general milder than in Syrian hamsters, and pneumonia was more prolonged. Specifically, prominent acute alveolar damage was present until 14 dpi with persistence of viral RNA (Figures 1c, 2g‐i and S2), indicating overall slower recovery than described for Syrian hamsters. Similarly, viral RNA was localized by in situ hybridization to bronchial epithelial cells, alveolar epithelial cells type‐I and type‐II and alveolar macrophages (Figure S2, arrows).
Figure 2.
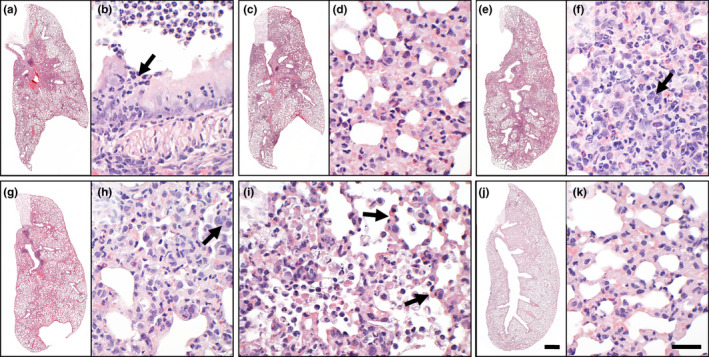
Histopathological assessment of mock‐infected and SARS‐CoV‐2‐infected Chinese hamsters. Histopathology of haematoxylin–eosin‐stained lung sections from SARS‐CoV‐2‐infected Chinese hamsters revealed suppurative bronchitis (a, b; arrow: neutrophils) and necrosuppurative pneumonia (c, d) at 2 and 3 dpi. At 5 dpi (e, f), additional hyperplasia of alveolar epithelial cells (AEC)‐type II was salient (f, arrow). Tissue damage, cell influx and hyperplasia of AEC‐II (h, arrow) were milder but still present at 14 dpi (g, h). Of note, acute alveolar damage (I, arrows) was multifocally distributed throughout the lungs across all time points investigated. None of these lesions was detected in mock‐infected animals (j, k). Bars: 1 mm (a, c, e, g, j) or 50 µm (b, d, f, h, i, k) [Colour figure can be viewed at wileyonlinelibrary.com]
In agreement with the clinical course of disease, virological and histopathological results confirm that this animal model withstands the comparison with the Syrian hamster model with the advantage of a prolonged period of significantly reduced body weights following infection with SARS‐CoV‐2. Moreover, the considerably smaller size of the Chinese hamster offers an important practical advantage when compared to the rather large Syrian hamster and allows husbandry in smaller cages and lager groups. Additionally, the Chinese hamster genome, transcriptome and translatome are well characterized and a variety of molecular tools is available for this species as Chinese hamster ovary (CHO) cells are widely used in biopharmaceutical research and industry (Matasci et al., 2008; Walsh, 2018). At the same time, the usefulness of any model depends on fundamental knowledge of species‐specific similarities to and differences from the human disease, as well as other confounding factors, including age and comorbidities (Metersky & Waterer, 2020). Because of the heterogeneous disease phenotype in humans, there is a need for different SARS‐CoV‐2 animal models that allow evaluation of vaccines and antiviral therapies for different subsets of the human population.
Taken together, our results suggest the suitability of the Chinese hamster small animal model to study SARS‐CoV‐2 infections, with body weight losses as a robust clinical disease parameter. As an established model for SARS‐CoV‐1 infection, the Chinese hamster may also allow comparison between experimental coronavirus infections. Moreover, our findings highlight the possibility of comparing, in future studies, the effects of preventive as well as therapeutic measures to restrain infection and viral replication in different animal models.
CONFLICT OF INTEREST
The authors declare no competing interests.
AUTHOR CONTRIBUTIONS
NO and JT were involved in conceptualization. LDB, DV, KD, AA, ADG and JT were involved in investigation. LDB, DV, KD, ADG, NO and JT were involved in writing. All authors were involved in editing and had the opportunity to comment on the draft manuscript.
ETHICAL APPROVAL
The authors confirm that the ethical policies of the journal, as noted on the journal's author guidelines page, have been adhered to, and the appropriate ethical review committee approval has been received. Animal experimentations were approved by the Landesamt für Gesundheit und Soziales in Berlin, Germany (AUP number 0086/20) and performed in compliance with relevant national and international guidelines for care and humane use of animals. All in vitro and animal work was conducted under appropriate biosafety conditions in the BSL‐3 facility at the Institute of Virology, Freie Universität Berlin, Germany.
Supporting information
Fig S1‐S2
ACKNOWLEDGMENTS
We cordially thank Ann Reum, Annett Neubert, Jana Enders, Angela Linke and Michaela Scholz for excellent technical assistance. This research was supported by COVID‐19 grants from Freie Universität Berlin and the Berlin University Alliance to N.O. and J.T. and the Deutsche Forschungsgemeinschaft grant SFB‐TR84/Z01b awarded to A.D.G and J.T. Open access funding enabled and organized by Projekt DEAL.
Bertzbach LD, Vladimirova D, Dietert K, et al. SARS‐CoV‐2 infection of Chinese hamsters (Cricetulus griseus) reproduces COVID‐19 pneumonia in a well‐established small animal model. Transbound. Emerg. Dis. 2021;68:1075–1079. 10.1111/tbed.13837
Bertzbach and Vladimirova equally contributed to this article.
DATA AVAILABILITY STATEMENT
All data relevant to this study are included in the manuscript and supplementary information.
REFERENCES
- Andersen, K. G. , Rambaut, A. , Lipkin, W. I. , Holmes, E. C. , & Garry, R. F. (2020). The proximal origin of SARS‐CoV‐2. Nature Medicine, 26(4), 450–452. 10.1038/s41591-020-0820-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, J. F. , Zhang, A. J. , Yuan, S. , Poon, V. K. , Chan, C. C. , Lee, A. C. , … Yuen, K. Y. (2020). Simulation of the clinical and pathological manifestations of Coronavirus Disease 2019 (COVID‐19) in golden Syrian hamster model: Implications for disease pathogenesis and transmissibility. Clinical Infectious Diseases, ciaa325. 10.1093/cid/ciaa325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corman, V. M. , Landt, O. , Kaiser, M. , Molenkamp, R. , Meijer, A. , Chu, D. K. , … Drosten, C. (2020). Detection of 2019 novel coronavirus (2019‐nCoV) by real‐time RT‐PCR. Eurosurveillance, 25(3), 2000045. 10.2807/1560-7917.ES.2020.25.3.2000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhama, K. , Khan, S. , Tiwari, R. , Sircar, S. , Bhat, S. , Malik, Y. S. , … Rodriguez‐Morales, A. J. (2020). Coronavirus Disease 2019–COVID‐19. Clinical Microbiology Reviews, 33(4). 10.1128/CMR.00028-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber, A. D. , Osterrieder, N. , Bertzbach, L. D. , Vladimirova, D. , Greuel, S. , Ihlow, J. , … Dietert, K. (2020). Standardization of Reporting Criteria for Lung Pathology in SARS‐CoV‐2 Infected Hamsters – What Matters? American Journal of Respiratory Cell and Molecular Biology. 10.1165/rcmb.2020-0280LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halfmann, P. J. , Hatta, M. , Chiba, S. , Maemura, T. , Fan, S. , Takeda, M. , & Kawaoka, Y. (2020). Transmission of SARS‐CoV‐2 in domestic cats. New England Journal of Medicine, 383(6), 592–594. 10.1056/NEJMc2013400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, M. , Iwatsuki‐Horimoto, K. , Hatta, M. , Loeber, S. , Halfmann, P. J. , Nakajima, N. , … Kawaoka, Y. (2020). Syrian hamsters as a small animal model for SARS‐CoV‐2 infection and countermeasure development. Proceedings of the National Academy of Sciences of the United States of America, 117(28), 16587–16595. 10.1073/pnas.2009799117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreye, J. , Reincke, S. M. , Kornau, H. C. , Sanchez‐Sendin, E. , Corman, V. M. , Liu, H. , Pruess, H. (2020). A SARS‐CoV‐2 neutralizing antibody protects from lung pathology in a COVID‐19 hamster model. bioRxiv. 10.1101/2020.08.15.252320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakdawala, S. S. , & Menachery, V. D. (2020). The search for a COVID‐19 animal model. Science, 368(6494), 942–943. 10.1126/science.abc6141 [DOI] [PubMed] [Google Scholar]
- Leroy, E. M. , Ar Gouilh, M. , & Brugere‐Picoux, J. (2020). The risk of SARS‐CoV‐2 transmission to pets and other wild and domestic animals strongly mandates a one‐health strategy to control the COVID‐19 pandemic. One Health, 100133. 10.1016/j.onehlt.2020.100133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luan, J. , Jin, X. , Lu, Y. , & Zhang, L. (2020). SARS‐CoV‐2 spike protein favors ACE2 from Bovidae and Cricetidae. Journal of Medical Virology. 10.1002/jmv.25817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luan, J. , Lu, Y. , Jin, X. , & Zhang, L. (2020). Spike protein recognition of mammalian ACE2 predicts the host range and an optimized ACE2 for SARS‐CoV‐2 infection. Biochemical and Biophysical Research Communications, 526(1), 165–169. 10.1016/j.bbrc.2020.03.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, D. , Ni, B. , Zhao, G. , Jia, Z. , Zhou, L. , Pacal, M. , & Wang, X. (2007). Protection from infection with severe acute respiratory syndrome coronavirus in a Chinese hamster model by equine neutralizing F(ab')2. Viral Immunology, 20(3), 495–502. 10.1089/vim.2007.0038 [DOI] [PubMed] [Google Scholar]
- Matasci, M. , Hacker, D. L. , Baldi, L. , & Wurm, F. M. (2008). Recombinant therapeutic protein production in cultivated mammalian cells: Current status and future prospects. Drug Discovery Today: Technologies, 5(2–3), e37–42. 10.1016/j.ddtec.2008.12.003 [DOI] [PubMed] [Google Scholar]
- Metersky, M. , & Waterer, G. (2020). Can animal models really teach us anything about pneumonia? Con. European Respiratory Journal, 55(1), 1901525. 10.1183/13993003.01525-2019 [DOI] [PubMed] [Google Scholar]
- Nakamura, T. , Karakida, N. , Dantsuka, A. , Ichii, O. , Elewa, Y. H. A. , Kon, Y. , & Yoshiyasu, T. (2017). Effects of a mixture of medetomidine, midazolam and butorphanol on anesthesia and blood biochemistry and the antagonizing action of atipamezole in hamsters. Journal of Veterinary Medical Science, 79(7), 1230–1235. 10.1292/jvms.17-0210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterrieder, N. , Bertzbach, L. D. , Dietert, K. , Abdelgawad, A. , Vladimirova, D. , Kunec, D. , & Trimpert, J. (2020). Age‐Dependent Progression of SARS‐CoV‐2 Infection in Syrian Hamsters. Viruses, 12(7), 779. 10.3390/v12070779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sia, S. F. , Yan, L. M. , Chin, A. W. H. , Fung, K. , Choy, K. T. , Wong, A. Y. L. , & Yen, H. L. (2020). Pathogenesis and transmission of SARS‐CoV‐2 in golden hamsters. Nature, 583(7818), 834–838. 10.1038/s41586-020-2342-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trimpert, J. , Vladimirova, D. , Dietert, K. , Abdelgawad, A. , Kunec, D. , Dökel, S. , … Osterrieder, N. (2020). The Roborovski Dwarf Hamster – A highly susceptible model for a rapid and fatal course of SARS‐CoV‐2 infection. Social Science Research Network (SSRN). 10.2139/ssrn.3659394 (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh, G. (2018). Biopharmaceutical benchmarks 2018. Nature Biotechnology, 36(12), 1136–1145. 10.1038/nbt.4305 [DOI] [PubMed] [Google Scholar]
- Wölfel, R. , Corman, V. M. , Guggemos, W. , Seilmaier, M. , Zange, S. , Müller, M. A. , & Wendtner, C. (2020). Virological assessment of hospitalized patients with COVID‐2019. Nature, 581(7809), 465–469. 10.1038/s41586-020-2196-x [DOI] [PubMed] [Google Scholar]
- Yuan, L. , Tang, Q. , Cheng, T. , & Xia, N. (2020). Animal models for emerging coronavirus: Progress and new insights. Emerging Microbes & Infections, 9(1), 949–961. 10.1080/22221751.2020.1764871 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1‐S2
Data Availability Statement
All data relevant to this study are included in the manuscript and supplementary information.


