Abstract
Aim
COVID‐19 has affected millions of people worldwide. This paper reviews the Swedish pandemic response.
Methods
A narrative review was carried out and a timeline constructed.
Results
By September 1, 2020, 0.8% of Swedish residents had tested positive for the virus and 0.06% of the population had died, which was higher than neighbouring Nordic countries, but lower than some European countries with general lockdowns. The main actors were the Public Health Agency, the National Board of Health and Welfare, the Civil Contingencies Agency and the Government. County councils and regions implemented policies, in conjunction with the Department of Education and county administrative boards. Sweden's response was less invasive than many other countries, with no general lockdown. It focused on mitigation: slowing, but not stopping, the pandemic. Physical distancing was recommended in public spaces, but mandatory in bars, restaurants and at events. Visits to nursing facilities were banned. Kindergartens and schools for children up to 16 stayed open, but closed for older children for three months. There were no enforced quarantines for infected households or geographical regions, and facemasks were not recommended outside health care.
Conclusion
Sweden chose a different pandemic strategy to its peer nations. This paper examines the first eight months.
Keywords: coronavirus, COVID‐19, pandemic, social distancing, transmission
Abbreviations
- COVID‐19
coronavirus disease 2019
- ICU
intensive care unit
- PHA
Swedish Public Health Agency
Key Notes.
Sweden's response to COVID‐19 was less invasive than many other countries during the first eight months, with no general lockdown and a focus on slowing, not stopping, the pandemic.
This review of the timeline and key actors shows that schools for children up to 16 were kept open, but older children studied at home.
Physical distancing was strongly recommended, and mandatory in some situations, but facemasks were not recommended outside health care.
1. INTRODUCTION
The World Health Organization (WHO) classified COVID‐19 as a threat to human health on January 30, 2020, and upgraded it to a pandemic on March 11. Since then, many countries have taken extensive steps to restrict transmission, but Sweden adopted a more measured approach, without the national lockdowns instigated by many of its European neighbours. The actions taken in Sweden in the eight months up to September 1, and the key actors who were involved, can be seen in the detailed timeline that accompanies this paper (Figure 1).
Figure 1.
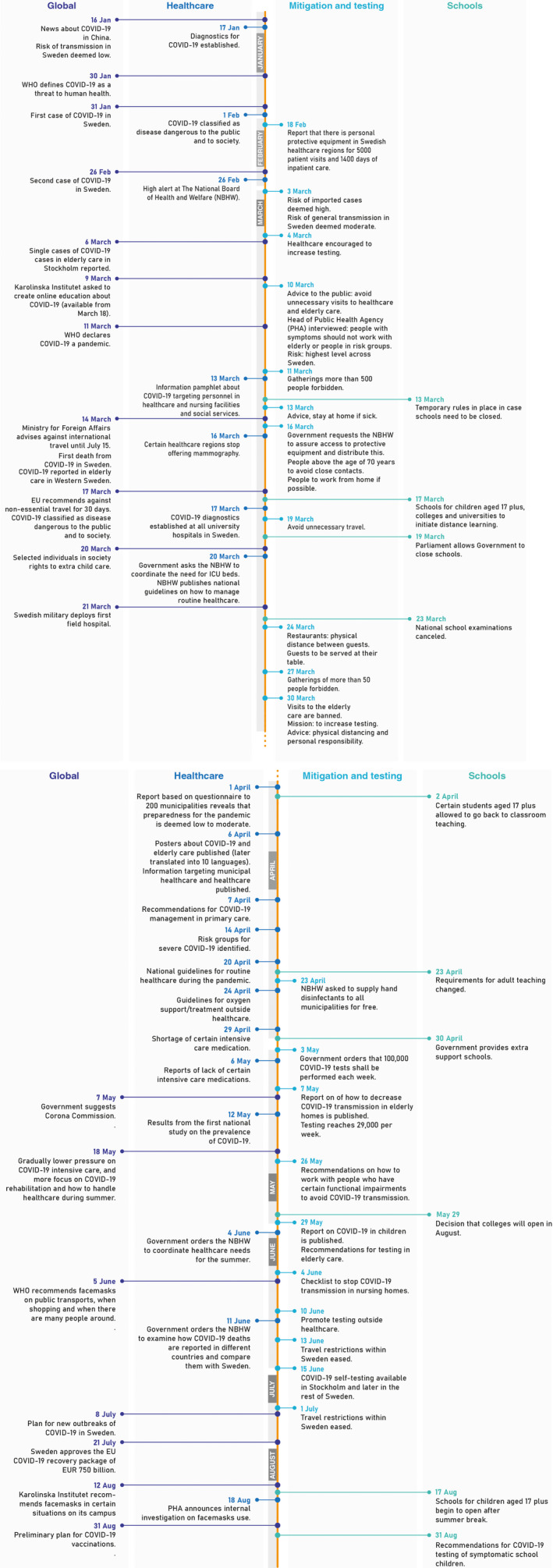
Timeline of the Swedish COVID‐19 strategy (parts 1 and 2). ICU, intensive care unit; NBHW, Swedish National Board of Health and Welfare; PHA, Swedish Public Health Agency. Data sources: NBHW, PHA and the Department of Education
Earlier reviews on Sweden's pandemic response have been published, 1 but there have been little data on what has set Sweden apart from other countries. These differences include the timing of pandemic‐related actions, the way that COVID‐19 has been coded in medical records, how different parts of the healthcare system reacted to the pandemic and the legal framework covering the relationship between the Government and other actors. They also include actions taken with regard to schools.
This paper covers the eight‐month period up to September 1 and presents a detailed timeline on how Sweden flattened the curve, protected elderly and risk groups and ensured that health and medical care resources were available in all regions. Less attention is paid to actions that primarily sustained the economy.
2. METHODS
National government agencies were contacted by email in July to August 2020, and web pages and reports were examined. The study period was the eight months ending September 1, 2020.
3. RESULTS
3.1. COVID‐19 in Sweden
By September 2020, 84 521 Sweden residents had tested positive for the virus, 2560 had been admitted to an intensive care unit (ICU) and 5813 had died. These represented 0.8%, 0.03% and 0.06% of the total population, respectively (Figure 2). The number of deaths from all causes in Sweden between March 1 and August 25 was 46 746, an excess mortality rate of 11% compared with the average death rate of 41 934 for 2015‐2019 (Figure 3). However, when the calculations included January and February, which is when influenza is generally prevalent in Sweden, the overall weekly mortality rate per one million people between January and June was very similar for the years between 2015 and 2020:187, 176, 180, 179, 165 and 187, respectively.
Figure 2.
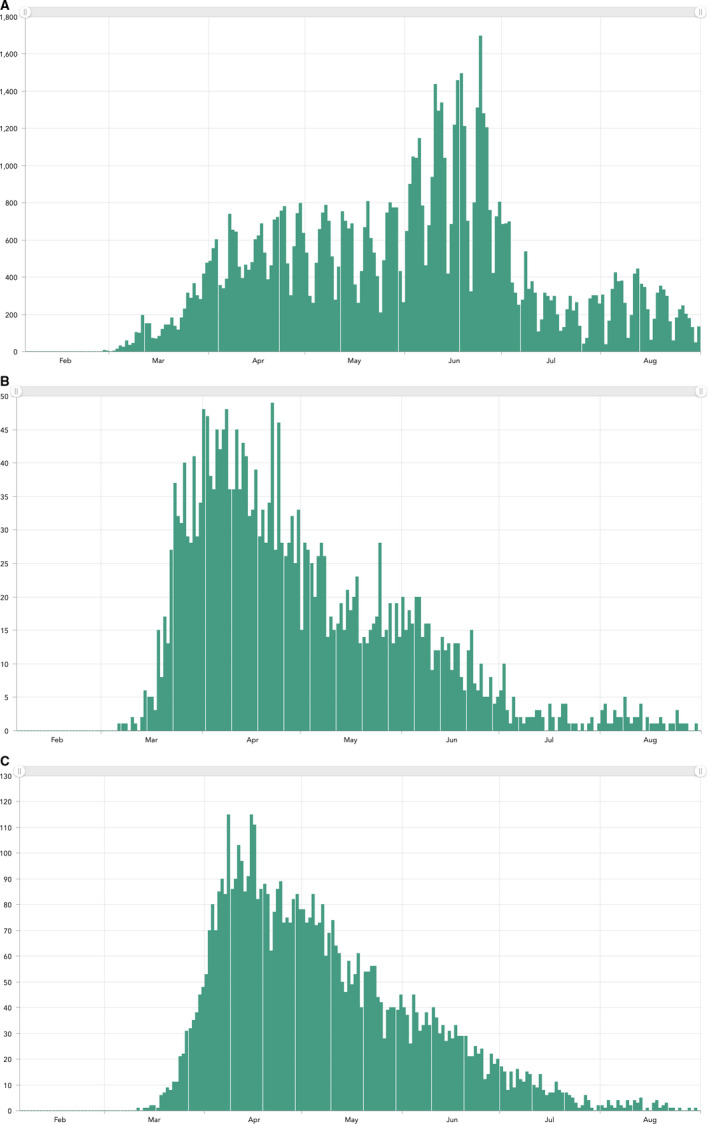
A, Incidence of COVID‐19 cases in Sweden from February 1 to August 31, 2020 (source: Swedish Public Health Agency). B, Incidence of COVID‐19 cases admitted to Swedish intensive care units from February 1 to August 31, 2020 (source: Swedish Public Health Agency). C, Deaths from COVID‐19 in Sweden from February 1 to August 31, 2020 (source: Swedish Public Health Agency)
Figure 3.
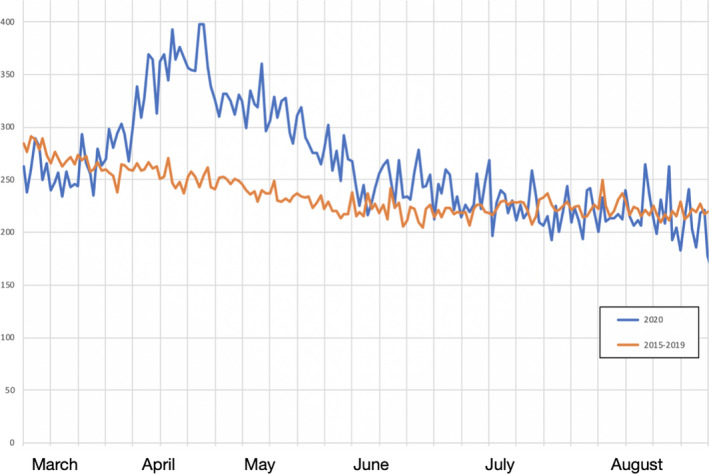
Number of deaths (any cause) per day in Sweden from March 1 to August 31, 2020, compared with the average rates for 2015‐2019. The excess mortality rate during these 6 mo was 11%. (Source: Statistics Sweden)
Regional differences were large, with the Stockholm region, which is home to 22.3% of the Swedish population, being severely affected. More details on regional differences can be found on the Statistics Sweden website and in Kavaliunas et al. 1
COVID‐19 has been registered in Swedish healthcare registers using the U07 emergency codes from the International Classification of Diseases, Tenth Revision (ICD‐10), namely U07.1 for COVID‐19, virus identified, and U07.2 for COVID‐19, virus not identified. These codes have previously been used for other healthcare emergencies.
Swedish paediatricians have generally assigned children with multi‐inflammatory syndrome, 2 , 3 which has been linked with COVID‐19, to U07.1 or U07.2, and some have used ICD‐10 code M30.3 for Kawasaki disease, or M35.8 (Other specified systemic involvement of connective tissue).
3.2. The Swedish population
According to Statistics Sweden, the country had a population of 10 327 589 in December 2019. Of these, 20.7% were children under the age of 18 and 33.1% were either born outside the country (19.6%) or had at least one parent born outside Sweden.
In addition, 19.6% of the Swedish population were 65 years or older at this date, which is the cut‐off age used by the Swedish Intensive Care Register 4 for its risk group classification. Special recommendations have been issued for people aged 70 years or above, who accounted for 14.5% of the population.
3.3. Administrative regions and Swedish health care
Sweden is divided into 290 municipalities and 21 county councils and regions, which are run by elected politicians.
The municipalities are responsible for Government‐funded community health and nursing services, but not those provided by commercial organisations and charities. Many older people require home care and these services are often provided by visiting nurses, who liaise with family doctors and various healthcare departments.
Swedish health care is carried out by the 21 county councils and regions, funded by taxes and universally available. 5 , 6 The Government‐funded healthcare system comprises primary care and hospital‐based outpatient and inpatient care. Hospital visits are recorded in the Swedish Patient Register, 7 but primary care visits are not. During the pandemic, patients with severe cases of COVID‐19 were cared for by Sweden's 83 ICUs, who reported all cases to the Swedish Intensive Care Register. 4 The data on COVID‐19–positive cases in the Intensive Care Register were cross‐validated against data from the Swedish Public Health Agency (PHA).
Each of the county councils and regions has infectious disease units that aim to prevent the spread of infections, through epidemiological surveillance, information and education and by identifying cases. The units have wide‐ranging authority, including the power to order quarantine. Their work is regulated by the Infectious Diseases Act 2004:168, which is discussed later.
3.4. Main actors
The main actors involved in the pandemic response all interacted, and often informed and advised, the Swedish Government (Appendix 1).
The PHA provides information to the Swedish Government and other key actors. It is overseen by a transparency council that mostly comprises members with experience of politics, health care or research. The PHA has set up a temporary COVID‐19 unit. Its other areas of responsibility are public health, communication and support, lifestyle and living conditions, microbiology and infectious disease control. Throughout the pandemic, the PHA has formulated measures using an evidence‐based approach.
The National Board of Health and Welfare aims to provide equal access to good health, social welfare and high‐quality health and social care. It issues national guidelines and general medical recommendations and oversees national screening programmes. During the pandemic, its number one priority has been to ensure a sufficient number of COVID‐19 beds.
The Swedish Civil Contingencies Agency analyses the short‐term and long‐term consequences of COVID‐19, including the impact on society, supports collaboration between different actors and is responsible for COVID‐19 public information campaigns.
The Department of Education is responsible for schools, colleges and university education, adult education, educational funding and the Government's research policy. It works closely with the Swedish National Agency for Education. This Agency is responsible for overseeing online and distance education for students if their schools are closed and enforcing attendance rules if they are open.
3.5. Other actors
The other actors have included Swedish universities, who encouraged COVID‐19 research. The Ministry for Foreign Affairs has provided travel advice and assisted repatriation. The Medical Product Agency has co‐ordinated discussions about medication and is likely to play an important role in any vaccination campaign. External actors that have influenced the Swedish COVID‐19 strategy include the WHO and the European Union (EU) and its agency, the European Centre for Disease Control.
4. LEGAL FRAMEWORK
4.1. The pandemic
Two main laws regulate COVID‐19 in Sweden. The Infectious Diseases Act 2004:168 states that everyone has a personal responsibility to limit the transmission of infectious diseases. The Code of Conduct 1993:1617 protects public health.
4.2. The Swedish Constitution
In an article, in the Swedish daily newspaper Dagens Nyheter on August 1, 2020, Jonung and Nergelius reviewed the legal framework for the pandemic in Sweden. 8 They suggested that the main reason for avoiding a general lockdown was that since 1974 the Swedish Constitution has stipulated that ‘Swedish citizens have the right to move freely within Sweden and leave the country’.
Although the Swedish Infectious Diseases Act can restrict individuals, it does not allow for a general lockdown, which is why so many COVID‐19 measures in Sweden have been voluntary, rather than compulsory. The Constitution also stipulates that the Government cannot influence how individual Government agencies carry out their work, especially with regard to individual citizens. Government Ministers have been able to voice their opinions, but have had no power to override the actions of independent agencies. The PHA plays a very strong role in Sweden, and while the Government can reject the PHA’s recommendations, it has traditionally followed them.
The Swedish Constitution stipulates that municipalities enjoy local self‐government. They have elected assemblies, who can tax residents and are responsible for local matters such as infrastructure, housing, business development, schools and elderly care. Municipalities legally share power with the Government, and this decentralised responsibility is likely to have had an impact on the early decision‐making during the pandemic.
5. INTERVENTIONS
Sweden's response to COVID‐19 has been less invasive than in many other countries, with no general lockdown. Bars, restaurants, public spaces, kindergartens and schools for children up to the age of 16 continued to operate throughout the pandemic, but schools for older children were closed for three months. Sweden did not enforce quarantine for infected households, or for parts of the country, in the first eight months. Physical distancing was strongly recommended, but was only mandatory in bars, restaurants, at events and when visiting elderly care homes. Wearing facemasks was not recommended. People were urged to work from home, if possible, to minimise travel. Although the recommendations were mainly voluntary, an opinion poll in early April found that 98% of respondents had changed their behaviour to protect themselves from COVID‐19. 9 A poll in early May found that 87% of respondents kept a greater distance from other people when shopping, visiting restaurants or using public transport. 10
Sweden's COVID‐19 strategy had eight key aims up to September 1 11 : first, to use mitigation, rather than suppression, by minimising COVID‐19 transmission to flatten the curve and ensure that large numbers of people were not ill at the same time; second, to protect those groups at greatest risk, who were mainly individuals aged 70 years or above; third, to safeguard other health determinants and health outcomes, including keeping schools for children up to 16 open; fourth, to ensure that health and medical care resources were available in all regions and to avoid a healthcare collapse; fifth, to ensure that society could continue to function, including health care, the police, energy supplies, communications, transport and food supply systems; sixth, to ease public concerns and communicate with all residents through official website information and regular press conferences; seventh, to explain the underlying reasons for the measures taken; and last, but not least, to implement the right measures at the right time. It is worth noting that the PHA has repeatedly denied that attaining herd immunity was part of Sweden's strategy.
5.1. Analysis of risk of COVID‐19 transmission
News of COVID‐19 12 reached Sweden in mid‐January, and the risk of transmission to Sweden was deemed to be low. One early model published in the Lancet assumed that transmission would principally affect major urban areas in China and cities outside China with frequent air travel to Wuhan, such as Bangkok, Seoul, Singapore and Tokyo. 13 However, COVID‐19 soon spread outside China and Asia. In February, Swedish travellers from China, and later South Korea, Italy and Iran, were urged to be aware of symptoms, but not advised to quarantine.
On March 3, the risk of transmission in Sweden was upgraded to moderate and travellers from Italy were urged to undergo virus testing if they had had symptoms in the 14 days after they left Italy. On March 10, the PHA reviewed the alert level and the risk of transmission was upgraded to high for the whole of Sweden.
Most measures to limit transmission were taken in February and March 2020. By February 1, Sweden had classified COVID‐19 as dangerous to the public and to society.
5.2. Healthcare visits and elderly residents
On March 10, the public was advised to avoid unnecessary visits to hospital inpatients or elderly care facilities. Private elderly care providers and nursing facility providers banned visits shortly afterwards, while visits to municipal nursing facilities were stopped from March 30. The PHA also urged people aged 70 years or above to avoid close contact with others from March 16. In early May, a PHA report was published on how to decrease transmission in homes for the elderly and the debate on the risks of social isolation among elderly people began. In August, some people started arguing that younger people needed to shoulder more responsibility so that elderly people did not have to isolate themselves to the same extent.
On March 10, the head of the PHA urged people with COVID‐19 symptoms to avoid working with the elderly or people in risk groups.
5.3. Risk groups
The National Board of Health and Welfare identified risk groups for severe COVID‐19 and these initially included subsets of children. However, these were removed from the list of risk groups after discussions with the Swedish Society of Paediatrics. The final list included people with conditions such as cardiovascular disease—such as high blood pressure—diabetes, respiratory disease and obesity and individuals living in nursing facilities or receiving municipal health care.
5.4. Sick leave
On March 19, the Government made three decisions to limit the spread of COVID‐19. First, the qualifying period for benefits was abolished to promote responsible behaviour. The aim of this was to stop people feeling that they had to work, despite being infected, because they had no money to live on. Second, the Government took on the responsibility, from companies, for sick leave costs for the first two months after an employee became ill as a result of COVID‐19. Third, a sick leave compensation package was launched for workers with suspected or verified COVID‐19.
5.5. Travel restrictions and working from home
The Ministry for Foreign Affairs advised against international travel on March 14. 14 Three days later, the EU issued a recommendation against non‐essential travel for the next 30 days. On March 17, the PHA urged residents to work from home if possible.
Travel within Sweden decreased substantially during spring 2020 and, to some extent, in summer 2020. Daily travel was lowest from mid‐March to mid‐May. 15 Travel restrictions were lifted on June 13, before most residents began their summer holidays, but the recommendations to work from home were still in place on September 1.
5.6. Facemasks and protective equipment
Throughout the pandemic, healthcare personnel have used facemasks when seeing patients with suspected or verified COVID‐19. Staff working at elderly care and nursing facilities began using facemasks in April to May, when COVID‐19 fatalities in the elderly care homes became known.
The availability of protective equipment was low during the early pandemic. A report from the National Board of Health and Welfare in mid‐February showed that the healthcare regions estimated that they only had protective equipment for 5000 patient visits and 1400 days of inpatient care. On March 16, the Government ordered the Board to distribute enough protective equipment to cover demand.
On August 12, the Karolinska Institutet in Stockholm recommended facemasks in settings where physical distancing was deemed impossible, such as close patient contact and when students and teachers performed autopsies.
On June 5, the WHO recommended facemasks on public transport, when people were shopping or with a number of other people. However, the Swedish authorities did not recommend facemasks outside health care and elderly care. On August 18, the PHA announced an ongoing investigation into the use of facemasks in public. On September 1, it declared that facemasks may be recommended in certain settings in the future, such as restricted geographical areas with local outbreaks.
5.7. Public gatherings and physical distance
Gatherings of more than 500 people were banned on March 11 and reduced to less than 50 two weeks later. On April 1, the PHA once more emphasised the importance of physical distancing to reduce transmission, which had been the key component of its mitigation strategy since the start of the pandemic. Distances of 1.0, 1.5 or 2.0 m were recommended, depending on the situation.
On March 24, the PHA issued guidance for restaurants, bars and cafés and stated that standing in queues and crowded tables were not allowed. In many restaurants, guests were served at their table and urged to keep at least 1 m away from other parties. A number of restaurants and bars were closed by the municipal authorities for breaching the guidance.
In August, physical distancing and public transport were debated. This was particularly important as children aged 17 plus returned to school that month. Government agencies urged the public transport companies to increase the number of buses and trains to avoid overcrowding and make physical distancing possible. The limit of 50 people applied to sporting events and cultural events throughout summer, but did not apply to businesses and shopping venues. This inconsistent approach was criticised by a number of bodies, including football associations and the organisers of cultural activities.
6. SCHOOLS AND KINDERGARTENS
6.1. Schools for children up to 16
On March 19, the Swedish Parliament formally allowed the Government to close schools for children up to 16 at short notice. The next day, the Government provided a list of critical occupations, so that the key workers that keep Sweden functioning could be offered extra childcare if schools, pre‐schools and kindergartens closed.
An early systematic review suggested that children rarely developed severe COVID‐19. 16 This may have influenced the Government to keep schools for children up to 16 open.
Parents still had the same duty to send their children to schools if they were open. In the early phase of the pandemic, a small proportion of parents kept their children home from school, probably because they were worried that the child would become seriously ill or that they would pick up the virus at school and transmit it to other family members. On May 6, Swedish television reported that school absences had mostly occurred in families with immigrant backgrounds and a number of reasons have been suggested for this. These included fears that COVID‐19 affected ethnic minorities more severely than Swedish‐born residents and that immigrant households were more likely to contain a greater number of generations living together. It has also been suggested that ethnic minorities were more likely to be influenced by news reports from other countries, where general lockdowns and school closures were common. Media reports also suggested that school absences were primarily an issue until the Easter vacation in mid‐April 2020 and that most of the children who had been absent returned to school after those holidays. On May 21, a scientific paper suggested that children were unlikely to drive the pandemic. 17
6.2. Schools for children aged 17 plus
On March 17, schools for children aged 17 plus were closed and online teaching was the norm until the students returned to school. However, due to the summer holidays, many of these schools only opened again in mid‐August. Some cities restricted full‐time classroom teaching to secondary students aged 17‐19, even in August, with older students receiving part‐time classroom teaching. In other cities, all students received full‐time classroom teaching as soon as they returned to school.
6.3. Colleges and universities
Colleges and universities closed on March 17 and initiated distance learning, but re‐introduced some classroom teaching in August 2020.
7. HEALTH CARE
7.1. Primary care
In February and March 2020, most authorities focused on COVID‐19 in relation to hospitals. On March 26, the National Board of Health and Welfare issued national guidelines for palliative care drugs to relieve end‐of‐life symptoms. However, primary care recommendations for COVID‐19 were not issued until April 7. Early difficulties included how to manage large numbers of elderly people with COVID‐19 in their homes and how to establish well‐functioning collaboration between primary care, hospital care and ambulance and mobile health care. There was a lack of virus testing and COVID‐19 information adapted for primary care. Information on how to treat the elderly, and how to meet the need for oxygen in elderly care homes and nursing facilities that were often served by family doctors, was also lacking. Many doctors raised the alarm that there was a lack of palliative drugs and equipment to administer them. A lack of equipment also meant that virus tests could not be carried out on primary care patients at health centres. Primary care organisations have also had insufficient personnel, protective equipment and oxygen supplies. Due to the lack of national and local guidelines for primary care, family doctors tried to solve shortages themselves, by using private contacts from other countries and relying on guidelines from other countries. Some family doctors also reviewed nursing facilities and talked to the families of elderly residents to prepare them mentally for the pandemic.
Family doctors also started to use phone or online consultations for patients, especially those without airway symptoms, to reduce the risk of transmission and the need for personal protective equipment.
Separate patient areas were established for patients with respiratory symptoms, including tents. Staff were informed about how to use protective equipment. Drop‐in consultations were cancelled, and regular non–COVID‐19 visits were postponed. In some cities, primary care centres were merged to strengthen staffing and provide back‐up capacity if healthcare staff got COVID‐19. Some family doctors who were in risk groups were allowed to work from home. Over time, primary care played an important role in managing less severe COVID‐19 cases and handling virus testing.
7.2. Hospital care, including intensive care
Hospital care was the focus of COVID‐19 treatment in Sweden during the study period. On March 23, the national need for healthcare beds was estimated and all Swedish hospitals were mobilised. This was a few days after the Swedish military started setting up the first field hospital.
The number of COVID‐19 beds rose dramatically around March 20 and peaked in late April to early May, when almost 1800 beds, including 500 ICU beds, contained COVID‐19 patients. This meant that one in 5700 Swedish residents were receiving COVID‐19 care at one point. The need for COVID‐19 hospital beds decreased quickly in mid‐July to around 250 beds and then to 150 beds, including ICU beds, on September 1. April 2020 was the deadliest month in Sweden since 1993.
The Stockholm region was particularly affected, and about 950 beds were occupied by COVID‐19 patients at the peak of the pandemic at the beginning of May. These included just over 300 ICU beds. As an emergency measure, the Government ordered the National Board of Health and Welfare to coordinate the need for ICU beds at a national level. The number of ICU beds across Sweden increased dramatically from 500 to 600 before the pandemic to over 1000 beds at the peak of the pandemic.
Gradually, the pressure on ICUs decreased and there was a shift towards post–COVID‐19 rehabilitation and how to manage the summer vacation period and postponed routine health care. On June 11, the Government ordered the National Board of Health and Welfare to coordinate national healthcare needs for the summer.
Scheduled health care that was postponed included breast cancer screening and elective surgery. Surgery was limited by a lack of peri‐operative drugs and anaesthesiologists, who were working in ICUs with patients who needed mechanical ventilation. Other routine health care was postponed, and national guidelines were published by the National Board of Health and Welfare on April 20 to tackle this issue.
Swedish hospitals converted selected departments to COVID‐19 wards, led by infectious disease specialists or internal medicine specialists. They worked with junior physicians, who were felt to face a lower risk of COVID‐19 than older physicians, as well as nurses and other healthcare personnel from all specialties. These included surgeons, as elective surgery was cancelled. The COVID‐19 wards often had their own on‐call services. Transferring healthcare personnel from their usual departments, and replacing these with other personnel, put increased pressure on all staff. Staff holidays and research leave were cancelled and vacations shortened or postponed. In some healthcare regions, personnel were banned from leaving the county to ensure that hospitals could be staffed.
Emergency departments were re‐organised to separate patients with, and without, suspected COVID‐19 to reduce virus transmission. During summer 2020, when COVID‐19 decreased and protective equipment increased, COVID‐19 patients were more likely to be cared for in non–COVID‐19 departments, but with the relevant virus hygiene precautions.
In the Stockholm region, a special crisis contract between employers and healthcare staff was activated during the pandemic. Staff were paid more, but had to work 48 hours instead of their normal 40.
7.3. Pharmacies and medication
On April 1, the Government banned prescriptions that exceeded three months’ supply. During spring 2020, several ICUs were short of the routine anaesthetics used to sedate patients on invasive mechanical ventilation. The distribution of medications was beyond the scope of this review.
8. TESTING
On January 17, polymerase chain reaction (PCR) testing for the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) that causes COVID‐19 was set up in Sweden. All university hospitals had this testing in place by February 28 and most regional laboratories by the end of March. The Government requested increased virus testing on March 4 and April 17.
Testing initially focused on hospital patients with severe COVID‐19 symptoms. Sweden had the same lack of testing equipment as many other countries at the start of the country's outbreak. At first, healthcare personnel with symptoms were simply urged to stay at home, but staff testing became available in some parts of Sweden in late March. This did not include personnel working in elderly care homes. Lack of testing meant that the Swedish COVID‐19 statistics were probably greatly underestimated during the early months of the pandemic.
While the regions and county councils accepted their responsibility for testing sick patients and healthcare staff, it was not initially clear who was responsible for testing members of the public with mild symptoms However, a COVID‐19 testing agreement was put in place in early June, which enabled individuals to book tests through different web‐based solutions. This started on June 15 in Stockholm. Self‐testing using mouth and nostril swabs and saliva was also introduced.
During July 2020, antibody tests were made available primarily not only for healthcare personnel and personnel in community health and nursing services, 18 but also for the public in many parts of the country. People with a positive antibody test were then allowed to visit elderly people or risk groups. The lack of mass testing during this period was mostly due to the lack of equipment. Several countries banned exports of critical testing equipment and this had an impact on Sweden, as it does not produce much in the way of testing and sampling equipment. Some testing equipment failed to meet the quality requirements and not just at the start of the pandemic. In August 2020, it was discovered that 3700 virus tests had probably reported false‐positive results, due to the suboptimal quality of the reagents that were used.
9. THE CORONA COMMISSION
On May 7, the Government suggested forming a Corona Commission and it was established on July 1. The Commission will evaluate actions related to COVID‐19 by the Government, Government agencies, regions and municipalities 19 and compare the Swedish strategy to that of other countries. An initial report is anticipated in late November 2020, with a final report in February 2022.
10. INFORMATION CAMPAIGNS
10.1. Health care
In March, the National Board of Health and Welfare was ordered to inform healthcare personnel and staff at social services and nursing facilities about COVID‐19. One week later, the Karolinska Institutet launched an e‐learning campaign. 20
10.2. The public
A large proportion of the early cases of severe COVID‐19 affected ethnic minorities. This underlined the need for information in languages other than Swedish and English, and 17 new languages were added to the PHA web page on COVID‐19 in early September.
Between March and August 2020, the PHA and other Government authorities held press conferences every weekday and these were broadcast on television and on the Internet.
11. FUTURE STRATEGY
When this paper was written in early September 2020, the Swedish Government had asked several Government agencies to suggest measures and actions for the future COVID‐19 strategy. The PHA has modelled three scenarios for autumn, winter and spring 2020‐2021, based on different assumptions. To a large extent, future strategies depend on how well the Swedish public adheres to current recommendations and physical distancing.
Sweden also needs to address the healthcare needs that have accumulated during the first eight months of the pandemic. During autumn 2020, the country needs to tackle the elective and routine healthcare needs delayed by the pandemic.
12. DISCUSSION
During the first eight months of the COVID‐19 pandemic, the Swedish strategy mainly focused on voluntary measures, with no general lockdown. When one evaluates the effect of Sweden's approach, it is important to take into account that COVID‐19 was not uniformly spread in Sweden. The Stockholm urban area has had a major impact on all national COVID‐19 parametrics, due to its size, and the patterns were different in other regions that adopted the same national strategies. For example, the per capita mortality rate in Sweden's third largest city, Malmö, which lies in the south of the country, was lower in May 2020 than in the neighbouring Danish capital of Copenhagen, which is approximately 40 km away. 1 However, it should also be noted that large differences were also seen within the Stockholm region, with the highest risk of COVID‐19 in the Rinkeby‐Kista area, where many ethnic minorities live. This is important because one in five Swedish residents were born outside the country. To tackle the high mortality rates in these groups, Government agencies have created information in various languages and interacted with community leaders. But the high death rates were probably multi‐factorial and are unlikely to be explained by just a lack of information.
During the pandemic period studied, the ICD‐10 codes U07.1 and U07.2 were used to register patients with COVID‐19. Reporting COVID‐19 cases to the PHA was mandatory. During the early phase of the pandemic, the presence of these codes was likely to indicate severe disease, as testing capacity was limited to hospital admissions. This has implications for epidemiological research, as it makes comparisons with later COVID‐19 patients with less severe symptoms difficult. Patients diagnosed in the early stages of the pandemic may have had a poorer prognosis, and higher mortality than patients diagnosed later, especially from June when the public could order tests themselves. We are unaware of any validation for the use of those codes in epidemiological research, but U07.1 is likely to have a higher specificity than U07.2, as the latter is not verified by laboratory tests. Since testing recommendations played an important role in diagnosing the virus, one possibility for future epidemiological COVID‐19 research is to focus on severe COVID‐19 of high clinical importance. Three possible definitions for research purposes are suggested in Table 1. A wider definition of ‘any COVID‐19’ may include U07.1 + U07.2 in any Swedish clinical register and in the PHA COVID‐19 database.
Table 1.
Suggested research definitions for COVID‐19 when used as an outcome measure
| Definitions | Source | |
|---|---|---|
| COVID‐19 hospital admission | Inpatient hospital admission (event date) with a primary, laboratory‐verified inpatient diagnosis of ICD‐10 code U07.1 | Patient Register (inpatient data) |
| COVID‐19 death a |
Underlying cause of death was ICD‐10 code U07.1 or death from any cause up to 30 d after inpatient hospital admission (event date), as specified above (U07.1 is primary inpatient diagnosis). |
Cause of Death Register and Patient Register (inpatient data) |
| COVID‐19 intensive care a | ICU admission (event date), with a primary discharge diagnosis of ICD‐10 code U07.1 recorded in Swedish Intensive Care Register. | Swedish Intensive Care register |
Death and ICU admission may be combined into one composite outcome: critical illness/death from COVID‐19.
Sweden's strategy was different to many other countries and has been both criticised and praised. By September 1, 0.06% of the Swedish population had died with a COVID‐19 diagnosis. It is important to note that countries use different mortality measures, and this may explain some of the differences in mortality statistics. In Sweden, deaths occurring outside hospitals were counted and the data included those where COVID‐19 was not the main cause of death. In fact, one small regional study of COVID‐19 deaths outside hospitals up to July 31 suggested that COVID‐19 was the main cause of death in 15% of cases, contributed to death in 70% and was an incidental finding in 15%. 21 This study also suggested that COVID‐19 was the main cause of death for 72% of ICU deaths and for 60% of deaths in ordinary wards among COVID‐19 positive patients who died. It should be noted that the PHA and the National Board for Health and Welfare, which have been the two main Government agencies involved, use slightly different reporting systems for COVID‐19 mortality. The PHA reports deaths within 30 days of a laboratory‐verified diagnosis, but the Board also includes deaths in patients with suspected COVID‐19.
Most Swedish health‐related measures were voluntary up to September 1, but they seem to have been followed by the public. This may partly be due to the high public trust in the Swedish Government and Government health agencies, which was the third highest in the 28 EU countries between 2013 and 2019, at 55%. 22 A Swedish opinion poll in May 2020 reported that 80% of respondents had a moderate or high trust in both Swedish health care and the PHA. 10
However, while trust is important, the Swedish Constitution may also have had an impact on the Swedish COVID‐19 strategy. The Constitution is characterised by decentralised power sharing, the strong role of both the municipalities and Government agencies and limited opportunities for Government ministers to intervene in the day‐to‐day activities of Government agencies. This precluded the kind of ‘strong and fast decisions’ taken by politicians in some other countries. 22
Both the PHA and the Government have been criticised for their handling of the pandemic. Initial criticism focused on the PHA not recommending quarantine for Swedish travellers returning from Northern Italy in late February.
Later criticism focused on the lack of interventions and 22 researchers formed the Vetenskapsforum opinion group, which has since welcomed even more members. The group published a number of articles criticising the strategies of the various Government agencies 23 and has suggested alternative ways to handle the pandemic. In their debate, article on April 14, in the Swedish daily newspaper Dagens Nyheter, the group suggested that schools and restaurants should be closed and that personnel working with the elderly should have appropriate protective equipment. They also suggested that mass testing of all healthcare personnel should begin and that such personnel should also be offered antibody testing to see whether they had already had COVID‐19. The group also said that whole families should be quarantined if one family member was sick or tested positive for the virus. Furthermore, they criticised the civil servants working with COVID‐19, saying that they had ‘so far have shown no talent’, and suggested that politicians take the lead, rather than the PHA.
Although economic measures were not the focus of this review, the Swedish Government has launched massive financial aid packages to support individuals and companies. Despite this, unemployment has risen and gross domestic product has decreased. This will probably have a major effect on the health of Swedish people in terms of poorer psychiatric health and increased risks of suicide and violence. It could also reduce future healthcare funding due to the need for austerity measures.
Sweden kept schools open for children up to 16. Closing schools has a negative impact on children, and real‐world evidence suggested that children have rarely become very sick. 16 Older children were back at school by the end of the study period.
Mask wearing was not recommended outside hospitals, except for personnel in elderly homes or those caring for risk groups. This contrasted with the WHO recommendations, which were primarily based on a meta‐analysis in the Lancet. 24 However, the limitations of that meta‐analysis included the lack of randomised clinical trials. Only three of the 29 studies examined the protective effect of facemasks outside health care, and none of these three studies dealt with COVID‐19. 24 A funnel plot in that study suggested publication bias, with an Egger test score of P = .001. This indicated that small studies that showed a protective effect from masks were more likely to be published than small negative studies. In August 2020, the PHA announced an internal investigation on facemask use outside health care. The Karolinska Institutet had already recommended facemask use on its campus in certain situations, but none of the other Swedish universities had followed their lead by September 1.
The timeline of this study shows that a large number of decisions affecting Sweden were taken, especially in March and April. Decisions after that have been less invasive and have often modified or reversed earlier decisions. Sweden did not apply a general lockdown. It focused on evidence‐based decisions, and experts played a major role in the decision‐making process. The PHA aimed to make recommendations that would be tolerated by the public for a prolonged period of time, so that society could keep operating.
Excess mortality rose by 11% between March and August 2020, with elderly and ethnic minorities particularly affected. The mortality per capita was higher in Sweden than in neighbouring countries, but lower than in several other European countries that had applied a general lockdown.
13. CONCLUSION
This review covers the first eight months since COVID‐19 was first observed in early 2020. It may therefore be premature to evaluate how successful or unsuccessful Sweden's COVID‐19 strategy has been from a long‐term perspective. On July 1, the new Corona Commission began to evaluate the Swedish COVID‐19 strategy, which focused on mitigation rather than suppressing the disease, kept many schools open and placed the emphasis on protecting the elderly and risk groups.
As cases and deaths continue to rise globally, with a second surge in Europe, we must continue to study the evidence and make sure that our future actions are in the best interest of Swedish society. History will tell us if Sweden's approach was right.
CONFLICT OF INTEREST
None.
Appendix 1.
English and Swedish names of main actors
Civil Contingencies Agency (Myndigheten för samhällsskydd och beredskap)
County Administrative Boards (Länsstyrelser).
Medical Product Agency (Läkemedelsverket)
Ministry for Foreign Affairs (Utrikesdepartementet)
National Agency for Education (Skolverket)
National Board of Health and Welfare (Socialstyrelsen)
Public Health Agency (Folkhälsomyndigheten)
Schools Inspectorate (Skolinspektionen)
Ludvigsson JF. The first eight months of Sweden’s COVID‐19 strategy and the key actions and actors that were involved. Acta Paediatr. 2020;109:2459–2471. 10.1111/apa.15582
REFERENCES
- 1. Kavaliunas A, Ocaya P, Mumper J, et al. Swedish policy analysis for Covid‐19. Health Policy Technol. 2020. Epub 2020/09/10 10.1016/j.hlpt.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Riphagen S, Gomez X, Gonzalez‐Martinez C, et al. Hyperinflammatory shock in children during COVID‐19 pandemic. Lancet. 2020;395:1607‐1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Whittaker E, Bamford A, Kenny J, et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS‐CoV‐2. JAMA. 2020;324:259‐269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Emilsson L, Lindahl B, Koster M, et al. Review of 103 Swedish Healthcare Quality Registries. J Intern Med. 2015;277(1):94‐136. [DOI] [PubMed] [Google Scholar]
- 5. Wettergren B, Blennow M, Hjern A, et al. Child Health Systems in Sweden. J Pediatr. 2016;177S:S187‐S202. [DOI] [PubMed] [Google Scholar]
- 6. Anell A. The public‐private pendulum–patient choice and equity in Sweden. N Engl J Med. 2015;372(1):1‐4. [DOI] [PubMed] [Google Scholar]
- 7. Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11(1):450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jonung L, Nergelius J.Grundlagen sätter ramarna för Sveriges coronastrategi (English: The Swedish constitution sets the limits for Sweden’s corona strategy). Dagens Nyheter. 2020. https://www.dn.se/debatt/grundlagen‐satter‐ramarna‐for‐sveriges‐coronastrategi/. Accessed August 31, 2020
- 9. Myndigheten‐för‐Samhällsskydd‐och‐Beredskap . Nästan hela befolkningen har ändrat sitt beteende med anledning av coronapandemin (almost everyone has changed their behaviour due to the corona pandemic). 2020. https://www.msb.se/sv/aktuellt/nyheter/2020/april/nastan‐hela‐befolkningen‐har‐andrat‐sitt‐beteende‐med‐anledning‐av‐coronapandemin/.. Accessed September 30, 2020
- 10. Myndigheten‐för‐Samhällsskydd‐och‐Beredskap . Svenska folket håller fysiskt avstånd (The Swedish people observe physical distancing). 2020. https://www.msb.se/sv/aktuellt/nyheter/2020/maj/svenska‐folket‐haller‐fysiskt‐avstand/. Accessed September 30, 2020
- 11. Swedish‐Government . Strategy in response to the COVID‐19 pandemic. 2020. https://www.government.se/articles/2020/04/strategy‐in‐response‐to‐the‐covid‐19‐pandemic/. Accessed September 1, 2020.
- 12. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019‐nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225):689‐697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Regeringskansliet . UD avråder. https://www.regeringen.se/uds‐reseinformation/ud‐avrader/. Accessed September 1, 2020
- 15. Telia‐crowd‐insights. Telia COVID‐19 mobilitetsanalys: Svenskarnas resande. 2020. https://www.telia.se/privat/aktuellt/hemma‐i‐folknatet/covid‐19‐mobilitetsanalys. Accessed September 1, 2020
- 16. Ludvigsson JF. Systematic review of COVID‐19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109:1088‐1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ludvigsson JF. Children are unlikely to be the main drivers of the COVID‐19 pandemic ‐ a systematic review. Acta Paediatr. 2020;109:1525‐1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vårdpersonal ska prioriteras vid antikroppstest (Healthcare personnel prioritized for antibody testing). Läkartidningen. 2020. https://lakartidningen.se/aktuellt/nyheter/2020/07/vardpersonal‐ska‐prioriteras‐vid‐antikroppstest/. Accessed September 15, 2020 [Google Scholar]
- 19. Swedish‐Government . Kommittédirektiv 2020:74: Utvärdering av åtgärderna för att hantera utbrottet av det virus som orsakar sjukdomen covid‐19. 2020. https://www.regeringen.se/49f46d/contentassets/593c32df14114d9c81eeba9c96e26e41/dir2020_74.pdf. Accessed September 30, 2020
- 20. Karolinska‐Institutet . E‐utbildningar om covid‐19. 2020. https://utbildning.ki.se/e‐utbildningar‐om‐covid‐19. Accessed September 1, 2020
- 21. Covid‐19 oftast inte ensam dödsorsak bland äldre . Lakartidningen 2020. https://lakartidningen.se/aktuellt/nyheter/2020/08/covid‐19‐oftast‐inte‐ensam‐orsak‐vid‐dodsfall‐bland‐aldre/ Accessed September 1, 2020 [Google Scholar]
- 22. Jonung L.Sweden’s constitution decides its exceptional Covid‐19 policy. 2020. https://voxeu.org/article/sweden‐s‐constitution‐decides‐its‐exceptional‐covid‐19‐policy. Accessed September 1, 2020.
- 23. DN‐Debatt . Folkhälsomyndigheten har misslyckats ‐ nu måste politikerna gripa in. Dagens Nyheter, 2020. April 4, 2020.
- 24. Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person‐to‐person transmission of SARS‐CoV‐2 and COVID‐19: a systematic review and meta‐analysis. Lancet. 2020;395(10242):1973‐1987. [DOI] [PMC free article] [PubMed] [Google Scholar]


