Excessive alcohol use is a leading cause of preventable death in the United States (1) and costs associated with it, such as those from losses in workplace productivity, health care expenditures, and criminal justice, were $249 billion in 2010 (2). CDC used the Alcohol-Related Disease Impact (ARDI) application* to estimate national and state average annual alcohol-attributable deaths and years of potential life lost (YPLL) during 2011–2015, including deaths from one’s own excessive drinking (e.g., liver disease) and from others’ drinking (e.g., passengers killed in alcohol-related motor vehicle crashes). This study found an average of 95,158 alcohol-attributable deaths (261 deaths per day) and 2.8 million YPLL (29 years of life lost per death, on average) in the United States each year. Of all alcohol-attributable deaths, 51,078 (53.7%) were caused by chronic conditions, and 52,921 (55.6%) involved adults aged 35–64 years. Age-adjusted alcohol-attributable deaths per 100,000 population ranged from 20.8 in New York to 53.1 in New Mexico. YPLL per 100,000 population ranged from 631.9 in New York to 1,683.5 in New Mexico. Implementation of effective strategies for preventing excessive drinking, including those recommended by the Community Preventive Services Task Force (e.g., increasing alcohol taxes and regulating the number and concentration of alcohol outlets), could reduce alcohol-attributable deaths and YPLL.†
CDC has updated the ARDI application, including the causes of alcohol-attributable death, International Classification of Diseases, Tenth Revision codes,§ and alcohol-attributable fractions.¶ CDC used ARDI to estimate the average number of annual national and state alcohol-attributable deaths and YPLL caused by excessive drinking (i.e., deaths from conditions that are 100% alcohol-attributable, acute conditions that involved binge drinking, and chronic conditions that involved medium or high average daily alcohol consumption). ARDI estimates alcohol-attributable deaths by multiplying the total number of deaths (based on vital statistics) with an underlying cause corresponding to any of the 58 alcohol-related conditions in the ARDI application by its alcohol-attributable fraction. Some conditions (e.g., alcoholic liver cirrhosis) are wholly (100%) attributable to alcohol (alcohol-attributable fraction = 1.0), whereas others are partially attributable (alcohol-attributable fraction <1.0) to alcohol (e.g., breast cancer and hypertension). Deaths are assessed by age group and sex and averaged over a 5-year period. The alcohol-attributable fractions for chronic conditions are generally calculated using relative risks from published meta-analyses and the prevalence of low, medium, and high average daily alcohol consumption among U.S. adults, based on data from the Behavioral Risk Factor Surveillance System.** The prevalence estimates are adjusted to account for underreporting of alcohol use during binge drinking episodes (3). Alcohol-attributable fractions for acute causes (e.g., injuries) are generally based on studies that measured the proportion of decedents who had a blood alcohol concentration ≥0.10 g/dL (4). Alcohol-attributable fractions for motor vehicle crash deaths are based on the proportion of crash deaths that involved a blood alcohol concentration ≥0.08 g/dL.†† For 100% alcohol-attributable conditions, deaths are summed without adjustment.§§ YPLL, a commonly used measure of premature death, are calculated by multiplying the age-specific and sex-specific alcohol-attributable deaths by the corresponding reduction in years of life potentially remaining for decedents relative to average life expectancies.¶¶ Chronic causes of death are calculated for decedents aged ≥20 years, and acute causes are generally calculated for decedents aged ≥15 years. Deaths involving children that were caused by someone else’s drinking (e.g., deaths caused by a pregnant mother’s drinking and passengers killed in alcohol-related motor vehicle crashes) are also included.
CDC used the data available in ARDI to estimate the average annual national and state alcohol-attributable deaths and YPLL associated with excessive drinking and national estimates of alcohol-attributable deaths and YPLL by cause of death, sex, and age group. National and state alcohol-attributable deaths and YPLL per 100,000 population were calculated by dividing the average annual alcohol-attributable death and YPLL estimates, respectively, by average annual population estimates from the U.S. Census for 2011–2015, and then multiplying by 100,000. The alcohol-attributable death rates were then age-adjusted to the 2000 U.S. population.*** The number of YPLL per alcohol-attributable death was calculated by dividing total YPLL by total alcohol-attributable deaths in the United States and in states.
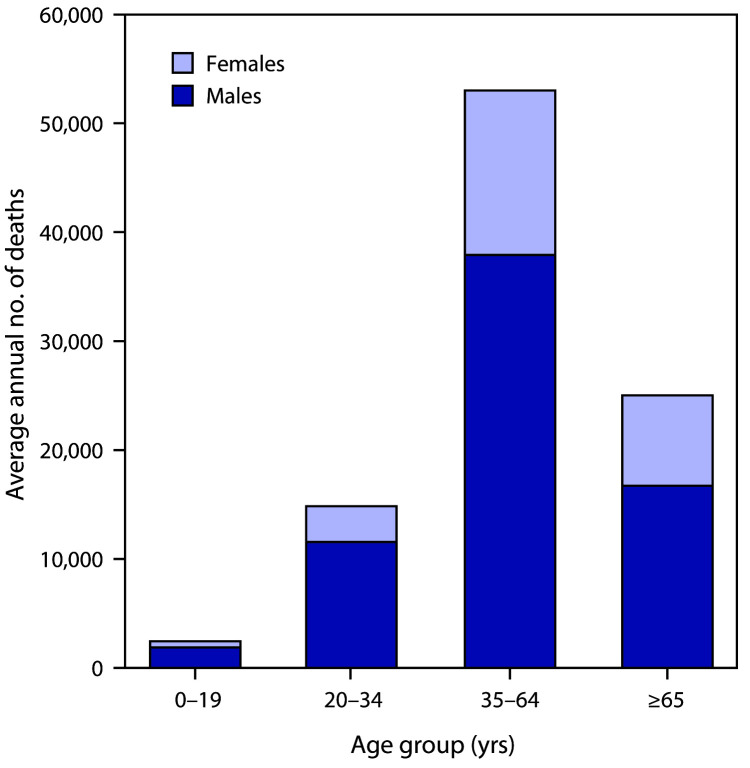
During 2011–2015 in the United States, an average of 95,158 alcohol-attributable deaths occurred, and 2.8 million years of potential life were lost annually (29.0 YPLL per alcohol-attributable death) (Table 1) (Table 2). Among the 95,158 deaths, 51,078 (53.7%) were caused by chronic conditions and 44,080 (46.3%) by acute conditions. Of the 2.8 million YPLL, 1.1 million (40.0%) were because of chronic conditions, and 1.7 million (60.0%) were because of acute conditions. Overall, 67,943 (71.4%) alcohol-attributable deaths and 2.0 million (71.0%) YPLL involved males. Among all alcohol-attributable deaths, 52,921 (55.6%) involved adults aged 35–64 years, 24,972 (26.2%) involved adults aged ≥65, and 14,819 (15.6%) involved young adults aged 20–34 years (Figure).
TABLE 1. Average annual number of deaths and years of potential life lost attributable to excessive alcohol use,* by condition and sex — United States, 2011–2015.
| Cause | Alcohol-attributable deaths |
Years of
potential life lost |
||||
|---|---|---|---|---|---|---|
| Total† | Males no. (%) | Females no. (%) | Total† | Males no. (%) | Females no. (%) | |
|
Total†
|
95,158
|
67,943 (71.4)
|
27,215 (28.6)
|
2,763,055
|
1,962,436 (71.0)
|
800,619 (29.0)
|
|
Chronic
causes
|
51,078 |
35,583 (69.7) |
15,495 (30.3) |
1,105,190 |
752,936 (68.1) |
352,253 (31.9) |
| Alcohol abuse |
2,591 |
1,986 (76.6) |
605 (23.4) |
66,839 |
49,129 (73.5) |
17,710 (26.5) |
| Alcohol cardiomyopathy |
510 |
432 (84.7) |
78 (15.3) |
12,235 |
10,136 (82.8) |
2,099 (17.2) |
| Alcohol dependence
syndrome |
4,258 |
3,269 (76.8) |
989 (23.2) |
109,911 |
81,192 (73.9) |
28,719 (26.1) |
| Alcohol polyneuropathy |
3 |
3 (100.0) |
0 (—) |
54 |
54 (100.0) |
0 (—) |
| Alcoholic gastritis |
33 |
26 (78.8) |
7 (21.2) |
890 |
696 (78.2) |
194 (21.8) |
| Alcoholic liver disease |
18,164 |
12,887 (70.9) |
5,277 (29.1) |
467,996 |
313,897 (67.1) |
154,099 (32.9) |
| Alcoholic myopathy |
0 |
0 (—) |
0 (—) |
0 |
0 (—) |
0 (—) |
| Alcoholic psychosis |
703 |
549 (78.1) |
154 (21.9) |
14,129 |
10,799 (76.4) |
3,330 (23.6) |
| Alcohol-induced acute
pancreatitis |
278 |
214 (77.0) |
64 (23.0) |
8,284 |
6,247 (75.4) |
2,037 (24.6) |
| Alcohol-induced chronic
pancreatitis |
52 |
38 (73.1) |
14 (26.9) |
1,507 |
1,046 (69.4) |
461 (30.6) |
| Atrial fibrillation |
329 |
228 (69.3) |
100 (30.4) |
2,943 |
2,084 (70.8) |
860 (29.2) |
| Cancer, breast (females
only) |
584 |
NA |
584 (NA) |
11,203 |
NA |
11,203 (NA) |
| Cancer, colorectal |
996 |
898 (90.2) |
98 (9.8) |
15,540 |
14,016 (90.2) |
1,524 (9.8) |
| Cancer,
esophageal§ |
494 |
430 (87.0) |
64 (13.0) |
8,038 |
7,007 (87.2) |
1,031 (12.8) |
| Cancer, laryngeal |
248 |
233 (94.0) |
15 (6.0) |
4,002 |
3,737 (93.4) |
265 (6.6) |
| Cancer, liver |
1,609 |
1,545 (96.0) |
64 (4.0) |
28,191 |
27,129 (96.2) |
1,061 (3.8) |
| Cancer, oral cavity and
pharyngeal |
909 |
830 (91.3) |
79 (8.7) |
16,034 |
14,715 (91.8) |
1,319 (8.2) |
| Cancer,
pancreatic¶ |
186 |
151 (81.2) |
35 (18.8) |
2,827 |
2,301 (81.4) |
526 (18.6) |
| Cancer, prostate (males
only) |
188 |
188 (NA) |
NA |
1,952 |
1,952 (NA) |
NA |
| Cancer,
stomach¶ |
58 |
56 (96.6) |
3 (5.2) |
943 |
897 (95.1) |
46 (4.9) |
| Chronic hepatitis |
2 |
2 (100.0) |
0 (0.0) |
42 |
36 (85.7) |
6 (14.3) |
| Coronary heart disease |
3,537 |
2,971 (84.0) |
567 (16.0) |
46,698 |
40,183 (86.0) |
6,515 (14.0) |
| Degeneration of nervous system
attributable to alcohol |
145 |
118 (81.4) |
27 (18.6) |
2,617 |
2,030 (77.6) |
587 (22.4) |
| Esophageal varices |
112 |
77 (68.8) |
34 (30.4) |
2,414 |
1,711 (70.9) |
703 (29.1) |
| Fetal alcohol syndrome |
4 |
2 (50.0) |
2 (50.0) |
212 |
122 (57.5) |
90 (42.5) |
| Fetus and newborn affected by
maternal use of alcohol |
1 |
1 (100.0) |
0 (0.0) |
76 |
76 (100.0) |
0 (—) |
| Gallbladder disease |
0 |
0 (—) |
0 (—) |
0 |
0 (—) |
0 (—) |
| Gastroesophageal
hemorrhage |
31 |
20 (64.5) |
10 (32.3) |
517 |
359 (69.4) |
157 (30.4) |
| Hypertension |
3,584 |
1,638 (45.7) |
1,946 (54.3) |
50,016 |
26,021 (52.0) |
23,994 (48.0) |
| Infant death, low
birthweight** |
2 |
1 (50.0) |
1 (50.0) |
133 |
69 (51.9) |
65 (48.9) |
| Infant death, preterm
birth** |
44 |
24 (54.5) |
19 (43.2) |
3,410 |
1,845 (54.1) |
1,565 (45.9) |
| Infant death, small for
gestational age** |
0 |
0 (—) |
0 (—) |
13 |
5 (38.5) |
7 (53.8) |
| Liver cirrhosis,
unspecified |
9,801 |
5,696 (58.1) |
4,105 (41.9) |
197,875 |
114,580 (57.9) |
83,295 (42.1) |
| Pancreatitis, acute |
0 |
0 (—) |
0 (—) |
0 |
0 (—) |
0 (—) |
| Pancreatitis, chronic |
15 |
12 (80.0) |
3 (20.0) |
317 |
252 (79.5) |
65 (20.5) |
| Pneumonia†† |
133 |
105 (78.9) |
29 (21.8) |
3,714 |
2,839 (76.4) |
875 (23.6) |
| Portal hypertension |
61 |
34 (55.7) |
26 (42.6) |
1,267 |
729 (57.5) |
538 (42.5) |
| Stroke, hemorrhagic |
938 |
565 (60.2) |
374 (39.9) |
14,497 |
8,856 (61.1) |
5,641 (38.9) |
| Stroke, ischemic |
342 |
243 (71.1) |
100 (29.2) |
3,867 |
2,837 (73.4) |
1,030 (26.6) |
| Unprovoked seizures, epilepsy, or
seizure disorder |
134 |
112 (83.6) |
22 (16.4) |
3,987 |
3,352 (84.1 |
635 (15.9) |
|
Acute
causes
|
44,080 |
32,360 (73.4) |
11,720 (26.6) |
1,657,865 |
1,209,500 (73.0) |
448,365 (27.0) |
| Air-space transport |
75 |
64 (85.3) |
11 (14.7) |
2,268 |
1,867 (82.3) |
401 (17.7) |
| Alcohol poisoning |
2,288 |
1,735 (75.8) |
553 (24.2) |
76,224 |
56,511 (74.1) |
19,713 (25.9) |
| Aspiration |
255 |
141 (55.3) |
114 (44.7) |
4,765 |
2,695 (56.6) |
2,070 (43.4) |
| Child
maltreatment§§ |
148 |
87 (58.8) |
61 (41.2) |
11,000 |
6,294 (57.2) |
4,706 (42.8) |
| Drowning |
1,043 |
820 (78.6) |
223 (21.4) |
35,969 |
28,803 (80.1) |
7,167 (19.9) |
| Fall
injuries¶¶ |
2,015 |
1,427 (70.8) |
588 (29.2) |
53,954 |
38,009 (70.4) |
15,945 (29.6) |
| Fire injuries |
1,066 |
640 (60.0) |
426 (40.0) |
25,550 |
15,145 (59.3) |
10,405 (40.7) |
| Firearm injuries |
129 |
109 (84.5) |
20 (15.5) |
4,947 |
4,124 (83.4) |
823 (16.6) |
| Homicide |
7,334 |
5,899 (80.4) |
1,436 (19.6) |
318,006 |
258,572 (81.3) |
59,434 (18.7) |
| Hypothermia |
296 |
194 (65.5) |
102 (34.5) |
6,199 |
4,354 (70.2) |
1,845 (29.8) |
| Motor-vehicle nontraffic
crashes |
190 |
144 (75.8) |
47 (24.7) |
5,588 |
4,249 (76.0) |
1,339 (24.0) |
| Motor-vehicle traffic
crashes*** |
7,092 |
5,522 (77.9) |
1,570 (22.1) |
323,610 |
245,447 (75.8) |
78,163 (24.2) |
| Occupational and machine
injuries |
126 |
117 (92.9) |
9 (7.1) |
3,294 |
3,060 (92.9) |
234 (7.1) |
| Other road vehicle
crashes |
170 |
137 (80.6) |
33 (19.4) |
5,632 |
4,473 (79.4) |
1,159 (20.6) |
| Poisoning (not alcohol) |
11,839 |
7,524 (63.6) |
4,315 (36.4) |
444,235 |
280,270 (63.1) |
163,965 (36.9) |
| Suicide |
9,899 |
7,711 (77.9) |
2,189 (22.1) |
332,791 |
252,674 (75.9) |
80,117 (24.1) |
| Suicide by and exposure to
alcohol |
38 |
24 (63.2) |
14 (36.8) |
1,267 |
764 (60.3) |
503 (39.7) |
| Water transport | 75 | 65 (86.7) | 9 (12.0) | 2,566 | 2,189 (85.3) | 377 (14.7) |
Abbreviation: NA = not applicable.
* In the Alcohol-Related Disease Impact application (https://www.cdc.gov/ARDI), deaths attributable to excessive alcohol use include deaths from 1) conditions that are 100% alcohol-attributable, 2) deaths caused by acute conditions that involved binge drinking, and 3) deaths caused by chronic conditions that involved medium (>1 to ≤2 drinks of alcohol [women] or >2 to ≤4 drinks [men]) or high (>2 drinks of alcohol [women] or >4 drinks [men]) levels of average daily alcohol consumption.
† Numbers might not sum to totals, and row percentages might not sum to 100% because of rounding.
§ Deaths calculated for the proportion of esophageal cancer deaths caused by squamous cell carcinoma only, based on the Surveillance, Epidemiology, and End Results data in 18 states (SEER18). https://seer.cancer.gov/.
¶ Deaths among those consuming high average daily levels of alcohol only.
** Alcohol consumption prevalence estimates calculated among women aged 18–44 years only.
†† Deaths among persons aged 20–64 years only because of the high number of deaths from pneumonia among persons aged ≥65 years that are not alcohol-related and the lack of relative risks that differ by age.
§§ Deaths among persons aged 0–14 years.
¶¶ Deaths among persons aged 15–69 years only because of the high number of deaths from falls among persons aged ≥70 years that are not alcohol-attributable and the lack of alcohol-attributable fractions that differ by age.
*** Deaths among persons of all ages. A blood alcohol concentration level of ≥0.08 g/dL is used for defining alcohol attribution for this condition.
TABLE 2. Annual average number of deaths and years of potential life lost from excessive alcohol use,* by state — United States, 2011–2015.
| Location | Alcohol-attributable deaths | Age-adjusted alcohol-attributable deaths per 100,000-population | Years of potential life lost | Years of potential life lost per 100,000-population | Years of potential life lost per alcohol-attributable death |
|---|---|---|---|---|---|
|
U.S. total
|
95,158
|
28.0
|
2,763,055
|
873.0
|
29.0
|
| Alabama |
1,504 |
29.2 |
46,347 |
959.4 |
30.8 |
| Alaska |
297 |
40.0† |
9,794 |
1,335.5 |
33.0 |
| Arizona |
2,629 |
37.5 |
76,039 |
1,144.8 |
28.9 |
| Arkansas |
923 |
29.4 |
27,699 |
936.3 |
30.0 |
| California |
11,026 |
27.5 |
308,831 |
803.8 |
28.0 |
| Colorado |
1,821 |
32.7 |
54,564 |
1,033.6 |
30.0 |
| Connecticut |
913 |
23.2 |
26,366 |
733.8 |
28.9 |
| Delaware |
278 |
27.6† |
8,445 |
911.5 |
30.4 |
| District of Columbia |
219 |
33.0† |
6,440 |
994.6 |
29.4 |
| Florida |
6,903 |
30.4 |
188,713 |
960.6 |
27.3 |
| Georgia |
2,637 |
25.6 |
79,017 |
789.6 |
30.0 |
| Hawaii |
349 |
22.3† |
9,482 |
674.3 |
27.2 |
| Idaho |
493 |
29.5 |
14,099 |
872.2 |
28.6 |
| Illinois |
3,391 |
24.8 |
100,018 |
776.9 |
29.5 |
| Indiana |
1,946 |
28.1 |
58,407 |
889.2 |
30.0 |
| Iowa |
841 |
24.8 |
22,266 |
719.8 |
26.5 |
| Kansas |
764 |
25.2 |
22,725 |
785.5 |
29.7 |
| Kentucky |
1,552 |
33.0 |
46,452 |
1,056.4 |
29.9 |
| Louisiana |
1,591 |
33.0 |
50,180 |
1,084.9 |
31.5 |
| Maine |
427 |
27.2† |
11,375 |
855.8 |
26.6 |
| Maryland |
1,505 |
23.8 |
46,185 |
778.8 |
30.7 |
| Massachusetts |
1,744 |
23.6 |
49,020 |
731.0 |
28.1 |
| Michigan |
3,205 |
29.7 |
92,753 |
936.8 |
28.9 |
| Minnesota |
1,343 |
22.9 |
37,011 |
683.0 |
27.6 |
| Mississippi |
954 |
30.7 |
29,516 |
987.8 |
30.9 |
| Missouri |
1,913 |
29.7 |
58,107 |
961.2 |
30.4 |
| Montana |
416 |
37.6 |
12,289 |
1,211.1 |
29.5 |
| Nebraska |
460 |
23.3 |
12,899 |
690.0 |
28.0 |
| Nevada |
1,051 |
35.1 |
30,229 |
1,080.1 |
28.8 |
| New Hampshire |
421 |
27.5† |
11,389 |
860.1 |
27.1 |
| New Jersey |
2,016 |
20.9 |
59,604 |
669.4 |
29.6 |
| New Mexico |
1,145 |
53.1 |
35,087 |
1,683.5 |
30.6 |
| New York |
4,473 |
20.8 |
124,315 |
631.9 |
27.8 |
| North Carolina |
2,876 |
27.2 |
85,199 |
865.4 |
29.6 |
| North Dakota |
216 |
28.7† |
6,402 |
887.1 |
29.6 |
| Ohio |
3,674 |
29.2 |
106,752 |
922.2 |
29.1 |
| Oklahoma |
1,497 |
37.2 |
44,920 |
1,166.8 |
30.0 |
| Oregon |
1,508 |
33.8 |
39,705 |
1,007.9 |
26.3 |
| Pennsylvania |
3,843 |
27.2 |
111,516 |
872.6 |
29.0 |
| Rhode Island |
339 |
28.8† |
9,346 |
887.0 |
27.6 |
| South Carolina |
1,679 |
32.4 |
50,141 |
1,049.5 |
29.9 |
| South Dakota |
283 |
32.9† |
8,681 |
1,029.5 |
30.7 |
| Tennessee |
2,151 |
30.8 |
64,392 |
990.7 |
29.9 |
| Texas |
7,245 |
27.4 |
219,901 |
828.6 |
30.4 |
| Utah |
686 |
26.2 |
21,937 |
755.6 |
32.0 |
| Vermont |
203 |
27.2† |
5,085 |
811.5 |
25.0 |
| Virginia |
2,011 |
22.7 |
58,540 |
709.0 |
29.1 |
| Washington |
2,214 |
29.1 |
60,508 |
866.2 |
27.3 |
| West Virginia |
738 |
36.1 |
22,087 |
1,193.0 |
29.9 |
| Wisconsin |
1,737 |
27.5 |
48,122 |
838.1 |
27.7 |
| Wyoming | 237 | 38.8† | 7,329 | 1,264.3 | 30.9 |
* In the Alcohol-Related Disease Impact application (https://www.cdc.gov/ARDI), deaths attributable to excessive alcohol use include deaths from 1) conditions that are 100% alcohol-attributable, 2) deaths caused by acute conditions that involved binge drinking, and 3) deaths caused by chronic conditions that involved medium (>1 to ≤2 drinks of alcohol [women] or >2 to ≤4 drinks [men]) or high (>2 drinks of alcohol [women] or >4 drinks [men]) levels of average daily alcohol consumption.
† The estimate might be unreliable because of suppressed estimates of the number of alcohol-attributable deaths in two or more age groups, and estimates might not account for the total number of alcohol-attributable deaths in the state.
FIGURE.
Average annual number of deaths attributable to excessive alcohol use,* by sex and age group — United States, 2011–2015
* In the Alcohol-Related Disease Impact application (https://www.cdc.gov/ARDI), deaths attributable to excessive alcohol use include deaths from 1) conditions that are 100% alcohol-attributable, 2) deaths caused by acute conditions that involved binge drinking, and 3) deaths caused by chronic conditions that involved medium (>1 to ≤2 drinks of alcohol [women] or >2 to ≤4 drinks [men]) or high (>2 drinks of alcohol [women] or >4 drinks [men]) levels of average daily alcohol consumption.
Alcoholic liver disease was the leading chronic cause of alcohol-attributable deaths overall (18,164) and among males (12,887) and females (5,277) (Table 1). Poisonings that involved another substance in addition to alcohol (e.g., drug overdoses) were the leading acute cause of alcohol-attributable deaths overall (11,839) and among females (4,315); suicide associated with excessive alcohol use was the leading acute cause of alcohol-attributable deaths among males (7,711). Conditions wholly attributable to alcohol accounted for 29,068 (30.5%) of all alcohol-attributable deaths and 762,241 (27.6%) of all YPLL.
The national average annual age-adjusted alcohol-attributable death rate was 28.0 per 100,000, and the YPLL per 100,000 was 873.0 (Table 2). The average annual number of alcohol-attributable deaths and YPLL varied across states, ranging from 203 alcohol-attributable deaths in Vermont to 11,026 in California, and from 5,085 YPLL in Vermont to 308,831 in California. Age-adjusted alcohol-attributable death rates among the 40 states with reliable estimates (excluding those with suppressed data where estimates might not account for all the alcohol-attributable deaths in the state) ranged from 20.8 per 100,000 in New York to 53.1 in New Mexico. YPLL per 100,000 ranged from 631.9 in New York to 1,683.5 in New Mexico.
Discussion
Excessive alcohol use was responsible for approximately 95,000 deaths and 2.8 million YPLL annually in the United States during 2011–2015. This means that an average of 261 Americans die from excessive drinking every day, shortening their lives by an average of 29 years. The majority of these alcohol-attributable deaths involved males, and approximately four in five deaths involved adults aged ≥35 years. The number of alcohol-attributable deaths among adults aged ≥65 years was nearly double that among adults aged 20–34 years. Approximately one half of alcohol-attributable deaths were caused by chronic conditions, but acute alcohol-attributable deaths, all of which were caused by binge drinking, accounted for the majority of the YPLL from excessive drinking.
Little progress has been made in preventing deaths caused by excessive drinking; the average annual estimates of alcohol-attributable deaths and YPLL in this report are slightly higher than estimates for 2006–2010, and the age-adjusted alcohol-attributable death rates are similar (5), suggesting that excessive drinking remains a leading preventable cause of death and disability (1). From 2006–2010 (5) to 2011–2015, average annual deaths caused by alcohol dependence increased 14.2%, from 3,728 to 4,258, and deaths caused by alcoholic liver disease increased 23.6%, from 14,695 to 18,164. These findings are consistent with reported increasing trends in alcohol-induced deaths (e.g., deaths from conditions wholly attributable to alcohol) among adults aged ≥25 years,††† including alcoholic liver disease,§§§ as well as with increases in per capita alcohol consumption during the past 2 decades.¶¶¶
Age-adjusted alcohol-attributable death rates varied approximately twofold across states, but deaths caused by excessive drinking were common across the country. The differences in alcohol-attributable death and YPLL rates in states might be partially explained by varying patterns of excessive alcohol use, particularly binge drinking, which is affected by state-level alcohol pricing and availability strategies (6) and differential access to medical care.
The findings in this report are subject to at least five limitations. First, the prevalence of alcohol consumption ascertained through the Behavioral Risk Factor Surveillance System is based on self-reported data, which substantially underestimates alcohol consumption (7). Second, these estimates are conservative, because former drinkers, some of whom might have died from alcohol-related conditions, are not included in the estimates of alcohol-attributable deaths and YPLL for partially alcohol-attributable causes of death. Third, direct alcohol-attributable fraction estimates for some chronic and acute conditions rely on data older than that of 2011–2015 (4) and might not accurately represent the proportion of excessive drinkers among persons who died of some conditions (e.g., drug overdoses) during that period. This emphasizes the importance of more timely information on alcohol involvement and various health conditions. Fourth, several conditions partially related to alcohol (e.g., tuberculosis, human immunodeficiency virus, and acquired immunodeficiency syndrome)**** are not included because published risk estimates were not available. Finally, the alcohol-attributable deaths and YPLL are based on alcohol-related conditions that were listed as the underlying (i.e., primary) cause of death, and not as a multiple cause of death, yielding conservative estimates.
The implementation of effective population-based strategies for preventing excessive drinking, such as those recommended by the Community Preventive Services Task Force (e.g., increasing alcohol taxes and regulating the number and concentration of alcohol outlets), could reduce alcohol-attributable deaths and YPLL. These strategies can complement other population-based prevention strategies that focus on health risk behaviors associated with excessive alcohol use, such as safer prescribing practices to reduce opioid misuse and overdoses (8,9) and alcohol-impaired driving interventions (10).
Summary.
What is already known about this topic?
Excessive drinking is a leading cause of preventable death in the United States and is associated with numerous health and social problems.
What is added by this report?
During 2011–2015, excessive drinking was responsible for an average of 95,158 deaths (261 per day) and 2.8 million years of potential life lost (29 years lost per death, on average) in the United States each year.
What are the implications for public health practice?
Widespread implementation of prevention strategies, including those recommended by the Community Preventive Services Task Force (e.g., increasing alcohol taxes and regulating the number and concentration of places that sell alcohol) could help reduce deaths and years of potential life lost from excessive drinking.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. Timothy Stockwell reports grants and personal fees from Alko, Finland, outside the submitted work. Richard Saitz reports nonfinancial support from Alkermes; personal fees from UpToDate and Massachusetts Medical Society; support and consulting fees from the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and the Patient-Centered Outcomes Research Institute; travel support and consulting fees from the American Medical Association, the American Society of Addiction Medicine, Wolters Kluwer, National Council on Behavioral Healthcare, the International Network on Brief Intervention for Alcohol and other drugs, Systembolaget, Kaiser Permanente, RAND, the Institute for Research and Training in the Addictions, the National Council on Behavioral Healthcare, Charles University (Czech Republic), National Committee on Quality Assurance, and the University of Oregon; and salary support from Burroughs Wellcome Fund. No other potential conflicts of interest were disclosed.
Footnotes
Conditions that that are 100% alcohol-attributable include 13 chronic conditions (alcoholic psychosis, alcohol abuse, alcohol dependence syndrome, alcohol polyneuropathy, degeneration of the nervous system caused by alcohol use, alcoholic myopathy, alcohol cardiomyopathy, alcoholic gastritis, alcoholic liver disease, alcohol-induced acute pancreatitis, alcohol-induced chronic pancreatitis, fetal alcohol syndrome, and fetus and newborn affected by maternal use of alcohol) and two acute conditions (suicide by and exposure to alcohol and alcohol poisoning).
References
- 1.Mokdad AH, Ballestros K, Echko M, et al. ; US Burden of Disease Collaborators. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA 2018;319:1444–72. 10.1001/jama.2018.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD. 2010 national and state costs of excessive alcohol consumption. Am J Prev Med 2015;49:e73–9. 10.1016/j.amepre.2015.05.031 [DOI] [PubMed] [Google Scholar]
- 3.Stahre M, Naimi T, Brewer R, Holt J. Measuring average alcohol consumption: the impact of including binge drinks in quantity-frequency calculations. Addiction 2006;101:1711–8. 10.1111/j.1360-0443.2006.01615.x [DOI] [PubMed] [Google Scholar]
- 4.Smith GS, Branas CC, Miller TR. Fatal nontraffic injuries involving alcohol: a metaanalysis. Ann Emerg Med 1999;33:659–68. [PubMed] [Google Scholar]
- 5.Stahre M, Roeber J, Kanny D, Brewer RD, Zhang X. Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Prev Chronic Dis 2014;11:E109 . 10.5888/pcd11.130293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xuan Z, Blanchette J, Nelson TF, Heeren T, Oussayef N, Naimi TS. The alcohol policy environment and policy subgroups as predictors of binge drinking measures among US adults. Am J Public Health 2015;105:816–22. 10.2105/AJPH.2014.302112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nelson DE, Naimi TS, Brewer RD, Roeber J. US state alcohol sales compared to survey data, 1993-2006. Addiction 2010;105:1589–96. 10.1111/j.1360-0443.2010.03007.x [DOI] [PubMed] [Google Scholar]
- 8.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep 2016;65(No. RR-1):1–49. 10.15585/mmwr.rr6501e1 [DOI] [PubMed] [Google Scholar]
- 9.Esser MB, Guy GP Jr, Zhang K, Brewer RD. Binge drinking and prescription opioid misuse in the U.S., 2012–2014. Am J Prev Med 2019;57:197–208. 10.1016/j.amepre.2019.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Academies of Sciences, Engineering, and Medicine. Getting to zero alcohol-impaired driving fatalities: a comprehensive approach to a persistent problem. Washington, DC: National Academies Press; 2018. [PubMed] [Google Scholar]