Objective:
To examine changes in pulmonary function over a 5-year period in US firefighters.
Methods:
Spirometry values from occupational medical examinations separated by 5 years (2009 to 2016) were examined from 662 career firefighters in Virginia. Predicted values and expected 5-year changes in one-second forced expiratory volume (FEV1), forced vital capacity (FVC), and FEV1/FVC were estimated using reference equations generated from the Third National Health and Nutrition Examination Survey (NHANES III) data. Paired t-tests were used to identify significant changes over time and between the observed and expected changes.
Results:
FEV1 and FVC (percentage of predicted) decreased (P < 0.001) from 100.9 ± 0.6% to 92.3 ± 0.5% and 99.0 ± 0.6% to 91.9 ± 0.5%, respectfully. The observed decreases in FEV1, FVC, and FEV1/FVC were two to four times greater (P < 0.001) than the expected decrease over 5 years.
Conclusion:
Increased efforts are needed to ensure respiratory protection for US firefighters to minimize their risk of pulmonary damage.
Keywords: firefighters, lung health, pulmonary function, spirometry
Firefighters are an important occupational group that are exposed to multiple inhalation hazards and for whom pulmonary function tests are recommended prior to employment and on an annual basis.1 Pulmonary function tests provide objective and quantifiable measures of lung function and are used for multiple reasons, including: to monitor the effects of environmental, occupational or drug exposures; to assess risks of surgery; and to assist in evaluations performed before employment or for insurance reasons.2 In 1974, The New England Journal of Medicine published a paper documenting impaired respiratory and pulmonary function among firefighters.3 The rate of loss in forced vital capacity (FVC) observed in these firefighters over a 1-year period was more than twice the decline expected in the general population. Further, the study demonstrated that the decreases in pulmonary function measures were significantly related to frequency of fire exposure. In the decades following the publication of this article, numerous studies reported on the acute and chronic decrements in one-second forced expiratory volume (FEV1), FVC, FEV1/FVC, and overall pulmonary function following acute and chronic exposure among US firefighters.4–13 Collectively, the decreased pulmonary function identified in these studies encouraged more consistent use of respiratory protection, specifically the use of self-contained breathing apparatus (SCBA) within the fire service.9,14 Currently, the Occupational Safety and Health Administration (29 cfr 1910.134)15 and the National Fire Protection Agency16 provide guidance on the mandatory use of SCBA when operating within the Immediately Dangerous to Life and Health environment (IDLH).
While the use of SCBA during fire suppression operations has increased, there is a pressing need to remain concerned about the respiratory health and respiratory protection of firefighters. Modern fires are producing smoke and byproducts of combustion, including polycyclic aromatic hydrocarbons (PAHs), volatile organic compounds (VOCs), di-(2-ethylhexyl) phthalate (DEHP), and polybrominated diphenyl ethers (PBDEs), that are far more toxic than the contaminates released from fires decades ago.17–23 Furthermore, there is evidence of increased risk of cancer in the fire service24 and respiratory exposure is considered an important route for exposure to carcinogenic chemicals.20,22 Although SCBAs are now nearly ubiquitous across the US fire service, there is evidence that SCBAs are not routinely used during all phases of firefighting.9,25,26 Specific times when firefighters may be exposed to smoke and other hazards include working on the scene of a structure fire before entering the structure (ie, firefighters often do not don the facemask until they enter the structure) or after the fire has been suppressed while they are performing overhaul duties in the structure.
A recent systematic review of longitudinal changes in lung function in firefighters found high variability in the reported rates of decline, and the authors concluded that more evidence is needed on the effects of routine firefighting on lung function.27 Therefore, the purpose of this study was to investigate changes in pulmonary function in a large cohort of career firefighters over a 5-year period using occupational medical records.
METHODS
A cohort of career firefighters (n = 662) from Virginia was examined based on records from occupational medical examinations that were performed between 2009 and 2016. The medical evaluations were conducted by an occupational health clinic that performs annual medical evaluations on a contract basis to a large county-wide fire department. The medical evaluations are consistent with the National Fire Protection Association's 1582 Standard on Comprehensive Occupational Medical Program for Fire Departments and include assessment of pulmonary function via spirometry.28 To examine changes in pulmonary function over time within firefighters, the medical records of firefighters who had two examinations separated by 5 years (4 to 6-year range) were examined.
During the occupational examination, height and weight were recorded using a digital physician's scale and stadiometer. Current smoking status was not reported due to a smoking ban policy initiated prior to baseline in this cohort. Experienced technicians collected spirometry values from a standard spirometer.29,30 The technician had participants complete three to five technically adequate efforts, with efforts automatically graded by the software. The largest acceptable values were recorded for data analysis. Data from the questionnaire and medical examination were entered into a database by the clinic staff and a de-identified dataset was transferred by the occupational clinic to researchers in the First Responder Health and Safety Laboratory at Skidmore College. This protocol was reviewed and deemed to be exempt by the Skidmore College Institutional Review Board.
Age, sex, and race-specific spirometric reference equations generated from a cross-sectional national sample of asymptomatic lifelong nonsmoking adults (NHANES III) were used to calculate predicted values for FEV1 and FVC.31 Baseline age and the time duration between examinations were used to estimate the expected change over time using the same spirometric reference equations from Hankinson et al.31
Paired t-tests were used to identify statistical differences in the observed changes in pulmonary measures over time and differences between the observed and the expected changes over time. McNemar's test of differences were conducted to identify statistical differences in the percentages of firefighters with observed FEV1 and FVC below 80% and 70% of their predicted volume and FEV1/FVC ratios below 70%. The cut-offs for sprirometric measures were based on medical requirements for firefighters, and were not intended to identify individuals with medical conditions. The level of significance for all analyses was considered at P < 0.05 and was two sided for all tests. All analyses were conducted using Stata 15.1 (StataCorp, College Station, TX).
RESULTS
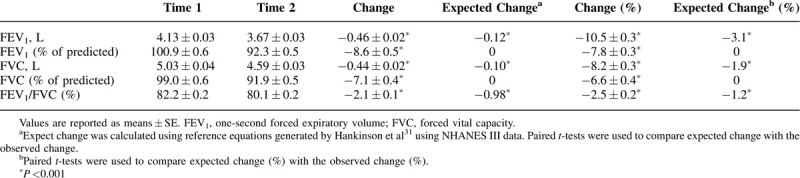
The cohort of firefighters was on average 38.1 ± 7.7 years of age at baseline, predominately male and Caucasian, and had a mean BMI (28.0 ± 3.9 kg/m2) in the overweight category (Table 1). Baseline values for FEV1 and FVC were 100.9 ± 0.6% and 99.0 ± 0.6% of predicted values, respectively. Over the 5-year period, significant decreases in FEV1 (–0.46 ± 0.02 L; P < 0.001), FVC (–0.44 ± 0.02 L; P < 0.001), and FEV1/FVC (–2.1 ± 0.1%; P < 0.001) were found. Observed absolute 5-year changes and percent changes in FEV1, FVC, and FEV1/FVC were significantly greater than expected values (P < 0.001) (Table 2).
TABLE 1.
Baseline Descriptive Statistics of a US Firefighter Cohort (n = 662)
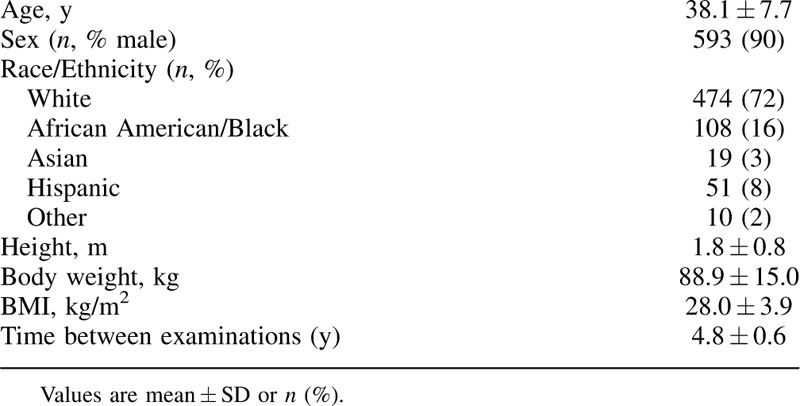
TABLE 2.
Five-Year Changes in Pulmonary Measurements Among a Cohort of US Firefighters
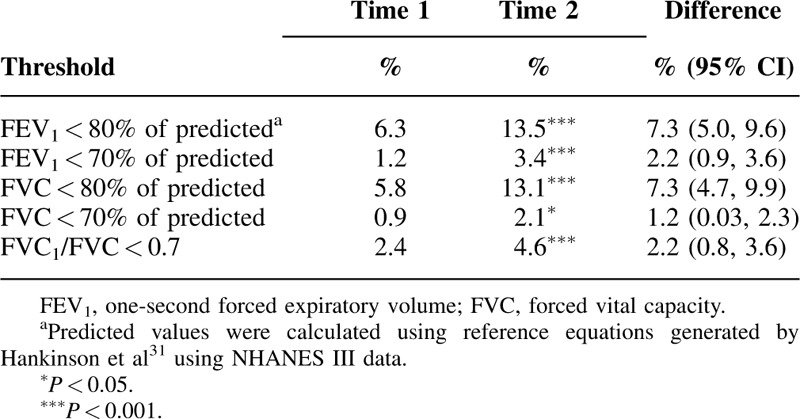
The percentage of firefighters with less than 80% of predicted FEV1 significantly increased (P < 0.001) from 6% to 14%, and the percentage of firefighters with less than 70% of predicted FEV1 increased from 1% to 3% (P < 0.001) (Table 3). The percentage of firefighters with less than 80% of predicted FVC significantly increased (P < 0.001) from 6.3% to 13.5% (P < 0.001) and the percentage with less than 70% of predicted FVC significantly increased (P < 0.001) from 0.9% to 2.1%. The percentage of firefighters with a FEV1/FVC ratio less than 0.7 significantly increased (P < 0.001) from 2.4% to 4.6%.
TABLE 3.
Percentages of Firefighters With Pulmonary Scores Below Thresholds Over a 5-Year Period
DISCUSSION
The primary findings of this study are that pulmonary function in this large cohort of career firefighters significantly decreased over the 5-year period, and the observed decreases were two to four times greater than the estimated decreases that would be expected in the general population over a 5-year period.
There are known changes in the pulmonary system as individuals age, including alterations in the size of the thoracic cavity, limiting lung volumes, and altering the muscles that aid in respiration.10,31 However, the findings from the current study indicate that these age-associated changes were augmented in this cohort of firefighters and are consistent with research conducted on the fire service during the 1970s. A study of 1430 firefighters from the greater Boston area between 1970 and 1972 found significant decreases in spiromentry values3 that are similar to the rate of decline in individuals with chronic obstructive pulmonary disease (∼80 mL/yr).32 Furthermore, the loss of pulmonary function was associated with the frequency of fire exposure, with twice the loss among heavily exposed firefighters as compared with firefighters with light exposure.3 Additional studies have also shown decreases in spirometry values during active duty4–13 as well as during wildland firefighting33 and work at the World Trade Center disaster.10
Heterogeneity and lack of excessive declines in pulmonary function in firefighters and associations with fire fighting duties have also been shown across cohorts.14,27,34,35 Studies observing the Boston Fire Department from the late 1970s to the early 1980s found that firefighters who were not engaged in active firefighting duty also had large reductions in both FEV1 and FVC, suggesting that other factors besides fire and smoke exposure promoted respiratory and pulmonary ailments. Additionally, these studies showed that firefighters who transitioned to less active assignments also had a greater decrement in ventilatory capacity than those who remained in fire-fighting positions.34 Some limitations in these studies, including the crude assessment and definition of exposure, as well as the limited number of subject responses, may explain the divergent findings.34,35 Furthermore, evidence suggests that some of these subjects were in fact retiring prematurely because of respiratory impairment, which could have significantly altered the findings.35
More recently, a study in 2013 that investigated changes in pulmonary function over 5 years in NYC firefighters who were not exposed to the World Trade Center disaster found that the decline in FEV1 among newly hired firefighters was not significantly different from a control group (EMS workers) over a 5-year period.36 Firefighters in the Aldrich et al36 study had a FEV1 (98.8% of predicted) at the time of hire which is similar to the 100.9% of predicted FEV1 that was found in the current study at baseline. However, the current study found an annual rate of decline in FEV1 (92 mL/yr) that was about two times as large as the yearly decline (45 mL/yr) reported by Aldrich et al.36 The current study sample was on average 12 years older than the firefighters in the Aldrich et al study,36 and longitudinal decreases in FEV1 are larger among older adults,37 which might partially explain the difference in FEV1 decline observed between the two cohorts.
In 1981, the NFPA required US firefighters to wear personal protective equipment (PPE) and SCBA.38 Although the use of respiratory protection has become standard in the fire service, certainly in large career fire departments, the systematic use of SCBAs is arguably more important now than when first introduced due to the increasing toxicity of smoke in modern fires.39 Unfortunately, there may be inconsistent and inadequate use of respiratory protection in the fire service. Research from 2001 suggests that SCBAs are used around 50% of the time during structural fires, yet only 6% of the time during all other types of fires.26 Removal of SCBA prior to overhaul can result in exposure to respiratory toxins, asphyxiants, synthetic polymers, and smoke plumes on the foreground, which promote adverse health effects in firefighters.25,39 It is also possible that other factors, such as particulate matter from the diesel exhaust of rescue equipment, could affect spirometry values of firefighters. The use of respiratory protection is important in protecting against lung damage and decreases in pulmonary function, and may partially explain some of the heterogeneity in pulmonary decline across studies.26 A systematic review of longitudinal changes in lung function among firefighters found non-smoking firefighters who routinely wore respiratory protection were more likely to have normal rates of decline in lung function.27 Firefighters who reported “never or rarely” using their respiratory protection equipment during fire knockdown had a higher odds (odds ratio [OR]: 2.20; 95% confidence interval [CI]: 1.02 to 4.74) of accelerated FEV1 decline (greater than 50 mL/yr) than those who “often or frequently” used their respiratory protection equipment.40 The unprotected airway also provides an important exposure risk to carcinogens. Modest associations of firefighter exposure with lung cancer and leukemia mortality have been reported.24 Excess malignant mesothelioma among firefighters has also been shown, suggesting a workplace asbestos hazard for firefighters given that asbestos is the only known causal agent for malignant mesothelioma.41
The results presented demonstrate that most of the firefighters examined had spirometry values that were in the upper range of normal and remained well within the normal range (more than 80% of predicted value) after 5 years, even though significant decreases were observed. However, over the 5-year period, significantly more firefighters had lung function that would have resulted in disqualification of a recruit firefighter, or additional testing and potential medical disqualification for a continuing member of the fire department. The increased percentage of firefighters not meeting clinical thresholds over the 5-year period is an important finding of this study. In addition, a decrease in lung function may be important even among firefighters whose lung function values remain within the normal range. An excessive decrease in lung function is an indication that respiratory protection was not being used as often or stringently as desired. Though not tested directly in this study, it is possible that the greater toxicity of smoke based on current home furnishings and other commercial exposures are creating an occupational exposure where even limited smoke exposure may result in decreased respiratory function. Monitoring changes in pulmonary function provides an opportunity for health care providers to discuss the benefits of respiratory protection, including decreased risk of pulmonary disease and cancer, with firefighters.
There are important limitations to note to provide context for the results found in this study. The findings presented are from one large fire department, a control group of non-firefighters from the same county were not observed, and fire exposure and use of respiratory protection was not recorded; therefore, the changes reported may not reflect the changes that occurred among firefighters at a national level. In addition, several studies have shown discrepancies between estimates of annual decline in pulmonary function between cross-sectional and longitudinal studies.42 Two large cohort studies showed that the longitudinal decline was smaller than what was predicted from cross-sectional analyses43,44 among younger subjects, and that this relationship was age-related and switched between 40 and 45 years of age.44 Nevertheless, the extent to which the spirometric measures decreased in the current study were well above those observed longitudinally in the studies noted above and indicate that a higher than normal decrease in pulmonary function occurred in this cohort of firefighters during the 5-year period as compared with what would be expected in the general population.
CONCLUSION
A reduction in firefighter respiratory function two-to-four-times greater than the estimated decrease expected in the general population over a 5-year period was found among career firefighters. These findings provide evidence that more stringent use of SCBA is still needed to protect the respiratory health of firefighters. Respiratory protection should be used when firefighters are exposed to smoky conditions, such as on the fireground, or during overhaul activities when gas and particulate levels are elevated even if the air appears clear.
Footnotes
Funding: This work was supported by the Federal Emergency Management Agency, Assistance to Firefighters Grant [EMW-2017-FP-PP-00445].
Conflicts of Interest: None declared.
Clinical significance: The decreases in pulmonary function over 5 years in a cohort of career firefighters were two to four times greater than expected. Health care providers should track decrements in spirometry values to identify excessive changes and encourage the use of respiratory protection during all phases of fire suppression.
REFERENCES
- 1.Technical Committee on Fire Service Occupational Safety and Health. NFPA 1582, Standard on Comprehensive Occupational Medical Program for Fire Departments. Quincy, USA: National Fire Protection Association; 2018. 11–12. [Google Scholar]
- 2.Crapo RO. Pulmonary-function testing. N Engl J Med 1994; 331:25–30. [DOI] [PubMed] [Google Scholar]
- 3.Peters JM, Theriault GP, Fine LJ, Wegman DH. Chronic effect of fire fighting on pulmonary function. N Engl J Med 1974; 291:1320–1322. [DOI] [PubMed] [Google Scholar]
- 4.Sherman CB, Barnhart S, Miller MF, et al. Firefighting acutely increases airway Responsiveness1-3. Am Rev Respir Dis 1989; 140:185–190. [DOI] [PubMed] [Google Scholar]
- 5.Sheppard D, Distefano S, Morse L, Becker C. Acute effects of routine firefighting on lung function. Am J Ind Med 1986; 9:333–340. [DOI] [PubMed] [Google Scholar]
- 6.Betchley C, Koenig JQ, van Belle G, Checkoway H, Reinhardt T. Pulmonary function and respiratory symptoms in forest firefighters. Am J Ind Med 1997; 31:503–509. [DOI] [PubMed] [Google Scholar]
- 7.Miedinger D, Chhajed PN, Stolz D, et al. Respiratory symptoms, atopy and bronchial hyperreactivity in professional firefighters. Eur Respir J 2007; 30:538–544. [DOI] [PubMed] [Google Scholar]
- 8.Greven FE, Krop EJ, Spithoven JJ, et al. Acute respiratory effects in firefighters. Am J Ind Med 2012; 55:54–62. [DOI] [PubMed] [Google Scholar]
- 9.Greven F, Krop E, Spithoven J, Rooyackers J, Kerstjens H, Heederik D. Lung function, bronchial hyperresponsiveness, and atopy among firefighters. Scand J Work Environ Health 2011; 37:325–331. [DOI] [PubMed] [Google Scholar]
- 10.Prezant DJ, Weiden M, Banauch GI, et al. Cough and bronchial responsiveness in firefighters at the world trade center site. N Engl J Med 2002; 347:806–815. [DOI] [PubMed] [Google Scholar]
- 11.Tepper A, Comstock GW, Levine M. A longitudinal study of pulmonary function in fire fighters. Am J Ind Med 1991; 20:307–316. [DOI] [PubMed] [Google Scholar]
- 12.Mustajbegovic J, Zuskin E, Schachter EN, et al. Respiratory function in active firefighters. Am J Ind Med 2001; 40:55–62. [DOI] [PubMed] [Google Scholar]
- 13.Large AA, Owens GR, Hoffman LA. The short-term effects of smoke exposure on the pulmonary function of firefighters. Chest 1990; 97:806–809. [DOI] [PubMed] [Google Scholar]
- 14.Musk AW, Peters JM, Bernstein L, Rubin C, Monroe CB. Pulmonary function in firefighters: a six-year follow-up in the Boston fire department. Am J Ind Med 1982; 3:3–9. [DOI] [PubMed] [Google Scholar]
- 15.Occupational Safety and Health Administration. Occupational Safety and Health Standards: Personal Protective Equipment, Respiratory Protection. Available at: https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134. Accessed February 12, 2020. [Google Scholar]
- 16.Technical Committee on Respiratory Protection Equipment. NFPA 1981, Standard on Open-Circuit Self-Contained Breathing Apparatus (SCBA) for Emergency Services. Quincy, MA: National Fire Protection Association; 2019. [Google Scholar]
- 17.Fabian TZ, Borgerson JL, Gandhi PD, et al. Characterization of firefighter smoke exposure. Fire Technol 2014; 50:993–1019. [Google Scholar]
- 18.Fent KW, Alexander B, Roberts J, et al. Contamination of firefighter personal protective equipment and skin and the effectiveness of decontamination procedures. J Occup Environ Hyg 2017; 14:801–814. [DOI] [PubMed] [Google Scholar]
- 19.Alexander BM, Baxter CS. Plasticizer contamination of firefighter personal protective clothing–a potential factor in increased health risks in firefighters. J Occup Environ Hyg 2014; 11:D43–D48. [DOI] [PubMed] [Google Scholar]
- 20.Fent KW, Toennis C, Sammons D, et al. Firefighters’ absorption of PAHs and VOCs during controlled residential fires by job assignment and fire attack tactic. J Expo Sci Environ Epidemiol 2019; 30:338–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park J, Voss RW, McNeel S, et al. High exposure of California firefighters to polybrominated diphenyl ethers. Environ Sci Technol 2015; 49:2948–2958. [DOI] [PubMed] [Google Scholar]
- 22.Fent KW, Evans DE, Babik K, et al. Airborne contaminants during controlled residential fires. J Occup Environ Hyg 2018; 15:399–412. [DOI] [PubMed] [Google Scholar]
- 23.Horn GP, Stewart JW, Kesler RM, et al. Firefighter and fire instructor's physiological responses and safety in various training fire environments. Saf Sci 2019; 116:287–294. [Google Scholar]
- 24.Daniels RD, Bertke S, Dahm MM, et al. Exposure–response relationships for select cancer and non-cancer health outcomes in a cohort of US firefighters from San Francisco, Chicago and Philadelphia (1950–2009). Occup Environ Med 2015; 72:699–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burgess JL, Nanson CJ, Bolstad-Johnson DM, et al. Adverse respiratory effects following overhaul in firefighters. J Occup Environ Med 2001; 43:467–473. [DOI] [PubMed] [Google Scholar]
- 26.Austin CC, Dussault G, Ecobichon DJ. Municipal firefighter exposure groups, time spent at fires and use of self-contained-breathing-apparatus. Am J Ind Med 2001; 40:683–692. [DOI] [PubMed] [Google Scholar]
- 27.Slattery F, Johnston K, Paquet C, Bennett H, Crockett A. The long-term rate of change in lung function in urban professional firefighters: a systematic review. BMC Pulm Med 2018; 18:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Technical Committee on Fire Service Occupational Safety and Health. NFPA 1582, Standard on Comprehensive Occupational Medical Program for Fire Departments. Quincy, MA: National Fire Protection Association; 2018. [Google Scholar]
- 29.Walters JA, Wood-Baker R, Walls J, Johns DP. Stability of the EasyOne ultrasonic spirometer for use in general practice. Respirology 2006; 11:306–310. [DOI] [PubMed] [Google Scholar]
- 30.Skloot GS, Edwards NT, Enright PL. Four-year calibration stability of the EasyOne portable spirometer. Respir Care 2010; 55:873–877. [PubMed] [Google Scholar]
- 31.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general US population. Am J Respir Crit Care Med 1999; 159:179–187. [DOI] [PubMed] [Google Scholar]
- 32.Mannino DM. Chronic obstructive pulmonary disease: definition and epidemiology. Respir Care 2003; 48:1185–1193. [PubMed] [Google Scholar]
- 33.Liu D, Tager IB, Balmes JR, Harrison RJ. The effect of smoke inhalation on lung function and airway responsiveness in wildland fire fighters. Am Rev Respir Dis 1992; 146:1469–1473. [DOI] [PubMed] [Google Scholar]
- 34.Musk AW, Peters JM, Wegman DH. Lung function in fire fighters, I: a three year follow-up of active subjects. Am J Public Health 1977; 67:626–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Musk AW, Petters JM, Wegman DH. Lung function in fire fighters, II: a five year follow-up fo retirees. Am J Public Health 1977; 67:630–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aldrich TK, Ye F, Hall CB, et al. Longitudinal pulmonary function in newly hired, non-World Trade Center-exposed fire department city of New York firefighters: the first 5 years. Chest 2013; 143:791–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging 2006; 3:253–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Park H, Park J, Lin S, Boorady LM. Assessment of firefighters’ needs for personal protective equipment. Fashion Textiles 2014; 1:8. [Google Scholar]
- 39.Alarie Y. Toxicity of fire smoke. Crit Rev Toxicol 2002; 32:259–289. [DOI] [PubMed] [Google Scholar]
- 40.Schermer TR, Malbon W, Adams R, Morgan M, Smith M, Crockett AJ. Change in lung function over time in male metropolitan firefighters and general population controls: a 3-year follow-up study. J Occup Health 2013; 55:267–275. [DOI] [PubMed] [Google Scholar]
- 41.Daniels RD, Kubale TL, Yiin JH, et al. Mortality and cancer incidence in a pooled cohort of US firefighters from San Francisco, Chicago and Philadelphia (1950–2009). Occup Environ Med 2014; 71:388–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kerstjens HA, Rijcken B, Schouten JP, Postma DS. Decline of FEV1 by age and smoking status: facts, figures, and fallacies. Thorax 1997; 52:820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Van Pelt W, Borsboom GJ, Rijcken B, Schouten JP, Van Zomeren BC, Quanjer PH. Discrepancies between longitudinal and cross-sectional change in ventilatory function in 12 years of follow-up. Am J Respir Crit Care Med 1994; 149:1218–1226. [DOI] [PubMed] [Google Scholar]
- 44.Ware JH, Dockery DW, Louis TA, Xu X, Ferris BG, Jr, Speizer FE. Longitudinal and cross-sectional estimates of pulmonary function decline in never-smoking adults. Am J Epidemiol 1990; 132:685–700. [DOI] [PubMed] [Google Scholar]


