Objective:
To evaluate effectiveness of a workplace educational intervention at improving health-related outcomes in carer-employees.
Methods:
A pre-post test design compared with health of a sample (n = 21) of carer-employees before (T1) and after (T2) a workplace intervention, as well as a final timepoint (T3) 12 months after T1. An aggregate health score was used to measure health and consisted three scales; depression (CES-D), psychosocial (CRA), and self-reported health (SF-12), where higher scores indicated higher frequency of adverse health symptoms. Three random-slope models were created via the linear mixed modeling method (LMM) to illustrate changes in reported health.
Results:
All three LMM models reported a reduction in participants’ health score, particularly between T1 and T2, indicating a decrease in reported adverse health symptoms.
Conclusion:
The intervention was successful in improving the health of carer-employees.
Keywords: caregiver-friendly workplace policies, employee health, intervention, time series
BACKGROUND
Introduction
Currently, there are over 700 million individuals aged 65 years or older globally, with this number expected to burgeon to 1.5 billion in 2050.1 Demographic trends in Canada, such as: the growing labor force participation of women, declining average household family size, and rising retirement age have led to increased pressure on the working population to provide informal care to the elderly population, as they increase in number.2 This research defines family caregivers, herein named carers, as individuals that provide unpaid informal care for family members and friends due to health, disability, or age-related conditions.3 In Canada, over 8 million individuals or 23.5% of the total population, provide such aid to family members or friends, with 60% of carers managing employment responsibilities alongside caring duties.2 These carers, shouldering professional work duties on top of care provision are known as carer-employees. As a growing cohort alongside the aging population, they are commonly aged 45 to 64, caring for a parent, and at or near the height of their careers, creating tensions in the labor market when work and care obligations conflict.2,4
Care responsibilities often include: personal/medical assistance, transportation, emotional support, management of finances and medical appointments, shopping, meal preparation, and housework. These unpaid services performed by carer-employees save the Canadian government $25 billion annually in health expenditures.5,6 It can be surmised then, that carer-employees produce significant and invaluable contributions to the healthcare sector on top of paid work obligations.
Demands of care and work have increased in recent years, due to the deinstitutionalization of formal care, together with the movement towards a connected global economy. This has led to a growing burden on carer-employees. This burden has potential ramifications on their capacity to maintain both roles, leading to deterioration of health and job performance. For example, carers have a higher risk for developing depression, sleep disturbance, psychosocial issues, and increased stress levels when compared with non-carers.7,8 In addition, lack of carer programs in the workplace can result in an increase of absenteeism (missing work), presenteeism (distraction), and issues with retention and productivity.9 We have estimated previously that the economic consequence of care provision costs the specific workplace that is the focus of this study, approximately $8674 CAD per carer-employee.10 A more conservative estimate found that, on average, American employers may lose at least $2400 USD per employee due to lack of carer workplace programs that result in loss of productivity and absenteeism.11 Given that the number of carer-employees in Canada are projected to rise with the aging population, there will be a growing need for recognition and support of carer-employees from employers and policy-makers. One strategy to be considered by employers is the implementation of carer-friendly workplace programs (CFWPs) such as: flexible working hours, telecommuting, support services, paid or unpaid leave, financial assistance, and culture change.12
This study seeks to explore the effects of implementing a CFWP on carer-employee's health in a university workplace. The following section presents a literature review discussing: carer-employee burden, the relationship to physical and mental health in Canada, current state of CFWPs, and evidence for carer interventions. This section is followed by a presentation of our research objectives, before continuing with methodology, results, and finally, an argument for greater integration of CFWPs in the discussion and conclusion.
LITERATURE REVIEW
Carer-Employee Burden
Carer burden refers to the perceived stress associated with the carer role, and is often associated with poor physical and mental health. Burden can be both objective, denoted by physical, financial, and social demands of care provision, as well as subjective, relating to the carer's reaction towards performing care tasks.13 The majority (89%) of Canadian carers report caregiving for over 1 year.2 Generally, carer burden results in depressed mood, greater perceived difficulty in performing care work, anxiety, sleep disturbance, and social isolation.13–16 Carer burnout is a recognized clinical condition, reached when carer burden results in extensive feelings of exhaustion from strain in the carer's physical, psychosocial, financial, and emotional capacities.14 Most commonly, burden and eventually burnout, arises when paid work and personal obligations are incongruent with each other, and there is a lack of services and accommodations to assist in negotiating work-life balance.15
The majority of carers are often women, with approximately 54% of Canadian carers identifying as women in 2012.2 Greater carer burden is experienced both acutely and chronically in female carers as compared with male carers, with female carers being significantly more likely to be responsible for tasks such as personal care, medical assistance, housework, emotional support, and meal preparation.2,4,17–19 These tasks are generally time sensitive and urgent, allowing for less flexibility in the carer's schedule. Male carers are significantly more likely to provide physical assistance in house maintenance and repairs, which generally allows for greater flexibility to schedule such commitments outside of traditional working hours. This division of tasks is reflected in the time spent on care-related tasks; women are more likely than men to spend more than 20 hours per week on caregiving related activities than men, with 17% of female carers doing so as compared with 11% of male carers.2,18,19 Additionally, women average approximately 5.8 years of caregiving throughout their lives, while men average approximately 3.4 years.19 These duties result in women being more time-constrained and for longer periods of time, which impact their health as well as ability to perform in other areas of their lives.
Carer burden can include financial commitments such as out of pockets costs of medication and transportation, which may cost on average $3300 CAD annually.20–22 Given this, the financial burden of caring influences lower-income carer-employees significantly more than well-resourced carer-employees.23 Low-income carer-employees were found to have a higher probability of suffering from mental health issues, when compared with higher-income carer-employees.16 A high carer burden can manifest in other dimensions of carer-employee's lives, such as quality of sleep and mental health, compromising their wellbeing and productivity at work.
Effects on Work and Health
Carer-employees may accrue a multitude of health and employment impacts due to the burden of managing their work-life balance. This is exacerbated by the often-chronic nature of caring. There is an observed positive correlation between reported carer burden and length of time spent as a carer, in which burden is greater the longer one has been in a carer role.24–26 Other adverse effects incurred due to carer-employee responsibilities include: poor morale, reduction in quality of interpersonal relationships, reduced social activities, and loss of one's sense of independence.9 This results in poorer overall quality of life in carer-employees, leaving many carer-employees feeling isolated, frustrated, fatigued, and stressed. Approximately 38% of Canadians report overall health decline due to caring duties.27
For many carers, carer burden and time constraints lead to diminished capacity to engage in paid work. Forty three percent (43%) of Canadian carers in 2012 reported missing partial or full days of work due to caring responsibilities, while 15% reduced their work hours to accommodate their work-life balance.27 Of those 43%, a further 14% lost employer provided health benefits, pension, and insurance as a direct result of reduced engagement in the workforce. From 2003 to 2008, net lost wages because of caregiving duties amounted to $336.8 million CAD annually, representing a direct loss of financial capital for carer-employees.28 We estimated that the annual economic cost absorbed by carer-employees at the research worksite of concern herein was approximately $32,922 per carer, due to loss of income, out of pocket caregiving expenses, and opportunity cost of caregiving labor.10
Perceived burden is the result of a variety of dynamic factors, including: intensity of care, sex, care recipient condition, and carers’ financial status—all of which uniquely impact work-life balance. Understanding how each of these factors interact dynamically to form the carer-employee experience may shed light on how carer burden and health outcomes can be improved through CFWPs to produce healthier and productive work environments.
Workplace Accommodations
CFWPs are designed modifications to organizational structure, policies, or programs for the purpose of supporting employee work-life balance and reducing conflicts for carer-employees.12,29,30 Interest in implementation of CFWPs has been growing in recent years, with the finance, technology, and healthcare sectors leading in terms of present CFWP prevalence.12,31 Canadian businesses have been losing an approximate $1.3 billion worth of productive hours annually due to caregiving demands on employee time.32 Recognizing this, many workplaces are motivated to adopt various CFWPs to avert these costs as well as additional benefits such as increased employee satisfaction, and positive company reputation.29,31,33 The most common forms of CFWPs are currently flexible working arrangements, support services (eg, counselling), and paid/unpaid leaves.12 Within the Canadian context, little is known about the efficiency and uptake of these CFWPs in any form.
Carer Interventions
Interventions targeted towards carers generally fall into the following types: education, behavioral change, case study, support services, and psychosocial (eg, counseling, therapy).34 Carer interventions are developed with the aim of being therapeutic while building supportive capacity for carers.35,36 Common intervention protocols have intentionally sought to build: coping skills, knowledge of available resources, knowledge of how to best manage care recipient conditions, psychosocial health, carer burden, and planning skills.37
Generally, carer interventions tend to produce modest but positive effects.37,38 This is largely theorized to be the result of the multidimensional and complicated nature of carer burden.37,39 Multicomponent interventions tend to show more pronounced intervention effects, likely due to a broader range of resources offered to carers.35 A 2002 meta-analysis of 78 carer interventions found two broad classes of interventions: (1) respite-type interventions aimed at reducing objective burden, and; (2) psychoeducational interventions targeting wellbeing.37 In addition, intervention effects related to building carer capacity and knowledge were found to have greatest short-term changes.37
While workplace carer interventions have not been extensively explored, there is evidence that workplaces may be useful interventions sites for health factors by reducing work-family conflict. Modification to employee work environment, such as increased opportunity for job control and decision making at work or increased supports to decrease workload, has been associated with improved mental health and physical health in employees.40 This finding was reflected in the results of a meta-analysis of workplace interventions for healthcare workers, where work schedules conducive to work-life balance were associated with significant reductions in stress.41 Given the increasing elderly population and demands of eldercare, carer burden greatly contributes to work-family conflict. Workplace interventions for carer-employees may offer a preventative solution to employee stress and burnout.
RESEARCH OBJECTIVES
This CFWP intervention pilot program is divided into three phases, with the overall goal of building the business case regarding the implementation of workplace programs for carer-employees.3 Approved by the university's Research Ethics Board (ISRCTN 16187974), this study pertains specifically to the first phase (Phase A), in which a web-based decision tool was developed as an intervention for improving carer-employee health outcomes. This specific paper examines quantitative health outcomes at the conclusion of Phase A.
We aim to evaluate the effectiveness of an educational CFWP when implemented in the work environment over time. More specifically, this research asks the following question: does the implementation of CFWPs improve the health condition of carer-employees over time? The results will offer actionable evidence to policy decision makers on the benefits of CFWPs, while providing guidelines regarding the organizational changes necessary for the inclusion of carer-employees in healthy productive workplaces.
In keeping with the literature review, our CFWP intervention explores educational effects of a CFWP intervention on carer-employee's health and wellbeing. The multicomponent intervention was designed to include both an educational and behavior change component, to maximize potential intervention effects. Additionally, our participants include carers of care recipients of all disease-types, in order to yield more inclusive narratives.
METHODS
As part of a larger research program, the full methodology has previously been published.3 Phase A employed the use of a pre-post intervention design to empirically quantify changes in carer-employee's health following the CFWP intervention. Interview survey measures used to capture carer-employee health include: self-reported health; psychosocial health, and depression. The intervention took place between the pre-test (Time 1 or T1) and post-test (Time 2 or T2), while the terminal point (Time 3 or T3) survey was implemented approximately 6 months after T2.
Recruitment and Demographics
This study was conducted at a large university located in Southern Ontario, Canada. Individual participants employed at the university were invited to participate in the study through an extensive multi-pronged recruitment strategy which encompassed: postcard and poster advertisements, electronic ads on TV displays screens, advertisements via e-mail lists, word of mouth, and, cold calling across various departments.
Eligibility criteria of participants included: working full-time in some capacity at the institution concerned while also actively caring for an adult dependent. The study procedure and purpose were verbally explained to each potential participant over email or phone. Interested participants were provided with a written consent form to review and sign. Before each data collection point, oral consent from participants were confirmed when verbally reminded of the study's goals, design, and their rights as participants to withdraw at any time or choose not to answer any questions. A total of 21 participants made up the convenience sample.
Each participant completed the same CFWP interview survey, where researchers would verbally ask each question (either in person or verbally over the phone) and record participant responses on an electronic copy of the survey. Survey data were collected at three different time periods (T1 to T3) across a 12-month period. The first T1 surveys were collected in the spring of 2016 and the last T3 surveys were concluded January 2018.
Table 1 depicts fluctuations in the sociodemographic profile of each participant pool across time. Overall, our sample population appears to be fairly homogenous. The participant population were female-skewed, mostly over the age of 45 years old, Caucasian, highly educated, and likely to have a household income of over $70k CAD per annum.
TABLE 1.
Descriptive Statistics Containing General Demographics of Sample
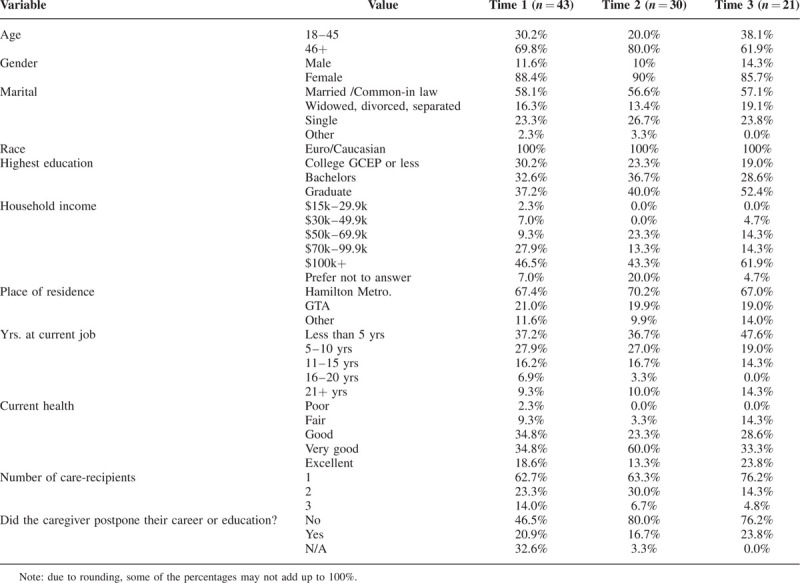
Marital status, income, sex, education, years are current job, and number of care-recipients tend to be fairly stable over time, even with participant drop-out. Overall, the sociodemographic profile of withdrawing participants was fairly similar to the remaining pool. While we cannot argue for random distribution of participant drop-out, we observe that there does not appear to be an overt sociodemographic pattern of participant withdrawals.
Participant Drop-Out
Forty-three (43) participants were originally recruited at T1. From T1 to T2, 13 of the 43 participants withdrew (N = 30). By the end of this study (T3), only half of the sample size (n = 21) was left due to the disqualification of participants based on the inclusivity criteria. Disqualification was due to: (1) the care-recipient passing away (two participants); (2) the participant no longer providing informal care (two participants); (3) the participant no longer working full-time (three participants). Ten participants withdrew from the research program for reasons not disclosed, while an additional two participants withdrew citing time constraints due to work and family responsibilities. Three participants were non-responsive or had invalid responses. Data from these participants were removed from the study, as per ethics guidelines.
Intervention
The educational intervention itself consisted of an in-person meeting with each individual participant, which occurred between T1 and T2 with the first author. Demographic and employment data were collected from the participants and entered into a web-based decision tool, which then produced a customized list of tailored caregiving and work-related resources and programs at the community, workplace, provincial and federal level. These options were explored in detail between the researcher and participant. Following this, participants were provided a list of behavior change goals from a checklist and encouraged to focus on two items to attempt to accomplish by the next meeting. Participant progress on the checklist activity was then followed up with at T2 and T3.
Survey Instruments
The selection of instruments and variables captured in the survey was designed by the Principle Investigator in consultation with economists and work-family researchers. The survey captured a diverse set of variables; however, only health related variables are reported in this paper. The three manifest scales used for analysis in this paper include: self-reported health (SF-12), carer reaction (CRA), and depression (CES-D). All instruments were selected for their validity, moderate to excellent internal consistency and reliability, in addition to their prevalence in clinical health and sociological literature, particularly in American and European contexts.42–46
The SF-12 manifest scale contained 12 items that evaluated participants’ perception of their own physical and mental wellbeing. Examples of topics probed include: level of physical activity, self-assessments of pain/discomfort, mood, emotional problems, and execution of routine tasks. The CRA scale contains 24 items and probed dimensions of psychosocial health pertaining to financial burden, caring activity, familial support, physical/emotional strain, and attitude towards caring. The CES-D is a 10-item scale investigating frequency and intensity of depressive symptoms. Most of the answer options for each scale were formatted using a Likert scale, such as: from “Excellent” (a score of 1) to “Poor” (a score of 5), and “All of the time” (a score of 5) to “None of the time” (a score of 1). All three scales explore multidimensional aspects of health.
Analysis of all data was conducted on R version 3.5.3 (R Foundation for Statistical Computing, Vienna, Austria). All items were converted to numerical values and coded in the same direction, such that lower scale sums are associated with positive outcomes and higher scale sums indicated more adverse outcomes. All scales were individually tested for reliability within the context of our study by creating a time-series correlation matrix and using the test-retest via intra-class correlation (ICC) coefficient method using data collected from all time points.
A health condition scale was generated by summing up all three scales at each time point, due to the multidimensional nature of the scales investigating overlapping phenomena and high reliability of the scales. This health condition scale was used as the dependent variable in the linear mixed modeling (LMM). The complete longitudinal dataset contained less than 5% missingness where instances of missing data were randomly distributed single items within the aforementioned scales. Missing data were therefore imputed using multiple imputation via predictive mean matching with five iterations, if the total number of missing items were less than 30% of the total items in the scale; otherwise, the scale would be excluded from analysis for that specific participant.47 The datasets from all three time periods were cleaned up and aggregated into long format (longitudinal) to conduct linear mixed modelling (LMM).
Linear Mixed Modeling
LMM was selected as the most appropriate method for analysis due to its ability to: (1) handle longitudinal data; and, (2) analyze the changes in health condition as a random effect measurement for the intervention. LMM is an extension of the simple linear regression model for longitudinal or group structured data.48 While linear regressions measure single fixed effects of a dependent variable, LMM measures the random effects, or differences, between grouped data in addition to these fixed effects. Fixed effects represent a scaled relationship between the predictor and explanatory variables, in this case, the relationship between participants’ health scores and time (T1 to T3).49 Random effects are represented by a categorical variable with levels assumed to be a random selection from a hypothetical larger population.49 They can act as a grouping factor to be controlled. In the case of this analysis, participant ID numbers were used as random effects to account for variation in health score between participants.49 In layman terms, this analysis is identifying associations between the health condition of participants and time, specifically examining the impact of the intervention on participant health, while controlling for inter-participant variation. Each time period (T1 to T3) in the regression was indicated by a dummy variable, while an additional dummy variable was created using time data to denote whether the intervention had occurred (T2 and T3) or not (T1).
Three random intercept LMM were created to investigate if there is an association between health scores and time as well as which time periods indicate greater changes to the participant's health. The first model compares changes between participants health amongst the entire intervention, where T2 and T3 are aggregated as a dummy variable. The second and third model expands upon the first by examining the specific effects of the T2 or T3 dummy variables respectively, as a separate independent variable within the entire intervention.
RESULTS
Reliability Analysis
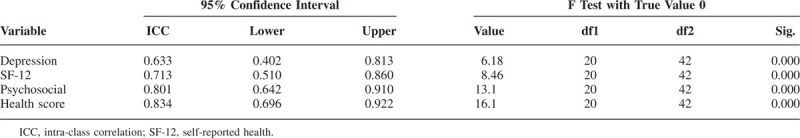
The correlation matrix reported the manifest scales across all time periods to be: reliable; somewhat consistent; showing a significant increase from T1 to T2, and; having relatively strong linkages (Table 2). The strength of all correlations are classified as strong (0.5+) with a range of 0.58 to 0.92, indicating strong correlations between all the scales.50
TABLE 2.
Correlation Matrix With Respective Correlation Coefficients of Health Indices Across Three Time Periods
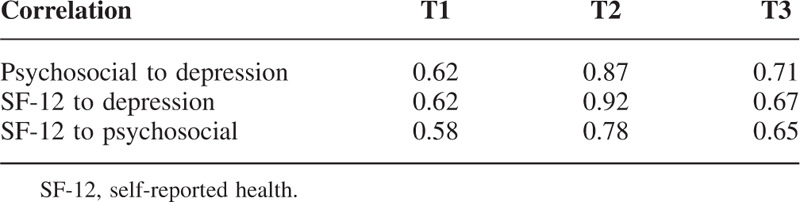
The ICC test-retest analysis shown in Table 3 conveys a range of good (depression and SF-12 scales) to excellent (psychosocial and health score) inter-rater agreement measures.44 This indicates that the manifest scales in all time periods are reliable and consistent for further analysis.
TABLE 3.
Test-Retest One-Way Random Effects Model Using Single Measures
Descriptive Statistics
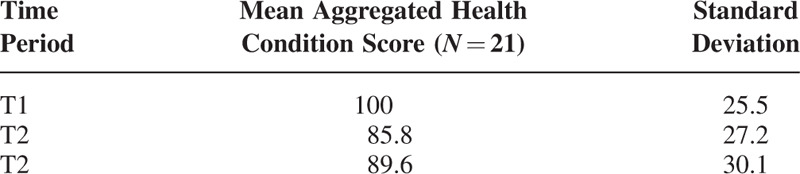
Figure 1 displays the health score of each participant over time, and Table 4 shows mean values and standard deviation of the health score. The majority of the participants’ health improved greatly between pre-intervention (T1) to the first wave of the intervention (T2), as noted by the downward trend in health condition score (from 100 at T1 to 85.8 at T2). Between T2 and T3, the plot (Fig. 1) illustrates mixed results with some participants getting a bit worse while others not improving much relative to the changes from T1 to T2. Overall, the health condition score increased from 85.5 at T2 to 89.6 at T3 (Table 4). The average health condition scores from T1 to T3 conveys a downward trend, from 100 (T1) to 89.6 (T3).
FIGURE 1.
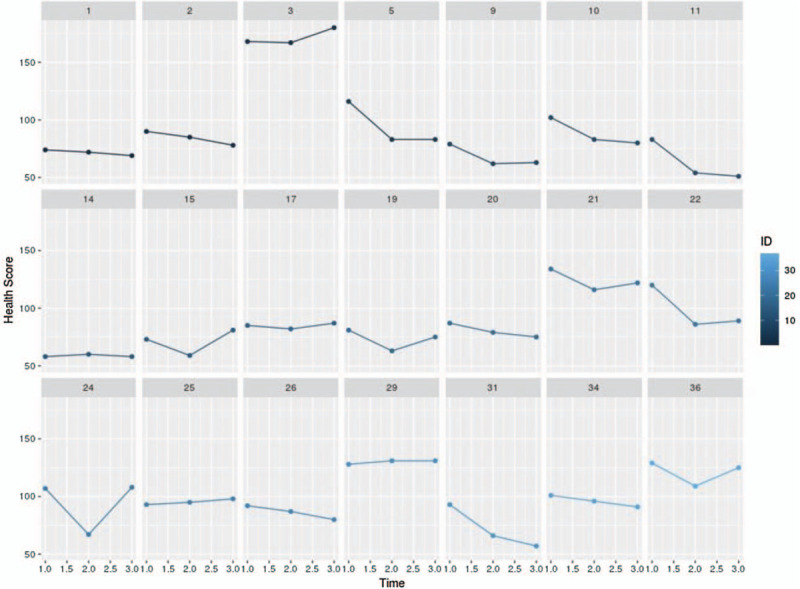
Individual participant aggregated health condition scores over time (T1 to T3), where each plot represents a participant. Participant numbers are labeled above each plot.
TABLE 4.
Aggregated Health Scale Means at Each Time Point (T1–T3)
Power Analysis
Given the small sample size, a power analysis was necessary to validate the results of the analysis. Figure 2 depicts a plot of minimum sample size required for a specific effect size. In the context of our study, we set our type I error at 0.05 (paired), and the statistical power (1 – β) was set at 0.8 to test the validity of intervention when the effect size goes from about 1.0 to 0.1. Based on Cohen guidelines,51 a moderate to large effect size (d > 0.5) requires a sample size of approximately 20 or less. Based on this result, we can verify the validity of our results with a small sample size.
FIGURE 2.
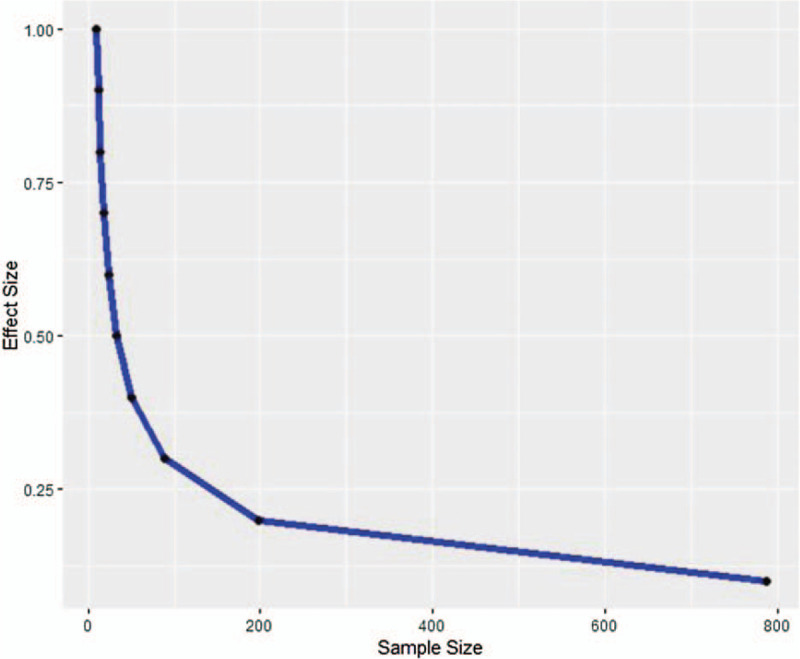
Minimum sample size required for effective changes, where greater sample sizes are needed to verify smaller effect sizes.
Principal Component Analysis
A socioeconomic index was generated using principal component analysis (PCA) to determine the extent of social and demographic variation in our final T3 sample.52 This was done as the small sample size in our study precluded the addition of sociodemographic and economic variables in our LMM models, and there was a need to control these variables. PCA was conducted to reduce the dimensionality of socioeconomic variables, such as age, sex, education level, income and marital status, through creating an index that examines total variance. The first principal component (PC1) indicates the orthogonal linear combination of the variables that accounts for the maximum variance in the data.53 Subsequent components capture unrelated and lesser variation; thus, PC1 provides the most information.54 Socioeconomic and demographic data for each participant was converted into a binary format, and tetrachoric correlation was used for the PCA index, as seen in Table 5 below.
TABLE 5.
Assignment of Participant Categorical Data into Binary Values
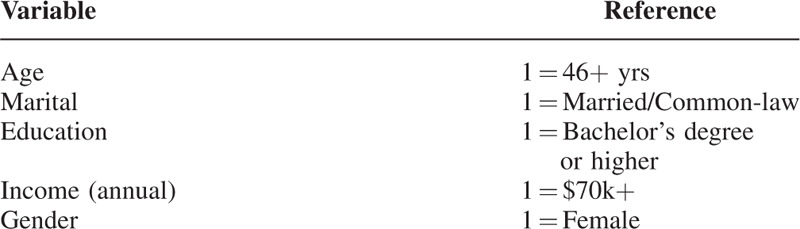
Table 6 depicts the variable loadings resulting from the PCA, as well as the proportion of variance of each component. Principal component loadings represent eigenvalues that indicate weights of each variable on the principal component.55 PC1 had a proportion variance of 38%, in contrast to PC2 and PC3, which had 32% and 23% respectively. Only the first three components (PC1 to PC3) were retained, as the variance in the first three components account for 93% of the total variation when the proportion of variance score was summed.
TABLE 6.
Variable Loadings of First Three Principal Components
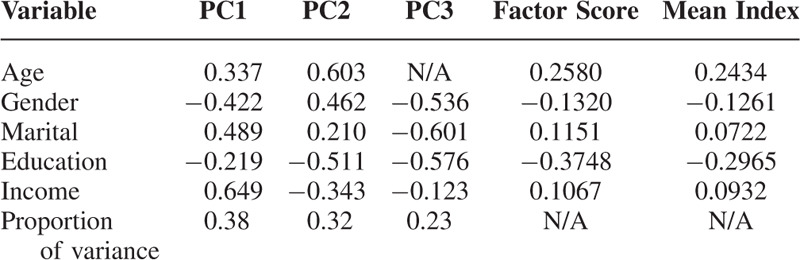
PC1 explains the largest variance of the data and has large positive loadings on income and marital status together with large negative loadings on sex; this indicates that income and marital status are inversely proportional to sex. PC2 had large positive loadings on age and sex, while having large negative loading on education. PC3 contains large negatively loadings on sex, marital status, and education only.
Factor scores were generated by multiplying principal component loadings with the proportion of variance for each variable and summed through PC1 to PC3 (Table 6). The absolute value of each factor score represents the weighting of each respective variable (either as positive or negative) of the carer-employee's socio-economic status. Age (46+ years), marital status (married), and income ($70k+) are positive, indicating a higher socio-economic status of the carer-employee. These findings match the demographic profile found in the caregiving literature.2,19 Interestingly, education (Bachelors or higher) and sex (female) reveal negative scores, thus, lowering the socio-economic status of the carer-employee. A plausible explanation for sex may be that women are more likely to be carers when compared with men (as noted earlier), which would hinder their career potential. A higher education may entail more job responsibilities and, together with the responsibilities of caregiving, may leave the carer-employee stressed. Overall, socioeconomic variation within our sample population is not strong, suggesting that these demographic variables are likely not underlying confounding factors within the analysis.
Linear Mixed Models
All three models reported similar goodness of fit and statistically significant intercepts on both random effects and fixed effects (Tables 7–9). The first model (Table 7) looked at intervention effects over the whole study (T1 to T3), with T2 and T3 variable aggregated. The model showed the intercepts on both random and fixed effects to be statistically significant with relatively low standard errors. The coefficient of overall time of intervention was approximately –12 and statistically significant. This indicates that from T1 to the combined time of intervention (T2 and T3), the participants reduced their health condition score by –12.
TABLE 7.
Random Intercept Model 1: Intervention (T2 and T3 Aggregated)
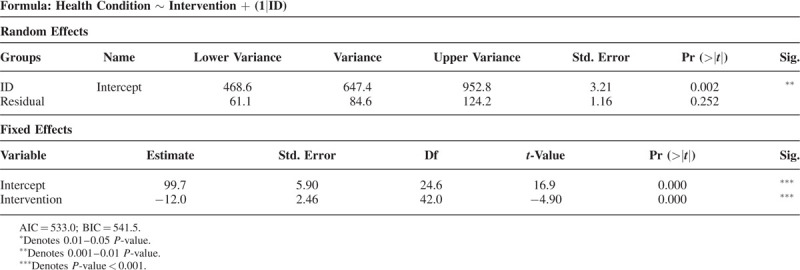
TABLE 9.
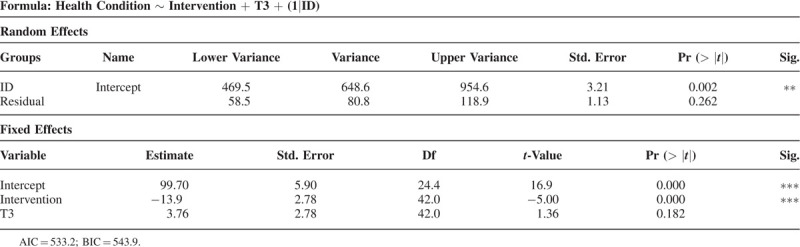
Random Intercept Model 3: T3 and Intervention (T2 and T3 Aggregated)
The second model (Table 8) used the same aggregation of T2 and T3 to examine intervention effects over the entire study, but used T2 as a factor in the regression equation. Model 2 had a coefficient of –10 for the overall intervention, when factoring T2 as a dummy variable, while the T2 variable had a coefficient of –4, though this was not statistically significant.
TABLE 8.
Random Intercept Model 2: T2 and Intervention (T2 and T3 Aggregated)
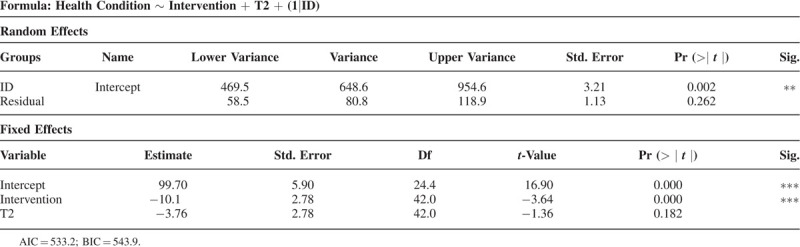
For the third model (Table 9), the overall time of the intervention had a coefficient of –14, with statistical significance. The dummy variable of T3 displays an approximate increase of 4, despite not being statistically significant. This finding similarly reflects the plot in Fig. 1, which illustrates that some participants increased their health condition score after T2. In general, when implementing the overall intervention, the health condition score of the participants is reduced, which improves their general wellbeing. Overall, the first model seems to be the most appropriate model for the data, as it is simpler and has slightly better Akaike information criterion (AIC) and Bayesian information criterion (BIC) scores.
DISCUSSION
This study examines the effectiveness of CFWPs within the workplace environment by assessing changes in carer-employees’ health. To our knowledge, this is the first study of its kind, where the relationship between a workplace-based CFWP intervention for carer-employees, and the mitigation of negative effects with respect to physical and emotional health, psychosocial health, and mental aptitude has been studied. Data were cleaned and validated for suitability prior to all analysis. Due to the small sample size, several preliminary analyses, such as: reliability analysis, correlation matrices, power analysis, and PCA, had to be conducted to confirm appropriateness of our data for final analysis.
Our findings suggest that the original objective of this paper was met; the workplace intervention was successful in reducing self-reported health, psychosocial health, and depression outcome variables, resulting in overall improvements of carer-employees’ health from T1 to T3. Compared with the baseline measurements of T1, all of the participants (N = 21) who received the standardized intervention generally reported significantly fewer or reduced symptoms of depression, psychosocial burden, and poor self-reported health during the post intervention assessment (T2) (Fig. 1). These effects were measured to be statistically significant (P < 0.05) within and between participants (Tables 7–9). While we observed an overall decline in adverse health variables throughout the whole project (T1 to T3), transformations were non-statistically significant (P > 0.05) between T2 to T3 (Tables 8 and 9), suggesting that intervention effects were maintained over time. The improvement in health outcomes are evident across all three LMM models.
Model 2 and 3 (Tables 8 and 9) explored the effects of T2 and T3 as a dummy variable in the regression equation. However, the exact effects of T2 and T3 specifically on the intervention were inconclusive due to the non-significance of T2 and/or T3 as a regression variable, despite the models indicating significant overall intervention effects. With that, we highlight Model 1 is the best representation of the data, as it is the simplest model that conveys the effectiveness of the intervention over time.
While existing evidence for carer interventions are limited, our findings generally align with evidence from the literature, in which carer health can be improved by interventions. A meta-analysis of 127 interventions found that psychoeducational interventions are able to produce significant effects on carer burden, depression, subjective wellbeing, carer knowledge, and care recipient symptoms, although these effects are most pronounced in interventions with active carer participation rather than information only.38 Our study differs in that we were able to produce significant effects on carer health with a largely informational intervention. This may reflect the setting of our intervention, in which information and resources were provided in person and discussed with the carer. This dialogue between the research and participant may allow greater information processing, understanding, feedback, and encourage greater positive behavior change than solely an information exchange.
Beyond short-term intervention effects, few studies have examined the long-term maintenance of intervention effects, with existing literature having mixed results. In previous literature, the magnitude of observed educational intervention effects on carer burden tend to decrease over time.56,57 This may be due to the fact that carer burden, stress, and mental health are complex multidimensional phenomena, that may not be easily treated with educational interventions.37,39 Indeed, interventions with more psychosocial components appear to have a higher maintenance rate of effects; Vázquez et al58 were able to produce a significant reduction in major depressive episodes between the intervention groups and control groups 12 months after a cognitive-behavioral intervention for carers. In addition, the New York University Caregiver Intervention (NYUCI), a popular psychosocial intervention for dementia carers, has extensive evidence from several clinical randomized controlled trials demonstrating long-term (12 months post-intervention) reduction of depression symptoms in carers.59–61
We believe our study is unique in carer literature in that we are evaluating a workplace based intervention for carer-employees with carer-specific resources from multiple avenues, including workplace resources, as well as governmental and community resources. The workplace setting and composition of our sample, composed entirely of carer-employees, differs from other caregiving intervention research, as the context of the workplace and employment introduces additional nuances, such as work culture or supervisory relationships, that may complicate compliance with the intervention.
Despite this, our results indicated a tangible effect of the workplace intervention on carer-employee health outcomes, specific to self-report health, psychosocial health, and depression. Further research, such as modifying the intervention design to include counselling components and extending the time period, may be required to expand our findings. One potential adaptation particularly amendable to workplaces is the introduction of multi-level interventions, which calls for multiple targeted interventions at the individual and organizational levels.62
IMPORTANT IMPLICATIONS
Our findings affirm that our designed intervention may serve as an effective workplace accommodation tool for uptake by organizations to avert not only the clinical burden of caring but also protect employee health. While this study was not a clinical study, our findings may be useful for policy-makers, HR professionals, occupational health specialists, managers and employers, as our outcomes demonstrates effectiveness of an educational intervention at improving employee health, particularly mental health. The impact of such an intervention in the workplace is twofold: (1) employees’ health may be improved longitudinally, resulting in less sick days and reduced absenteeism and; (2) enhanced employer reputation, resulting in increased employee satisfaction, productivity, and retention as a result of reduced conflict between work and non-work.63,64 Our study is supportive of the estimations made in a prior paper estimating the economic effects of our intervention, where an analysis of different effectiveness scenarios proposed that our intervention may have saved the workplace between $48,010 to $676,657 CAD.10 While we did not evaluate work-related variables in this paper, our findings specific to intervention outcomes are encouraging, as increases in health outcomes are associated with work performance.65
The caregiving population is expected to increase in the coming years and is poised to become a dominant issue for employers. When supports for carers are inadequate, carer burden can progress into carer burnout, a serious mental health condition that can lead to deterioration in many facets of carer's lives, including paid work performance and health. Carer educational interventions in the workplace offer several unique advantages: (1) ability to reach large audiences at once, (2) utilization of existing infrastructure (HR staff, existing work policies) to augment interventions, and (3) benefit to the bottom line.
In the past, issues regarding childcare prompted employers to implement flexible work arrangements, and maternity/paternity leaves in order the keep the workforce healthy and aid their employees in maintenance of their multiple obligations.66 Similarly, eldercare issues should now receive the same attention and support from workplaces as our global population ages. We conclude that this intervention, an education resource for carer-employees, is a feasible and effective strategy for uptake by workplaces.
It is important that we underscore here that, although our intervention demonstrated substantive influence in reducing negative health outcomes, the nature of our recruitment strategies likely yielded high-interest carer-employees who were seeking and/or open to CFWP accommodations. While we have observed effectiveness of our designed intervention in a convenience sample of carer-employee participants in researcher-controlled conditions, we cannot make the same argument for the broader working environment. As the data collection points and intervention session were conducted one-on-one in-person, between the participants and researcher, it is possible that participants may have modified their behavior during these meetings. Additional studies could assess: reproducibility of results, barriers to implementation, and uptake of a standardized intervention in the work setting.
We recognize that this intervention study has a number of limitations, the foremost being the small sample size. Of the initial 43 participants at T1, only 21 participants remained by T3, creating only 21 sets of complete longitudinal data. Despite the power analysis and PCA, we are unable to determine if there were systemic or selection biases present in the population that left the study. Given the nature of the carer-employee role, our study targeted a population known for being highly stressed and over-burdened, leading to difficulties in recruitment and retention. It is possible that the participants engaged in our research are not representative of the whole carer population, as many highly burdened carers would likely not be able to join our study. Furthermore, those who withdrew from our study likely experienced high stress and work-life conflict, resulting in their departure. This may render fluctuation effects more pronounced in our analyses, and potentially skew our produced results.67 A further limitation includes the lack of a control group in our study to compare intervention results, which may lead to misidentification of random noise in our data.67 Lastly, our intervention study was conducted solely on university employees; further studies may need to be done to determine effectiveness of intervention protocols in different sectors and workplaces.
CONCLUSIONS
Carer-employees are a large and important segment of Canadian society, and given Canada's aging demographic, provide an innumerable service to their families as well as society. This underscores the need for recognition and support for CEs from a wider audience, including not only employers, but also public health and occupational health specialists. In our examination of the effects of the CFWP intervention, our current understanding is that the intervention was generally successful in decreasing negative health outcomes longitudinally in our population of university-employed carer-employees. This intervention can be considered effective in improving carer-employees overall health outcomes, such as self-reported health, psychosocial health, and depression, over time. Regardless, the limitations present in this study calls for the need to carry out similar types of studies with larger sample sizes and in different workplaces. Subsequent studies should focus on applicability of our results in other employment sectors, while identifying barriers to uptake within working environments.
Footnotes
This research was funded through a Canadian Institutes of Health Research (CIHR) Operating Grant (2014) MOP 137044. Additionally, this research is supported by the Canadian Institutes of Health Research (CIHR) program, and specifically Dr. Allison Williams – Chair in Gender, Work & Health, which examines Gender, Health and Caregiver Friendly Workplaces (CG1 1265885).
Conflicts of Interest: None declared.
Clinical Significance: This paper highlights the ability for workplaces to act as sources of support for the incoming influx of employed caregivers, as our population ages. Our paper displays potential for dissemination, by demonstrating that our educational intervention was successful at improving aspects of caregiver-employee psychosocial, general self-reported and depression symptoms.
REFERENCES
- 1.United Nations, World Population Ageing 2019 Highlights; 2019. Available at: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf. Accessed June 4, 2020. [Google Scholar]
- 2.Sinha M. Portrait of caregivers; 2012. Available at: https://www150.statcan.gc.ca/n1/pub/89-652-x/89-652-x2013001-eng.htm. Accessed August 8, 2018. [Google Scholar]
- 3.Williams AM, Tompa E, Lero DS, Fast J, Yazdani A, Zeytinoglu IU. Evaluation of caregiver-friendly workplace policy (CFWPs) interventions on the health of full-time caregiver employees (CEs): implementation and cost-benefit analysis. BMC Public Health 2017; 17:728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fast J. Caregiving for older adults with disabilities. Montreal, QC: IRPP; 2015. Available at: http://irpp.org/wp-content/uploads/2015/12/study-no58.pdf. Accessed August 8, 2018. [Google Scholar]
- 5.Bastawrous M. Caregiver burden—a critical discussion. Int J Nurs Stud 2013; 50:431–441. [DOI] [PubMed] [Google Scholar]
- 6.Hollander MJ, Liu G, Chappell NL. Who cares and how much. Healthc Quart 2009; 12:42–49. [DOI] [PubMed] [Google Scholar]
- 7.Statistics Canada. Fifty Years of Families in Canada: 1961 to 2011. Statistics Canada; 2012. Available at: https://www12.statcan.gc.ca/census-recensement/2011/as-sa/98-312-x/98-312-x2011003_1-eng.cfm. Accessed October 17, 2018. [Google Scholar]
- 8.Sacco LB, Leineweber C, Platts LG. Informal care and sleep disturbance among caregivers in paid work: longitudinal analyses from a large community-based Swedish cohort study. Sleep 2017; 41:zsx198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fast JE, Williamson DL, Keating NC. The hidden costs of informal elder care. J Fam Econ Issues 1999; 20:301–326. [Google Scholar]
- 10.Mofidi A, Tompa E, Williams A, Yazdani A, Lero D, Mortazavi SB. Impact of a caregiver-friendly workplace policies intervention: a prospective economic evaluation. J Occup Environ Med 2019; 61:461–468. [DOI] [PubMed] [Google Scholar]
- 11.Wagner DL, Lottes J, Neal M. The MetLife Caregiving Cost Study: Productivity Losses to US Business. 2006. [Google Scholar]
- 12.Ireson R, Sethi B, Williams A. Availability of caregiver-friendly workplace policies (CFWPs): an international scoping review. Health Soc Care Community 2018; 26:e1–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Govina O, Kotronoulas G, Mystakidou K, Katsaragakis S, Vlachou E, Patiraki E. Effects of patient and personal demographic, clinical and psychosocial characteristics on the burden of family members caring for patients with advanced cancer in Greece. Eur J Oncol Nurs 2015; 19:81–88. [DOI] [PubMed] [Google Scholar]
- 14.Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA 2014; 311:1052–1060. [DOI] [PubMed] [Google Scholar]
- 15.Gordon JR, Pruchno RA, Wilson-Genderson M, Murphy WM, Rose M. Balancing caregiving and work: role conflict and role strain dynamics. J Fam Issues 2012; 33:662–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andrén S, Elmståhl S. Relationships between income, subjective health and caregiver burden in caregivers of people with dementia in group living care: a cross-sectional community-based study. Int J Nurs Stud 2007; 44:435–446. [DOI] [PubMed] [Google Scholar]
- 17.Swinkels J, Tilburg TV, Verbakel E, Broese van Groenou M. Explaining the gender gap in the caregiving burden of partner caregivers. J Gerontol B Psychol Sci Soc Sci 2019; 74:309–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fast J, Lero D, DeMarco R, Ferreira H, Eales J. Combining care work and paid work: is it sustainable. Research on Aging, Policies and Practice. Edmonton: University of Alberta; 2014. Available at: http://www. rapp. ualberta. ca/en/∼/media/rapp/Publications/Documents/Combining_care_ work_and_paid_work_2014-09-16.pdf (accessed on November 24, 2019). [Google Scholar]
- 19.Vanier Institute of the Family. Facts and Stats: Families and Active Leisure in Canada (2017 Update); 2017. Available at: http://vanierinstitute.ca/category/publications/fact-sheets/?print=print-search. Accessed August 8, 2018. [Google Scholar]
- 20.Tal B, Mendes R. Who cares: The Economics of Caring for Aging Parents. CIBC; 2017. Available at: https://www.cibc.com/content/dam/pwm-public-assets/documents/pdfs/insights/who-cares-the-economics-of-caring-for-aging-parents-in-focus-en.pdf. Accessed August 8, 2018. [Google Scholar]
- 21.Grunfeld E, Coyle D, Whelan T, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ 2004; 170:1795–1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schulz R, Eden J. Families Caring for an Aging America. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 23.Van Ryn M, Sanders S, Kahn K, et al. Objective burden, resources, and other stressors among informal cancer caregivers: a hidden quality issue? Psychooncology 2011; 20:44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carers Trust. Caring About Older Carers; 2015. Available at: https://professionals.carers.org/sites/default/files/caring_about_older_carers.pdf. Accessed August 8, 2018. [Google Scholar]
- 25.Weitzner MA, Jacobsen PB, Wagner H, Friedland J, Cox C. The Caregiver Quality of Life Index–Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Qual Life Res 1999; 8:55–63. [DOI] [PubMed] [Google Scholar]
- 26.Chiao CY, Wu HS, Hsiao CY. Caregiver burden for informal caregivers of patients with dementia: a systematic review. Int Nurs Rev 2015; 62:340–350. [DOI] [PubMed] [Google Scholar]
- 27.Fast J, Lero D. Modern Caregiving in Canada. The Vanier Institute of the Family. Available at: http://vanierinstitute.ca/download/5186/. Accessed October 17, 2018. [Google Scholar]
- 28.Fast J, Dosman D. Monetizing the costs of eldercare-related employment consequences; 2014. Available at: http://www.rapp.ualberta.ca/en/∼/media/rapp/Publications/Documents/MonetizingCostsOfEldercareRelatedEmploymentConsequences_2014May21.pdf. Accessed October 17, 2018. [Google Scholar]
- 29.Ramesh S, Ireson R, Williams A. International synthesis and case study examination of promising caregiver-friendly workplaces. Soc Sci Med 2017; 177:52–60. [DOI] [PubMed] [Google Scholar]
- 30.Kelly K, Reinhard SC, Brooks-Danso A. Executive summary: professional partners supporting family caregivers. J Soc Work Educ 2008; 44: suppl: 5–15. [DOI] [PubMed] [Google Scholar]
- 31.Vuksan M, Williams A, Crooks V. Family friendly policies: accommodating end-of-life caregivers in workplaces. Int J Workplace Health Manag 2012; 5:4–14. [Google Scholar]
- 32.Government of Canada, Employment and Social Development Canada, Government of Canada. Employer Panel for Caregivers. When Work and Caregiving Collide: How Employers Can Support Their Employees Who Are Caregivers. 2015. [Google Scholar]
- 33.Centre for Families, Work & Well-Being, University of Guelph, Keating NC, Lero DS, Fast J, Lucas SJ, Eales J. A Framework and Literature Review on the Economic Cost of Care. 2013. [Google Scholar]
- 34.Knight BG, Lutzky SM, Macofsky-Urban F. A meta-analytic review of interventions for caregiver distress: recommendations for future research. Gerontologist 1993; 33:240–248. [DOI] [PubMed] [Google Scholar]
- 35.Brodaty H, Green A, Koschera A. Meta-analysis of psychosocial interventions for caregivers of people with dementia. J Am Geriatr Soc 2003; 51:657–664. [DOI] [PubMed] [Google Scholar]
- 36.Farran CJ. Family caregiver intervention research. J Gerontol Nurs 2001; 27:38–45. [DOI] [PubMed] [Google Scholar]
- 37.Sörensen S, Pinquart M, Duberstein P. How effective are interventions with caregivers? An updated meta-analysis. Gerontologist 2002; 42:356–372. [DOI] [PubMed] [Google Scholar]
- 38.Pinquart M, Sörensen S. Helping caregivers of persons with dementia: which interventions work and how large are their effects? Int Psychogeriatr 2006; 18:577–595. [DOI] [PubMed] [Google Scholar]
- 39.Acton GJ, Kang J. Interventions to reduce the burden of caregiving for an adult with dementia: a meta-analysis §. Res Nurs Health 2001; 24:349–360. [DOI] [PubMed] [Google Scholar]
- 40.Egan M, Bambra C, Thomas S, Petticrew M, Whitehead M, Thomson H. The psychosocial and health effects of workplace reorganisation. 1. A systematic review of organisational-level interventions that aim to increase employee control. J Epidemiol Community Health 2007; 61:945–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev 2014. CD002892. [DOI] [PubMed] [Google Scholar]
- 42.Post MW, Festen H, van de Port IG, Visser-Meily JM. Reproducibility of the Caregiver Strain Index and the Caregiver Reaction Assessment in partners of stroke patients living in the Dutch community. Clin Rehabil 2007; 21:1050–1055. [DOI] [PubMed] [Google Scholar]
- 43.Nijboer C, Triemstra M, Tempelaar R, Sanderman R, van den Bos GA. Measuring both negative and positive reactions to giving care to cancer patients: psychometric qualities of the Caregiver Reaction Assessment (CRA). Soc Sci Med 1999; 48:1259–1269. [DOI] [PubMed] [Google Scholar]
- 44.O’Malley KA, Qualls SH. Preliminary evidence for the validity and reliability of the caregiver reaction scale. Clin Gerontol 2017; 40:281–294. [DOI] [PubMed] [Google Scholar]
- 45.Huo T, Guo Y, Shenkman E, Muller K. Assessing the reliability of the short form 12 (SF-12) health survey in adults with mental health conditions: a report from the wellness incentive and navigation (WIN) study. Health Qual Life Outcomes 2018; 16:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cosco TD, Prina M, Stubbs B, Wu YT. Reliability and validity of the Center for Epidemiologic Studies Depression Scale in a population-based cohort of middle-aged US adults. J Nurs Measur 2017; 25:476–485. [DOI] [PubMed] [Google Scholar]
- 47.Lodder P. To Impute or not Impute: That's the Question. Advising on research methods: Selected topics. Huizen, The Netherlands: Johannes van Kessel Publishing; 2013. [Google Scholar]
- 48.McCulloch CE, Neuhaus JM. Generalized linear mixed models. Encyclopedia of Biostatistics 2005. 4. [Google Scholar]
- 49.Smith MK. Inappropriately Designating a Factor as Fixed or Random. [Google Scholar]
- 50.Explorable. Statistical Analysis; 2011. Available at: https://explorable.com/statistical-analysis. Accessed Feburary 3, 2019. [Google Scholar]
- 51.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York: Routledge; 2013. [Google Scholar]
- 52.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan 2006; 21:459–468. [DOI] [PubMed] [Google Scholar]
- 53.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography 2001; 38:115–132. [DOI] [PubMed] [Google Scholar]
- 54.Krishnan V. Constructing an Area-Based Socioeconomic Index: A Principal Components Analysis Approach. Edmonton, Alberta: Early Child Development Mapping Project; 2010. [Google Scholar]
- 55.Friesen CE, Seliske P, Papadopoulos A. Using principal component analysis to identify priority Neighbourhoods for health services delivery by ranking socioeconomic status. Online J Public Health Inform 2016; 8:e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Haley WE. Group intervention for dementia family caregivers: a longitudinal perspective. Gerontologist 1989; 29:478–480. [DOI] [PubMed] [Google Scholar]
- 57.Mittelman MS, Roth DL, Coon DW, Haley WE. Sustained benefit of supportive intervention for depressive symptoms in caregivers of patients with Alzheimer's disease. Am J Psychiatry 2004; 161:850–856. [DOI] [PubMed] [Google Scholar]
- 58.Vázquez FL, Torres Á, Blanco V, Otero P, Díaz O, Ferraces MJ. Long-term follow-up of a randomized clinical trial assessing the efficacy of a brief cognitive-behavioral depression prevention intervention for caregivers with elevated depressive symptoms. Am J Geriatr Psychiatry 2016; 24:421–432. [DOI] [PubMed] [Google Scholar]
- 59.Mittelman MS, Bartels SJ. Translating research into practice: case study of a community-based dementia caregiver intervention. Health Aff (Millwood) 2014; 33:587–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mittelman MS, Ferris SH, Shulman E, et al. A comprehensive support program: effect on depression in spouse-caregivers of AD patients. Gerontologist 1995; 35:792–802. [DOI] [PubMed] [Google Scholar]
- 61.Gaugler JE, Reese M, Mittelman MS. Effects of the Minnesota adaptation of the NYU caregiver intervention on depressive symptoms and quality of life for adult child caregivers of persons with dementia. Am J Geriatr Psychiatry 2015; 23:1179–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cleary PD, Gross CP, Zaslavsky AM, Taplin SH. Multilevel interventions: study design and analysis issues. J Natl Cancer Inst Monogr 2012; 2012:49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Richman AL, Civian JT, Shannon LL, Jeffrey Hill E, Brennan RT. The relationship of perceived flexibility, supportive work–life policies, and use of formal flexible arrangements and occasional flexibility to employee engagement and expected retention. Commun Work Fam 2008; 11:183–197. [Google Scholar]
- 64.Beauregard TA, Henry LC. Making the link between work-life balance practices and organizational performance. Hum Resourc Manag Rev 2009; 19:9–22. [Google Scholar]
- 65.Ford MT, Cerasoli CP, Higgins JA, Decesare AL. Relationships between psychological, physical, and behavioural health and work performance: a review and meta-analysis. Work Stress 2011; 25:185–204. [Google Scholar]
- 66.Boswell WR, Olson-Buchanan JB. The use of communication technologies after hours: the role of work attitudes and work-life conflict. J Manag 2007; 33:592–610. [Google Scholar]
- 67.Hackshaw A. Small studies: strengths and limitations. Eur Respir J 2008; 32:1141–1143. [DOI] [PubMed] [Google Scholar]


