Abstract
Health disparity refers to systematic differences in health outcomes between groups and communities based on socioeconomic isolation. In the USA, health disparities among minority groups, especially African Americans, limit their access to quality medical care and other beneficial resources and services. Presently, the novel coronavirus (COVID-19) highlights the extreme healthcare challenges that exist in the African American and other minority communities in the USA. African Americans are dying at a rate nearly four times higher than the national average. With inadequate access to quality healthcare, viable resources, and information, COVID-19 will continue to have a disastrous effect on African American communities. This communication provides a brief overview of the health inequalities resulting in African Americans dying disproportionately during the COVID-19 pandemic.
Keywords: African American, Coronavirus, Health disparity, Socioeconomic
Introduction
The novel coronavirus (COVID-19) emerged from Wuhan, China, in late 2019 and quickly became a global pandemic that has already affected more than 115 countries and territories [1]. In symptomatic patients, this highly transmissible disease causes severe acute respiratory syndrome, which infects lower respiratory airways and results in fatal pneumonia. The effect of this pandemic is widely visible, resulting in about a 5.6% mortality rate and causing major economic and social devastations [2]. Studies have shown that COVID-19 is transmitted via human interactions when uninfected individuals come in contact with mucus and respiratory droplets or surfaces that contain the virus. On surfaces where it is present, the virus can remain infectious from 2 hours and up to 9 days depending on the surface materials. Also, it can remain airborne for up to 3 hours post aerosolization [3]. Furthermore, a small majority of carriers develop mild to no symptoms. As a result, transmission occurs rapidly and inconspicuously with both symptomatic and asymptomatic individuals unknowingly transmitting the virus, resulting in more people being infected. Research data continues to show that COVID-19 affects all age groups. Older individuals and those with underlying health conditions are more prone to experiencing severe illnesses and death. Data analysis of COVID-19 from the USA highlights pre-existing health disparities among African Americans as the potential cause of poor prognosis. Based on reports from National Health Care disparities, in comparison with non-Hispanic whites, African Americans have a 44% greater chance of dying from stroke, 20% more likely to have asthma, 25% more likely to have heart disease, 72% more likely to have diabetes, and 23% more likely to be obese [4]. This is a major concern that government and public health officials should address as it has been shown that in 21 out of 30 states reporting data, black people accounted for a higher share of COVID-19 cases than their share in the population [5]. In 19 out of 24 states, they accounted for a higher share of deaths than their share of the total population [5]. In such regard, an immediate plan of action is urgently needed to address and mitigate the effects of health disparities. This communication briefly examines the health disparities among African Americans in the USA during the COVID-19 pandemic.
Racial and Demographic Analysis of COVID-19
In the early phase of the outbreak in the USA, access to testing was limited to government officials, celebrities, and a selected number of healthcare workers—symptomatic or asymptomatic. It was not until 18 March 2020 when the federal government passed the Families First Coronavirus Response Act (FFCRA), which allows free COVID-19 testing for all individuals [6], that large-scale testing became available nationwide. While FFCRA is a great response for all citizens, the lack of testing remains, especially in minority communities.
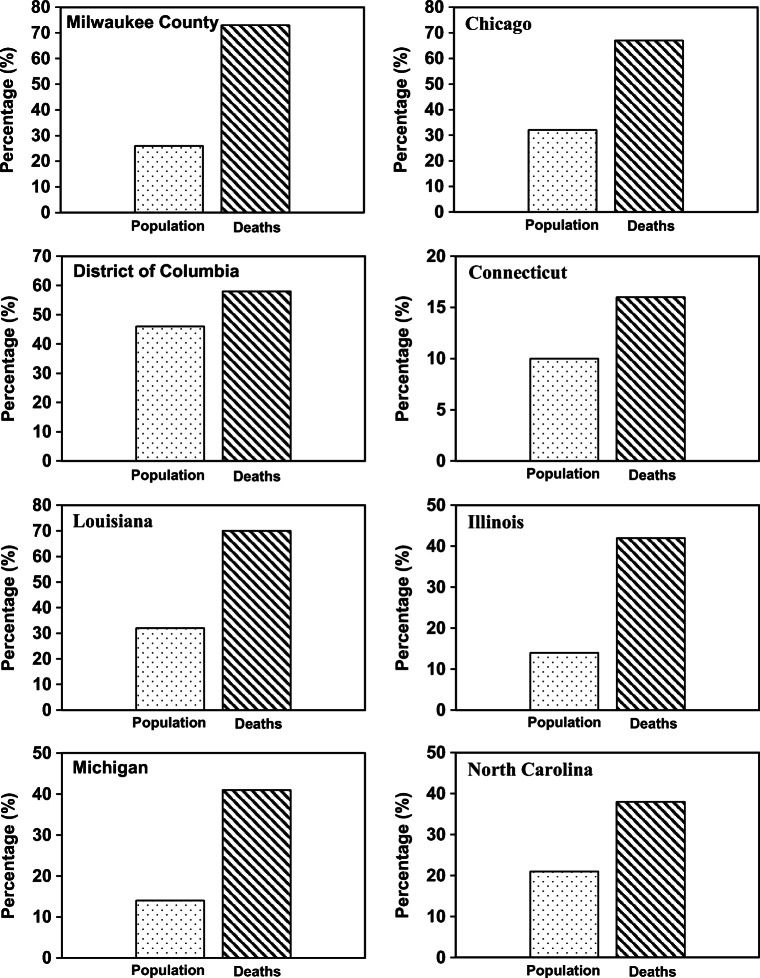
In the USA, the racial breakdown of COVID-19 cases and deaths is now starting to be made available. In Louisiana, where 32% of its population is African American [7], 70% of deaths—as a result of the novel coronavirus—are among African Americans. Meanwhile, white Americans in Louisiana account for 62% of the population but recorded only 28% of COVID-19 deaths [8]. Of the 380 COVID-19 deaths in Illinois [9], the percentage of deaths among black Americans (43%) is higher compared with those among whites (36%), Hispanics (8.4%), Asians (3.7%), and others (6.8%). This is an area where the majority of the population is white (77%) and the black population is about 15%. The same phenomenon is occurring in Michigan [10]; the black population is about 14% but accounted for 40% of COVID-19 deaths. In New York, both Hispanics and African Americans are dying at a relatively higher rate in comparison with other ethnic groups. They account for 29% and 22% of New York’s population, respectively. However, the reported death toll [11] for Hispanics and African Americans is 34% and 28%, respectively. In Connecticut, the black population is about 10%, but represents more than 16% of COVID-19 deaths [12, 13]. In Milwaukee County, the black population is about 26% but represents 77% of COVID-19 deaths [14, 15]. In North Carolina, 49% of deaths are among African Americans, who represent 21% of the total population [16]. The trend and commonality transcend state lines. The common denominator for the high mortality rate in all these states is race and ethnic background. Of note, all data presented in this communication and Fig. 1 are subject to change as more data becomes available. For more up-to-date data, refer to the States Department of Public Health and Services.
Fig. 1.
Percent of population and percentage of COVID-19 deaths among black Americans in various jurisdictions. Sources in text
Health Disparities
A recent study showed that in zip codes with high numbers of unemployed and uninsured residents, fewer test kits were available [17, 18]. Most of those zip codes have disproportionate numbers of African Americans. It is no surprise that underserved communities such as the African American communities would also have less access to COVID-19 test kits in a time that kits are scarce.
Assuming that African Americans are seeking medical attention for COVID-19, they will most likely do so at minority-serving institutions which already have [19]:
-
(i)
Lower quality care due to low budgets and lack of resources
-
(ii)
Shortage of critical care physicians
-
(iii)
Inadequate number of medical supplies and equipment (i.e., personal protective equipment and ventilators for critically ill patients).
This is in parallel to years of ongoing racial and socioeconomic discrimination in the USA [20, 21]. While a series of landmark court cases such as Simkins v Moses H. Cone Memorial Hospital (1963) and Cypress v Newport News Hospital Association (1967) litigated by the National Association for the Advancement of Colored People (NAACP) Legal Defense and Education Fund took legal actions against racial policies and discriminations in healthcare, the challenges for quality healthcare for African Americans remain [22]. The pursuit of legal strategies against racist policies was an essential element in a national campaign to eliminate discrimination in healthcare delivery in the USA.
As COVID-19 cases and related deaths continue to rise in the USA, data demonstrates that African American communities in various cities are the most affected (Fig. 1). This is a challenge that the federal government and its COVID-19 task force have pointed out. However, in a White House press briefing, Dr. Anthony Fauci of the National Institute of Allergy and Infectious Diseases recently expressed, “…there is nothing we [the federal government] can do about it [COVID-19] right now except to give them [African Americans] the best possible care to avoid complications.”
Health disparities and institutional racism [20, 21, 23–27] make the COVID-19 pandemic worse for African Americans. There are studies on the effects of stress and health for African Americans as stress can increase vulnerability, which in turn is a factor in determinants of health disparities. Perceived discrimination can add to stress, which increases vulnerability to the health effects of environmental hazards, thus adding to health disparities. Harburg et al. highlighted that darker-skinned black men having racist interactions and living in neighborhoods with high rates of social instability have an increased risk and incidence of stressful experiences in daily life, which in turn increases their likelihood of high blood pressure along with other health conditions they are predisposed to from their environment [28]. Conditions resulting from these conditions are listed as risk factors for more severe COVID-19 cases [29].
Constant streams of statistical data (Fig. 1) about the novel coronavirus are showing that African Americans are dying from COVID-19-related complications at a disproportionately higher rate than other ethnic and racial groups. Racial inequities in healthcare institutions, lack of access to information, higher levels of preventable chronic diseases (i.e., diabetes, asthmas, hypertension, etc.), and COVID-19 testing not being widely available in minority communities are among the many factors resulting in African Americans dying at disproportionate numbers during this pandemic [30]. Failure to rapidly test and segregate individuals infected with COVID-19 can result in major chain-of-transmission reactions and deaths.
COVID-19 and Socioeconomic Stratification
The socioeconomic discrimination has confined African Americans to overpopulated housing estates (ghettos) and low-wage jobs. From the very genesis of this country, African Americans have always been the essential or sacrificial workers used to ensure the continuity of this economy. From centuries of free slave labor to years of sharecropping to low-paying domestic jobs, African Americans have always played a role in shaping the very essence of what America is [31, 32]. Today, a large number of African Americans work in retail, home healthcare, mass transit, plant factories, and prisons/jails where social distancing is almost impossible. As a result, African Americans became more vulnerable to the disease combined with inadequate access to proper healthcare in their communities [13].
Preventative Measures and Challenges
In many cities in the USA, stay-at-home orders are placed to mitigate the spread of the virus. This is a great effort, which has shown promising results. However, African Americans and other minority groups account for 68% of the US homeless population [33]. These individuals stand no chance against the trail of devastation that COVID-19 will leave behind since it is almost impossible for them to follow preventative guidelines issued by the Centers for Disease Control and Prevention (CDC) and government officials. To help flatten the curve, many doctors, nurses, and other healthcare professionals from non-profit organizations are volunteering their services to the homeless community. Among other preventative measures highlighted by the CDC as well as healthcare and government officials is the use of face masks in public settings. While this effort can limit and reduce the spread of COVID-19, this could pose a challenge to African Americans and other minorities as they are more likely to be criminalized based on their appearances while wearing masks.
Of note, many individuals have failed to understand the zoonotic origin of COVID-19 [34–37]. As a result, significant misinformation and conspiracy theories continue to circulate on the web and social media. While the Internet is an open platform to share and access information, individuals should be aware of conspiracy theories and follow credible sources for relevant information. While there is no evidence showing a correlation between COVID-19 and the upcoming fifth-generation (5G) technology, people continue to share misinformation linking the current pandemic to 5G technology. Initially, there was the belief that black individuals and minorities were not susceptible to being infected with the virus. There is no available research showing that black individuals are biologically and genetically immune to the virus. Without proper information, these artificial assumptions can usher individuals into disastrous directions.
COVID-19 and Black Migrants
On a global scale, COVID-19 is not only affecting people of African descent in the USA but across the world. Minority groups everywhere are harassed and discriminated against during this pandemic. In China where the virus emerged, Africans living in Guangzhou are being evicted from their homes as the virus sparked fear and racial discrimination. Of equal challenges, minorities and migrant workers from Caribbean countries, such as Haiti, living in the USA are being detained by the Immigration and Customs Enforcement (ICE) at detention centers where the virus is uncontrollable. These Haitians—some of whom are infected with or are COVID-19 carriers—are subjected to deportation to their native land of Haiti, a country with a very weak public healthcare system [38]. Only a few examples are highlighted here; a comprehensive analysis is underway. Altogether, African Americans and individuals of African descent are more vulnerable to the impact of the virus.
African American Distrust in the Healthcare System
It is no secret that the US government has misguided and often used African Americans as guinea pigs for medical research. During the time of slavery, psychologists and doctors deemed it a disease for slaves to long for freedom or want to “run away.” Runaway slaves were diagnosed with what was called “drapetomania,” which was considered, at the time, a mental illness that amplifies the desire to become a fugitive–run away [32]. Furthermore, after slaves were freed, many American doctors continued to argue that former slaves were incapable of thriving as free members of society because their minds could not function beyond the established orders of slavery.
Among many other diseases, the syphilis outbreak in the south highlighted another dark chapter in African Americans’ relations with the healthcare system in America. Many African Americans infected with syphilis were promised treatment from the Public Health Department. Instead, those patients were denied treatment and turned into “guinea pigs” to monitor the progression of the disease. The patients were unaware and were lied to repeatedly about their conditions. Many of those untreated “guinea pigs” of the syphilis experiment infected their wives and other women they had gotten in contact with. Furthermore, many of them had unknowingly fathered children born with congenital syphilis. The syphilis experiment lasted for 40 years, and it was a major ethical violation. The US government had broken its laws and experimented on its citizens. The US Public Health Service did not treat the people who were experimented on even after penicillin—the effective cure for the disease—was made available. Historically, this injustice has established a certain level of distrust among African Americans in the US public health system; therefore, they are more reluctant in seeking routine preventative care [39].
The time for a healthcare revolution for African Americans is long overdue. This is not a surprise, as 100 years ago, the 1918 flu pandemic highlighted the racial bias and distrust that existed in the medical community [40, 41]. Jim Crow laws and pseudoscientific theories made the impact of the flu go unnoticed in black communities. All efforts and resources were made available to white communities as physicians believed that the virus only affected white individuals. Many healthcare officials, with no reliable scientific evidence, believed that African Americans were not susceptible to the flu as the linings of their “big noses” were resistant to the microorganism that affects the respiratory system. As a result, black communities were forced to battle the 1918 flu pandemic on their own, using limited resources and inadequate medical care at segregated healthcare institutions [41]. The current COVID-19 pandemic reflects a mirror image of the 1918 flu pandemic for African Americans and other minorities in the USA [40]. Such patterns will possibly continue if the socioeconomic, health disparities, and the dividing racial lines stretch to upcoming generations.
Discussion and Approach
Other jurisdictions have yet to publicly report their data based on race and ethnicity; regardless, the challenges remain from social and economic factors that drive health outcomes. Altogether, African Americans are dying at a much higher rate compared with any other ethnic group. Due to various factors that affect health outcomes, a plan of action is urgently needed to respond to the challenges of this pandemic and any health threats in African American communities [42]. Access to testing and proper medical treatment is necessary to ensure the safety of African Americans, the most vulnerable group. The embedded racism in the healthcare system and the socioeconomic and health disparities [25, 27] continue to make the effect of the virus worst—for black Americans and other minorities in the USA. Overall, the lack of testing made available to the black community for COVID-19, the continuous poor healthcare system for African Americans, and the systematic health disparity are what makes this virus more dangerous to African Americans; although COVID-19 is a new pandemic, it is deeply rooted in history in the continuous plight of African Americans in this country [13]. It is an unsettling reality for African Americans to rely on the same systems that historically inflicted harm and damage on them to protect and serve them against this virus [31, 32, 43].
More research is needed to understand the source of exposure to COVID-19 for African Americans as well as a plan of care and health outcomes of African Americans in various zip codes. Further research can also shed light into the type of facilities a majority of African Americans receive care in, such as nursing homes, and assess their preparedness looking into their access to resources such as personal protective equipment (PPE) during the COVID-19 pandemic, current and past documented deficiencies from state surveys, and infection control measures taken during COVID-19, and overall health outcome. More research is also needed to understand how the environment affects health outcome or the severity of COVID-19 cases in terms of environmental exposures, social, and economic factors that can affect mortality, morbidity, life expectancy, healthcare expenditures, and health status amidst the COVID-19 pandemic. This is relevant since a recent study found that living in areas with high air pollution is associated with an 8% increase in the COVID-19 death rate [44].
Black leaders in all communities, historically black colleges and universities (HBCUs), and minority-serving institutions (MSIs) should continue to engage and educate students to respond to the needs of their communities. This will require these institutions to reinvent and alter their curriculums to provide more health and medical programs (including medical history), engineering, science, and technology. Currently, these institutions are operating with low resources, many are underfunded, and others are on the verge of being permanently closed. This is very unfortunate for African Americans and other minority communities especially when analyzing the impact of COVID-19. As the pandemic forced all teaching to be done remotely, HBCUs’ and MSIs’ students and institutions are at higher risks of not being able to satisfy their educational needs [45]. Many have limited to no access to technological devices and reliable Internet access to fully respond to the spontaneous remote teaching caused by the effect of the virus.
Conclusion
The gravity of the novel coronavirus COVID-19 (SARS-CoV-2) pandemic is yet another event showing the racialized health inequalities that exist in the USA. African Americans have systematically experienced the worst health outcomes compared with any other racial and ethnic group in the USA. The burdens of COVID-19 are much greater among minorities living in low-income communities where access to quality healthcare and other relevant needs is scarce. The health disparities in the USA did not start with the COVID-19 pandemic. However, the virus has significantly highlighted the pre-existing racial inequalities.
Altogether, the socioeconomic status and the well-being of African Americans require intervention and significant improvement is needed. This will require mutual inclusions of community leaders from various organizations (i.e., churches, Divine Nine Organizations: Fraternities and Sororities), local government, policymakers, and researchers to mend healthcare in low-income communities.
Acknowledgments
Thanks are due to Miriame Etienne, Ruthonce Stvil Louis-Jean, Isaiah Herbert, and Magdonald Aimé for their feedback.
Data Availability
All materials and data used in this communication are publicly available and are cited throughout the text.
Compliance with Ethical Standards
Ethics Approval and Consent
Ethical approval or consent was not applicable for this paper.
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.a. Coronavirus Disease 2019 (COVID-19) Situation Report–77 [Internet]. World Heal. Organ. 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200406-sitrep-77-covid-19.pdf?sfvrsn=21d1e632_2. b.Coronavirus Disease 2019 (COVID-19) Situation Report – 133 [Internet]. World Heal. Organ. 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200601-covid-19-sitrep-133.pdf?sfvrsn=9a56f2ac_4.
- 2.Louis-Jean J, Aime M. On the novel coronavirus (COVID-19): a global pandemic. J Teknol Lab. 2020;9:103–14. 10.29238/teknolabjournal.v9i1.230.
- 3.Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246–51. https://linkinghub.elsevier.com/retrieve/pii/S0195670120300463. [DOI] [PMC free article] [PubMed]
- 4.Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National Surveillance of Asthma: United States, 2001-2010. Vital Heal Stat 3. 2012:1–58. http://www.ncbi.nlm.nih.gov/pubmed/24252609. [PubMed]
- 5.Artiga S, Orgera K, Pham O, Corallo B. Growing data underscore that communities of color are being harder hit by COVID-19 [Internet]. Kaiser Fam. Found. 2020. https://www.kff.org/coronavirus-policy-watch/growing-data-underscore-communities-color-harder-hit-covid-19/?utm_campaign=KFF-2020-Medicaid&utm_source=hs_email&utm_medium=email&utm_content=86645517&_hsenc=p2ANqtz%2D%2DRBk58ZkW7WUKTgP6RM7OlSdkJW5McG2Mkh6AAb_kfx.
- 6.Families First Coronavirus Response Act. United States of America: U.S. Government Publishing Office. 2020 p. 177–220.
- 7.Louisiana Population 2020 (Demographics, Maps, Graphs). World Popul. Rev. 2020. https://worldpopulationreview.com/states/louisiana-population/.
- 8.Coronavirus (COVID-19). Louisiana State Dep. Heal. 2020. http://ldh.la.gov/Coronavirus/.
- 9.Coronavirus Disease 2019 (COVID-19) in Illinois test results. Illinois State Dep. Public Heal. 2020. http://dph.illinois.gov/covid19/covid19-statistics.
- 10.Michigan Data. Michigan State Dep. Public Heal. 2020. https://www.michigan.gov/coronavirus/0,9753,7-406-98163_98173---,00.html.
- 11.Fatalities. New York State Dep. Public Heal. 2020. https://covid19tracker.health.ny.gov/views/NYS-COVID19-Tracker/NYSDOHCOVID-19Tracker-Fatalities?%3Aembed=yes&%3Atoolbar=no&%3Atabs=n.
- 12.COVID-19 Update April 09, 2020. Connect. State Dep. Public Heal. 2020. https://portal.ct.gov/-/media/Coronavirus/CTDPHCOVID19summary4092020.pdf?la=en.
- 13.Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Heal Disparities. 2020; 10.1007/s40615-020-00756-0. [DOI] [PMC free article] [PubMed]
- 14.COVID-19: County Data. Wisconsin State Dep. Heal. Serv. 2020. https://www.dhs.wisconsin.gov/covid-19/county.htm.
- 15.Outbreaks in Wisconsin. Wisconsin State Dep. Heal. Serv. 2020. https://www.dhs.wisconsin.gov/outbreaks/index.htm.
- 16.COVID-19 North Carolina Dashboard. North Carolina State Div. Public Heal. 2020. https://www.ncdhhs.gov/divisions/public-health/covid19/covid-19-nccase-count#by-race/ethnicity.
- 17.Taylor K-Y. The Black Plague. New Yorker. 2020. https://www.newyorker.com/news/our-columnists/the-black-plague.
- 18.Reid A. Coronavirus Philadelphia: positive tests higher in poorer neighborhoods despite six times more testing in higher-income neighborhoods, researcher says. CBS Philly. 2020. https://philadelphia.cbslocal.com/2020/04/06/coronavirus-philadelphia-positive-tests-higher-in-poorer-neighborhoods-despite-six-times-more-testing-in-higher-income-neighborhoods-researcher-says/.
- 19.Danziger J, de la Hoz MÁA, Li W, Komorowski M, Deliberato RO, Rush BNM, et al. Temporal trends in critical care outcomes in U.S. minority-serving hospitals. Am J Respir Crit Care Med. 2020;201:681–7. [DOI] [PMC free article] [PubMed]
- 20.Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Heal Soc Behav 2010;51:S28–S40.10.1177/0022146510383498. [DOI] [PubMed]
- 21.Giles WH, Tucker P, Brown L, Crocker C, Jack N, Latimer A, et al. Racial and ethnic approaches to community health (REACH 2010): an overview. Ethn Dis. 2004;14:S5–8. http://www.ncbi.nlm.nih.gov/pubmed/15682765. [PubMed]
- 22.Reynolds PP. Professional and hospital discrimination and the US Court of Appeals Fourth Circuit 1956–1967. Am J Public Heal. 2004;94:710–720. 10.2105/AJPH.94.5.710. [DOI] [PMC free article] [PubMed]
- 23.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Heal Soc Behav. 1995:80–94. http://www.ncbi.nlm.nih.gov/pubmed/7560851. [PubMed]
- 24.Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis. 1992;2:207–21. http://www.ncbi.nlm.nih.gov/pubmed/1467758. [PubMed]
- 25.Giles WH. The US perspective: lessons learned from the Racial and Ethnic Approaches to Community Health (REACH) Program. J R Soc Med. 2010;103:273–276. 10.1258/jrsm.2010.100029. [DOI] [PMC free article] [PubMed]
- 26.Cooper RS, Freeman VL. Limitations in the use of race in the study of disease causation. J Natl Med Assoc. 1999;91:379–83. http://www.ncbi.nlm.nih.gov/pubmed/10643209. [PMC free article] [PubMed]
- 27.Kaufman JS, Cooper RS. Seeking causal explanations in social epidemiology. Am J Epidemiol. 1999;150:113–120. 10.1093/oxfordjournals.aje.a009969. [DOI] [PubMed]
- 28.Harburg E, Erfurt JC, Hauenstein LS, Chape C, Schull WJ, Schork MA. Socio-ecological stress, suppressed hostility, skin color, and black-white male blood pressure: Detroit. Psychosom Med. 1973;35:276–96. http://journals.lww.com/00006842-197307000-00003. [DOI] [PubMed]
- 29.Chow N, Fleming-Dutra K, Gierke R, Hall A, Hughes M, Pilishvili T, et al. Preliminary estimates of the prevalence of selected underlying health conditions among patients with Coronavirus Disease 2019 — United States, February 12–March 28, 2020. Morb Mortal Wkly Rep [Internet]. 2020;69:382–6 (Available from: http://www.cdc.gov/mmwr/volumes/69/wr/mm6913e2.htm?s_cid=mm6913e2_w). [DOI] [PMC free article] [PubMed]
- 30.Cunningham TJ, Croft JB, Liu Y, Lu H, Eke PI, Giles WH. Vital signs: racial disparities in age-specific mortality among blacks or African Americans — United States, 1999–2015. MMWR Morb Mortal Wkly Rep. 2017;66:444–56. [DOI] [PMC free article] [PubMed]
- 31.McGuire DL. At the dark end of the street: black women, rape, and resistance—a new history of the civil rights movement from Rosa parks to the rise of black power. Knopf Publishing Group. 2010.
- 32.Franklin JH, Higginbotham E. From slavery to freedom: a history of African Americans. 9th ed: McGraw-Hill; 2010.
- 33.Who is Homeless? Natl. Coalit. Homeless. 2009. https://web.archive.org/web/20100414172730/http://nationalhomeless.org/factsheets/who.html.
- 34.Salata C, Calistri A, Parolin C, Palù G. Coronaviruses: a paradigm of new emerging zoonotic diseases. Pathog Dis. 2019;77. 10.1093/femspd/ftaa006/5739327. [DOI] [PMC free article] [PubMed]
- 35.York A. Novel coronavirus takes flight from bats? Nat Rev Microbiol. 2020;18:191–191. http://www.nature.com/articles/s41579-020-0336-9. [DOI] [PMC free article] [PubMed]
- 36.Wong S, Lau S, Woo P, Yuen K-Y. Bats as a continuing source of emerging infections in humans. Rev Med Virol. 2007;17:67–91. 10.1002/rmv.520. [DOI] [PMC free article] [PubMed]
- 37.Chen L, Liu B, Yang J, Jin Q. DBatVir: the database of bat-associated viruses. Database (Oxford). 2014;2014:bau021. 10.1093/database/bau021. [DOI] [PMC free article] [PubMed]
- 38.Louis-Jean J, Cenat K, Sanon D, Stvil R. Coronavirus (COVID-19) in Haiti: a call for action. J Community Heal. 2020;45:437–439. 10.1007/s10900-020-00825-9. [DOI] [PMC free article] [PubMed]
- 39.Alsan M, Wanamaker M. Tuskegee and the health of black men. Q J Econ. 2018;133:407–55. http://www.ncbi.nlm.nih.gov/pubmed/30505005. [DOI] [PMC free article] [PubMed]
- 40.Gamble VN. “There Wasn’t a lot of comforts in those days:” African Americans, public health, and the 1918 influenza epidemic. Public Heal Rep. 2010;125(Suppl):113–22. http://www.ncbi.nlm.nih.gov/pubmed/20568573. [PMC free article] [PubMed]
- 41.Jones MM, Saines M. The Eighteen of 1918–1919: Black Nurses and the Great Flu Pandemic in the United States. Am J Public Heal. 2019;109:877–84. 10.2105/AJPH.2019.305003. [DOI] [PMC free article] [PubMed]
- 42.Yancy CW. COVID-19 and African Americans. JAMA. 2020. https://jamanetwork.com/journals/jama/fullarticle/2764789. [DOI] [PubMed]
- 43.Gupta S. Why African-Americans may be especially vulnerable to COVID-19. Sci News. 2020. https://www.sciencenews.org/article/coronavirus-whyafrican-americans-vulnerable-covid-19-health-race.
- 44.Wu X, Nethery RC., Sabath BM., Braun D, Dominici F. Exposure to air pollution and COVID-19 mortality in the United States: a nationwide cross-sectional study. MedRxiv. 2020. 10.1101/2020.04.05.20054502v2. [DOI] [PMC free article] [PubMed]
- 45.Louis-Jean J, Cenat K. Beyond the face-to-face learning: a contextual analysis. Pedagog Res. 2020;5. 10.29333/pr/8466.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All materials and data used in this communication are publicly available and are cited throughout the text.