Abstract
Background
Workplace bullying (WPB) refers to any form of repeated and unreasonable verbal, physical or sexual harassment that an employee endures by a person or a group. In healthcare settings, practitioners are occasionally victims of WPB incidents. The aim of this study was to survey victims of WPB and determine factors associated with being a victim of WPB at a multiregional health care facility in Saudi Arabia.
Methods
This cross-sectional study was conducted in 2018, by distributing a self-administered questionnaire via a private electronic mail to all fulltime healthcare practitioners within a multi-regional hospital in Saudi Arabia. Healthcare practitioners included physicians, nurses, allied healthcare professionals and pharmacists who reported being exposed to WPB in the past year. Study outcomes were the prevalence rate ratio of WPB and its associated factors, such as victim, perpetrator and incident characteristics.
Results
WPB has been reported by 684 participants. Perpetrators were mainly patients (36.1%), their families/relatives (29.5%), and hospital staff (27.2%) or managers/supervisors (7.2%). The type of WPB incident was mostly verbal abuse (98.1%) followed by physical harassment (11.8%) and sexual connotations (5.8%). WPB was 30% more prevalent among younger nurses and 24% less prevalent among higher educated nurses compared to their counter groups, P<0.001 each. Among technicians and administrative employees, WPB was 54% more prevalent among females, 36% more prevalent among the younger group, and 25% more prevalent among expatriate workers compared to their counter groups P<0.014, P<0.001 and P=0.017, respectively. WPB was 20% less prevalent among higher educated allied health professionals, P=0.002. Among physicians, WPB was 33% more prevalent among females, P=0.041 and was 47% more prevalent among higher educated physicians compared to their counter groups, P=0.018.
Conclusion
WPB might occur any time, anywhere and by any person within health care facilities. The prevalence of WPB varies within health occupational groups. Gender, age, educational level, and nationality were significantly associated factors with WPB.
Keywords: nurse, physician, pharmacist, bullying, verbal, physical, sexual
Background
Workplace Bullying (WPB) is generally known as a repeated and unreasonable mistreatment by a person or a group.1 WPB exemplifies itself in various forms such as verbal, physical or sexual harassment.2 The operational definition of bullying is a situation where one or several individuals, persistently and over a period of time are exposed to negative actions from one or several persons.3 Its prevalence varies across different industries all over the world, as some occupations, face a greater risk of exposure than others.4 Healthcare workers are occasionally victims of workplace hostility. For instance, in the United States, the rates of physical mistreatment against physicians and nurses were 16.2 per 1,000 and 21.9 per 1,000 employees, respectively.5 Furthermore, around 34.5% of emergency practitioners experience physical mistreatment, 71.6% of them encounter verbal abuse, and 44.4% report being bullied annually in one Iranian medical center.6 Apparently, WPB occurs because of a triad that constitutes a vulnerable victim, a bystander and a non-deterred perpetrator.7
WPB among healthcare practitioners varies in its prevalence and characteristics across and within countries.8 In the European Union, 52% of the victimized healthcare employees have experienced bullying at work.9 Among US surgeons, one report showed that 40% of both residents and faculty reported being bullied, while 54.3%–58.5% witnessed a bullying incident.3 One study examining 3,700 respondents showed that 47% of physicians were bullied by other physicians, 29% by administrators, non-medical personnel, or patients, 17% by nurses, 4% by medical residents and fellows and 1% by medical students.10
Many experts view bullying as a direct reflection of misused power of the traditional hierarchy that exists in many healthcare organizations.9 For example, individuals with authority are often the perpetrators who bully their subordinates, solely driven by the virtue of their position.11 In addition, the absence of stringent laws and policies sometimes make employers pay less attention to prevent it.12 In a systematic review paper, WPB was a predictor of various mental health problems and sleep disturbances,13 yet sadly, about 29% of victims remain silent about their WPB experience.14 However, the most serious form of socioeconomic consequences of WPB is when practitioners who try to stop it voluntarily decide to leave their job.15 Unfortunately, WPB in healthcare settings affects teamwork, jeopardizes its integrity,11 and negatively affects patients’ safety and quality of care.16 Intimidating and disruptive behaviors associated with WPB fuel medical errors and lead to adverse outcomes.16,17 In addition to being a dramatic threat to patient safety,18 WPB weakens staff morale and increases absenteeism, leading to higher turnover rates of qualified staff.19
Although several studies have extensively examined the prevalence and characteristics of WPB, it is unfortunate that this phenomenon has not been addressed sufficiently in some Middle Eastern settings. For instance, in Saudi Arabia, studies on WPB are few, which leaves numerous gaps in the body of knowledge.16 The Saudi Arabian community is distinctive compared to Western settings, in terms of race and ethnicity, with deeply rooted traditions framed by tribal bounds and religious constraints.20 The Saudi Arabian health industry is in high demand for international expatriates, and hospitals in this region employ healthcare practitioners from all over the world.21 In addition to the rules and regulations that ban WPB, the culture and religion supposedly create further restraints on harming other individuals. On the other hand, victims of WPB in such settings might under report such unfortunate events, driven by the fear of being laid off.22 Therefore, it is imperative for different healthcare settings to detect any case of WPB, to analyze its characteristics and to determine high-risk work environments. The aim of this study was to survey victims of WPB and determine factors associated with being a victim of WPB at a multiregional health care facility in Saudi Arabia.
Methods
Study Design and Setting
This was a cross-sectional correlation study based on an anonymous self-reported survey. It is the second part of a project and a follow-up paper to a previous publication that determined to what extent healthcare practitioners worry about WPB and whether it affects the quality of care and patient safety from their perception.16 The targeted setting comprised four hospitals situated in various geographical regions in Saudi Arabia (Two Eastern, one Central and one Western) all affiliated with one governmental institution. It employs more than 7,000 employees with a total bed capacity exceeding 1,000 beds. It has been accredited by the Joint Commission International several times. The health care industry in Saudi Arabia employs local Saudi healthcare workers who serve a relatively religious, tribal, and conservative culturally oriented community. However, due to the severe shortage in the work force, an influx of expatriates of various races, ethnicities and cultures from all over the world has been observed.21
Study Participants
The accessible population was fulltime healthcare practitioners (physicians, nurses, pharmacists, administrative employees and technicians) of various career levels and registered with the Saudi Commission for Health Care Specialties. These participants were asked if they were victims of WPB by reporting their experience with any form of violence regardless of its magnitude and duration in the past year. They were asked to report the details of their WPB experience (type of violence, perpetrator, place, initial reaction, method of reporting). Perpetrators were either healthcare practitioners, patients or visitors of patients who committed various forms of violent acts as perceived and reported by the victims. Due to the sensitivity of this topic and to maximize on the participants’ privacy, the data collection package consisted of a letter of invitation, an informed consent and an English language survey, all electronically accessible through a hyperlink sent through a private electronic mail. The invitation letter clarified the objectives of the study to the invitees and informed them that their participation will contribute to the body of science on WPB. A written informed consent was secured by electronically ticking on an “agreement to participate” statement. By convenience, all participants were exposed to the study, as the survey was distributed via a mass email service in 2018, twice with a one-month interval. Those who participated the first time were instructed to refrain from participating again. A disabled tracking of the filed surveys to the participants’ email addresses insured confidentiality of participants.
Data Collection Tool
The survey measured both participants’ and WPB’s characteristics. Participants’ characteristics were commonly assessed variables in the literature associated with WPB. These included gender (male vs female), age (years), marital status (single, married, separated/widowed), level of education (diploma, bachelor, masters or PhD degree), nationality (Saudis vs, Expatriates), work duration (years) and occupation (nurses, technicians, administrative, physician, pharmacists). While there is no commonly reported cut-off for age and work duration when investigating WPB, we have categorized them based on ten-year intervals, before collapsing them into binary groups. Participants with a diploma or bachelor’s degree were grouped under lower education, while those with Master’s or PhD degree were grouped under higher education. Technicians and administrative practitioners were grouped under the allied health category of occupation.
As per the World Health Organization (WHO), WPB was defined as a multifaceted form of mistreatment, characterized by a repeated exposure to physical and/or emotional aggression. Physical bullying includes an assault (with or without injury) to the individual’s body or property, such as beating, kicking, spitting, pinching, pushing, or using a rude body language. Verbal bullying involves the use of offensive words through teasing, name-humiliating, and unacceptable sexual comments.23 Participants who met the criteria of WPB23 were counted as victims . WPB characteristics were mainly the identity of the perpetrator (patient, family of patient, employees), the timing, and the place of the incidents as reported by the victims. In addition, victims were questioned about their personal reactions or responses to WPB, if they received any support, as well as the underlying cause of WPB as perceived by the participant. The consequences of WPB against the perpetrator were also recorded. The feasibility and content validity of the questionnaire were tested before being piloted among 16 practitioners. Their subjective feedback was analyzed, and modifications were made to enhance the comprehension of the survey.
Statistical Analysis
Data entry and analyses were conducted using SPSS v.26 (IBM, NY). Participants’ and WPB incident characteristics were presented in frequencies (n) and percentages (%). Factors associated with being a victim were tested using Pearson’s chi-square. Since the prevalence of the outcome was high, the prevalence rate ratio (PRR) was presented as the measure of association between exposures and outcomes.24 PRR is calculated by dividing the prevalence rate of WPB within one subgroup over the prevalence rate of WPB in the counter group. Higher PRR indicated how large is the prevalence of WPB in one group (percentage ratio) relative to the other group of the same characteristics. PRRs and their 95% confidence interval (95% CI) were obtained by conducting Poisson regression analyses (robust error estimation) to model the relationship between the study exposures (gender, age, marital status, nationality, education) and WPB as a binary outcome. Regression analyses were stratified by occupation (nurses, allied health, physicians) due to the differences in their scope of practice, chain of command, level of teamwork, and type of workload for each occupation. Statistical significance was set at P-value<0.05.
Ethics Approval and Consent to Participate
A self-explanatory letter of invitation to participate in this study was presented to each of the participants. All participants gave written informed consents for their enrollment in the study presented in this manuscript with full knowledge of the possible risks and benefits of participation. Participants consented by ticking “agree”, indicating their agreement to provide their feedback for this research study. Study was approved by the Institutional Review Board at the Saudi Ministry of National Guard – Heath Affairs (Protocol # SP18/057/R). This study followed the recommendations of the International Conference on Harmonization for Good Clinical Practice (ICH-GCP) and in compliance with the Declaration of Helsinki.
Results
Participant and WPB Characteristics
A total of 1,074 participants responded to the survey, among whom 684 (63.7%) admitted to being victims of WPB in the past year and agreed to disclose its details. The majority of participants were females (85.8%), while 67.6% were ≥30 years of age. Almost half of the nurses admitted to being victims (48.3%), administrative staff (22.7%), physicians (13.6%), technicians (12.9%) and pharmacists (2.5%). Other participants’ characteristics are presented in Table 1.
Table 1.
Association of Workplace Bullying With Sample Characteristics
| Exposure to Workplace Bullying | P-value | |||
|---|---|---|---|---|
| Yes n (%) 684 (63.7) |
No n (%) 390 (36.3) |
Total n (%) 1074 (100) |
||
|
Gender Male Female |
74 (48.7) 610 (66.2) |
78 (51.3) 312 (33.8) |
152 (14.2) 922 (85.8) |
<0.001* |
|
Age (years) <30 30–40 >40 |
269(77.3) 139(46.8) 276(64.3) |
79(22.7) 158(53.2) 153(35.7) |
348(32.4) 297(27.7) 429(39.9) |
<0.001* |
|
Marital status Single/separated Married |
373(69.9) 311(57.6) |
161(30.1) 229(42.4) |
536(49.7) 540(50.3) |
<0.001* |
|
Educational status Diploma’s/Bachelor’s degree Master’s/PhD degree |
549(63.3) 135(65.2) |
318(36.7) 72(34.8) |
867(80.7) 207(19.3) |
0.610 |
|
Nationality Local Expatriate |
165(56.5) 519(66.4) |
127(43.5) 263(33.6) |
292(27.2) 782(72.8) |
0.003* |
|
Work experience (years) ≤10 >10 |
411(70.0) 273(56.1) |
176(30.0) 214(43.9) |
587(54.7) 487(45.3) |
<0.001* |
|
Occupation Nurses Technicians Administrative Physician Pharmacists |
336(64.7) 74(53.2) 166(68.0) 100(68.5) 8(30.8) |
183(35.3) 65(46.8) 78(32.0) 46(31.5) 18(69.2) |
519(48.3) 139(12.9) 244(22.7) 146(13.6) 26(2.5) |
<0.001* |
Note: *Signifies statistical significance using Pearson’s chi-square test.
Abbreviations: n, frequency; %, percentage.
WPB perpetrators were mainly patients (36.1%), their relatives or families (29.5%), work colleagues (27.2%) or managers/supervisors (7.2%). The type of incident was mainly verbal abuse (98.1%), physical harassment (11.8%) and sexual connotation (5.8%). WPB mainly occurred at day shifts (80.3%) and at working stations/offices (52.6%). Almost half of the victims decided to inform a friend or a family member (48.4%) and/or report to a senior staff (28.8%). Most of the nurses claimed that the cause of the incident was misunderstanding (77%), yet 58.2% claimed that it was due to a lack of disciplinary actions that holds perpetrators accountable to their behavior. As reported by the WPB victims, only 33.6% of perpetrators received verbal warning, while no action was taken in 23.4% of the incidents. Other WPB characteristics have been enlisted in Table 2.
Table 2.
Distribution of Workplace Bullying Incident Characteristics
| n(%) 684(100.0) |
|
|---|---|
|
Type of bullying* Verbal Physical Sexual |
671(98.1) 81(11.8) 40(5.8) |
|
Perpetrator of incidents Patient Relatives of patients (visitors) Manager or supervisor Employees |
247(36.1) 202(29.5) 49(7.2) 186(27.2) |
|
Time of incident Day shift Evening shift Night shift |
549(80.3) 46(6.7) 89(13.0) |
|
Area of incident Patient room Treatment room/Clinic Working station/office Nonclinical areas |
142(20.9) 157(23.0) 360(52.6) 24(3.5) |
|
Reaction to workplace bullying* Told friends/family Reported to senior staff member Told the person to stop Told a colleague Tried to defend self physically Completed incident or accident form Sought counseling Transferred to another position No action, pretended it never happened |
331(48.4) 197(28.8) 183(26.8) 180(26.3) 124(18.1) 76(11.1) 55(8.0) 46(6.7) 71(6.6) |
|
Causes of workplace bullying* Misunderstanding Lack of discipline to hold people accountable about their behavior Concern of patients Communication or Language barriers Lack of explicit rights or procedure Illness Personal problem of coworker Scapegoat for medical dispute Poor training on WPB Fault of oneself Drinking problem |
527(77.0) 398(58.2) 279(40.8) 267(39.0) 118(17.3) 106(15.5) 96(14.0) 26(3.8) 24(3.5) 23(3.4) 15(2.2) |
|
Consequences to the perpetrator None Verbal warning issued Written warning Care discontinued Counseling Reported to police (prosecution) Do not know |
160(23.4) 230(33.6) 83(12.1) 58(8.5) 10(1.5) 9(1.3) 134(19.6) |
Note: *Non-mutually exclusive.
Abbreviations: n, frequency; %, percentage.
Workplace Bullying Across Sample Characteristics
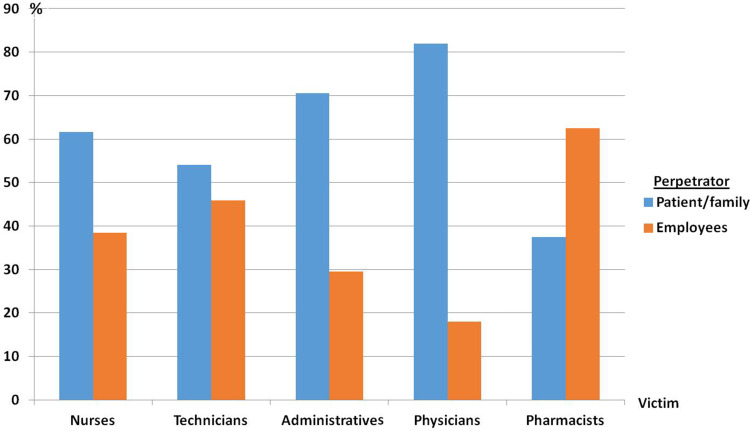
WPB was significantly more prevalent among female healthcare practitioners 66.2%, compared to male practitioners (48.7%), P<0.001. Healthcare practitioners <30 years were also more likely to be bullied (77.3%) compared to older practitioners ≥30 years of age (57.2%), P<0.001. Single or separated healthcare practitioners were also more likely to be exposed to WPB (69.9%), compared to married ones (57.6%), P<0.001. WPB was more prevalent among expatriate non-Saudi healthcare practitioners (66.4%), and practitioners with ≤10 years work experience (70.0%), P=0.003 and P<0.001, respectively. In terms of occupation, 64.7% of nurses, 68.5% of physicians, 68.0% of administrative employees, 53.2% of technicians and 30.8% of pharmacists were exposed to WPB, Table 1. The percentage distribution of perpetrator with the occupation of WPB victims is illustrated in Figure 1.
Figure 1.
Perpetrator of Work Place Bullying with the occupation of victims.
Factors Associated with Being a Victim of WPB
Poisson binary regression analyses were conducted stratified by occupation. Pharmacists were not included in the regression model analysis due to the low sample size (n=26). WPB was 30% (95% CI: 14%–48%) more prevalent among younger nurses and 24% (95% CI: 21%–34%) less prevalent among higher educated nurses compared to their counter groups, P<0.001 each. Among technicians and administrative employees, WPB was 54% (95% CI: 9%–117%) more prevalent among females, 36% (95% CI: 16%–61%) more prevalent among the younger group, and 25% (95% CI: 4%–50%) more prevalent among expatriates compared to their counter groups, P<0.014, P<0.001 and P=0.017, respectively. WPB was 20% (95% CI: 9%–117%) less prevalent among higher educated allied health, P=0.002. Among physicians, WPB was 33% (95% CI: 1%–76%) more prevalent among females compared to male physicians, P=0.041 and it was 47% (95% CI:7%–104%) more prevalent among higher educated physicians compared to their counter group, P=0.018 (Table 3).
Table 3.
Poisson Binary Regression Analyses of Factors Associated with Being a Victim of Workplace Bullying Stratified by Victims’ Occupation
| Nurse | Allied Health (Technicians and Administrative) |
Physicians | ||||
|---|---|---|---|---|---|---|
| PRR [95% CI] | P-value | PRR [95% CI] | P-value | PRR [95% CI] | P-value | |
|
Gender Male (Ref) Female |
0.83[0.67–1.03] |
0.083 |
1.54[1.09–2.17] |
0.014* |
1.33[1.01–1.76] |
0.041* |
|
Age ≥30(Ref) <30 |
1.30[1.14–1.48] |
<0.001* |
1.36[1.16–1.61] |
<0.001* |
1.12[0.85–1.46] |
0.428 |
|
Marital status Married (Ref) Single |
1.10[0.95–1.27] |
0.206 |
0.95[0.80–1.13] |
0.587 |
1.21[0.91–1.60] |
0.187 |
|
Nationality local (Ref) Expatriate |
1.14[0.94–1.38] |
0.195 |
1.25[1.04–1.50] |
0.017* |
1.20[0.98–1.48] |
0.084 |
|
Education Lower (Ref) Higher |
0.76[0.66–0.88] |
<0.001* |
0.80[0.69–0.92] |
0.002* |
1.47[1.07–2.04] |
0.018* |
| Intercept | 0.76[0.57–1.03] | 0.076 | 0.41[0.29–0.58] | <0.001* | 0.31[0.22–0.44] | <0.001* |
Note: *Significance of P < 0.05.
Abbreviations: (Ref), reference group; %, percentage; CI, confidence interval; PRR, prevalence rate ratio.
Discussion
Hospital administrators should be cautioned that WPB is more prevalent among female healthcare practitioners compared to males. This finding was similar to the report of a Swedish health care system where victims of WPB were predominantly women (90%).8 Gender plays an important role in predicting WPB;25 however, gender should not be accounted as a single precursor to WPB at health care facilities. In this setting, occupation was associated with WPB. This phenomenon can be attributed to the scope of practice. Some healthcare practitioners, such as nurses or allied health employees are more involved in bedside care and differ in their chain of command compared to physicians or pharmacists.26 Nurses and allied healthcare practitioners report to unit managers, nurse coordinators, shift supervisors, and other health disciplines. They operate in larger teams and their workload is more physically demanding, even though they are limited to fewer patients when compared to physicians or pharmacists.27 Authors believe that this difference in scope of practice and work relationships contributed to the variation in WPB incidents between them. On the other hand, physicians/pharmacists tend to rotate between various hospital wards. They usually communicate more with patients/families, especially when it has to do with reporting medical diagnoses, clinical progress and critical lifesaving decisions. Therefore, WPB among physicians/pharmacists might have been due to disrupted communication with the patients/families, lack of patients’ expectations, or patients’ misinterpretation of the delivered messages. In this setting, bullied physicians/pharmacists claimed that it was due to miscommunication with patients (27.7%) or misinterpretation of medical instructions (86%). Any disrupted communication between families and health care teams eventually results in stress, temper, lack of confidence, and, subsequently, violence.28
Age was a significant factor associated with WPB in this setting, as WPB was more prevalent (77.3%) among younger healthcare practitioners (<30 years). WPB was also more prevalent (70%) among less experienced employees (<10 years). Age and work experience are collinear variables. We believe that fresh graduates and junior practitioners have not sufficiently developed their interpersonal work relationships or communication skills, which explains why 70% of WPB was observed among this group. A synthesis of evidence from 16 studies showed that newly graduated employees were at higher risk of being exposed to a negative workplace behavior.29 In this setting, the young and less experienced practitioners who reported WPB were probably incapable of delivering the message properly to patients or their families (33.4%). Furthermore, in one study, nurses who have been abused by a patient or family member failed to find support from their managers.30 This was comparable with findings in this setting, as 30.6% of nurses who were bullied reported a lack of support from management. In addition, authors found that junior practitioners in this setting were subject to criticizing comments from senior practitioners (11.9%). The stressful work environment might be challenging to them, which makes them lose focus on properly handling a WPB incident when the need arises. For instance, it has been reported that practitioners usually focus on their own patient assignments with little time or interest in conflict resolution.30 Hectic duties and stressful work environments witnessed by these practitioners might trigger a loss of temper. In this setting, 39% of practitioners reported that the lack of communication contributed to WPB, while 14% stated that it was due to poor collaboration. Furthermore, healthcare practitioners regularly find short-notice and multiple batch admissions or discharges as major stressors, especially if it is not well coordinated with the admission office. Unmet patient/family expectations, such as lack of vacant beds or absence of resources, will eventually create a chaotic work environment where WPB might arise.30 In this setting, 40.8% of practitioners who were bullied claimed that it was due to their inability to satisfy patient/family needs.
WPB was also more prevalent among expatriate healthcare practitioners compared to local Saudi employees. Victims of WPB in one setting reported that these incidents arose due to cultural difference or language barriers.31 In this setting, English language is the predominant language used among healthcare practitioners, yet Arabic language is the official language for the public community. Non-Arabic speaking expatriate healthcare practitioners strive to communicate with their patients using simplified, unstructured Arabic dialect. This factor might have aggravated a potential misunderstanding that escalated to WPB, simply due to a failure in expressing the true thoughts, as reported by 77% of bullied victims in this study. Currently, there have been no previously published studies that related WPB to language and cultural differences between healthcare practitioners and patients/their relatives. Accordingly, hospital administrators are encouraged to disseminate educational offerings throughout the health care settings about proper work relationships and professional communication.
Limitations
A number of limitations have been observed in this study. Authors believe that WPB is an under-reported phenomenon, so the recruited sample might not be exhaustive in its representativness. We suspect that some participants might have been exposed to a certain form of harassment once, and perceived it is as bullying. Nevertheless, some victims might have been harassed once, yet from different patients, visitors or employees. This makes the perpetrator not necessarily restricted to one confined incident. In addition, there is a possibility that some participants had experience with WPB or were more likely to be interested to respond to the survey compared to non-participants. Moreover, although participants were not involved in the recruitment of other study participants, there is a chance that some might have shared the link of the survey with other participants who were not originally invited to participate. Disclosing the WPB incidents to hospital administrators necessitates a supportive work culture and a transparent reporting system that insures the privacy and safety of WPB victims. Another limitation is recall bias, taking into account the retrospective design of the study. However, authors believe that the details of WPB, whether it is an isolated or a repetitive incident, are unlikely to be forgotten by the victims. In addition, certain conflicts, among employees or between employees and patients/their families, might have been misinterpreted by the victims as an act of aggression or bullying. Furthermore, life factors such as social/financial stressors, previous mental/psychological disorders or even prior traumas might have elicited a WPB incident from the perpetrator’s side or increased the vulnerability from the victim’s side. Therefore, in-depth analyses of the true causes and implications of WPB incidents require a more personal qualitative research methodological approach, which was beyond the scope of this study.
Conclusion
WPB might occur any time, anywhere and by any person within healthcare facilities. The prevalence of WPB varies within occupational groups. Gender, age, educational level, and nationality were all factors associated with WPB. The leading form of WPB in this setting was verbal abuse that mainly occurred during day shifts. WPB was more prevalent among female healthcare practitioners, <30 years of age, and expatriates. Among nurses, it was more prevalent among those <30 years old, and those with advanced educational levels. Among allied healthcare professionals (technicians and administrative staff), female gender, young age, expatriate, and advanced education were factors associated with WPB incidents. WPB was more prevalent among female physicians and those with higher educational degrees. WPB incidents were more likely to occur at work stations, followed by treatment rooms or clinics.
WPB is unfortunate by all means. It is the employees’ and patients’ right, as well as the duty of all hospital administrators, to promote a safe working environment, free of any harassment type. This study analyzed actual WPB incidents in attempt to identify occupational groups with high prevalence rates of WPB. Accordingly, action plans can be launched to educate and train vulnerable groups, and to closely monitor work environments. Identifying high-risk work environments includes detecting, reporting and resolving early warning signs of WPB. Regrettably, some believe that interventions to prevent WPB are ineffective, with emphasis on the fact that WPB is being primarily facilitated by organizational causes and culture that hinders the formation of collegiality and trust among employees.32
Acknowledgments
This study was approved and monitored by King Abdullah International Medical Research Center, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia. The authors would like to thank Mr. Mohamad Al-Assiri and Mrs. Lara Afesh for their tremendous support. The authors are grateful to the participants who shared the details of unfortunate WPB incidents. We hereby presented this valuable contribution for the sake of protecting healthcare practitioners from WPB incidents in the future.
Funding Statement
There is no funding to report.
Article Summary
Strengths and Limitations
Workplace bullying has not been addressed sufficiently in Middle Eastern settings.
It is imperative to all healthcare settings to detect any case of WPB, to analyze its characteristics, determine high-risk groups, and take the right action.
This study analyzed the various characteristics of WPB incidents at a multi-regional healthcare facility in Saudi Arabia.
Most WPB incidents remain under reported, so the recruited sample might not be exhaustive .
Certain conflicts, among employees or between employees and patients/their families, might have been misinterpreted by the victims as an act of aggression or bullying.
Key Points
Leading type of WPB in this healthcare setting is verbal abuse that occurred during day shifts.
WPB seems more prevalent among females, young age group, and expatriates.
WPB is more likely to occur at work stations or offices.
WPB perpetrators were mainly patients, relatives of patients, employees or managers/supervisors.
Abbreviations
95% CI, 95% confidence interval; PRR, prevalence rate ratio; WPB, workplace bullying; WHO, World Health Organization.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available due to the institutional rules and regulations but are available from the corresponding author on reasonable request.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests for this work.
References
- 1.Al-Ghabeesh SH, Qattom H. Workplace bullying and its preventive measures and productivity among emergency department nurses. BMC Health Serv Res. 2019;19(1):445. doi: 10.1186/s12913-019-4268-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hollis LP. Bully university? The cost of workplace bullying and employee disengagement in American higher education. Sage Open. 2015;5(2):2158244015589997. [Google Scholar]
- 3.Pei KY, Hafler J, Alseidi A, Slade MD, Klingensmith M, Cochran A. National assessment of workplace bullying among academic surgeons in the US. JAMA Surg. 2020;155(6):524. doi: 10.1001/jamasurg.2020.0263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feijó FR, Gräf DD, Pearce N, Fassa AG. Risk factors for workplace bullying: a systematic review. Int J Environ Res Public Health. 2019;16(11):1945. doi: 10.3390/ijerph16111945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Rourke M, Wrigley C, Hammond S. Violence within mental health services: how to enhance risk management. Risk Manag Healthc Policy. 2018;11:159. doi: 10.2147/RMHP.S131834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saleh LA, Niroumand S, Dehghani Z, Saleh TA, Mousavi SM, Zakeri H. Relationship between workplace violence and work stress in the emergency department. J Inj Violence Res. 2020;12(2). [DOI] [PubMed] [Google Scholar]
- 7.Cantone E, Piras AP, Vellante M, et al. Interventions on bullying and cyberbullying in schools: a systematic review. Clin Pract Epidemiol Ment Health. 2015;11:58. doi: 10.2174/1745017901511010058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahm G, Rystedt I, Wilde-Larsson B, Nordström G, Strandmark KM. Workplace bullying among healthcare professionals in Sweden: a descriptive study. Scand J Caring Sci. 2019;33(3):582–591. doi: 10.1111/scs.12633 [DOI] [PubMed] [Google Scholar]
- 9.Ariza-Montes A, Muniz N, Montero-Simó M, Araque-Padilla R. Workplace bullying among healthcare workers. Int J Environ Res Public Health. 2013;10(8):3121–3139. doi: 10.3390/ijerph10083121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Medscape. Medscape report finds physicians are sexually harassed on the job. June, 2018.
- 11.Bjørkelo B, Einarsen S, Matthiesen SB. Predicting proactive behaviour at work: exploring the role of personality as an antecedent of whistleblowing behaviour. J Occup Organ Psychol. 2010;83(2):371–394. doi: 10.1348/096317910X486385 [DOI] [Google Scholar]
- 12.Rivara F, Le Menestrel S. Preventing Bullying Through Science, Policy, and Practice. The National Academies Press; 2016. [PubMed] [Google Scholar]
- 13.Nielsen MB, Harris A, Pallesen S, Einarsen SV. Workplace bullying and sleep–a systematic review and meta-analysis of the research literature. Sleep Med Rev. 2020;101289. [DOI] [PubMed] [Google Scholar]
- 14.Namie G, Namie R. US workplace bullying: some basic considerations and consultation interventions. Consult Psychol J: Pract Res. 2009;61(3):202. doi: 10.1037/a0016670 [DOI] [Google Scholar]
- 15.Sansone RA, Sansone LA. Workplace bullying: a tale of adverse consequences. Innov Clin Neurosci. 2015;12(1–2):32. [PMC free article] [PubMed] [Google Scholar]
- 16.Al Omar M, Salam M, Al-Surimi K. Workplace bullying and its impact on the quality of healthcare and patient safety. Hum Resour Health. 2019;17(1):89. doi: 10.1186/s12960-019-0433-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaffney DA, DeMarco RF, Hofmeyer A, Vessey JA, Budin WC. Making things right: nurses’ experiences with workplace bullying—a grounded theory. Nurs Res Pract. 2012;2012:1–10. doi: 10.1155/2012/243210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Srabstein JC, Leventhal BL. Prevention of bullying-related morbidity and mortality: a call for public health policies. SciELO Public Health. 2010;403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hogh A, Hoel H, Carneiro IG. Bullying and employee turnover among healthcare workers: a three-wave prospective study. J Nurs Manag. 2011;19(6):742–751. doi: 10.1111/j.1365-2834.2011.01264.x [DOI] [PubMed] [Google Scholar]
- 20.Almutairi KM. Culture and language differences as a barrier to provision of quality care by the health workforce in Saudi Arabia. Saudi Med J. 2015;36(4):425. doi: 10.15537/smj.2015.4.10133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Hanawi MK, Khan SA, Al-Borie HM. Healthcare human resource development in Saudi Arabia: emerging challenges and opportunities—a critical review. Public Health Rev. 2019;40(1):1. doi: 10.1186/s40985-019-0112-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kvas A, Seljak J. Unreported workplace violence in nursing. Int Nurs Rev. 2014;61(3):344–351. doi: 10.1111/inr.12106 [DOI] [PubMed] [Google Scholar]
- 23.Leisy HB, Ahmad M. Altering workplace attitudes for resident education (AWARE): discovering solutions for medical resident bullying through literature review. BMC Med Educ. 2016;16(1):127. doi: 10.1186/s12909-016-0639-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tamhane AR, Westfall AO, Burkholder GA, Cutter GR. Prevalence odds ratio versus prevalence ratio: choice comes with consequences. Stat Med. 2016;35(30):5730–5735. doi: 10.1002/sim.7059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang M-L, Hsieh Y-H. Do gender differences matter to workplace bullying? Work. 2016;53(3):631–638. doi: 10.3233/WOR-152239 [DOI] [PubMed] [Google Scholar]
- 26.Colón-Emeric CS, Ammarell N, Bailey D, et al. Patterns of medical and nursing staff communication in nursing homes: implications and insights from complexity science. Qual Health Res. 2006;16(2):173–188. doi: 10.1177/1049732305284734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Montgomery A, Spânu F, Băban A, Panagopoulou E. Job demands, burnout, and engagement among nurses: a multi-level analysis of ORCAB data investigating the moderating effect of teamwork. Burn Res. 2015;2(2–3):71–79. doi: 10.1016/j.burn.2015.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Loghmani L, Borhani F, Abbaszadeh A. Factors affecting the nurse-patients’ family communication in intensive care unit of kerman: a qualitative study. J Caring Sci. 2014;3(1):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hawkins N, Jeong S, Smith T. New graduate registered nurses’ exposure to negative workplace behaviour in the acute care setting: an integrative review. Int J Nurs Stud. 2019;93:41–54. doi: 10.1016/j.ijnurstu.2018.09.020 [DOI] [PubMed] [Google Scholar]
- 30.Taylor R. Nurses’ perceptions of horizontal violence. Glob Qual Nurs Res. 2016;3:1–9. doi: 10.1177/2333393616641002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Makarem NN, Tavitian-Elmadjian LR, Brome D, Hamadeh GN, Einarsen S. Assessment of workplace bullying: reliability and validity of an Arabic version of the Negative Acts Questionnaire-Revised (NAQ-R). BMJ Open. 2018;8(12):e024009. doi: 10.1136/bmjopen-2018-024009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arnetz JE, Fitzpatrick L, Cotten SR, Jodoin C. Workplace bullying among nurses: developing a model for intervention. Violence Vict. 2019;34(2):346–362. doi: 10.1891/0886-6708.VV-D-17-00211 [DOI] [PubMed] [Google Scholar]