Abstract
Background
Mental health diagnoses (MHD) are common among those with opioid use disorders (OUD). Methadone/buprenorphine are effective medication-assisted treatment (MAT) strategies; however, treatment receipt is low among those with dual MHDs. Medicaid expansions have broadly increased access to OUD and mental health services over time, but MAT uptake may vary depending on multiple factors, including MHD status, state Medicaid expansion decisions, and race/ethnicity and gender. Examining clinical and policy approaches to promoting MAT uptake may improve services among marginalized groups.
Methods
MAT treatment discharges were identified using the Treatment Episodes Dataset–Discharges (TEDS-D; 2014–2017) (n=1,400,808). We used multivariate logistic regression to model MAT receipt using interactions and adjusted for several potential confounders.
Results
Nearly one-third of OUD treatment discharges received MAT. Dual MHDs in both expansion and non-expansion states were positively associated with MAT uptake over time. Dual MHDs were negatively associated with MAT receipt only among American Indian/Alaska Native women residing in Medicaid expansion states (aOR=0.58, 95% CI=0.52–0.66, p<0.0001).
Conclusion
Disparities in MAT utilization are nuanced and vary widely depending on dual MHD status, Medicaid expansion, and race/ethnicity/gender. Medicaid is beneficial but not a universal treatment panacea. Clinical decisions to initiate MAT are dependent on multiple factors and should be tailored to meet the needs of high-risk, historically disadvantaged clients.
Keywords: Mental health, opioid use disorder, medication-assisted treatment, health policy, health disparities
1.1. Introduction
The modern epidemic of opioid overdose and opioid-related deaths contributes substantially to the overall morbidity and mortality in the United States (Manchikanti et al., 2012; Rudd, 2016; Spaniol et al., 2019). In response to these trends, a variety of novel public health and clinical approaches focus on reducing opioid misuse and mitigating the medical, psychological, and public health effects arising from opioid misuse and withdrawal (Johnson et al., 2018; Spaniol et al., 2019). Specifically, medication-assisted treatment (MAT) is an effective strategy to treat opioid use disorders (OUDs), demonstrating improved outcomes and lower relapse rates among patients when providers include MAT as a component of treatment programming (McElrath & Joseph, 2018; Zoorob et al., 2018). In many clinical settings, MAT with buprenorphine is often the first line treatment for OUDs (Dunlap & Cifu, 2016). Other medications used in OUD treatment include the prescribed use of methadone and naltrexone (Alderks, 2017). However, the availability of MAT may be dependent on a variety of geographic, demographic, and health policy factors. Related to client demographic factors, co-occurring mental health diagnoses (MHD) and OUDs present clinicians with a more complex psychological and medical profile when prescribing and monitoring MAT.
1.1.2. Co-occurring disorders and MAT
MHDs are common among people diagnosed with OUDs (Campbell et al., 2018; Sullivan et al., 2006), but few individuals (16%) with co-occurring mental health and opioid use disorders receive the integrated treatment they need (Novak et al., 2019). People diagnosed with co-occurring disorders face an increased likelihood for opioid overdose and death (Johnson et al., 2013), due in part to lower treatment engagement and the financial resources needed to enroll in treatment (Novak et al., 2019; Schafer et al., 2010). Additionally, clients living with untreated MHDs experience symptoms that may inhibit their access to and compliance with MAT (Carpentier et al., 2009). These factors may be further compounded by racial/ethnic differences in adherence rates and access to services.
1.1.3. Racial/ethnic and gender disparities in MAT
There are a variety of disparities related to utilization of MAT between racial/ethnic groups (Wu et al., 2016). Racial/ethnic minorities with OUD often suffer worse health outcomes related to involvement in the criminal justice system, elevated risk of exposure to violence, and experiences with medical complications (Alegria et al., 2011). Findings on racial/ethnic disparities in MAT initiation are mixed, however, depending on the specific opioid indicated at treatment admission, the specific MAT medication type under study, as well as the study design and target populations. For example, Krawczyk and colleagues (2017) found that White heroin users in treatment were less likely than Blacks and Hispanics to receive methadone or buprenorphine, despite Whites demonstrating among the highest rates of illicit opioid abuse (Friedman et al., 2019). Conversely, among Medicaid enrollees and following the federal approval of buprenorphine in 2002, receipt of buprenorphine increased at a much higher rate in predominately White counties, compared to counties with higher concentrations of Black and Hispanic individuals (Stein et al., 2018). Finally, among a sample of primary care patients with OUD in the Pacific Northwest, Cantone and colleagues (2019) found no difference in the odds of receiving buprenorphine or naltrexone between Whites and a single group of all non-White racial/ethnic minorities. Although the picture of disparities is complex and dependent on many factors, questions about racial/ethnic differences in MAT receipt remain unanswered and demand much needed public health and clinical attention.
Related to integrated treatment for co-occurring mental health disorders, people from racial/ethnic minority groups face additional burdens related to care, including stigma, economic disadvantages, fear of arrest, and lack of health insurance (Gary, 2005; Lui et al., & Campbell, 2017; Saloner & Cook, 2013). In addition, racial/ethnic minorities experience lower rates of treatment retention and completion, and longer episodes of treatment when compared to White counterparts (Garrison et al., 2018; Mennis & Stahler, 2016; Mennis et al., 2019; Stahler & Mennis, 2018).
Gender disparities are also apparent in OUD treatment services utilization. The prevalence of opioid misuse is higher among women than men (Serdarevic et al., 2018). Women suffer greater rates of chronic pain and pain-related disability compared to their male counterparts (Mogil & Bailey, 2010; Musey et al., 2014), both of which are risk factors for opioid misuse (Volkow & McLellan, 2016). Women also experience a more rapid onset of addiction and increased deleterious consequences of opioid misuse compared to men (Becker & Mazure, 2019). As many OUDs are closely related to chronic pain and physical concerns, the availability of health insurance and access to medical care can present barriers to integrated care of medical and opioid use disorders.
Race/ethnicity and gender are key factors in investigations about MAT disparities. However, critical relationships between race/ethnicity and gender remain unexplored, including examinations of gender effects within racial/ethnic groups and effects of race/ethnicity within gender groups. For example, drawing on Kimberlé Crenshaw’s Intersectionality Theory (Crenshaw, 1989, 1991), there may be unique clinical experiences among Native American women that further our understanding of MAT disparities that would not otherwise be documented in research that reports on aggregate effects within Native Americans and women separately. Thus, in the current study we report estimates of MAT receipt among racial/ethnic groups disaggregated by gender.
1.1.4. Health insurance and Medicaid expansion
Lack of insurance presents a significant barrier that limits access to substance use disorder (SUD) treatment (Ali et al., 2017), especially among low socioeconomic groups who are eligible for Medicaid (Buck, 2011). While some states expanded Medicaid coverage for SUD treatment, many Medicaid eligible individuals still do not seek SUD treatment (Andrews et al., 2019). Despite the gains made through Medicaid expansion – coupled with federal approval of buprenorphine – significant disparities remain between expansion and non-expansion states with respect to their enrollment in MAT. Between 2011 and 2016, rates of buprenorphine and naltrexone prescriptions increased more in expansion states (200% increase) than in non-expansion states (50% increase) (Sharp et al., 2018), but there were no indications of whether these increases were experienced equally among multiple subpopulations in this report. Similarly, Wen and colleagues found that Medicaid expansions were associated with a 70% increase in Medicaid-covered buprenorphine prescriptions (Wen et al., 2017), but did not disaggregate rate changes by groups that have been disproportionately burdened by the opioid epidemic.
Recent research indicates that Medicaid expansion has not necessarily translated into more and better MAT coverage (Olfson et al., 2018), as several expansion states demonstrate a very high need for MAT but lack the resources and capacity to provide services (Abraham et al., 2018). Meinhofer and colleagues (2018) demonstrated that buprenorphine coverage varies within expansion states. Specifically, the effect of Medicaid expansion on buprenorphine coverage was greatest within states with pre-existing comprehensive MAT coverage, while no change in buprenorphine coverage was observed in expansion states with limited treatment infrastructure.
Research also indicates that the increase in MAT through Medicaid expansions primarily grew in wealthier and predominately White counties (Stein et al., 2018). Although Medicaid expansions increased rates of mental health treatment utilization overall (McMorrow et al., 2016), racial/ethnic minority groups did not seek services at higher rates following expansions (Creedon & Cook, 2016).
While Medicaid expansions are broadly associated with an increase in MAT availability and use, substantial gaps in the literature remain regarding disparities in MAT receipt. Little is known about whether the effects of individual demographic and clinical characteristics on MAT receipt vary by Medicaid expansion status. Documenting disparities on multiple levels is an important strategy in identifying subgroups that may benefit from targeted treatment interventions. In addition, better understanding differences between expansion and non-expansion states may inform health policy aimed at increasing uptake of MAT.
2.1. Rationale and Purpose of the Study
The ability to identify and treat people with dual OUDs and MHDs is crucial to mitigate the burden of opioid misuse and lessen the public health toll exacted by overdoses in the United States. Currently, there is little research exploring treatments that tailor MAT approaches for clients also diagnosed with a MHD. Even less is known about how race/ethnicity and gender may affect MAT among those with comorbid diagnoses of OUD and MHD. Finally, research is needed to estimate the moderating role of Medicaid expansion on MAT initiation for these clinically complex populations.
Using a large, population treatment data set, the purpose of this study was to address the crucial gaps identified in the public health and clinical literature by estimating the likelihood of MAT receipt among treatment discharges with OUD and MHDs. We explored the association between MAT receipt and dual MHD, as well as moderating effects by state-level Medicaid expansion status and race/ethnicity and gender. We assessed a change in the odds of MAT receipt over time by also including year as a moderator. Previous studies have examined MAT receipt within one or two of these variables in combination, but no reports have parsed out group differences in MAT receipt based on state-level policy indicators and multiple individual characteristics that are related to health services usage. Our aim was to illuminate the complexities of MAT disparities, while advancing the discussion of how to equitably alter the course of the opioid epidemic.
3.1. Methods
3.1.1. Data source and sample
We used the Treatment Episode Dataset – Discharges (TEDS-D) across four years of data (2014–2017) to identify treatment discharges that had heroin or other opioids indicated as primary substances at treatment admission, and that had complete data for all study variables (n=1,400,808). The timeframe of 2014–2017 was chosen so that all states would have a Medicaid expansion decision (yes or no) following the implementation of the Affordable Care Act. In short, TEDS-D is an annual, repeated cross-sectional dataset that includes treatment services and demographic information for treatment discharges that utilized services in facilities receiving any federal funding (Substance Abuse and Mental Health Data Archive, 2018).
3.1.2. Variables
We defined our primary outcome of interest as a pre-defined single TEDS-D variable indicating whether MAT (methadone or buprenorphine) was included as part of the treatment regimen. We considered three focal independent variables. We combined race/ethnicity and gender to create a race/ethnicity/gender variable, coded as White men, White women, Black men, Black women, Hispanic men, Hispanic women, AI/AN men, and AI/AN women. The mental health indicator was derived from a single TEDS-D variable that included whether the discharge had an MHD in addition to their alcohol or drug use problem (yes or no). We appended state-level data from the Kaiser Family Foundation to our TEDS-D dataset to create a state Medicaid expansion status categorical variable (yes/no) by year (Henry J. Kaiser Family Foundation, 2019). Because some states adopted federal Medicaid expansion provisions in different years after January 1, 2014, clients were coded as residents of Medicaid expansion states depending on the status of their state for each year.
We also considered several covariates based on a priori understanding of factors that likely confound the relationship between our focal independent variables and MAT receipt, including a) age group (18–29, 30–39, 40–49, or more than 50 years), b) educational attainment (less than high school, high school completion, some college, or college completion), c) primary opioid at treatment admission (heroin or prescription/other opioids), d) intravenous drug user at treatment admission (yes or no), alcohol, cocaine, or methamphetamine reported at treatment admission (yes or no), and e) treatment referral source (individual/self-referred, substance use or healthcare provider, the criminal justice system, or a combined group including school, employee assistance program, or community referrals).
3.1.3. Analyses
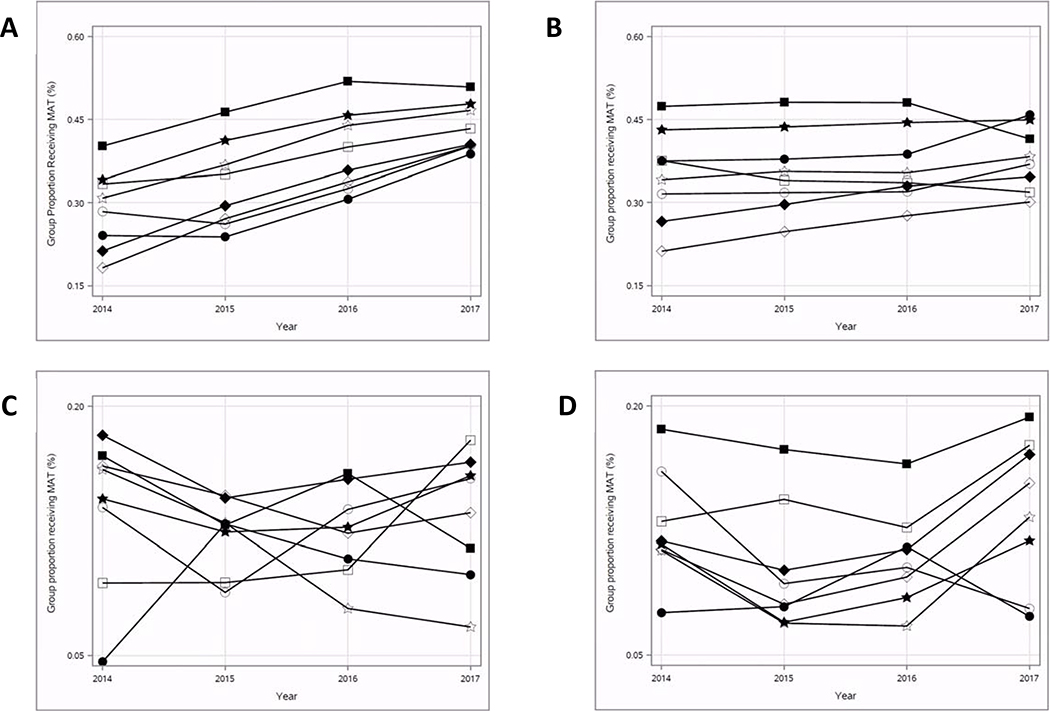
Using four years of TEDS-D data (2014–2017), we first plotted within-group proportions of treatment discharges which received MAT over time, stratified by four possible combinations of Medicaid expansion status and dual mental health status: 1) treatment discharges with dual mental health diagnoses in Medicaid expansion states; 2) treatment discharges without dual mental health diagnoses in expansion states; 3) treatment discharges with dual mental health diagnoses in non-expansion states, and; 4) treatment discharges without dual mental health diagnoses in non-expansion states. We then calculated the distributions of each study variable for the total sample, as well as stratified by our outcome of whether the treatment discharge received MAT. We used chi-square tests of independence to describe bivariate associations within each study variable and MAT receipt.
We used multivariable logistic regression to model MAT receipt. We included two two-way interaction terms between 1) dual MHD and race/ethnicity/gender and 2) dual MHD and year. We stratified our fitted models by Medicaid expansion status. Using SAS (v9.4) (SAS Institute Inc., Cary, NC), we utilized a generalized linear mixed models procedure (PROC GLIMMIX) with the LSMEANS statement and SLICEDIFF option, which generates within-group comparisons of dual MHD (versus no dual MHD) at multiple fixed levels of the second interaction term. Specifically, we estimated the association between MAT receipt and dual MHD within racial/ethnic/gender groups as well as within years. Our model was adjusted for all study covariates. We reported adjusted odds ratios, 95% confidence intervals, and p-values for the global association (dual MHD versus no dual MHD) as well as associations within each level of race/ethnicity/gender and within each year.
Because statistical tests of group differences are more likely to yield low and significant p-values with large sample sizes, even when between-group means are very close, we adjusted our alpha threshold of significance to p<0.0001 to account of our large sample size (Sahker, Toussaint, Ramirez, Ali, & Arndt, 2015) These procedures mirrored analyses that Krawczyk and colleagues (Krawczyk et al., 2017) used in analyses of large TEDS-D datasets.
4.1. Results
Overall, the global proportions of all OUD treatment discharges that received MAT were highest among 1) discharges with dual mental health diagnoses in Medicaid expansion states (35%), followed by 2) non-dual MHDs in expansion states (30%), 3) dual MHDs in non-expansion states (15%), and 4) non-dual MHDs in non-expansion states (12%). However, group proportions varied widely within racial/ethnic/gender groups and across years. Between 2014 and 2017, the proportion of OUD treatment discharges that received MAT increased most prominently among discharges with dual mental health diagnoses that also resided in Medicaid expansion states (Figure 1A). Within this subset, the biggest changes in MAT receipt between 2014 and 2017 were observed among White men (22% increase) and White women (19% increase), while the smallest change was observed among Black men (10% increase). Comparatively, also among treatment discharges with dual mental health diagnoses but in non-expansion states (Figure 1B), the biggest change in MAT receipt over time was observed among Hispanic men (9% decrease) and Black men (9% increase).
Figure 1.
A: Within-group proportions of MAT receipt among treatment episodes with heroin or other opioids reported as primary substances at treatment admission; Treatment episodes with dual mental health disorders in expansion states (TEDS-D, 2012–2017, n=398,155). Fig. 1B: Within-group proportions of MAT receipt among treatment episodes with heroin or other opioids reported as primary substances at treatment admission; Treatment episodes without dual mental health disorders in expansion states (TEDS-D, 2012–2017, n=755,827). Fig. 1C: Within-group proportions of MAT receipt among treatment episodes with heroin or other opioids reported as primary substances at treatment admission; Treatment episodes with dual mental health disorders in non-expansion states (TEDS-D, 2012–2017, n=88,201). Fig. 1D: Within-group proportions of MAT receipt among treatment episodes with heroin or other opioids reported as primary substances at treatment admission; Treatment episodes without dual mental health disorders in non-expansion states (TEDS-D, 2012–2017, n=158,625).
Note:
Circle outline = American Indian/Alaska Native men
Circle filled = American Indian/Alaska Native women
Square outline = Black men
Square filled = Black women
Star outline = Hispanic men
Star outline = Hispanic women
Diamond outline = White men
Diamond filled = White women
The majority of treatment discharges did not have a dual mental health diagnoses (65%) and resided in Medicaid expansion states (82%) (Table 1). Nearly half were White men (46%), followed by White women (30%) and Hispanic men (10%). The proportions of OUD treatment discharges that received MAT were higher among discharges with concurrent mental health diagnoses than those without diagnoses (p<0.0001), those which resided in Medicaid expansion states versus non-expansion states (p<0.0001), and all non-White, racial/ethnic minority discharges versus White discharges (p<0.0001). MAT receipt was also higher in later years (2016 and 2017 versus 2014 and 2015) (p<0.0001).
Table 1:
Descriptive characteristics of treatment episodes with heroin or other opioids reported as primary substances at treatment admission (TEDS-D, 2014–2017, n=1,400,808)
| MAT status |
||||||
|---|---|---|---|---|---|---|
| Variables | Total | Did not receive MAT n=1,004,724 (72%) | Received MAT n=396,084 (28%) | x2 | p | |
| n | % | col % | col % | |||
| Residence in Medicaid expansion state | 34720.96 | <0.0001 | ||||
| No | 246,826 | 17.62 | 21.39 | 8.07 | ||
| Yes | 1,153,982 | 82.38 | 78.61 | 91.93 | ||
| Dual mental health diagnosis | 1470.90 | <0.0001 | ||||
| No | 914,452 | 65.28 | 66.25 | 62.82 | ||
| Yes | 486,356 | 34.72 | 33.75 | 37.18 | ||
| Race/ethnicity/gender | 14755.52 | <0.0001 | ||||
| White men | 646,064 | 46.12 | 48.42 | 40.28 | ||
| White women | 423,905 | 30.26 | 30.34 | 30.06 | ||
| Hispanic men | 146,379 | 10.45 | 9.46 | 12.96 | ||
| Hispanic women | 48,373 | 3.45 | 2.89 | 4.88 | ||
| Black men | 81,499 | 5.82 | 5.55 | 6.49 | ||
| Black women | 37,948 | 2.71 | 2.19 | 4.03 | ||
| AIAN men | 7,881 | 0.56 | 0.56 | 0.58 | ||
| AIAN women | 8,759 | 0.63 | 0.59 | 0.73 | ||
| Year | 5927.37 | <0.0001 | ||||
| 2014 | 242,643 | 17.32 | 18.60 | 14.09 | ||
| 2015 | 407,824 | 29.11 | 29.59 | 27.91 | ||
| 2016 | 419,248 | 29.93 | 29.27 | 31.59 | ||
| 2017 | 331,093 | 23.64 | 22.54 | 26.41 | ||
| Covariates | ||||||
| Age group | 28305.36 | <0.0001 | ||||
| 18–29 | 533,706 | 38.10 | 40.81 | 31.22 | ||
| 30–39 | 490,655 | 35.06 | 35.78 | 33.12 | ||
| 40–49 | 212,879 | 15.20 | 14.20 | 17.72 | ||
| 50+ | 163,568 | 11.68 | 9.21 | 17.94 | ||
| Education | 1775.33 | <0.0001 | ||||
| Less than high school | 361,282 | 25.79 | 24.83 | 28.23 | ||
| HS completion | 683,666 | 48.81 | 49.27 | 47.62 | ||
| Some college | 294,969 | 21.06 | 21.47 | 20.02 | ||
| College completion | 60,891 | 4.35 | 4.43 | 4.13 | ||
| Primary opioid at admission | 7067.93 | <0.0001 | ||||
| Heroin | 1,127,347 | 80.48 | 78.71 | 84.96 | ||
| Prescription or other opioids | 273,461 | 19.52 | 21.29 | 15.04 | ||
| Intravenous drug user at admission | ||||||
| No | 392,538 | 28.02 | 28.07 | 27.90 | 4.43 | 0.04 |
| Yes | 1,008,270 | 71.98 | 71.93 | 72.10 | ||
| Alcohol reported at admission | 9210.98 | <0.0001 | ||||
| No | 1,168,972 | 83.45 | 81.56 | 88.25 | ||
| Yes | 231,836 | 16.55 | 18.44 | 11.75 | ||
| Cocaine reported at admission | 254.82 | <0.0001 | ||||
| No | 1,075,468 | 76.77 | 77.13 | 75.87 | ||
| Yes | 325,340 | 23.23 | 22.87 | 24.13 | ||
| Methamphetamine reported at admission | 1718.54 | <0.0001 | ||||
| No | 1,257,633 | 89.78 | 89.11 | 91.47 | ||
| Yes | 143,175 | 10.22 | 10.89 | 8.53 | ||
| Treatment referral source | 54555.88 | <0.0001 | ||||
| Individual/self-referred | 782,655 | 55.87 | 50.80 | 68.75 | ||
| Substance abuse or HC provider | 280,565 | 20.03 | 20.43 | 19.01 | ||
| School, EAP, or community | 101,808 | 7.27 | 7.78 | 5.98 | ||
| Criminal justice system | 235,780 | 16.83 | 21.00 | 6.27 | ||
Compared to discharges with no dual MHD, those with a dual MHD had significantly higher odds of MAT receipt in expansion (aOR = 1.07, 95% CI = 1.04–1.10, p<0.0001) and non-expansion states (aOR = 1.25, 95% CI = 1.16–1.35, p<0.0001) (Table 2). Although the overall magnitude of the association was higher in non-expansion states aggregated across four years, the odds of MAT receipt increased over time among discharges with a dual MHD (versus no MHD) in expansion states, and decreased over time in non-expansion states. Notably, by 2017, a dual MHD was positively associated with MAT receipt in expansion states (aOR = 1.43, 95% CI = 1.38–1.47, p<0.0001) and negatively associated with MAT receipt in non-expansion states (aOR = 0.85, 95% CI = 0.79–0.93, p<0.0001).
Table 2:
Multivariable logistic regression with two-way interactions modeling MAT receipt among treatment episodes with heroin or other opioids reported as primary substances of abuse at treatment admission (TEDS-D, 2014–2017, n=1,400,808)
| Expansion states |
Non-expansion states |
|||||
|---|---|---|---|---|---|---|
| Variables | aOR | 95% CI | p | aOR | 95% CI | p |
| Main effect | ||||||
| Dual mental health diagnosis | ||||||
| No | Ref. | Ref. | ||||
| Yes | 1.07 | 1.04, 1.10 | <0.0001 | 1.25 | 1.16, 1.35 | <0.0001 |
| Interactions | ||||||
| Dual mental health diagnosis | ||||||
| Yes vs. no (ref) | ||||||
| White men | 1.34 | 1.32, 1.36 | <0.0001 | 1.33 | 1.29, 1.39 | <0.0001 |
| White women | 1.14 | 1.12, 1.16 | <0.0001 | 1.40 | 1.34, 1.45 | <0.0001 |
| Hispanic men | 1.32 | 1.28, 1.36 | <0.0001 | 1.16 | 0.98, 1.36 | 0.07 |
| Hispanic women | 1.05 | 1.01, 1.10 | 0.01 | 1.91 | 1.60, 2.29 | <0.0001 |
| Black men | 1.29 | 1.24, 1.34 | <0.0001 | 0.86 | 0.77, 0.97 | 0.01 |
| Black women | 1.16 | 1.10, 1.22 | <0.0001 | 0.92 | 0.80, 1.06 | 0.26 |
| AIAN men | 0.91 | 0.79, 1.04 | 0.14 | 1.53 | 1.07, 2.18 | 0.02 |
| AIAN women | 0.58 | 0.52, 0.66 | <0.0001 | 1.20 | 0.82, 1.73 | 0.35 |
| Dual mental health diagnosis | ||||||
| Yes vs. no (ref) | ||||||
| 2014 | 0.75 | 0.73, 0.78 | <0.0001 | 1.46 | 1.34, 1.61 | <0.0001 |
| 2015 | 0.99 | 0.96, 1.02 | 0.48 | 1.53 | 1.41, 1.68 | <0.0001 |
| 2016 | 1.22 | 1.18, 1.26 | <0.0001 | 1.26 | 1.16, 1.38 | <0.0001 |
| 2017 | 1.43 | 1.38, 1.47 | <0.0001 | 0.85 | 0.79, 0.93 | <0.0001 |
Model adjusted for age group, educational attainment, primary opioid of abuse at treatment admission, intravenous drug user at treatment admission, alcohol/cocaine/methamphetamine reported at treatment admission, and treatment referral source
Adjusted alpha threshold for statistical significance is p<0.0001.
The association between MAT receipt and dual MHD varied widely within racial/ethnic/gender groups and between Medicaid expansion statuses. The strongest positive association was observed among Hispanic women in non-expansion states (aOR = 1.91, 95% CI = 1.60–2.29, p<0.0001). The only significant negative association was observed among AI/AN women in expansion states, such that AI/AN women with dual MHD had lower odds of MAT receipt, compared to AI/AN women without dual MHD (aOR = 0.58, 95% CI = 0.52–0.66, p<0.0001). White men and White women were the only groups to demonstrate significant positive associations in both expansion and non-expansion states. Conversely, AI/AN men were the only group to demonstrate no significant associations in either expansion or non-expansion states.
5.1. Discussion
Our findings that MAT receipt increased among treatment discharges in expansion states is aligned with other reports indicating a general positive association between Medicaid expansion and MAT availability and utilization (Meinhofer & Witman, 2018; Sharp et al., 2018; Wen et al., 2017). Our findings are also nuanced, however, in that the odds of MAT receipt in expansion states were not equal among treatment discharges with dual MHDs and within racial/ethnic/gender groups. Our report highlights the importance of health disparities frameworks and analyzing differential trends by subpopulations.
Dual MHDs are increasingly common among those with OUD (Campbell et al., 2018; Sullivan et al., 2006). Our findings that treatment discharges with dual MHDs are more likely to receive MAT are somewhat at odds with previous reports indicating those with dual MHD/OUD are less likely to received integrated behavioral health care and are a higher risk of overdose, compared to those with OUD only (Johnson et al., 2013; Novak et al., 2019). Future studies may investigate specific mechanisms that enable MAT receipt among treatment clients with dual MHDs, which may include relationships or interactions with MAT providers, or an increase of integrated specialty mental health services into treatment settings.
We noted several findings aligned with our framework of intersectionality and health disparities. Medicaid expansion is broadly associated with an increase in coverage for mental health services (Han et al., 2015). Our findings complement this report, such that dual MHDs were positively associated with MAT receipt in later years following the adoption of Medicaid expansions in some states. White, Black, and Hispanic men with dual MHDs generally demonstrated higher odds of MAT receipt than their female counterparts. Taken together, we posit that women with co-occurring MHDs and OUDs in expansion states may not be as well positioned to benefit from Medicaid coverage that includes payments for MAT. This may partially explain our findings that showed higher odds of men receiving MAT.
Dual MHDs were associated with high odds of MAT among certain sub-groups, namely Hispanic women in non-expansion states. Hispanics in non-expansion states are more likely than Whites and Blacks to be uninsured (Lee & Porell, 2018), but it is unknown whether uninsured rates vary by gender within the Hispanic group. Nevertheless, high rates of uninsured among Hispanics in non-expansion states seems contrary to our strong results among Hispanic women. This finding remained challenging to interpret, such that some underlying latent factor may be influencing the high odds of MAT receipt among Hispanic women with dual MHDs in non-expansion states.
Medicaid covers over a quarter of AI/AN in the US (Artiga et al., 2017), but Medicaid expansions have not improved access to MAT services equally between states, with some expansion states demonstrating the poorest MAT utilization in the nation (Clemans-Cape et al., 2019). Importantly, despite the overall MAT benefits seen in expansion states, we found that AI/AN women with co-occurring MHDs living in expansion states demonstrated lower odds of MAT receipt (versus AI/AN women with no MHDs). AI/AN individuals – and AI/AN women in particular – may be particularly negatively affected by the convergence of multiple health disparities, which may otherwise be buffered by benefits inherent in Medicaid coverage. Future research may address treatment experiences that are unique to AI/AN women, which may help partially explain why AI/AN women with dual MHDs are less likely than those with dual MHDs to receive MAT. Efforts targeting MAT uptake among AI/AN with MHD and OUD diagnoses are needed to more effectively treat OUDs in vulnerable groups. In line with recent calls by Venner and colleagues (Venner et al., 2018) and Tipps and colleagues (Tipps et al., 2018), MAT services that primarily serve AI/AN groups should reflect traditional AI/AN healing and cultural approaches to medicine.
Our study demonstrated differential associations within and between Medicaid-expansion and non-expansion states. Key factors in the ongoing battle against the opioid crisis include protecting existing Medicaid programs, identifying characteristics of non-expansion states that may enable MAT receipt among some subgroups, and tailoring MAT promotion to specific groups by considering racial/ethnic differences and dual MHD status.
5.1.1. Limitations
Our definition of MAT included a single grouping of methadone or buprenorphine. However, these medications differ, and our findings of race/ethnicity/gender disparities in MAT may be driven by one treatment modality or the other. Future research may address differences between methadone and buprenorphine by disaggregating study outcomes by specific MAT type.
Geographic and data restrictions may have influenced the results of this study. Georgia, Oregon, and West Virginia did not report data in both 2016 and 2017, so were therefore excluded from our regression analyses.
TEDS-D data includes characteristics of treatment discharges, not individuals, meaning that individuals who are discharged twice will be counted twice. Our analytic approach assumes independent observations; in this sense, it is important to interpret our findings as they relate to treatment discharges, not individual treatment participants.
5.1.2. Conclusion
We identified differential associations between MAT receipt and dual MHD by race/ethnicity/gender, state-level Medicaid expansion status, and year. Dual MHDs were positively associated with MAT receipt, most notably in later years within expansion states. However, dual MHDs were not predictive of MAT receipt in Medicaid expansion states equally for all groups – AI/AN women with comorbid MHDs and OUDs in Medicaid expansion states were at a high risk of not receiving MAT. We also identified wide racial/ethnic/gender differences in MAT receipt between expansion statuses.
Our results highlight the importance of considering the cumulative effect of multiple marginalizing characteristics as factors predicting access to MAT among vulnerable OUD treatment clients. We found that Medicaid expansion is not a universal panacea for OUD treatment initiation. Clinicians treating OUD should integrate a nuanced and culturally centered approach, recognizing the dynamic continuum of OUD and MHD services. Programs and clinicians that culturally tailor decisions to initiate MAT may better meet the needs of high-risk, historically disadvantaged clients.
References
- Abraham AJ, Andrews CM, Yingling ME, et al. (2018). Geographic disparities in availability of opioid use disorder treatment for Medicaid enrollees. Health Serv Res, 53(1), 389–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderks C (2017). Trends in the use of methadone, buprenorphine, and extended-release naltrexone at substance abuse treatment facilities: 2003–2015 (update) Substance Abuse and Mental Health Services Administration; The CBHSQ Report: Short Report. Bethesda, MD. [PubMed] [Google Scholar]
- Alegria M, Carson NJ, Goncalves M, et al. (2011). Disparities in treatment for substance use disorders and co-occurring disorders for ethnic/racial minority youth. J Am Acad Child Adolesc Psychiatry, 50(1), 22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali M, Teich J, & Mutter R (2017). Reasons for not seeking substance use disorder treatment: Variations by health insurance coverage. J Beh Serv Res, 44(1), 63–74. [DOI] [PubMed] [Google Scholar]
- Andrews C, Pollack H, Abraham A, et al. (2019). Medicaid coverage in substance use disorder treatment after the Affordable Care Act. J Subst Abuse Treat, 102, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artiga S, Orgera K, & Damico A (2019). Changes in health coverage by race and ethnicity since implementation of the ACA, 2013–2017 Henry J. Kaiser Family Foundation; Issue Brief: Disparities Policy. San Francisco, CA. [Google Scholar]
- Artiga S, Stephens J, & Damico A (2015). The impact of the coverage gap in states not expanding Medicaid by race and ethnicity Henry J. Kaiser Family Foundation; The Kaiser Commission on Medicaid and the Uninsured, April 2015 (Issue Brief). [Google Scholar]
- Artiga S, Ubri P, & Foutz J (2017). Medicaid and American Indian and Alaska Natives Henry J. Kaiser Family Foundation; Medicaid. San Francisco, CA. [Google Scholar]
- Becker JB, & Mazure CM (2019). The federal plan for health science and technology’s response to the opioid crisis: understanding sex and gender differences as part of the solution is overlooked. Biol Sex Differ, 10(1), 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buck J (2011). The looming expansion and transformation of public substance abuse treatment under the Affordable Care Act. Health Affairs, 30(8), 1402–1410. [DOI] [PubMed] [Google Scholar]
- Campbell CI, Bahorik AL, VanVeldhuisen P, et al. (2018). Use of a prescription opioid registry to examine opioid misuse and overdose in an integrated health system. Prev Med, 110, 31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantone R, Garvey B, O’Neill A, et al. (2019). Predictors of medication-assisted treatment initiation for opioid use disorder in an interdisciplinary primary care model. J Am Board Fam Med, 32, 724–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpentier P, Krabbe P, Van Gogh M, et al. (2009). Psychiatric comorbidity reduces quality of life in chronic methadone maintained patients. Am J Addict, 18(6), 470–480. [DOI] [PubMed] [Google Scholar]
- Clemans-Cape L, Lynch V, Winisky E, et al. (2019). State variation in Medicaid prescriptions for opioid use disorder from 2011 to 2018. The Urban Institute Health Policy Center; Washington, D.C. [Google Scholar]
- Creedon TB, & Cook BL (2016). Access to mental health care increased but not for substance use, while disparities remain. Health Affairs, 35(6), 1017–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K (1989). Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist policies. University of Chicago Legal Forum, 1(8), 139–167. [Google Scholar]
- Crenshaw K (1991). Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Law Review, 43(6), 1241–1299. [Google Scholar]
- Dunlap B, & Cifu AS (2016). Clinical management of opioid use disorder. JAMA, 316(3), 338–339. [DOI] [PubMed] [Google Scholar]
- Friedman J, Kim D, Schneberk T, et al. (2019). Assessment of racial/ethnic and income disparities in the prescription of opioids and other controlled medications in California. JAMA Internal Medicine, E-publication ahead of print; Published online on February 11, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg RK, Fulton-Kehoe D, & Franklin GM (2017). Patterns of opioid use and risk of opioid overdose death among Medicaid patients. Med Care, 55(7), 661–668. [DOI] [PubMed] [Google Scholar]
- Garrison YL, Sahker E, Yeung, et al. (2018). Asian American and Pacific Islander substance use treatment completion. Psychol Serv. [DOI] [PubMed] [Google Scholar]
- Gary FA (2005). Stigma: Barrier to mental health care among ethnic minorities. Iss Mental Health Nurs, 26(10), 979–999. [DOI] [PubMed] [Google Scholar]
- Han B, Gfroerer J, Kuramoto S, et al. (2015). Medicaid expansion under the Affordable Care Act: Potential changes in receipt of mental health treatment among low-income nonelderly adults with serious mental illness. Am J Public Health, 105(10), 1982–1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry J. Kaiser Family Foundation. (2019). Status of state Medicaid expansion decisions: Interactive map. San Francisco, CA: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/ [Google Scholar]
- Johnson E, Lanier W, Merrill R, et al. (2013). Unintentional prescription opioid-related overdose deaths: Description of decedents by next of kin or best contact, Utah 2008–2009. J Gen Intern Med, 28(4), 522–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson EM, Lanier WA, Merrill RM, et al. (2013). Unintentional prescription opioid-related overdose deaths: description of decedents by next of kin or best contact, Utah, 2008–2009. J Gen Intern Med, 28(4), 522–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K, Jones C, Compton W, et al. (2018). Federal response to the opioid crisis. Current HIV/AIDS Rep, 15(4), 293–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krawczyk N, Feder KA, Fingerhood,et al. (2017). Racial and ethnic differences in opioid agonist treatment for opioid use disorder in a U.S. national sample. Drug Alcohol Depend, 178, 512–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, & Porell F (2018). The effect of the Affordable Care Act Medicaid Expansion on disparities in access to care and health status. Med Care Res Rev. E-publication ahead of print. [DOI] [PubMed] [Google Scholar]
- Lui CK, Sterling SA, Chi FW, et al. (2017). Socioeconomic differences in adolescent substance abuse treatment participation and long-term outcomes. Addict Beh, 68, 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manchikanti L, Helm S, Fellows B, et al. (2012). Opioid epidemic in the United States. Pain Physician, 15(3 Suppl), Es9–38. [PubMed] [Google Scholar]
- McElrath K, & Joseph H (2018). Medication-Assisted Treatment (MAT) for Opioid Addiction: Introduction to the Special Issue. Subst Use Misuse, 53(2), 177–180. [DOI] [PubMed] [Google Scholar]
- McMorrow S, Kenney G, Long S, et al. (2016). Medicaid expansions from 1997–2009 increased coverage and improved access and mental health outcomes for low-income parents. Health Serv Res, 51(4), 1347–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinhofer A, & Witman A (2018). The role of health insurance on treatment for opioid use disorders: Evidence frm the Affordable Care Act Medicaid expansions. J Health Econ, 60, 177–197. [DOI] [PubMed] [Google Scholar]
- Mennis J, & Stahler GJ (2016). Racial and ethnic disparities in outpatient substance use disorder treatment episode completion for different substances. Journal Subst Abuse Treat, 63, 25–33. [DOI] [PubMed] [Google Scholar]
- Mennis J, Stahler GJ, El Magd SA, et al. (2019). How long does it take to complete outpatient substance use disorder treatment? Disparities among Blacks, Hispanics, and Whites in the US. Addict Beh, 93, 158–165. [DOI] [PubMed] [Google Scholar]
- Mogil JS, & Bailey AL (2010). Sex and gender differences in pain and analgesia. Progress Brain Res, 186, 140–157. [DOI] [PubMed] [Google Scholar]
- Musey PI Jr, Linnstaedt SD, Platts-Mills TF, et al. (2014). Gender differences in acute and chronic pain in the emergency department: results of the 2014 Academic Emergency Medicine consensus conference pain section. Acad Emer Med, 21(12), 1421–1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak P, Feder KA, Ali MM, et al. (2019). Behavioral health treatment utilization among individuals with co-occurring opioid use disorder and mental illness: Evidence from a national survey. J Subst Abuse Treat, 98, 47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M, Wall M, Barry C, et al. (2018). Impact of Medicaid expansion on coverage and treatment of low-income adults with substance use disorders. Health Affairs, 37(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA (2016). Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR, 65. [DOI] [PubMed] [Google Scholar]
- Sahker E, Toussaint MN, Ramirez M, et al. (2015). Evaluating racial disparity in referral source and successful completion of substance abuse treatment. Addict Behav, 48, 25–29. [DOI] [PubMed] [Google Scholar]
- Saloner B, & Cook BL (2013). Blacks and Hispanics are less likely than whites to complete addiction treatment, largely due to socioeconomic factors. Health Affairs, 32(1), 135–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. (Cary, NC). SAS/STAT. Cary, NC. [Google Scholar]
- Schafer I, Eiroa-Orosa FJ, Verthein U, et al. (2010). Effects of psychiatric comorbidity on treatment outcome in patients undergoing diamorphine or methadone maintenance treatment. Psychopathology, 43(2), 88–95. [DOI] [PubMed] [Google Scholar]
- Serdarevic M, Striley C, & Cottler L (2018). Gender differences in prescription opioid use. Curr Opin Psych, 30(4), 238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp A, Jones A, Sherwood J, et al. (2018). Impact of Medicaid expansion on access to opioid anelgesic medications and medication-assisted treatment. Am J Public Health, 108(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaniol ED, Smith WB, Thomas DA, et al. (2019). Addressing the opioid crisis: social and behavioral research contributions at the National Institutes of Health. Translational Beh Med. E-publication ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahler GJ, & Mennis J (2018). Treatment outcome disparities for opioid users: Are there racial and ethnic differences in treatment completion across large US metropolitan areas? Drug Alc Depend, 190, 170–178. [DOI] [PubMed] [Google Scholar]
- Stein BD, Dick AW, Sorbero M, et al. (2018). A population-based examination of trends and disparities in medication treatment for opioid use disorders among Medicaid enrollees. Subst Abuse, 39(4), 419–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Data Archive. (2018). Treatment Episode Data Set: Discharges (TEDS-D) Substance Abuse and Mental Health Services Administration, Treatment Episode Data Set: Discharges (TEDS-D). Rockville, MD. [Google Scholar]
- Sullivan MD, Edlund MJ, Zhang L, et al. (2006). Association between mental health disorders, problem drug use, and regular prescription opioid use. Arch Intern Med, 166(19), 2087–2093. [DOI] [PubMed] [Google Scholar]
- Tipps R, Buzzard G, & McDougall J (2018). The opioid epidemic in Indian Country. J Law Med Ethics, 46(2), 422–436. [DOI] [PubMed] [Google Scholar]
- Venner K, Donovan D, Campbell A, et al. (2018). Future directions for medication assisted treatment for opioid use disorder with American Indian/Alaska Natives. Addict Behav, 86, 111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N, & McLellan A (2016). Opioid abuse in chronic pain - Misconceptions and mitigation strategies. N Engl J Med, 374, 1253–1263. [DOI] [PubMed] [Google Scholar]
- Wen H, Hockenberry J, Borders T, et al. (2017). Impact of Medicaid expansion on Medicaid-covered utilization of buprenorphine for opioid use disorder treatment. Medical Care, 55(4), 336–341(336). [DOI] [PubMed] [Google Scholar]
- Wu L-T, Zhu H, & Swartz MS (2016). Treatment utilization among persons with opioid use disorder in the United States. Drug Alc Depend, 169, 117–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue D, Rasmussen P, & Ponce N (2018). Racial/ethnic differential effects of Medicaid expansion on health care access. Health Serv Res, 53(5), 3640–3656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoorob R, Kowalchuk A, & Mejia de Grubb M (2018). Buprenorphine therapy for opioid use disorder. Am Fam Physician, 97(5), 313–320. [PubMed] [Google Scholar]