Abstract
We report an extremely rare case of acute inflammatory myopathy during combination chemotherapy with docetaxel and transtuzumab for metastatic breast carcinoma in a 44-year-old female patient. Despite the significant response in the follow-up fluorodeoxyglucose (FDG) positron emission tomography/computed tomography, of the underlying malignancy to the chemotherapeutic regimen, there was diffusely increased FDG uptake in the upper and lower limb muscles with associated painful, proximal muscle weakness. These symptoms regressed after the discontinuation of docetaxel and the administration of corticosteroids, suggesting it to be the drug-induced myositis.
Keywords: Docetaxel, fluorodeoxyglucose positron emission tomography/computed tomography, myositis
A 44-year-old woman, presented to our hospital with a right breast lump. Trucut biopsy from the right breast lump showed invasive mammary carcinoma, no special type (Ductal, not otherwise specified), Nottingham score 9, Grade III, with a hormonal status of estrogen receptor −ve, progesterone receptor −ve, and human epidermal growth factor receptor 2neu +ve. Staging work up showed, right breast mass along with right axillary and right internal mammary lymph nodes. Then, the patient received four cycles of epirubicin and cyclophosphamide. Interim positron emission tomography/computed tomography (PET/CT) showed [Figure 1a- maximum intensity projection image] right breast mass [Figure 1f and g] along with right axillary [Figure 1d and e], right supraclavicular [Figure 1b and c] and mediastinal lymph nodal and presternal subcutaneous nodule metastases [Figure 1f and g]. Following this the patient was put on docetaxel and transtuzumab and underwent another PET/CT after four cycles. This PET/CT showed near complete metabolic response to the therapy with only minimal residual right breast lesion [Figure 2a, d and e]. However, in addition to that, the PET/CT images showed diffusely increased fluorodeoxyglucose (FDG) uptake in the skeletal muscles predominantly around shoulder and hip girdles [Figure 2a-g]. The patient also had an associated history of muscle and joint pains with weakness involving bilateral upper and lower limbs, approximately 3 weeks after the starting of docetaxel, which progressed gradually after each cycle. In suspicion of docetaxel induced myositis, erythrocyte sedimentation rate (ESR), and creatine phosphokinase (CPK) was advised which were found out to be raised, 41 mm/h (normal <20 mm/h) and 395 u/l (normal range: 30–135 u/l), respectively. Hence, docetaxel was stopped, and the patient was put on tapered doses of prednisolone, to which she responded quickly. The ESR and CPK also came down to normal within a week. Instant response to corticosteroid and withdrawal of docetaxel, confirmed the diagnosis of docetaxel-induced myositis.
Figure 1.
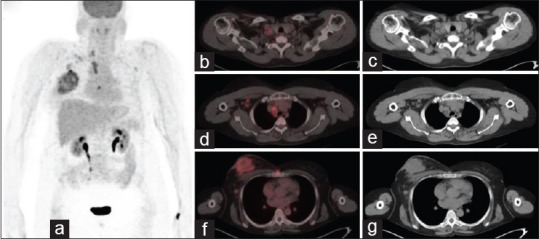
Interim positron emission tomography/computed tomography showed right breast mass along with right axillary, right supraclavicular and mediastinal lymph nodal and presternal subcutaneous nodule metastases (a) showing maximum intensity projection image and (b-g) showing fused positron emission tomography/computed tomography images and computed tomography images
Figure 2.
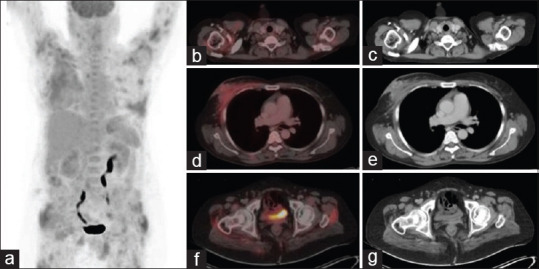
Follow-up positron emission tomography/computed tomography showed near complete metabolic response to the therapy with only minimal residual right breast lesion (a, d, e). Diffusely increased fluorodeoxyglucose uptake in the skeletal muscles predominantly around shoulder and hip girdles. (a) Showing maximum intensity projection and (b-g) showing fused positron emission tomography/computed tomography and computed tomography images of muscle uptake
Docetaxel is a taxane-based chemotherapeutic agent that promotes the polymerization and inhibits depolymerization of microtubules causing interference of cell division. It has been widely used in breast, ovarian, refractory prostate, head and neck, gastric, and non-small cell lung cancers.[1] The common side effects of taxane agents include peripheral edema and fluid retention; however, it can also cause dose-dependent severe myelosuppression, most commonly neutropenia. Myalgia and neuropathies were not noted as common taxane side effects. There are few studies in the late 1980s to mid-1990s which reported peripheral neuropathy[2,3,4] and myalgias[5,6,7,8,9] as side effects. This side effect can be easily overlooked by physicians particularly in the setting of other existing causative factors. However, as it is treatable, we should have a higher index of suspicion when monitoring patients on taxane therapies. FDG PET-CT has already been used for different inflammatory myopathies which showed increased tracer uptake in the inflamed muscles.[10,11,12,13,14,15] Hence, it is important for nuclear medicine physicians to be familiar with FDG PET-CT findings attributable to chemotherapy induced myositis so that an appropriate differential diagnosis can be established. Our case demonstrates a rare side effect of docetaxel on 18F FDG PET/CT. These rarer side-effects may become more important in future clinical practice as the use of docetaxel increases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bachegowda LS, Makower DF, Sparano JA. Taxanes: Impact on breast cancer therapy. Anti Cancer Drugs. 2014;25:512–21. doi: 10.1097/CAD.0000000000000090. [DOI] [PubMed] [Google Scholar]
- 2.Hilkens PH, Verweij J, Stoter G, Vecht CJ, van Putten WL, van den Bent MJ. Peripheral neurotoxicity induced by docetaxel. Neurology. 1996;46:104–8. doi: 10.1212/wnl.46.1.104. [DOI] [PubMed] [Google Scholar]
- 3.Hilkens PH, Pronk LC, Verweij J, Vecht CJ, van Putten WL, van den Bent MJ. Peripheral neuropathy induced by combination chemotherapy of docetaxel and cisplatin. Br J Cancer. 1997;75:417–22. doi: 10.1038/bjc.1997.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiernik PH, Schwartz EL, Strauman JJ, Dutcher JP, Lipton RB, Paietta E. Phase I clinical and pharmacokinetic study of taxol. Cancer Res. 1987;47:2486–93. [PubMed] [Google Scholar]
- 5.Donehower RC, Rowinsky EK, Grochow LB, Longnecker SM, Ettinger DS. Phase I trial of taxol in patients with advanced cancer. Cancer Treat Rep. 1987;71:1171–7. [PubMed] [Google Scholar]
- 6.Sulkes A, Beller U, Peretz T, Shacter J, Hornreich G, McDaniel C, et al. Taxol: Initial Israeli experience with a novel anticancer agent. Isr J Med Sci. 1994;30:70–8. [PubMed] [Google Scholar]
- 7.Valero V, Holmes FA, Walters RS, Theriault RL, Esparza L, Fraschini G, et al. Phase II trial of docetaxel: A new, highly effective antineoplastic agent in the management of patients with anthracycline-resistant metastatic breast cancer. J Clin Oncol. 1995;13:2886–94. doi: 10.1200/JCO.1995.13.12.2886. [DOI] [PubMed] [Google Scholar]
- 8.Giaccone G, Huizing M, Huinink WT, Koolen M, Postmus P, van Kralingen K, et al. Preliminary results of two dose-finding studies of paclitaxel (taxol) and carboplatin in non-small cell lung and ovarian cancer: A European Cancer Center effort. Seminars Oncol. 1994;21:34–8. [PubMed] [Google Scholar]
- 9.Rowinsky EK, Burke PJ, Karp JE, Tucker RW, Ettinger DS, Donehower RC. Phase I and pharmacodynamics study of taxol in refractory acute leukemias. Cancer Res. 1989;49:4640–7. [PubMed] [Google Scholar]
- 10.Owada T, Maezawa R, Kurasawa K, Okada H, Arai S, Fukuda T, et al. Detection of inflammatory lesions by f-18 fluorodeoxyglucose positron emission tomography in patients with polymyositis and dermatomyositis. J Rheumatol. 2012;39:1659–65. doi: 10.3899/jrheum.111597. [DOI] [PubMed] [Google Scholar]
- 11.Pipitone N, Versari A, Zuccoli G, Levrini G, Macchioni P, Bajocchi G, et al. 18F-Fluorodeoxyglucose positron emission tomography for the assessment of myositis: A case series. Clin Exp Rheumatol. 2012;30:570–3. [PubMed] [Google Scholar]
- 12.Kashyap R, Agrawal K, Singh H, Mittal BR. Disease- and treatment-related complication on f-18-fluorodeoxyglucose positron emission tomography/computed tomography in oncology practice: A pictorial review. Indian J Nucl Med. 2017;32:304–15. doi: 10.4103/ijnm.IJNM_78_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thulasidoss K, Sridharan S, Ashokan L, Chandra P. A rare case of sarcoidosis presenting as diffuse contracturing granulomatous myositis on fluorodeoxyglucose positron emission tomography/computed tomography. Indian J Nucl Med. 2018;33:148–51. doi: 10.4103/ijnm.IJNM_154_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rayamajhi SJ, Gorla AK, Basher RK, Sood A, Mittal BR. Unsuspected active ulcerative colitis in a patient with dermatomyosits: A rare association detected on 18F-FDG PET/CT during the search for an occult malignancy. Indian J Nucl Med. 2017;32:130–2. doi: 10.4103/0972-3919.202238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sood A, Khadwal AR, Lukose T, Kumar R, Singh H, Bal A, et al. 18F-FDG PET/CT in graft versus host disease-associated polymyositis. Clin Nucl Med. 2020;45:e106–7. doi: 10.1097/RLU.0000000000002818. [DOI] [PubMed] [Google Scholar]


