Abstract
Background
The effect of COVID-19 on pediatric trauma rates is still largely under investigation. With the potential need to reallocate human and financial resources at this challenging time, it will be useful to have detailed descriptions of the rates of pediatric trauma and understanding of how the pandemic affects these rates.
Questions/Purposes
We sought to describe the effect of the COVID-19 pandemic on the number of acute pediatric trauma admissions and procedures performed in a level-I trauma center in Cork University Hospital, Ireland.
Methods
We compared the number of acute traumatic pediatric admissions and procedures that occurred during the first 4 weeks of a nationwide lockdown due to COVID-19 with that of the same 4-week period in each of the preceding 11 years. Seasonal variables were measured and controlled for using multivariate regression analysis.
Results
A total of 545 pediatric patients (under 16 years of age) were included. Over 12 years, the lowest number of acute traumatic pediatric admissions and procedures was recorded during the 2020 pandemic. There was a significant correlation between the number of school days and the number of acute traumatic admissions, as well as the procedures performed. The relationship between the number of school days and the number of trauma procedures was evident even when controlling for confounder variables of seasonal variation.
Conclusion
The COVID-19 pandemic significantly reduced the number of acute traumatic pediatric admissions and procedures performed in our level-I trauma center, likely because of a reduction in school days. With the reopening of schools, playgrounds, and sporting events, an increase in pediatric trauma admissions is anticipated. The results of this study can help prepare institutions and regulatory bodies to plan appropriately for this new phase.
Electronic supplementary material
The online version of this article (10.1007/s11420-020-09807-y) contains supplementary material, which is available to authorized users.
Keywords: SARS-CoV-2, COVID-19, level-1 trauma center, pediatric trauma
Introduction
The COVID-19 pandemic set off catastrophic and far-reaching effects across the globe. The global orthopedic community channeled its efforts to restructure services in this time of crisis. Elective practice was ceased in order to reduce the patient volume. Expedient communication has enabled the experiences of the international scientific community to be shared efficiently enough to begin to curtail the impact of this virus [6, 9–11, 14, 15].
The orthopedic community experienced disruption on a number of fronts, including considerable reductions in the volume of non-urgent surgical procedures [7]. Every facet of orthopedic training and education was affected to some degree [13]. Level-I trauma centers experienced a significant shift in referral patterns and had to accommodate the changing landscape at an accelerated rate [6]. For example, at Cork University Hospital, located in the second largest city in Ireland, many ambulatory trauma cases were diverted to peripheral units in an effort to reduce the volume of patients. The preservation and appropriate allocation of human and financial resources within the hospital system were paramount [4].
Our aim with this study was to characterise the number of acute pediatric trauma cases the number of acute procedures performed at a level-I trauma center in a 4-week period during the pandemic shutdown. In addition, we aimed to compare those numbers with those from the same 4-week period in each of the preceding 11 years, considering the variables that may have contributed to any patterns observed. Our hope was that such information could be used by institutions charged with allocating resources while providing a high standard of acute trauma care to pediatric patients during a crisis.
Methods
A comparative analysis was performed assessing all acute pediatric trauma admissions and trauma procedures during the first 4 weeks of a nationwide lockdown, which enforced closure of schools and playground and the cessation of all sporting activity. All acute pediatric admissions for trauma to the level-I trauma center in Cork University Hospital, Ireland, were analysed between the dates of March 13, 2020, and April 13, 2020. These results were then compared with the same period (March 13 to April 13) for the preceding 11 years. Initially, the rate of acute pediatric admissions was analysed as absolute numbers. In order to allow for fluctuation in the size of the pediatric population at risk, we calculated the incidence rate (events per person-time in years) to compare the pediatric trauma admission rate for each year across the 12-year period. Accurate pediatric population sizes were retrieved from the central statistics office. The number of non-accidental injury (NAI) cases (including child abuse) and infection cases during this period was also analysed and compared with the preceding years.
Patient variables were collected from the Hospital In-Patient Enquiry database, an institutional database that is populated prospectively with each pediatric admission. These records were cross-referenced with operating room logs to identify the surgical procedure (if any) undergone by the patient. All data relating to NAI was collated using the database formulated by the regional medical social worker department. Demographic variables included patient age, gender, mechanism of injury, anatomical site of injury, and type of procedure performed. In an attempt to control for the confounding variables that are known to affect the seasonal variation in pediatric trauma, these variables were recorded over the 4-week period in question using national meteorological data. They included the total number of school days in the 4-week period, the total number of weekend days in the period, the average number of daily sunshine hours, the average daily rainfall (mm), the average maximum daily temperature (°F) and the average minimum daily temperature (°F).
Descriptive statistics were used to summarise demographic data and the pattern of common fractures over the reported time period. In order to assess the association between the year of admission and the number of pediatric admissions and procedures performed, Pearson’s correlation coefficient was used; a positive r value indicated a positive correlation and a negative r value indicated a negative correlation between the two variables. When assessing seasonal factors and their influence on acute trauma admissions and procedures, Spearman’s rank correlation coefficient was used. Simple linear regression analyses were also used to visually assess the relationship between these two interval variables. When analysing the relationship between the number of school days and the number of acute surgical procedures performed, a simple linear regression analysis was performed. The result was illustrated using a scatterplot with regression line. Once the predictor variables were identified, a multivariate regression analysis was performed to eliminate the effect of any confounder variables. In all cases, a p value of 0.05 was taken to be significant. The statistical software used was Stata/IC 13.1 (StataCorp LP, College Station, TX, USA).
Results
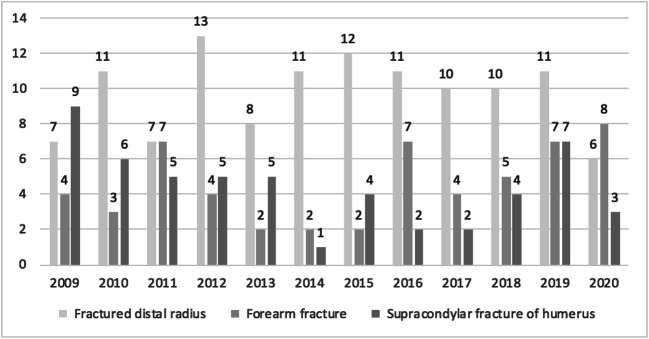
A total of 545 pediatric patients were admitted over the 12 4-week periods between the years of 2009 and 2020. All 545 admissions were acute in nature, 423 of these acute admissions were admitted for traumatic conditions and 365 of these underwent surgery for those traumatic conditions. The mean age of the entire cohort was 8.7 years (σ = 3.97, 1–15). The sample consisted of 59% males and 41% females. During the COVID-19 pandemic, the most common mechanism of injury for acute operative procedures was a fall from a standing height (75%). To summarise, one patient was the victim of a road traffic accident, one sustained a crush injury, one incident was activity-related and one was unrecorded. Over the 12-year period, the 3 most common injury types requiring admission were distal radius fractures (n = 117, 21.4%), bone forearm fractures (n = 55, 10%) and supracondylar fractures (n = 53, 9.7%) (Fig. 1).
Fig. 1.
Three commonest pediatric fractures from 2009 to 2020.
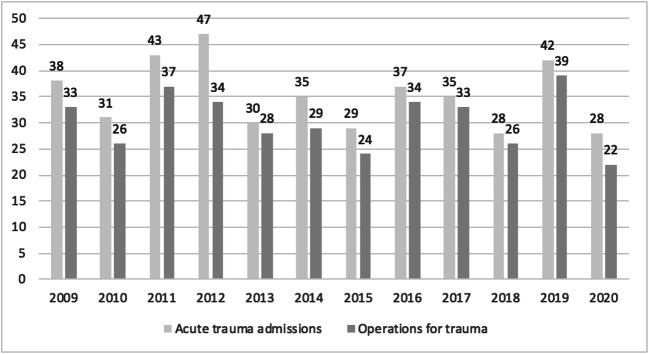
In total, over the 12 years between 2009 and 2020, the lowest number of admissions and surgical procedures for acute pediatric trauma were recorded during the pandemic in 2020 (Fig. 2). The mean number of trauma admissions in the 1-month periods between 2009 and 2019 was 35.9. In 2020, the number of trauma admissions was 28. The mean number of trauma procedures between 2009 and 2019 was 29.1. The number of trauma procedures in 2020 was 22. The size of the pediatric population at risk increased every year between 2009 and 2020. In 2009, the total pediatric population at risk was 132,700. By 2020, this figure had risen to 143,000. The incidence rate across the 12-year period was similar. In 2009, the incidence rate for acute trauma admission was 0.146 events per person-year. In 2015, the incidence rate was similar at 0.146 events per person-year. In 2020, the population at risk was at the highest recorded in the 12 years. In contrast, the number of trauma admissions was at its lowest in 2020 during the pandemic. This led to an incidence rate of 0.139 admissions per person-year. This was the lowest incidence rate recorded across the 12-year time period.
Fig. 2.
Acute pediatric admissions and surgical procedures from 2009 to 2020.
There were 372 operative cases in the entire cohort. Of these, 365 procedures were for trauma and seven procedures were for confirmed infection. In 2020, there were five distal radius closed reductions and casting, seven forearm closed reductions and casting and three closed reduction and K-wire insertions for supracondylar fractures. There were no admissions for suspected infection during the recorded 4-week period in 2020.
In considering the effect of the environment on our findings, we demonstrated a significant correlation between the increasing number of sunshine hours in a given period per year and the increasing number of acute admission for trauma (correlation coefficient + 0.18, p = 0.0003). There was also a significant positive correlation demonstrated between the maximum temperature and the number of acute traumatic admissions (correlation coefficient + 0.16, p = 0.002). In contrast, the mean rainfall in a given period per year was inversely related to the number of acute trauma admissions per year (correlation coefficient − 0.15, p = 0.0026). There was no relationship noted between minimum temperatures or the number of weekend days in a given period and the number of acute trauma admissions.
When analysing the number of school days in a given period and their relation to the number of acute traumatic admissions, we found a positive correlation of significance (r = 0.7, p = 0.037). This relationship was also confirmed with simple linear regression models (p = 0.037). When analysing the number of school days in a given period and its relation to the number of acute procedures for trauma, we found a positive correlation of significance (r = 0.77, p = 0.003). This relationship was confirmed with simple linear regression models (p = 0.0029). Visual scatterplots illustrated this relationship as in Fig. 3. When controlling for all confounder variables (sunshine hours and rainfall), we found a persistent predictive relationship between a reducing number of school days and a reducing number of acute traumatic procedures over the 12-year period (p = 0.015).
Fig. 3.
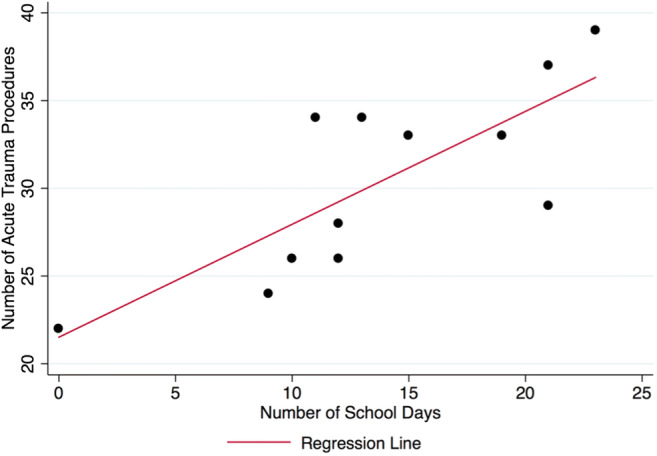
Linear regression model illustrating the relationship between the increasing number of school days and the number of acute pediatric trauma procedures.
The incidence of NAI for any given 4-week period assessed was low. During the 2020 time frame, there was one case of NAI reported in a 3-month-old infant. This is the youngest reported victim of NAI in the 12-year period. In 2019, there were four cases of NAI. The ages involved were 2 years, 9 years and 2 at 13 years of age. There was one case of NAI in a 4-year old in 2016. For the remaining 9 time periods, no cases of NAI were reported, so no meaningful associations were observed.
Over the 12 4-week periods between 2009 and 2020, there were 29 admissions for infection. In 2011, 2014 and 2020, there were no admissions for infection. Of the 29 patients who were admitted, seven underwent surgical intervention. Given the low incidence of infection, no statistical analysis was appropriate for this cohort.
Discussion
This aim of this study was to assess the effect of the COVID-19 pandemic on pediatric trauma from the perspective of a level-I trauma center in Cork, Ireland. It was observed that, over 12 4-week periods from 2009 to 2020, the lowest number of traumatic pediatric admissions and pediatric procedures occurred during the 2020 lockdown.
We note some limitations of this study. First, parents’ and patients’ fears of visiting the hospital during the COVID-19 pandemic may have delayed presentation. However, in a recent study of 1745 pediatric patients comparing a 1-month period under lockdown to a 1-month period during the previous year, Bram et al. found that there were no delays in time to presentation during lockdown [2]. Another limitation is our inability to specifically examine the effect of sporting activity, playground activity and other behaviors on the rate of acute trauma admissions and surgical procedures.
The 4-week period we studied, which took place at the beginning of lockdown, is a relatively short period of time. Accumulating data over a period of 12 years does, however, significantly increase the power of our study. Regarding NAI, child exposure time to potentially abusive parents in the home has increased along with rates of unemployment. This rate may continue to rise, so it is imperative that we continue to be vigilant in protecting children from these potentially lethal injuries when they present to our trauma centers.
Christey et al. illustrated a similar trend with a 48% reduction in pediatric admissions for a 2-week period during lockdown compared with a 2-week period preceding lockdown [3]. The researchers reported on a level-I trauma center in New Zealand, which has a similar rural and urban population profile as Ireland. We observed a similar trend. Further vigilant monitoring is still necessary, however, as lockdown continues and the risk of injuries is likely to increase with many households experiencing greater strain in different forms.
Explanations for our findings involve a number of factors. One contributing factor is environmental. Atherton et al. demonstrated the effect of temperature, sunshine hours and day of the week on pediatric trauma admissions [1]. Our analysis showed a significant correlation between increasing sunshine hours and increasing acute trauma admissions. An inverse correlation between rainfall and acute trauma admissions was also observed. Similar findings were reported over a 3-year period in 1993 by Masterson et al. [8]. This environmental contribution is intuitive as children are more likely to engage with potentially trauma-inducing activity with a higher number of sunshine hours and less likely to engage with these potentially dangerous activities when rainfall measurements are higher. Even during the pandemic, however, although children were not at school and playgrounds were closed, they were allowed to be outside as long as social distancing measures were observed.
The most relevant finding, with potentially far-reaching implications for the future, was a significant relationship between the number of schooldays and the number of acute pediatric trauma admissions (p = 0.03) and procedures performed (p = 0.003). With an increasing number of school days in a given date range, it was found that the number of trauma procedures increased significantly. For example, in the 4 weeks, we considered that in 2019, there were 23 school days (the most in the 12-year period). During that same period, there were also 42 admissions and 39 procedures performed. The year 2015 had the second lowest number of school days after 2020. It also had the second lowest number of admissions (n = 29) and procedures (n = 24). The lowest number of school days (n = 0) and the lowest number of admissions (n = 28) and procedures (n = 22) were recorded during the lockdown period of 2020. The effect of increasing school day numbers on increasing acute trauma procedures was observed even when controlling for all known seasonal predictor variables on multivariate regression analysis (p = 0.015).
We surmise that during the pandemic, children are not engaging with activities on local playgrounds or climbing equipment. They are also not participating in any potentially hazardous sporting activity at school or elsewhere. This would explain the pattern of traumatic injuries we have described over the last 12 years in our institution. In normal times, children at school are interacting more with their peers, playing on potentially hazardous equipment, and participating in all kinds of school-based sporting activity. In line with these findings, a recent article by Segal et al. confirmed that daily fracture rates significantly reduced from 6.62 to 4.45 per day when comparing fracture rates on a school day and fracture rates on a summer vacation day (p < 0.01) [12].
The implications for both trauma centers and regulatory bodies are such that during the pandemic, pediatric trauma volumes are significantly reduced. In treatment centers, staff and resource allocation may be amended to better serve patients suffering from COVID-19 without significantly affecting the standard of trauma care provided to pediatric populations. Many recommendations surrounding the management of pediatric orthopedic patients have become available [5]. We know that level-I trauma centers have been required to make drastic changes to their normal services regarding the redeployment of staff and accommodation of an increasing volume of patients with COVID-19-related respiratory conditions [6]. These findings may help shape future recommendations. Specifically, it may be reasonable to first consider the reallocation of staff involved in pediatric trauma to other areas of respiratory service that will potentially be overwhelmed by the burden of COVID-19.
In addition, the timing of the reopening of schools and their associated recreational and sporting activities should be carefully considered by all involved parties as there will predictably be an increase in the staffing and resources required to treat an increasing number of pediatric trauma patients when the reopening occurs. These decisions made in the context of COVID-19 should be measured and thoroughly considered. Our findings help to characterise the pattern of pediatric trauma that a level-I trauma center can expect to see over the coming weeks to months and the reasons why this change in pattern has occurred.
In conclusion, the COVID-19 pandemic and shutdown reduced the number of acute pediatric admissions and procedures performed for acute pediatric trauma in our level-I trauma center. For the same date range over the past 12 years, a reduction in the number of school days for a given period was associated with a significant reduction in the number of acute traumatic admissions and procedures performed. An increase in pediatric trauma admissions with the national reopening of schools, playgrounds, and sporting events is anticipated. Knowledge of the dynamics around pediatric trauma during this and potentially future pandemics will allow institutions to allocate staff and resources more appropriately. These findings will be useful for regulatory bodies that are responsible for the reopening of schools, sporting events and society as a whole.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Compliance with Ethical Standards
Conflict of Interest
Gerard A. Sheridan, Sch, MB, BAO, MCh, Matthew Nagle, MD, FRCS, Shane Russell, MD, Stanly Varghese, MD, Padhraig F. O’Loughlin, MD, FRCS, Sinead Boran, MD, FRCS, Colm Taylor, MD, FRCS, James A. Harty, MD, FRCS declare that they have no conflict of interest.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
References
- 1.Atherton WG, Harper WM, Abrams KR. A year’s trauma admissions and the effect of the weather. Injury. 2005;36(1):40–46. doi: 10.1016/j.injury.2003.10.027. [DOI] [PubMed] [Google Scholar]
- 2.Bram JT, Johnson MA, Magee LC, et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop. 2020;40(8):373–379. doi: 10.1097/BPO.0000000000001600. [DOI] [PubMed] [Google Scholar]
- 3.Christey G, Amey J, Campbell A, Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;133(1513):81–88. [PubMed] [Google Scholar]
- 4.Coccolini F, Perrone G, Chiarugi M, et al. Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020;15(1):25. doi: 10.1186/s13017-020-00307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farrell S, Schaeffer EK, Mulpuri K. Recommendations for the care of pediatric orthopaedic patients during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):e477–e486. doi: 10.5435/JAAOS-D-20-00391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Konda SR, Dankert JF, Merkow D, et al. COVID-19 Response in the global epicenter: converting a New York City Level 1 orthopedic trauma service into a hybrid orthopedic and medicine COVID-19 management team. J Orthop Trauma. 2020;34(8):411–417. doi: 10.1097/BOT.0000000000001792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liebensteiner MC, Khosravi I, Hirschmann MT, Heuberer PR; Board of the AGA-Society of Arthroscopy and Joint-Surgery, Thaler M Massive cutback in orthopaedic healthcare services due to the COVID-19 pandemic. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1705–1711. doi: 10.1007/s00167-020-06032-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Masterson E, Borton D, O’Brien T. Victims of our climate. Injury. 1993;24(4):247–248. doi: 10.1016/0020-1383(93)90179-a. [DOI] [PubMed] [Google Scholar]
- 9.Morgan C, Ahluwalia AK, Aframian A, Li L, Sun SNM. The impact of the novel coronavirus on trauma and orthopaedics in the UK. Br J Hosp Med (Lond) 2020;81(4):1–6. doi: 10.12968/hmed.2020.0137. [DOI] [PubMed] [Google Scholar]
- 10.Randelli PS, Compagnoni R. Management of orthopaedic and traumatology patients during the Coronavirus disease (COVID-19) pandemic in northern Italy. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1683–1689. doi: 10.1007/s00167-020-06023-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rodrigues-Pinto R, Sousa R, Oliveira A. Preparing to perform trauma and orthopaedic surgery on patients with COVID-19. J Bone Joint Surg Am. 2020;102(11):946–950. doi: 10.2106/JBJS.20.00454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Segal D, Slevin O, Aliev E, et al. Trends in the seasonal variation of paediatric fractures. J Child Orthop. 2018;12(6):614–621. doi: 10.1302/1863-2548.12.180114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stambough JB, Curtin BM, Gililland JM, et al. The past, present, and future of orthopedic education: lessons learned from the COVID-19 pandemic. J Arthroplasty. 2020;35(7S):S60–S64. doi: 10.1016/j.arth.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stinner DJ, Lebrun C, Hsu JR, Jahangir AA, Mir HR. The orthopaedic trauma service and covid-19: practice considerations to optimize outcomes and limit exposure. J Orthop Trauma. 2020;34(7):333–340. doi: 10.1097/BOT.0000000000001782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tang PF, Hou ZY, Wu XB, et al. Expert consensus on management principles of orthopedic emergency in the epidemic of coronavirus disease 2019. Chin Med J (Engl). 2020;133(9):1096–1098. doi: 10.1097/CM9.0000000000000810. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)