Background and aims
COVID-19 severity and mortality are elevated in individuals with diabetes. During the pandemic, interventions recommended globally for people with diabetes were to keep blood glucose on target whilst staying at home to curb the spread of the virus. In Brazil, similar measures were proposed. The aim of our observational study was to assess whether these measures achieved their objectives. Methods: An anonymous and untraceable survey was shared from April 22nd to May 4th. States with more than 30 respondents were included in the analysis and Fisher’s exact test was performed to identify associations, with p < 0.05 considered significant. Results: Type 1 diabetes and female participants were prevalent, 60.76% and 76.12% respectively. 10 out of 26 states were included, in addition to the Federal District (1562 responses). Only in three states (Bahia, Goiás and Pernambuco) less than 50% of the respondents experienced higher glycemia or higher variability during the pandemic. Goiás state, where almost half of the respondents (49.12%) have private insurance, presented the highest percentage of individuals receiving medicines for three months (35.48%) and one of the lowest percentages of blood glucose deterioration (47.17%). In the large states of Minas Gerais, Rio de Janeiro and São Paulo, consultations and/or lab exams were postponed by 37.14%, 34.33% and 40.88%, respectively. Conclusions: The decentralized measures implemented by states in Brazil left most people with diabetes unprotected. Many were forced to venture outside to collect or to purchase their medical supplies monthly and reported increased glycemic levels and/or variability.
Keywords: Diabetes, Coronavirus, SARS-CoV-2, COVID-19, Pandemic, Brazil
Highlights
-
•
22.51% of the individuals with diabetes benefited from the distribution of medicines and supplies enough for 3 months.
-
•
50.08% experienced increase or higher glycemic variability during the COVID-19 pandemic.
-
•
Measures to protect individuals with diabetes during the COVID-19 pandemic were not effective for most of this population.
1. Introduction
COVID-19 pandemic swiftly spread to all continents early 2020 [1]. The disease caused by a new coronavirus, SARS-CoV-2, placed humanity on alert and forced most of the world into quarantine coupled with lockdowns. In spite of the fact that any individual may be infected, it has been reported that 14% of cases are severe and 5% critical [2]. Moreover, some groups are threatened more than others including elders, male gender, and individuals with noncommunicable diseases (NCDs), such as cardiovascular diseases followed by diabetes at the top of the list [2,3].
After COVID-19 was declared a pandemic on March 11, 2020, on several occasions, the World Health Organization voiced concerns about the care of individuals with chronic conditions during this period [[3], [4], [5]]. In addition to the potential consequences of higher risk of poor prognosis in people with NCDs, factors that would enhance these negative outcomes were raised, such as shortage in medicines and supplies for NCDs, reallocation of health workers including emergency rooms and ICUs professionals and prioritization of financial resources to exclusively treat COVID-19 cases [3,[5], [6], [7]]. Countries all around the world established unprecedented national or state measures to deal with the pandemic challenges [[8], [9], [10]]. However, despite 66% of countries reporting continuity of NCD services in national COVID-19 plans, in 62%, services to treat diabetes and its complications were disrupted [5]. Some authors shared their concerns about Brazil, a country with one of the largest diabetes populations, facing political instability [11,12]. Replacement of the federal health minister forced states and municipalities to develop their strategies without support from the presidency [9,10,12,13]. Acknowledging that recommendations for individuals with diabetes were to stay-at-home and to maintain blood glucose on target [[14], [15], [16], [17]], the present study aimed to assess the effectiveness of measures implemented in different Brazilian states.
2. Methods
Data was collected through an anonymous and untraceable survey with 20 multiple-choice questions in Portuguese. The survey was shared from April 22nd to May 4th by the authors, their institutions and reshared by multiple diabetes groups and advocates in Brazil, especially on platforms such as Facebook and WhatsApp. Hence, the method for this study was convenience sampling which has some limitations. The online survey was only answered by individuals with diabetes of legal adulthood age (eighteen or older) with the form being transmitted once the respondent consented with the terms for participation. An initial general analysis of the responses was made covering all the 1701 answers [18], but did not include analysis by state. Thereafter, we decided that additional analyses by state would help to understand if measures to protect individuals with diabetes were more effective in certain states than in others. For this evaluation, only states with more than 30 respondents were included, which limited it to 10 states and the federal district; i.e. 1562 responses (91.83% of the total received forms) (Table 1 ), most of them from the South and Southeast regions (Table 2 ).
Table 1.
Demographic and clinical characteristics of respondents (n = 1562).
| Gender | n | % |
|---|---|---|
| Female | 1189 | 76.12% |
| Male | 371 | 23.75% |
| Non-binary | 2 | 0.13% |
| Age (years old) | n | % |
| 18–30 | 367 | 23.05% |
| 30–40 | 409 | 26.18% |
| 40–50 | 319 | 20.42% |
| 50–60 | 248 | 15.88% |
| 60–70 | 154 | 9.86% |
| 70–80 | 57 | 3.65% |
| >80 | 8 | 0.51% |
| Diabetes type | n | % |
| Type 1 | 949 | 60.76% |
| Type 2 | 479 | 30.67% |
| LADA | 60 | 3.84% |
| MODY | 14 | 0.90% |
| Gestational | 4 | 0.26% |
| Unknown | 56 | 3.59% |
| Presence of other chronic disease | n | % |
| Yes | 967 | 61.91% |
| No | 595 | 38.09% |
| Schooling | n | % |
| Elementary incomplete | 51 | 3.27% |
| Elementary complete | 42 | 2.69% |
| Middle incomplete | 51 | 3.27% |
| Middle complete | 323 | 20.68% |
| College incomplete | 283 | 18.12% |
| College complete | 408 | 26.12% |
| Postgraduate | 404 | 24.86% |
Table 2.
Characteristics of access to medical supplies, care and glycemia among respondents by states.
| States | Number of Answers | % of the answers | %Private insurance only | %Increased blood glucose levels or variabilitya | %Receiving medicines for 3 monthsb | %Going outside monthly to receive/buy medicinesc | %Postponing Consultations and/or lab exams |
|---|---|---|---|---|---|---|---|
| Bahia | 58 | 3.71% | 46.55% | 36.73% | 28.00% | 51.85% | 32.76% |
| Ceará | 43 | 2.75% | 39.53% | 51.28% | 8.33% | 43.90% | 53.49% |
| Federal District | 32 | 2.05% | 25.00% | 56.67% | 29.41% | 50.00% | 53.13% |
| Goiás | 57 | 3.65% | 49.12% | 47.17% | 35.48% | 41.82% | 36.84% |
| Minas Gerais | 140 | 8.96% | 30.71% | 55.56% | 20.00% | 47.76% | 37.14% |
| Paraná | 101 | 6.47% | 44.55% | 57.29% | 27.54% | 32.29% | 33.66% |
| Pernambuco | 43 | 2.75% | 30.23% | 39.39% | 23.53% | 52.50% | 37.21% |
| Rio de Janeiro | 233 | 14.92% | 49.79% | 50.24% | 29.70% | 37.44% | 34.33% |
| Rio Grande do Sul | 94 | 6.02% | 27.66% | 52.33% | 29.03% | 44.94% | 30.85% |
| Santa Catarina | 37 | 2.37% | 16.22% | 60.00% | 17.24% | 43.24% | 27.03% |
| São Paulo | 724 | 46.35% | 39.64% | 50.08% | 19.39% | 43.65% | 40.88% |
| Total/Mean | 1562 | 100% | 39.44% | 50.84% | 22.51% | 43.08% | 38.22% |
Individuals who do not measure blood glucose were excluded from this column (8.58%).
Only individuals who receive medicines and supplies from the public health system, and continued reclaiming during the pandemic, were included in this column (59.15%).
Individuals who stopped reclaiming their medicines and are using their personal stocks were not included in this column (2.5%).
Among the main goals of the survey was to investigate how respondents were accessing their medical supplies, since it is obvious that they needed to continue their treatment and hence needed to safely receive their medicines during the pandemic. We knew that the federal government and some states announced provision of medicines and medical supplies for chronic conditions for a 3-month period [[19], [20], [21]], in some locations coupled with other measures of home delivery [22,23], in order to avoid the risk of monthly return to public pharmacies or health centers. We classified these responses in terms of degree of exposure to COVID-19 using the following categories for getting hold of medical suppliers: a) he/she or a representative went to the public pharmacy or health facility to receive monthly supplies (public monthly receipt); b) he/she or a representative received at a public pharmacy or health facility enough for three months (public receipt for 3 months); c) he/she ordered from a private pharmacy to be delivered at home (private home delivery); d) he/she stopped buying or reclaiming and was making use of own stocks (using own stocks); e) he/she went to a private pharmacy to purchase (at private pharmacies). Association of variables were considered significant when p-value for the Fisher’s exact test was <0.05.
3. Results
The majority of the 1562 respondents indicated that they only used the private health system (39.44%), 32,65% used both systems, and 27.91% only used the public health system (see Table 2 for more details).
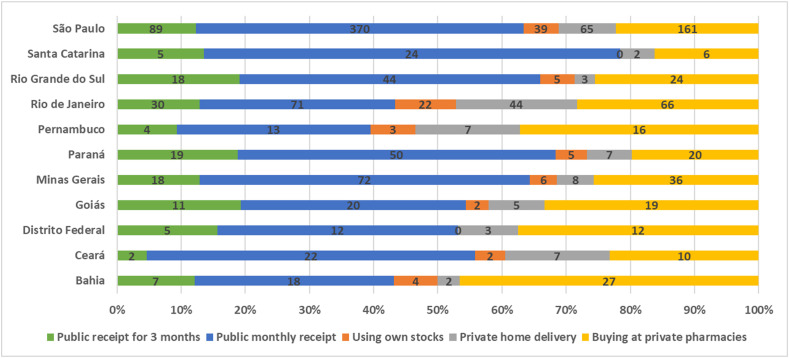
Considering all respondents in the study, a significant association was found between state and the way that individuals were accessing their medical supplies (p-value <0.0001). The low percentage of individuals receiving enough medical supplies for three months in all ten states and the Federal District was extremely shocking (Fig. 1 and Table 2). “Private home delivery”, which is another potential protective measure, was also much behind “going to a pharmacy to buy” (Fig. 1). Santa Catarina was found to be the state with the highest percentage of people receiving their medicine monthly (in addition to being the state with the lowest percentage of private insured and highest percentage of increased blood glucose level and variability); while Bahia had the highest percentage of those buying at private pharmacies (and one of the highest percentage of private insured and lowest increase in blood glucose level and variability) (Table 2). When the ways of seeking medication are separated into two categories, “he/she or a representative received at a public pharmacy or health facility enough for 3 months” and the other categories, there is no statistically significant association with the state (p-value = 0.309). This result would be interpreted as a lack of difference between states in terms of their low success in making the medical supplies available for three months.
Fig. 1.
Percentages according to the way that individuals were accessing their medical supplies by state (the numbers represent the total respondents in the category).
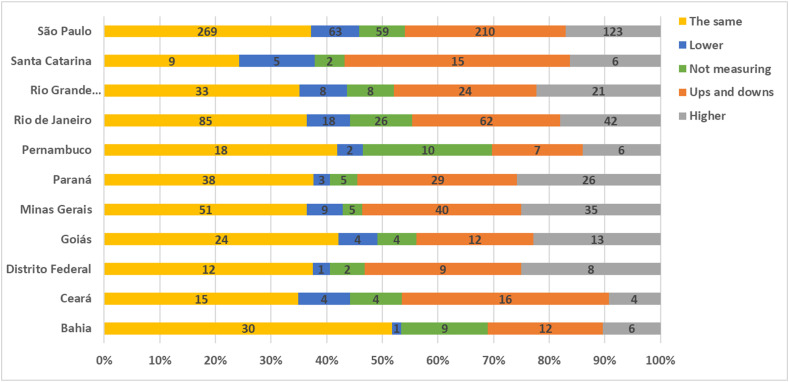
The pandemic impact on the individuals’ perceived glycemic changes was another aspect of high interest. As for the change in blood glucose level by state, we identified a statistically significant association (p-value = 0.0311). Fig. 2 depicts the distribution of glycemic level changes by states. The largest proportions of fluctuations in blood glucose levels (ups and downs) are in Santa Catarina and Ceará, while Bahia stands out as the only state where more than 50% of the respondents were able to maintain their blood glucose levels during the pandemic (Fig. 2).
Fig. 2.
Percentages according to blood glucose categories by state (the numbers represent the total respondents in the category).
4. Discussion
Table 2 provides a detailed view of some of the most relevant results, including the fact that only in Bahia, Goiás and Pernambuco less than 50% of respondents experienced blood glucose levels deterioration (higher glycemia or higher variability during the pandemic). An alarming finding which means that the great majority of individuals with diabetes in the country were experiencing deterioration of their glycemia and thus, with increased risk for severe COVID-19 and mortality if infected [16,24]. It is known that high blood glucose and variability should be avoided during the COVID-19 pandemic since it raises severity and mortality rates. Moreover, the fact that 61.91% reported having additional NCDs further increases the risks of poor outcomes among this population if infected by SARS-CoV-2 (Table 1) [25,26]. The lack of a federal level coordination, leading to decentralized measures implemented by states in Brazil, left most people with diabetes unprotected (going outside to receive or to purchase their medical supplies monthly) and at increased risk with higher glycemic levels or variability. Lack of specific measures to protect people with diabetes during the pandemic and their limited reach were also reported in neighboring countries in Latin America [27], where 68% experienced shortage of medicines or medical supplies and 57% experienced difficulties to access medical services already in the first months of the pandemic.
Regarding specific states, Santa Catarina was an example where, although the percentage of individuals postponing consultations and lab exams was lower than in other states (27.03%), the percentage of individuals experiencing deterioration of glucose control is the highest (60%). A possible explanation for this result is the socio-economic profile of these specific respondents, only 16.22% have private insurance. Therefore, as hypothesized by Barone et al. (2020) [18], this may be explained by an unequal and more devastating impact of the pandemic on the most socially vulverable populations. Goiás is an opposite example, where almost half of the respondents (49.12%) have private insurance, and it counts with the highest percentage of individuals receiving medicines for three months - but still much less than half (35.48%) - and one of the lowest percentage of blood glucose deterioration - though still very high (47.17%). Ceará is a state that detached from the others in terms of the least successful in the protective measures when considering the percentage that received medication for three months, only 8.33%. Not surprisingly, this state is also the highest in percentage of people postponing consultations and/or lab exams (53.49%) and is above the mean in terms of percentage experiencing deterioration of blood glucose control (51.28%).
Data depicted in Table 2, as well as in Fig. 1, Fig. 2, assist in concluding that there is not a state in Brazil where implemented measures to protect individuals with diabetes were mostly successful. The last line with the averages gives a good glimpse on that, with more than 50% experiencing blood glucose control deterioration, more than 38% postponing consultations and lab exams, and two times more people receiving medical supplies monthly than quarterly. While averages may limit analysis, data reveals that no state had less than a third of its respondents experiencing deterioration of their blood glucose control, which coincides with consultations and lab exams being postponed. A similar association of 87.81% reporting lack of access to healthcare services with 78.42% experiencing increase in blood glucose was reported in India [28]. Shortage of medicines, which was not evaluated in the present study, may also have hindered glycemic control, as shown in individuals with type 1 diabetes in India [29]. In this case, due to interruptions in the availability of insulin and glucose strips during lockdown period, HbA1c increased from 8.8% (73 mmol/mol, 206 mg/dL) to 10% (86 mmol/mol, 240 mg/dL). In Brazil, even the South states of Paraná, Santa Catarina and Rio Grande do Sul, considered developed, and Bahia barely reached around one-third postponing consultations and/or lab exams; with other states - including the large Southeast states of Minas Gerais, Rio de Janeiro and São Paulo - presenting worse results (37.14%, 34.33% and 40.88%, respectively).
We understand that our survey may not represent the entire population with diabetes, even of those 11 states, especially of states with fewer answers. At the same time, the fact that the group that answered this survey is a privileged cohort - with internet access, much higher proportion with college degrees than in the Brazilian population [30] - we do not see reasons to believe that non-respondents would have been more protected and presenting no glycemic alterations. It is worrisome to know that measures adopted in the different states, or at least in the 11 assessed, were not effective to protect most higher risk populations. Going outside monthly to risky environments, such as health facilities where people infected by SARS-CoV-2 seek assistance, should be a special concern. Moreover, measures to facilitate maintaining their blood glucose on target in the new routine were either missing or not working for most. In addition to the already high case fatality rate and total deaths in Brazil, we are concerned that the country may experience short, mid, and long-term consequences, including increase in prevalence and severity of diabetes and other NCDs chronic complications due to their poor management during the pandemic.
Different strategies have been implemented across the globe to effectively fight the pandemic. Australia and Portugal reported some of the most successful countrywide coordinated measures, implemented in partnership between the public and the private sectors [[31], [32], [33]]. Partnerships with communication and media channels were also shown to facilitate sharing of appropriate messages and guidance to the population in general, but also to those with diabetes and their caretakers [34]. In Brazil, the distribution of adequate medical supplies for three months and, whenever possible especially for elderly, delivered to their home, must be strengthened [18]. In addition, we emphasize that these individuals should not have their exams and appointments postponed or cancelled. As a matter of fact, they should receive medical assistance to adjust their therapy during the pandemic and be oriented to adapt healthy habits and behaviors [15]. Telemedicine, in its different forms, from teleconsultation to telediagnosis, should be considered [7,14,15,[31], [32], [33],[35], [36], [37]], as well as mobile options for collecting samples at the individuals’ homes or using point-of-care equipment and, this way, avoid putting them at risk leaving their homes for in-person consultations or exams [18,38,39].
The limitations of the presented results must be taken into consideration, because of the convenience nature of the sample without post-stratification weights, where only individuals with access to the internet could answer the survey. All collected data was based on their answers. Therefore, it is subjective in terms of being based on knowledge and perception of respondents, rather than on medical records or biochemical and physical exams. Furthermore, as the survey was disseminated by multiple diabetes groups and through their members, respondents constituted engaged and active individuals of these groups, clearly a higher proportion of people with type 1 diabetes, female gender, highly educated and younger than what could be expected for a general population with diabetes [40,41]. Therefore, even though the survey was freely shared using social media channels, primarily WhatsApp and Facebook, we hypothesize that the unexpected much higher number responses from young adults with type 1 than people with type 2 reflects the traditional engagement of these individuals in diabetes associations and online groups, as well as their commitment in sharing materials, in this case the survey, with peers. Consequently, the sample was biased towards the type 1 population profile (mean age of 30.3 years and 56.8% female, as reported by Gomes et al. [41]), but still with an even greater proportion of female respondents in the present study. Another important limitation is the uneven response from the different states, which adds some uncertainty to the results from states with less representation. Thus, although the challenges identified here, our results coincides with anecdotal reports and other analysis and studies of the country and its region [11,18,27,[42]].
5. Conclusion
Measures implemented to protect individuals with diabetes in Brazil during the COVID-19 pandemic were not effective for most of the population in any of the assessed states. We hypothesize that a uniform plan orchestrated by the federal ministry would have been more effective. This would ideally include collaboration between municipal, state and federal government in partnerships with civil society, academia and the private sector to ensure that individuals with diabetes and other NCDs received appropriate care to keep their health conditions under control, while allowing them to be safe and informed in their homes. We believe that the novel data presented here will assist Brazilian states to make appropriate adjustments and sound decisions to improve diabetes and other NCDs care and infection prevention during the COVID-19 pandemic, and inspire other countries to respond in an integrated and effective fashion to protect their population. We understand that protecting individuals with diabetes and other high-risk populations will start to dwindle the burden on populations, health systems and economies.
Ethics approval and consent to participate
The respondents were informed and needed to agree to have their answers submitted through the anonymous and untraceable online survey.
Consent for publication
All authors are fully aware and consent in publishing the present manuscript.
Availability of data and materials
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributions
All authors contributed equally in designing the study, Viviana Giampaoli led the analysis with Simone Berga Harnik, Matheus Chaluppe and Mark Thomaz Ugliara Barone and assistance from all other authors, and the results were discussed and the manuscript was written and reviewed collaboratively by all authors.
Declaration of competing interest
All authors declare no competing or conflicts of interest.
Acknowledgements
The authors acknowledge the non-governmental organizations ADJ Diabetes Brasil (ADJ), Institute for Children with Diabetes (ICD), Brazilian Diabetes Society (SBD), Brazilian Hypercholesterolemia Association (AHF), FórumDCNTs and their members and partner entities for assisting in sharing the survey and providing general support, and all respondents.
References
- 1.Wu D., Wu T., Liu Q., Yang Z. The SARS-CoV-2 outbreak: what we know. Int J Infect Dis. 2020;94:44-8. doi: 10.1016/j.ijid.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu Z., McGoogan J. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. JAMA Network. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Kluge H., Wickramasinghe K., Rippin H., Mendes R., Peters D.H., Kontsevaya A. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet. 2020:1–3. doi: 10.1016/S0140-6736(20)31067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . WHO; Geneva: 2020. NCDs & COVID-19.https://www.who.int/teams/ncds/covid-19 [cited 22 September 2020]. Available from: [Google Scholar]
- 5.World Health Organization (WHO) WHO; Geneva: 2020. Rapid assessment of service delivery for NCDs during the COVID-19 pandemic.https://www.who.int/publications/m/item/rapid-assessment-of-service-delivery-for-ncds-during-the-covid-19-pandemic [cited 22 September 2020]. Available from: [Google Scholar]
- 6.Ma R.C.W., Holt R.I.G. COVID-19 and diabetes. Diabet Med. 2020;37:723–725. doi: 10.1111/dme.14300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katulanda P, Dissanayake H, Ranathunga I. Prevention and management of COVID-19 among patients with diabetes: an appraisal of the literature. Diabetologia. 10.1007/s00125-020-05164-x. [DOI] [PMC free article] [PubMed]
- 8.Deloitte COVID-19 European measures. https://www2.deloitte.com/content/dam/Deloitte/ro/Documents/COVID-19%20CE%20Measures-version%2010.pdf Available from:
- 9.Kirby T. South America prepares for the impact of COVID-19. Lancet. 2020:1–2. doi: 10.1016/s2213-2600(20)30218-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Croda J., Oliveira W., Frutuoso R., Mandetta L.H., Baia-da-Silva D.C., Brito-Sousa J.D. COVID-19 in Brazil: advantages of a socialized unified health system and preparation to contain cases. Sociedade Brasileira de Medicina Tropical. 2020;53 doi: 10.1590/0037-8682-0167-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pititto BA, Ferreira SRG. Diabetes and covid-19: more than the sum of two morbidities. Revista de Saúde Pública. https://doi.org/10.11606/s1518-8787.2020054002577. [DOI] [PMC free article] [PubMed]
- 12.The Lancet COVID-19 in Brazil: ”so what? Lancet. 2020;395:1461. doi: 10.1016/S0140-6736(20)31095-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rafael R., Neto M., Carvalho M., David H.M.S.L., Acioli S., Faria M.G.A. Epidemiology, public policies and Covid-19 pandemics in Brazil: what can we expect? Rev Enferm UFPI. 2020;28 doi: 10.12957/reuerj.2020.49570. [DOI] [Google Scholar]
- 14.Puig-Domingo M., Marazuela M., Giustina A. COVID-19 and endocrine diseases. A statement from the European Society of Endocrinology. Endocrine. 2020;68:2–5. doi: 10.1007/s12020-020-02294-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bornstein S.R., Rubino F., Khunti K., Mingrone G., Hopkins D., Birkenfeld A.L. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 2020;8(6):546–550. doi: 10.1016/S2213-8587(20)30152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu L., She Z.G., Cheng X., Qin J.J., Zhang X.J., Cai J. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metabol. 2020;1(20):S1550–S4131. doi: 10.1016/j.cmet.2020.04.021. 30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Inglesby T.V. Public health measures and the reproduction number of SARS-CoV-2. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.7878. [DOI] [PubMed] [Google Scholar]
- 18.Barone M.T.U., Harnik S.B., de Luca P.V., Lima B.L.S., Wieselberg R.J.P., Ngongo B. The impact of COVID-19 on people with diabetes in Brazil. Diabetes Res Clin Pract. 2020;166:108304. doi: 10.1016/j.diabres.2020.108304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ministério da Saúde (BR) Brasília (DF); 2020. Alterações no Programa Farmácia Popular devido à situação de emergência de saúde pública decorrente do coronavírus (COVID19)https://www.saude.gov.br/noticias/farmacia-popular/46566 [cited 22 September 2020]. Available from: [Google Scholar]
- 20.Governo do Estado de São Paulo (BR) São Paulo (SP); 2020. Saúde amplia entrega de remédios nas farmácias de alto custo para prevenção do coronavírus.http://www.portaldenoticias.saude.sp.gov.br/saude-amplia-entrega-de-remedios-nas-farmacias-de-alto-custo-para-prevencao-do-coronavirus/ [cited 22 September 2020]. Available from: [Google Scholar]
- 21.Portal do Governo do Estado de São Paulo (BR) São Paulo (SP); 2020. SP amplia suprimento em farmácia de alto custo para proteger vulneráveis a coronavírus.https://www.saopaulo.sp.gov.br/spnoticias/governo-de-sao-paulo-anuncia-novas-medidas-de-combate-ao-novo-coronavirus/ [cited 22 September 2020]. Available from: [Google Scholar]
- 22.Agência de notícias do Paraná (BR) Paraná (PR); 2020. Saúde ampliará entrega de medicamentos em casa. [cited 22 September 2020]. Available from: http://www.aen.pr.gov.br/modules/noticias/article.php?storyid=106235&tit=Saude-ampliara-entrega-de-medicamentos-em-casa. [Google Scholar]
- 23.Secretaria de Estado de Saúde de Minas Gerais (BR) 2020. Governo de Minas anuncia projeto de entrega domiciliar de medicamentos durante pandemia pela Covid-19. Minas Gerais (MG)https://www.saude.mg.gov.br/component/gmg/story/12477-governo-de-minas-anuncia-projeto-de-entrega-domiciliar-de-medicamentos-durante-pandemia-pela-covid-19 [cited 22 September 2020]. Avaliable from: [Google Scholar]
- 24.Codo A.C., Davanzo G.G., Monteiro L.B., de Souza G.F., Muraro S.P., Virgilio-da-Silva J.V. Elevated glucose levels favor SARS-CoV-2 infection and monocyte response through a HIF-1α/Glycolysis-Dependent Axis. Cell Metabol. 2020;32(3):437–446. doi: 10.1016/j.cmet.2020.07.007. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cai Q., Chen F., Wang T., Luo F., Liu X., Wu Q. Obesity and COVID-19 severity in a designated hospital in shenzhen, China. Diabetes Care. 2020;14 doi: 10.2337/dc20-0576. [DOI] [PubMed] [Google Scholar]
- 26.Shi Q., Zhang X., Jiang F., Zhang X., Hu N., Bimu C. Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in wuhan, China: a two-center, retrospective study. Diabetes Care. 2020;43(5):1–10. doi: 10.2337/dc20-0598. [DOI] [PubMed] [Google Scholar]
- 27.Barone M.T.U., Villarroel D., de Luca P.V., Harnik S.B., Lima B.L.S., Wieselberg R.J.P. COVID-19 impact on people with diabetes in South and Central America (SACA region) Diabetes Res Clin Pract. 2020;166:108301. doi: 10.1016/j.diabres.2020.108301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khader M.A., Jabeen T., Namoju R. A cross sectional study reveals severe disruption in glycemic control in people with diabetes during and after lockdown in India. Diabetes Metabolic Syndrome. 2020;14(6):1579–1584. doi: 10.1016/j.dsx.2020.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Verma A., Rajput R., Verma S., Balania V.K.B., Jangra B. Impact of lockdown in COVID 19 on glycemic control in patients with type 1 Diabetes Mellitus. Diabetes Metabolic Syndrome. 2020;14(5):1213–1216. doi: 10.1016/j.dsx.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Organisation for Economic Co-operation and Development (OECD) OECD; Paris: 2019. Education at a glance 2019. Country note Brazil.https://www.oecd.org/education/education-at-a-glance/EAG2019_CN_BRA.pdf [cited 22 September 2020]. Available from: [Google Scholar]
- 31.Sacks L.J., Pham C.T., Fleming N., Neoh S.L., Ekinci E.I. Considerations for people with diabetes during the Coronavirus Disease (COVID-19) pandemic. Diabetes Res Clin Pract. 2020;166 doi: 10.1016/j.diabres.2020.108296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andrikopoulos S., Johnson G. The Australian response to the COVID-19 pandemic and diabetes - lessons learned. Diabetes Res Clin Pract. 2020;165 doi: 10.1016/j.diabres.2020.108246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization, Regional Office for Europe . 2020. Ensuring people-centred diabetes care during the COVID-19 pandemic Experiences from Portugal.www.euro.who.int/__data/assets/pdf_file/0011/444791/Diabetes-care-during-COVID-19-eng.pdf?ua=1 [cited 22 September 2020] [Google Scholar]
- 34.Hopman J., Allegranzi B., Mehtar S. Managing COVID-19 in low- and middle-income countries. J Am Med Assoc. 2020;323(16):1549–1550. doi: 10.1001/jama.2020.4169. [DOI] [PubMed] [Google Scholar]
- 35.Sarti T., Lazarini W., Fontenelle L., Almeida A.P.S.C. What is the role of Primary Health Care in the COVID-19 pandemic? Epidemiol. Serv. Saúde. 2020;29(2) doi: 10.5123/s1679-49742020000200024. [DOI] [PubMed] [Google Scholar]
- 36.Gentile S., Strollo F., Ceriello A. COVID-19 Infection in Italian people with diabetes: lessons learned for our future (an experience to be used) Diabetes Res Clin Pract. 2020;162 doi: 10.1016/j.diabres.2020.108137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ghosh A., Gupta R., Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: guidelines for physicians. Diabetes Metabolic Syndrome. 2020;14(4):273–276. doi: 10.1016/j.dsx.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ranscombe P. How diabetes management is adapting amid the COVID-19 pandemic. Lancet Diabetes Endocrinol. 2020;8(7):571. doi: 10.1016/S2213-8587(20)30181-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kanc K., Komel J., Kos M., Wagner J.H. H(ome)bA1c testing and telemedicine: high satisfaction of people with diabetes for diabetes management during COVID-19 lockdown. Diabetes Res Clin Pract. 2020 doi: 10.1016/j.diabres.2020.108285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Malta D.C., Duncan B.B., Schmidt M.I., Machado Í.E., Silva A.G.D., Bernal R.T.I. Prevalence of diabetes mellitus as determined by glycated hemoglobin in the Brazilian adult population. National Health Survey. Rev. bras. epidemiol. 2019;22(S2) doi: 10.1590/1980-549720190006.supl.2. [DOI] [PubMed] [Google Scholar]
- 41.Gomes M.B., Coral M., Cobas R.A., Dib S.A., Canani L.H., Nery M. Prevalence of adults with type 1 diabetes who meet the goals of care in daily clinical practice: a nationwide multicenter study in Brazil. Diabetes Res Clin Pract. 2012;97(1):63–70. doi: 10.1016/j.diabres.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 42.Malta D.C., Szwarcwald C.L., Barros M., Gomes C.S., Machado Í.E., Souza Júnior P. Pandemic and changes in adult Brazilian lifestyles: a cross-sectional study, 2020. Epidemiol Serv Saude. 2020;29(4):e2020407–42. doi: 10.1590/S1679-49742020000400026. [DOI] [PubMed] [Google Scholar]