Abstract
Telehealth innovations in substance use treatment necessitated by the COVID-19 pandemic present a generational opportunity to increase family involvement in medication for opioid use disorders (MOUD) among youth. This commentary describes a conceptual framework for engaging and retaining youth and families across four stages of MOUD services: Preparation, Initiation, Stabilization, Remission & Recovery. Case vignettes illustrate provider-delivered and direct-to-family tele-interventions for augmenting family involvement in each MOUD stage: Family Outreach, Family Engagement, Family Training, Family Recovery Maintenance.
Keywords: COVID-19, Youth opioid use disorder, Medication assisted treatment, Family involvement, Telehealth
1. Introduction
The COVID-19 pandemic has upended the healthcare system in our country. It has inflicted staggering rates of hospitalization and death and dramatically altered how Americans seek health services (US Dept Health and Human Services, 2020). Moreover, COVID-19 erupted during another national health crisis: opioid misuse and overdose, which resulted in almost 450,000 deaths between 1999 and 2018 (https://www.cdc.gov/drugoverdose/epidemic/index.html). Older adolescents (age 16–18) and young adults (age 18–26) are especially vulnerable to the opioid epidemic: Between 1999 and 2016 the rate of lethal overdoses attributable to opioids in adolescents increased 268% (Gaither et al., 2018), and 1.1% of young adults experienced an opioid use disorder (OUD) (Volkow et al., 2019).
We believe the COVID-19 pandemic has also created a generational opportunity to transform routine care for youth OUD by spurring treatment providers to increase family involvement in services. Extensive research (see Ariss & Fairbairn, 2020; Hogue et al., 2018) suggests that family involvement is a key element of the most effective behavioral interventions for youth substance use. Due to the pandemic, substance use services of every kind are being reconfigured at unprecedented speed and scale to operate remotely via telehealth (Centers for Medicare & Medicaid Services, 2020). This commentary describes how tele-interventions enable pragmatic and sustainable changes in youth OUD services that clear a path for systematic integration of families into the national OUD treatment system.
2. Family-based tele-interventions for youth MOUD: framework and case vignettes
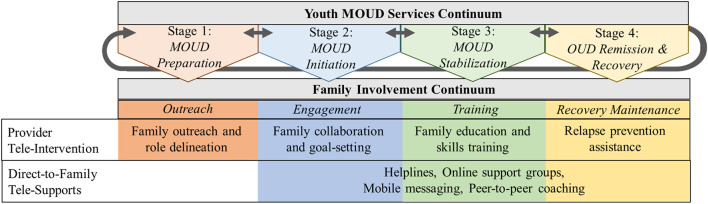
Medication for opioid use disorders (MOUD), in the form of opioid agonist or antagonist medication, is the only evidence-based treatment for youth OUD (Committee on Substance Use and Prevention, 2016). Unfortunately, it has proven enormously difficult to engage youth in OUD treatment (Hadland et al., 2017), and they drop out of care at alarmingly high rates (e.g., Schuman-Olivier et al., 2014). To address this challenge we propose a conceptual framework to organize efforts to engage and retain youth and families across the continuum of MOUD services. Fig. 1 depicts four overlapping stages and notes how tele-interventions present novel options for family involvement in each stage. Stage 1: MOUD Preparation includes identification, referral, and enrollment of youth patients in SUD treatment, including re-enrollment following recovery lapses. Stage 2: MOUD Initiation includes initial evaluation and medication induction. Stage 3: MOUD Stabilization includes dose titration and withdrawal management. Stage 4: OUD Remission & Recovery includes stability monitoring and relapse prevention. Importantly, behavioral interventions for substance use and co-occurring disorders are often integrated throughout Stages 2–4. Below we use case vignettes to illustrate how augmenting family involvement in MOUD services via tele-interventions can be a potent means to advance treatment success in each stage.
Fig. 1.
Conceptual framework for integrating family-based tele-intervention across the youth MOUD services continuum.
Note: Case progression along the services continuum is not necessarily linear, as many youth cycle in and out of stages and experience multiple treatment episodes.
2.1. MOUD preparation: family outreach
Assertive outreach to families at the start of MOUD service contact (Fishman et al., 2020), including messaging about the essential value of medication, can greatly facilitate treatment enrollment and preparation. MB was a 23-year-old entered residential treatment for intravenous fentanyl use. The counselor spoke by phone with MB's mother and arranged to include her remotely in a videoconference with MB and the residential staff to plan treatment with extended-release buprenorphine. Counselor and staff introduced MB and his mother to OUD medication protocols, delineated family member roles during treatment, and set ground rules for ongoing family-patient-staff interactions.
2.2. MOUD initiation: family engagement
Youth MOUD initiation can be solidified by employing family engagement techniques, such as family alliance-building and goal-setting, known to increase treatment motivation and participation among youth (Becker et al., 2018). AE was a 24-year-old attending a video session for initiation of buprenorphine treatment after moving back home following shelter-in-place edicts. He said his mother was skeptical of MOUD as “replacing one addiction with another.” The physician asked him to bring his mother into the live session so the physician could explain the treatment plan and establish a foundation for her involvement—a spontaneous engagement opportunity not available via in-person care. During two additional tele-sessions the physician explored the mother's concerns about MOUD, explained why medications are the most effective treatment option, and elicited her commitment to assisting with AE's treatment and recovery.
2.3. MOUD stabilization: family training
Family-based MOUD education and skills training can help knit family members into the complex weave of MOUD services and teach caregivers to support youth recovery efforts (Hornberger & Smith, 2011; Ventura & Bagley, 2017). This includes discussions about negotiating burgeoning independence, positive family communication, and anger management. GR was a 17-year-old in treatment for prescription opioid addiction. During the first six weeks of care her parents attended weekly virtual appointments—an extraordinary level of involvement under a usual-care model—to help them track treatment progress, communicate expectations, and set reasonable boundaries for her behavior. One day when GR left the family home intending not to return, the parents drove to meet her while remaining in audiovisual contact with the clinician via smartphone. The clinician prepped the parents to express love and concern, and to use the positive communication skills they had been practicing, upon seeing her. Once reunited, the clinician facilitated a brief reconciliation and safety planning session before they returned home.
2.4. OUD remission & recovery: family recovery maintenance
Family-focused recovery maintenance strategies can promote youth retention in ongoing services during OUD remission, formulate and monitor long-term recovery management plans, and encourage family members to enlist direct-to-family supports (Archer et al., 2020; Ventura & Bagley, 2017). BG was a 21-year-old in treatment with extended-release naltrexone. During her period of remission, her counselor routinely texted BG's mother (individually and via three-way group messaging) to encourage medication dose and other appointments, and praise BG's progress. When she later relapsed and dropped out of care, based on prior agreement the counselor reached out repeatedly to both BG and her mother via text and managed to arrange BG's re-enrollment. The counselor then advised BG's mother to sign up for a text messaging service that provided daily person-tailored texts about effective parenting, self-care, and coping with a child experiencing OUD. The service featured options for COVID-specific texts, immediate keyword help messaging such as “overdose”, and links to live peer-to-peer coaching (see Carpenter et al., 2020).
3. Conclusion
The rapid shift towards telehealth during the COVID-19 pandemic has expanded the possibilities for outreach to families of youth with OUD, both planned and spontaneous, and may contribute to a dramatic reduction in barriers for initiating and sustaining family involvement in treatment. Patient and family convenience is a substantial advantage of tele-interventions for MOUD, enabling caregivers to participate in services from the comfort of home with minimal disruption to other facets of life. Telehealth sessions are particularly valuable for families who bear substantial costs to attend in-person appointments, such as those who rely on public transportation, live in rural communities, and have physical disabilities (Center for Substance Abuse Treatment, 2015). Ongoing monitoring will be needed to assess whether tele-interventions emerging during the pandemic achieve their potential to boost youth and family engagement throughout the MOUD services continuum. We hope that such innovations become a permanent component of the services landscape, and that benefits will extend beyond MOUD to the abundance of evidence-based SUD interventions available for adolescents and young adults.
Declaration of competing interest
None.
Acknowledgements
Aaron Hogue, Family and Adolescent Clinical Technology & Science, Partnership to End Addiction; Sara J. Becker, Center for Alcohol and Addictions Studies, Brown University School of Public Health; Marc Fishman, Maryland Treatment Centers; Craig E. Henderson, Department of Psychology, Sam Houston State University; Sharon Levy, Adolescent Substance Use and Addiction Program, Boston Children's Hospital, Harvard Medical School.
All authors contributed equally to this article. The authors gratefully acknowledge the contributions of Nicole Porter and Molly Bobek to the ideas presented.
The conceptual work supporting this manuscript was supported by R24DA051946 funded by the National Institute on Drug Abuse (Principal Investigator: A. Hogue).
References
- Archer M., Harwood H., Stevelink S., Rafferty L., Greenberg N. Community reinforcement and family training and rates of treatment entry: A systematic review. Addiction. 2020;115(6):1024–1037. doi: 10.1111/add.14901. [DOI] [PubMed] [Google Scholar]
- Ariss T., Fairbairn C.E. The effect of significant other involvement in treatment for substance use disorders: A meta-analysis. Journal of Consulting and Clinical Psychology. 2020;88:526–540. doi: 10.1037/ccp0000495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker K.D., Boustani M., Gellatly R., Chorpita B.F. Forty years of engagement research in children’s mental health services: Multidimensional measurement and practice elements. Journal of Clinical Child & Adolescent Psychology. 2018;47(1):1–23. doi: 10.1080/15374416.2017.1326121. [DOI] [PubMed] [Google Scholar]
- Carpenter K.M., Foote J., Hedrick T., Collins K., Clarkin S. Building on shared experiences: The evaluation of a phone-based parent-to-parent support program for helping parents with their child’s substance misuse. Addictive Behaviors. 2020;100:106103. doi: 10.1016/j.addbeh.2019.106103. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment . Substance Abuse Services and Mental Health Administration; Rockville, MD: 2015. Using technology-based therapeutic tools in behavioral health services. [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services Medicare telemedicine health care provider fact sheet. 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet Website.
- Committee on Substance Use and Prevention Medication-assisted treatment of adolescents with opioid use disorders. Pediatrics. 2016;138(3) doi: 10.1542/peds.2016-1893. [DOI] [PubMed] [Google Scholar]
- Fishman M., Wenzel K., Vo H., Wildberger J., Burgower R. Youth Opioid Recovery Support: A pilot RCT of assertive treatment including family involvement and home delivery of medication for young adults with OUD. Addiction. 2020 doi: 10.1111/add.15181. (Under revision) [DOI] [PubMed] [Google Scholar]
- Gaither J.R., Shabanova V., Leventhal J.M. US national trends in pediatric deaths from prescription and illicit opioids, 1999-2016. JAMA Network Open. 2018;1(8):e186558. doi: 10.1001/jamanetworkopen.2018.6558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadland S.E., Wharam J.F., Schuster M.A., Zhang F., Samet J.H., Larochelle M.R. Trends in receipt of buprenorphine and naltrexone for opioid use disorder among adolescents and young adults, 2001-2014. JAMA Pediatrics. 2017;171(8):747–755. doi: 10.1001/jamapediatrics.2017.0745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A., Henderson C.E., Becker S.J., Knight D.K. Evidence base on outpatient behavioral treatments for adolescent substance use, 2014–2017: Outcomes, treatment delivery, and promising horizons. Journal of Clinical Child & Adolescent Psychology. 2018;47(4):499–526. doi: 10.1080/15374416.2018.1466307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornberger S., Smith S.L. Family involvement in adolescent substance abuse treatment and recovery: What do we know? What lies ahead? Children and Youth Services Review. 2011;33:S70–S76. [Google Scholar]
- Schuman-Olivier Z., Greene M.C., Bergman B.G., Kelly J.F. Is residential treatment effective for opioid use disorders? A longitudinal comparison of treatment outcomes among opioid dependent, opioid misusing, and non-opioid using emerging adults with substance use disorder. Drug and Alcohol Dependence. 2014;144:178–185. doi: 10.1016/j.drugalcdep.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services Telehealth: Delivering care safely during COVID-19. 2020. https://www.hhs.gov/coronavirus/telehealth/index.html Website.
- Ventura A.S., Bagley S.M. To improve substance use disorder prevention, treatment and recovery: Engage the family. Journal of Addiction Medicine. 2017;11(5):339–341. doi: 10.1097/ADM.0000000000000331. [DOI] [PubMed] [Google Scholar]
- Volkow N.D., Jones E.B., Einstein E.B., Wargo E.M. Prevention and treatment of opioid misuse and addiction: A review. JAMA Psychiatry. 2019;76(2):208–216. doi: 10.1001/jamapsychiatry.2018.3126. [DOI] [PubMed] [Google Scholar]