Abstract
Objectives
Heart transplantation has become an established procedure in India with increasing numbers being done annually. The majority of these patients are very sick with a history of multiple hospital admissions. The economic burden of such therapy is substantial and the costs are borne by the patients with very little insurance coverage. The objective of this study was to estimate the following:
The average cost of a heart transplant procedure in a “real-world setting” in a private healthcare facility in India, with varying patient risk profiles.
Identify the factors contributing to the wide variations in cost seen in practice.
Finally, based on data thus collected, can some kind of estimation be made about the expected cost in a given patient before the operation is done?
Methods
The cost incurred by the hospital in doing 168 heart transplants during a 3-year period was analyzed. Costs were divided into direct and indirect costs. The direct costs consisted of medical consumables, laboratory investigations, radiology, costs involved in organ harvest and transport, and diet. Direct cost was 40 % of the total cost of the procedure and was used as a surrogate for total costing estimates.
Results
There was a wide variation in direct costs almost tenfold, ranging from INR 240,882 to 2403193 with a mean of 603755.The cost was affected by length of stay in the hospital, whether a patient survived or died and whether the patient died within 7 days of surgery or later. It was also affected by patient-specific factors like the INTERMACS status and preoperative creatinine levels. The average cost of the entire transplant procedure was INR 1459000.
Conclusion
There is a wide variation in the cost incurred by the hospital in doing transplants dictated to a large extent by patient risk profiles. A “One package fits all model” is unrealistic. The data pertains to the cost to the hospital and not the hospital bill and is therefore relevant to any health care facility, public or private. This study provides a framework for Governmental and private insurance agencies to fix the reimbursement rates.
Keywords: Heart transplant, Cost of heart transplant, Costing studies, India heart transplant
Introduction
Heart transplantation has become an established procedure in India with increasing numbers being done annually. The majority of these patients are very sick and have had multiple hospital admissions. The economic burden of such therapy is substantial and the costs are borne by the patients with very little insurance coverage. The state government insurance in some states has started covering the cost of transplants, e.g., Tamil Nadu [1]. The amount covered is very variable and is often much less than the cost of providing this therapy. There have been no formal studies which have looked at the cost of this therapy in an Indian setting.
Aims and objectives of the study
The purpose of this study was threefold:
What is the average cost of a heart transplant procedure in a “real-world setting” in India, with varying patient risk profiles?
What are the factors contributing to the wide variations in cost seen in practice?
Finally, based on data thus collected, can some kind of estimation be made about the expected cost in a given patient before the operation is done?
Such an exercise will be invaluable for both medical personnel caring for these patients and for hospital administrators. It will also help in formulating more scientific and rational reimbursement policies, whether governmental or private.
Materials and methods
The procedure cost of 163 isolated heart transplants done during 2016–2019 was analyzed. Patients undergoing a combined heart and lung transplant were excluded from this study. The cost of preoperative hospitalizations, hemodynamic studies, investigations including those needed for workup for transplants, and stay in the city awaiting a donor organ are not included. The cost of intra-aortic balloon pump therapy or extra corporeal membrane oxygenation (ECMO) or left ventricular assist device (LVAD) as a bridge to transplant was not included, unless these were initiated after the transplant in the postoperative period. All patients had at least one surveillance endomyocardial biopsy by the second or third week after the transplant and analyzed for cell- and antibody-mediated rejection including immunohistochemistry and these costs and the cost of subsequent outpatient visits and hospitalizations, if needed, were not included in this study. It is important to emphasize that the study looked at the cost incurred by the hospital in providing this care, and not the hospital bill, which necessarily will be more. Therefore, the study has relevance regardless of the nature of the institution providing such care, public or private.
Total cost to the hospital for a patient was broken down into the following categories.
Direct costs
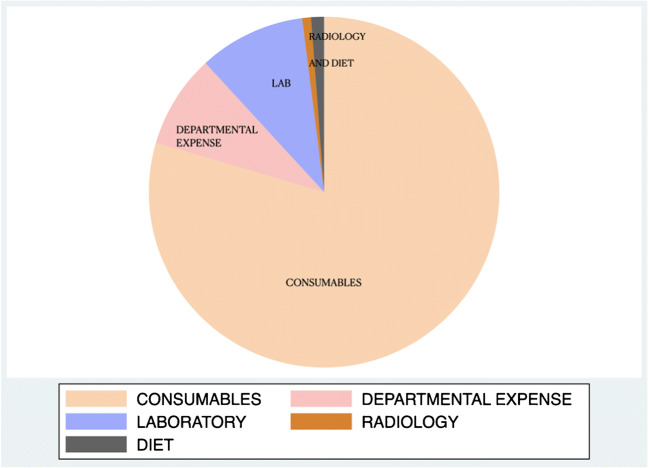
The breakup of direct costs is shown in Fig. 1.
Fig. 1.
Pie chart showing the breakup of direct costs
Consumables
These include all the disposable items used in the conduct of the operation and postoperative care, including immunosuppressive medication like basiliximab, antibiotics, blood products administered to the patient, renal replacement therapy whenever it was indicated, and intra aortic balloon pump (IABP) or ECMO if it was initiated after the transplant.
Laboratory charges
All investigations done on the patients including tacrolimus levels, and donor-specific antibody tests and Luminex single-antigen bead assays were included under this heading.
Radiology charges
This includes X-rays, CT scans, magnetic resonance imaging (MRI) scans, and ultrasound of the abdomen or vascular ultrasound. Echo routines done in the intensive care unit (ICU) were not billed separately.
Departmental expenses
This includes all drugs and consumables not used directly on the patient, but for a group of patients, for instance, hand-rub solutions which are bought in bulk for a ward. The donor heart needs to be transported from the donor hospital to the recipient hospital. These include costs involved in donor assessment, actual airlifting of organs, donor maintenance charges paid to donor hospitals, and other costs involved in the logistics of organ transplant. Not all visits to donor sites result in a transplant. Sometimes the organ is not usable or the donor sustains a cardiac arrest. All the costs incurred including the costs of failed assessments have also been included here.
Indirect costs
Included under this category are the costs incurred by the hospital other than what is directly attributable to the patients. These include costs like rentals, electricity charges, maintenance of facility and equipment, manpower costs including staff salaries, and outsourced costs like housekeeping and security.
Allocation of indirect costs
All indirect costs have been allocated based on proportion of bed days used by a heart transplant patient to the total number of bed days consumed by all inpatients in the hospital. Bed days refers to the number of days a patient stays in the hospital as an in-patient. All beds have been considered equivalent while allocating the costs.
Staff salaries
The staff costs pertaining to the cardiothoracic department alone have been allocated as a proportion of heart transplant revenue to the overall departmental revenue; all other staff costs have been allocated on the basis of bed days.
The salaries of the consultant doctors are not included in this calculation as that figure can vary greatly and in the case of government hospitals can include perks not available to private hospitals, free housing in prime localities and paid leave for sabbaticals, for example. The results of this study are therefore applicable across all spectrums of hospitals.
Direct costs contribute approximately 40% to the total cost of the procedure and are used as a marker for costing studies in this paper.
Statistical methodology
The costing data was retrieved from the hospital finance department and correlated with clinical outcomes. The statistical analysis was done in STATA (StataCorp LLC, Texas) and R. Some of the graphs were generated using ggplot 2 in R.
In relevant situations, we have provided “p” values, out of consideration for established traditions. We are fully aware of the recent position statement regarding p values by the American Statistical Association [2, 3]. While using logistic regression, we have chosen to use odds ratios rather than log coefficients.
Results
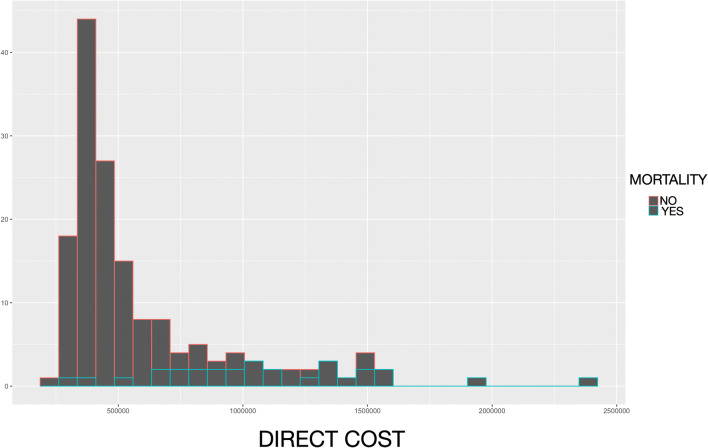
The detailed breakup of the various categories under direct cost is given in Table 1. Medical consumables contribute substantially to the total direct cost. There was a wide variation in total direct cost ranging from Indian rupee (INR) 240,882 to 2,403,193 (mean 603,755 ± 363,872; median 457,452) (Figs. 2 and 3). Heart transplants, like most other complex procedures, vary enormously in the resources utilized depending on the patients’ condition. In good risk cases, like in a dilated cardiomyopathy with a low pulmonary vascular resistance and normal renal function coming for an elective transplant, the direct cost of medical disposables can be as low as INR 250,000. On the other hand, a 60-year-old man with multiple previous coronary artery grafting procedures, on short-term mechanical support with a creatinine of 3.6, the cost is likely to be substantially higher. In this case, the highest in medical consumables was over INR 2,400,000. That is why it is important to take either an average or median costing into consideration while doing costing studies.
Table 1.
The detailed breakup of the components of direct costs
| Medical consumable | Radiology | Departmental consumption | Direct cost | |
|---|---|---|---|---|
| Minimum | 196,697 | 290 | 13,966 | 240,882 |
| 25th percentile | 286,818 | 2794 | 23,854 | 380,306 |
| Median | 352,464 | 3972 | 38,467 | 457,452 |
| Mean | 480,287 | 6632 | 53,708 | 603,755 |
| 75th percentile | 555,364 | 7810 | 61,832 | 683,577 |
| Maximum | 1,855,228 | 42,990 | 319,739 | 2,403,193 |
Fig. 2.
Histogram of direct costs categorized by survival. The skewed distribution and increase in direct costs with mortality are obvious
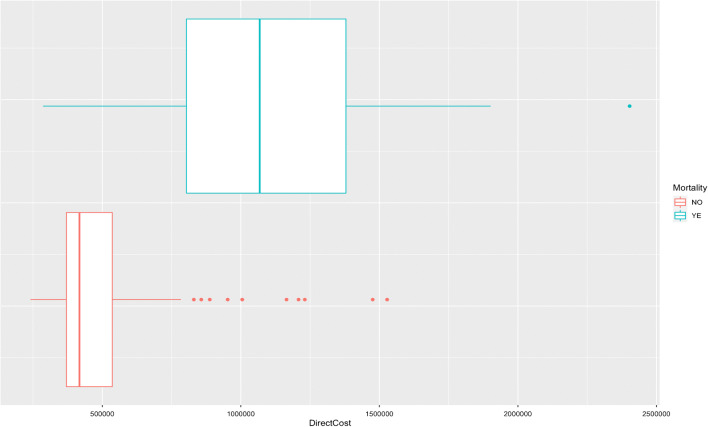
Fig. 3.
Box plot of direct costs. The edges of the box plot represent the 25th and 75th percentile, the line is the median, and the dots are the outliers. Mortality has significantly higher direct costs
We then looked at the factors contributing to such a wide tenfold variation in direct costs.
Length of stay
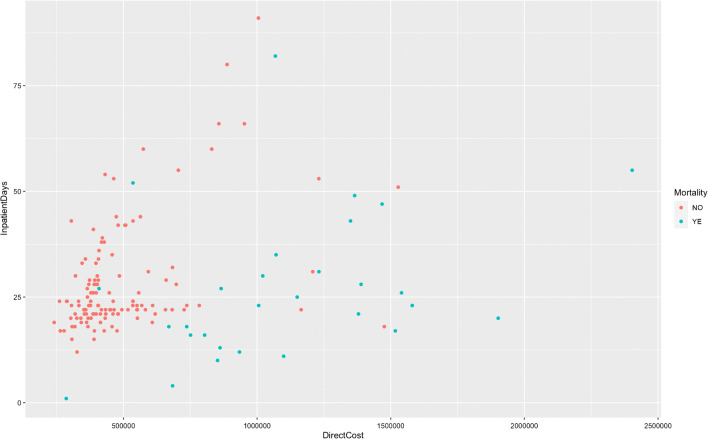
It should not come as a surprise to know that cost is directly related to length of hospital stay and this is borne out by our analysis as well. There is a clear relationship between length of hospital stay and direct costs (Figs. 4 and 5). Any patient factor which prolongs hospital stay can be expected to increase the costs.
Fig. 4.
Scatter plot between length of hospital stay and direct costs. It is not strictly linear because of the effects of mortality. The gray shading denotes confidence intervals
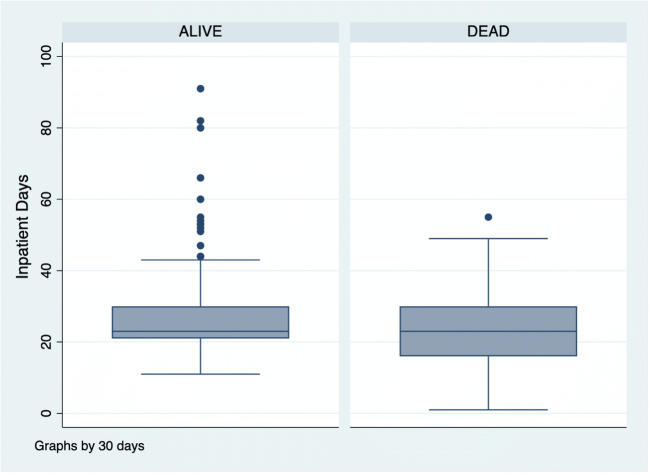
Fig. 5.
Scatter plot showing the relationship between direct cost and length of stay stratified by outcome. Clearly, the increased cost in patients who died is not always due to prolonged hospital admission
Outcome of the operation
The direct costs were significantly higher, almost double, if the patient died (p < 0.001) (Fig. 3). When we plotted the difference between costs incurred stratified by whether the death occurred within 7 days of surgery or beyond 7 days, again, there was a significant difference (p < 0.001) (Fig. 6). If the patient died within 7 days, the cost incurred was the same as the average for a surviving patient. The difference in cost between survivors and non survivors was not because of increased length of stay but resource utilization. The length of stay amongst surviving patients, in fact, was often longer (Figs. 7 and 8).
Fig. 6.
Box plot of direct costs showing the difference in cost between mortality under and over 7 days (p < .001)
Fig. 7.
Box plot comparing the inpatient admission days based on whether a patient lived or died. There are more outliers in the alive category
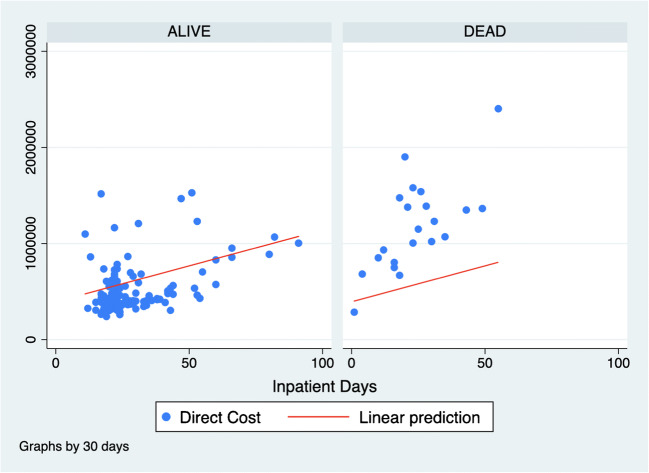
Fig. 8.
Scatter plot of inpatient days and direct costs with a linear regression line. Higher resource utilization and not increased length of hospital stay are the reasons for increased cost with mortality
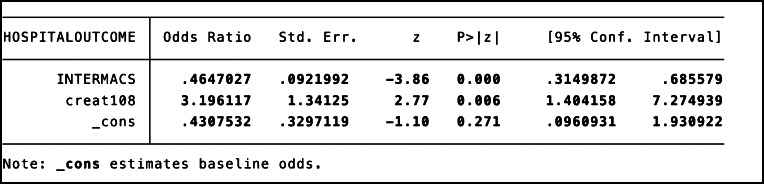
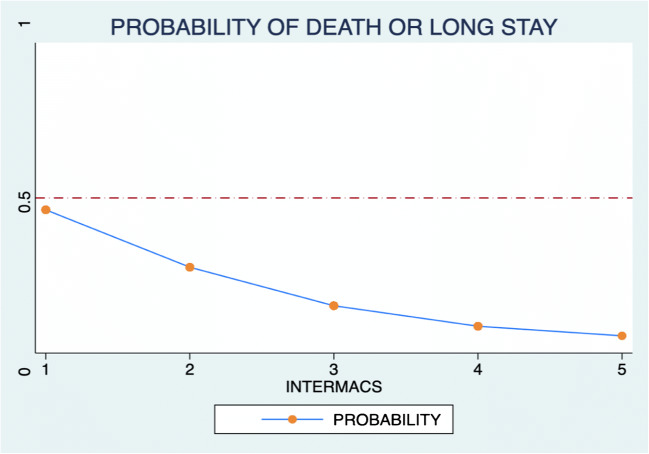
Identifying the high-risk patients
It is obviously important to identify patients at risk of prolonged stay or death not only for medical reasons but also from the point of view of the hospital bill. We did a logistic regression analysis of probability of death or prolonged hospital stay looking for predictor variables. A preoperative creatinine of more than or equal to 1.8 mg/dl (odds ratio = 3.6, p = 0.002) and low INTERMACS score (1 or 2, odds ratio = 0.27, p < 0.001) were strongly predictive of prolonged hospital stay or death (Figs. 9 and 10).
Fig. 9.
Logistic regression of hospital outcome with INTERMACS category and creatinine more than 1.8. Probability of death or prolonged hospital stay is significantly increased by serum creatinine > 1.8 mg/dl or low INTERMACS category (1 or 2)
Fig. 10.
Margins plot from a logistic regression analysis showing the relationship between length of stay or death and INTERMACS
The average cost of a heart transplant
The average cost of a heart transplant in this study including indirect costs is given in Table 2. Based on an average direct cost of INR 640,000/(6.4 lacs), the average cost to the hospital, excluding physician charges, is 14.59 lacs (INR 1.46 million),with a median cost of 13.13 lacs (INR1.3 million) if the median value of direct costs is taken.
Table 2.
The detailed breakup of indirect costs in a heart transplant
| Average cost in lacs | |
|---|---|
| Total number of transplants | 163 |
| Direct costs | 6.04 |
| Indirect costs | |
| Power and fuel | 0.26 |
| Housekeeping and security | 0.33 |
| Depreciation | 0.42 |
| Rent | 0.93 |
| Administrative costs | 0.86 |
| Staff salaries | 1.49 |
| Support salary | 0.85 |
| Cost of medical services | 3.41 |
| Total | 14.59 |
Discussion
Since donated organs from altruistic brain-dead donors are involved in this procedure and are allocated by the state government, a lot of media attention is often generated on hospital charges for these operations [4]. Unfortunately in our country, barring a few notable exceptions, the majority of such procedures are done in private hospitals. Often patients are referred late, after repeated hospital admissions, in poor physical shape, and after having pacemakers and other devices implanted.
These patients are at a significant risk for death or complications even after a transplant and these have enormous medical and financial implications. It is therefore important to analyze the costing of this procedure taking into account the risk factors for death or prolonged stay so that meaningful inferences can be drawn and might eventually help in formulating rational national policies of reimbursement.
What is a significant finding in this study is the enormous variation in direct cost incurred in a large subset of these patients, more than tenfold. At one end of the spectrum is a low-risk individual at INR 250,000 and at the other end is INR 2,400,000. A failure to appreciate this great diversity in patient population often results in reports in the press, often lamenting the fact that the organ is free and the patients are being “over charged.” The other important finding is the difference in cost incurred between a good and a poor outcome which is to a very significant extent related to the preoperative status of the patient. Death is expensive, a very harsh reality that most surgeons are aware of. There seems to be a clear relationship between hospital costs and early and late death. Balancing costs and outcomes often pose great moral and ethical challenges to the treating team. This is a complex subject relevant to every society and a subject of vigorous debate and discourse all over the world [5].
While calculating direct costs is relatively straightforward, indirect cost estimates are more challenging. We have calculated all indirect costs based on proportion of bed days used by a heart transplant patient to the total number of bed days consumed by all inpatients in the hospital. Another way of allocating the fixed costs is on a revenue basis. One can allocate the fixed costs based on revenue accruing from a transplant patient, as a proportion of total revenue of the hospital. In most cases, prices do not have a direct correlation to costs; secondly, pricing also differentiates between patients based on the paying capabilities, for the same procedure (general ward vs suite). This distorts the allocated costs arrived in this manner; hence, we have not used this method of calculating costs.
We attempted to identify risk factors which can lead to a longer hospital stay and increased costs, and two factors were very clearly identifiable, lower INTERMACS category and high preoperative creatinine values more than 1.8. It is almost certain that a patient in INTERMACS 1 or 2 or with a creatinine of 1.8 will have higher hospitalization costs. These findings are not meant as an advice to hospitals to revise their rates but to sensitize the care givers and governmental agencies to take risk profiles into consideration before fixing “packages.” In recent times, there has been a noticeable shift in government run insurance policies both at the state and at the center levels [6]. It is our hope that such studies will help in taking more scientific decisions regarding reimbursement.
Hospital charges, especially for complex procedures in sick individuals, cannot be decided by a single “package.” This often leads to discontent amongst patients and the public at large on the one hand for being “over charged” and the hospital on the other hand “for incurring losses” and the medical personnel who are valiantly trying their best are often left to bear the brunt of dissatisfaction from both parties. Our outcome studies, involving a large series of both adult and pediatric transplants, are being published elsewhere. This paper is not a sophisticated costing study meant for hospital management industry but rather an attempt at a medical perspective on cost. It is important to remember that the cost of this procedure, like most others, is amongst the lowest in the world with comparable outcomes [7]. Several of the findings highlighted in our study have been noted by other authors as well, the relationship between length of hospital stay and cost of care for example [8]. It is undeniable that heart transplants, like other major solid organ transplants, are expensive [9, 10]. We have used direct costs in all our calculations, and in our hospital, it is approximately 40% of the total cost. The method of analyzing costs in intensive care units has received much attention by other groups as well and there have been attempts to standardize the method of reporting so that meaningful comparisons can be made [11, 12].
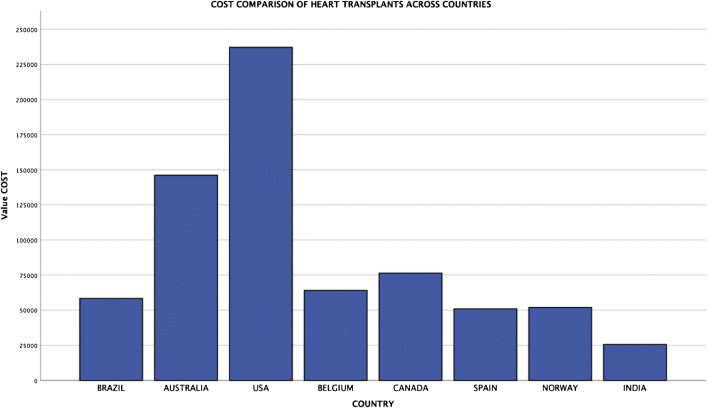
The cost of transplant can vary in different studies depending on several criteria including the criteria for patient selection [9]. A study from Brazil, which is somewhat comparable with that from India, in terms of economy though the transplants are funded by the state, looked at a total of only 27 transplants in very good risk individuals and yet their cost is significantly more [7] as it is in every country studied (Fig. 11) than in our study where a significant proportion of patients are INTERMACS 1 to 3. We have consistently directed our efforts towards cost-effective solutions in other important areas of transplantation like organ transport and this has been published as well [13]. Despite all the limitations, the cost of this procedure in India is the lowest in the world, with outcomes comparable with internationally published results (7-year survival outcomes of over 65%, manuscript under publication).
Fig. 11.
Cost of a heart transplant in US dollars in different countries
The effect of patient risk factors and mortality on costs has been documented by other studies also [14]. While costing studies are commonly published from the Western world [15], such studies from India are a rarity [16]. Finally, we did the comparisons with different patient variables using “direct costs” and not total costs because this was easier to do. Indirect cost calculations especially with regard to patient-specific variables are more complex and beyond the abilities of ordinary cardiac surgeons! Nevertheless, given that the direct costs contribute to 40% of the total costs, the conclusions of our study are valid. In terms of inferences from this study, the total cost of the procedure may vary amongst different hospitals but the broad underlying message of wide variability in costs depending on patient variables is universally applicable to all health systems. In our opinion, organ transplants are best carried out in a large university hospital, funded by the state and run as centers of excellence. Whether this will remain a pipe dream or become a reality in our post COVID world remains to be seen.
Limitations of the study
We have not been able to fully integrate patient outcomes with the cost because of the way our hospital information system is structured. We are currently working on correlating every clinical detail with the costing data. Therefore, a mathematical model for cost prediction, while possible in principle, is still at a nascent stage.
Conclusions
So what conclusions can be drawn from this study?
The cost to the hospital of doing a heart transplant is approximately between 1.3 to 1.5 million INR (13 to 15 lacs), if you take into consideration all risk profiles.
There is a wide variation in costs depending on patient factors.
If a patient dies after a transplant especially after a week, or the recovery is prolonged for whatever reason, the costs are likely to go up significantly.
All these factors need to be considered when decisions are taken about reimbursement for this therapy.
Acknowledgments
Our sincere thanks to Aishwarya Trust for help in data collection.
Funding
Not applicable
Compliance with ethical standards
Informed consent
Not applicable.
Ethics approval
Not applicable.
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
Not applicable.
Footnotes
The study is based on transplants done at Fortis Malar Hospital.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Komarakshi Balakrishnan, Email: cvskrb@gmail.com.
Coimbatore Nageswaran, Email: c.nageswaran@fortishealthcare.com.
References
- 1.Chief Minister’s Comprehensive Health Insurance Scheme. [cited 2020 Jun 8]. Available from: https://www.cmchistn.com/
- 2.Wasserstein RL, Schirm AL, Lazar NA. Moving to a world beyond “ p < 0.05”. Am Stat. 2019;73:1–19. doi: 10.1080/00031305.2019.1583913. [DOI] [Google Scholar]
- 3.Amrhein V, Greenland S. Remove, rather than redefine, statistical significance. Nat Human Behav. 2018. 10.1038/s41562-017-0224-0. [DOI] [PubMed]
- 4.Heart comes for free but transplant cost hits patients | Bengaluru News - Times of India. [cited 2020 Jun 8]. Available from: https://timesofindia.indiatimes.com/city/bengaluru/Heart-comes-for-free-but-transplant-cost-hits-patients/articleshow/51819396.cms
- 5.Emanuel EJ, Emanuel LL. The economics of dying -- the illusion of cost Savings at the end of life. New Eng J Med. 1994;330:540–544. doi: 10.1056/NEJM199402243300806. [DOI] [PubMed] [Google Scholar]
- 6.Home | Ayushman Bharat | National Health Authority | GoI. [cited 2020 Jun 8]. Available from: https://www.pmjay.gov.in/
- 7.Goldraich LA, Neyeloff JL, da Silva Etges APB, et al. Heart transplantation cost composition in Brazil: a patient-level microcosting analysis and comparison with international data. J Card Fail. 2018;24:860–863. doi: 10.1016/j.cardfail.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 8.Fine MJ, Pratt HM, Obrosky DS, et al. Relation between length of hospital stay and costs of care for patients with community-acquired pneumonia. Am J Med. 2000;109:378–385. doi: 10.1016/S0002-9343(00)00500-3. [DOI] [PubMed] [Google Scholar]
- 9.Evans RW. The economics of heart transplantation. Circulation. 1987;75:63–76. doi: 10.1161/01.CIR.75.1.63. [DOI] [PubMed] [Google Scholar]
- 10.Cope JT, Kaza AK, Reade CC, et al. A cost comparison of heart transplantation versus alternative operations for cardiomyopathy. Ann Thorac Surg. 2001;72:1298–1305. doi: 10.1016/S0003-4975(01)02997-6. [DOI] [PubMed] [Google Scholar]
- 11.Tan SS, Bakker J, Hoogendoorn ME, et al. Direct cost analysis of intensive care unit stay in four European countries: applying a standardized costing methodology. Value Health. 2012;15:81–86. doi: 10.1016/j.jval.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 12.Edbrooke D, Hibbert C, Ridley S, Long T, Dickie H. The development of a method for comparative costing of individual intensive care units. Anaesthesia. 1999;54:110–120. doi: 10.1046/j.1365-2044.1999.00650.x. [DOI] [PubMed] [Google Scholar]
- 13.Krishnan KB, Rao KS, Tanguturu MK, et al. Commercial airlines as a viable, safe and cost effective way for transporting the donor hearts across the country: single center experience. J Heart Lung Transplant. 2019;38:S133–S134. doi: 10.1016/j.healun.2019.01.317. [DOI] [Google Scholar]
- 14.Koster‐Brouwer ME, Klein Klouwenberg PM, Pasma W, Poll T, Bonten MJ, Cremer OL. Criticial care management of sepsis: a cost‐analysis from a health care perspective. Eur Soc Intensive Care Med. 2014;40:S1–S308.
- 15.Mercier G, Naro G. Costing hospital surgery services: the method matters. PLoS ONE. 2014;9:e97290 Available from: https://dx.plos.org/10.1371/journal.pone.0097290. [DOI] [PMC free article] [PubMed]
- 16.Chatterjee S, Laxminarayan R. Costs of surgical procedures in Indian hospitals. BMJ Open. 2013;3:e002844. doi: 10.1136/bmjopen-2013-002844. [DOI] [PMC free article] [PubMed] [Google Scholar]