Abstract
We present a rare case of primary colorectal linitis plastica presenting as an acute admission to hospital with a wide range of systemic symptoms, sudden rapid deterioration and subsequent mortality. A postmortem examination revealed a primary linitis plastica of the colon and rectum with diffuse metastatic disease. To our knowledge, this is the first report of primary colorectal linitis plastica presenting as an acute deterioration as a result of extensive metastatic disease.
Keywords: Linitis plastica, Colorectal malignancy, Oncology, Colorectal cancer, Ulcerative colitis
Background
Linitis plastica is a highly aggressive malignancy that spreads through submucosal and muscular layers of a hollow organ, almost exclusively the stomach.1 Colonic involvement is very rare, with the vast majority of cases being metastatic spread. Primary linitis plastica accounts for less than 0.1% of cases of colorectal cancer.2 This cancer is an adenocarcinoma characterised by anaplastic mucin secreting signet-ring cells scattered throughout poorly differentiated carcinoma.3 It carries a poor prognosis.
We report a rare case of primary linitis plastica extending proximally from the rectum to involve the entire colon. The patient deteriorated rapidly following presentation, with no diagnosis established antemortem. This owed to both the rarity of such an underlying pathology and the complex nature of his presentation. To the authors’ knowledge, this is only the third case in literature describing primary linitis plastica of the entire colon, and the first that describes a rapid acute deterioration and subsequent mortality as a result of the disease.4,5
Case history
A 71-year-old man presented to the emergency department with acute onset pleuritic chest pain. This was on a background of ulcerative colitis, first diagnosed at the age of 17 and managed medically over the following decades with minimal acute flare-ups. His most recent colonoscopy had been performed in 2018 and was unremarkable.
A computed tomography (CT) pulmonary angiogram was performed, which showed no evidence of pulmonary embolism but revealed multiple axial sclerotic lesions, most likely bony metastases from an unknown primary malignancy. A CT abdomen and pelvis demonstrated continuous thickened and featureless colon and rectum (Fig 1). These findings were presumed to be secondary to the patient’s ulcerative colitis. A colonoscopy was subsequently performed. Small polyps, probably pseudopolyps, were observed in the rectum, together with mild inflammation of the colonic mucosa (Fig 2). Multiple colorectal biopsies were taken at the time.
Figure 1.

Computed tomography image demonstrating thickening of bowel wall of transverse colon.
Figure 2.
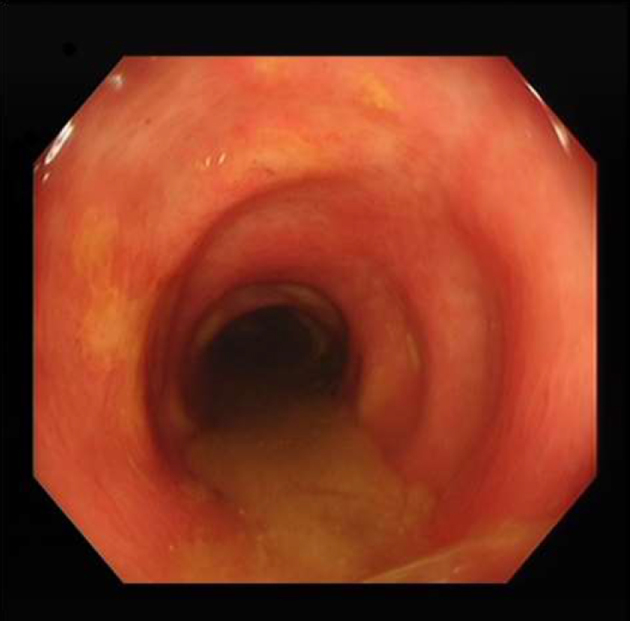
Mild inflammation throughout colon from rectum, atypical in appearance for ulcerative colitis.
Tumour markers were markedly elevated with carbohydrate antigen 19–9 being above 10,000kU/L (normal range: 0–37kU/L) and a carcinoembryonic antigen of 612.1mg/l (normal range: 0–3.5mg/l). Apart from a raised alkaline phosphatase of 778iu/l (normal range: 30–130iu/l), his liver function tests were unremarkable. Magnetic resonance cholangiopancreatography (MRCP) was performed and revealed several focally dilated peripheral bile ducts and multiple intrahepatic ductal strictures, particularly in the left lobe of the liver, raising the possibility of cholangiocarcinoma or cholangitis.
Following this, the patient acutely deteriorated. He developed new confusion, severe headaches and focal neurological deficits, with bilateral sixth cranial nerve palsy and cerebellar signs evident on examination. He also developed new-onset fast atrial fibrillation with right bundle branch block on his electrocardiogram. In conjunction with this, his abdominal pain and vomiting worsened, he became clinically and biochemically jaundiced and developed aspiration pneumonia.
Urgent CT and MRI brain scans were performed, which showed hydrocephalus and a 1.6cm right cerebellar lesion and leptomeningeal enhancement. Over the following days, the patient’s condition continued to worsen despite numerous treatments. He was commenced on intravenous steroids together with broad-spectrum antibiotics and antivirals, without improvement. Reviews from infectious diseases, gastroenterology, hepatology, neurology and ophthalmology services failed to provide a diagnosis. Worsening refractory hypertension and hypoxia mandated an intensive care unit admission. Shortly after this, he went into cardiopulmonary arrest and was declared dead following unsuccessful cardiopulmonary resuscitation. Biopsies taken at the time of colonoscopy were finalised after death and demonstrated infiltration of the bowel wall by poorly differentiated adenocarcinoma with signet-ring morphology.
Necroscopy demonstrated continuous involvement of the mucosa of the entire colon with poorly differentiated invasive adenocarcinoma with signet ring morphology classical of a linitis plastica carcinoma. Diffuse metastatic disease was found with involvement of the liver, both lungs, heart, pancreas, both adrenal glands and brain. Of note, there was no evidence of cholangiocarcinoma despite the MRCP findings. The cause of death was determined to be secondary to disseminated metastatic disease from a primary linitis plastica of the colon (Fig 3).
Figure 3.
Classical signet-ring morphology of a Linitis plastica carcinoma (circled in red) demonstrated in colonic biopsies taken.
Discussion
Primary linitis plastica of the colon is extremely rare.1 It spreads via rapid infiltration of surrounding tissue, with a particular affinity for submucosal tissue (and underlying muscularis mucosa).2 Despite being an adenocarcinoma, most infiltrating cells form abortive glandular structures, which produce copious amounts of connective tissue.3 Linitis plastica carries a poor prognosis.2 It is almost always diagnosed only at advanced stages or after death. Recognition of this condition is exceptionally difficult, owing to not only its rarity but the fact it mimics other more common conditions and often appears benign endoscopically and on imaging studies. Patients most commonly present with symptoms such as diarrhoea and weight loss, as in our case.4,5 A propensity for submucosal tissue leads to a relatively benign appearing endoscopic appearance, with only shallow ulcerations and mild inflammation seen as overlying mucosa is often unaltered.2
Our case is unique in the acute nature of the presentation. The patient presented with multiple systemic symptoms and rapidly deteriorated, with no positive response to any initiated treatment.
A primary carcinoma of the colon was never suspected in advance of the patient’s death, especially given the colonoscopy findings. His rapid deterioration would appear to be the result of widespread metastatic disease. His cerebellar symptoms resulted from the cerebellar metastasis and his neurological deterioration was deemed a result of raised intracranial pressure from leptomeningeal invasion, which impairs cerebrospinal fluid reabsorption. His postmortem examination revealed myocardial invasion, which probably impaired normal depolarisation pathways, resulting in atrial fibrillation and right bundle branch block. The postmortem examination also revealed a metastasis surrounding an intrahepatic bile duct in segment four of the liver, which probably explains his jaundice.
To our knowledge, this is the first report of primary colorectal linitis plastica presenting as rapid acute deterioration, all seemingly resulting from widespread metastases, and subsequent mortality. It presented a significant diagnostic and therapeutic challenge at the time, with a wide range of systemic symptoms that could not be connected until postmortem examination. Two other reported cases of colonic linitis plastica also occurred in patients with known ulcerative colitis.2,4 The diagnosis should be considered in the context of known ulcerative colitis and widespread metastatic disease without an obvious primary, even with macroscopically unimpressive colonoscopic findings.
References
- 1.Wei SC, Su WC, Chang MC et al. Incidence, endoscopic morphology and distribution of metastatic lesions in the gastrointestinal tract. J Gastroenterol Hepatol 2007; : 827–831. [DOI] [PubMed] [Google Scholar]
- 2.Wrobleski CS, Li J, Floch C et al. Linitis plastica of the colon in ulcerative colitis. Gastroenterologist 1997; : 247–251. [PubMed] [Google Scholar]
- 3.Agnes A, Estrella JS, Badgwell B. The significance of a nineteenth century definition in the era of genomics: linitis plastica. World J Surg Oncol 2017; : 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feinberg AE, Barnard M, Feinberg SM. Primary linitis plastica of the entire colon in a background of ulcerative colitis: a case report. World J Surg Oncol 2015; : 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park JY, Han DS, Lee HL et al. A case of linitis plastica involving the entire colon, ileum, and appendix. Korean J Gastroenterol 2003; : 237–241. [PubMed] [Google Scholar]



