Abstract
Background
Rigid bronchoscopy is often used to diagnose and treat the location of resection of the tracheal stenosis. It is a selective procedure for the dilatation of tracheal stenosis, especially when accompanied by respiratory distress.
Objectives
We introduced patients who were diagnosed with tracheal stenosis and candidate for rigid bronchoscopy dilatation by the upper airway nerve blocks.
Methods
This prospective observational study was conducted on 17 patients who underwent dilatation with rigid bronchoscopy in tracheal stenosis at Hospitals affiliated with Babol University of Medical Sciences from 2002 to 2017. The patients were given three nerve blocks, 6 bilateral superior laryngeal nerve block, bilateral glossopharyngeal nerve block, and recurrent laryngeal nerve block (transtracheal) before awake rigid bronchoscopy using 2% lidocaine. We evaluated the demographic data, the cause of tracheal stenosis, the quality of the airway nerve block (Intubation score), patients’ satisfaction from bronchoscopy and thoracic surgeons’ satisfaction. Complications of nerve blocks were recorded.
Results
From 2002 to 2017, 17 patients (14 were male and 3 were) female with tracheal stenosis who were candidates for dilatation with bronchoscopy and accepted the upper nerve block were included. The quality of the block was acceptable in 16 (94%) patients. 15 patients received fentanyl, and only two patients did not need to intravenous sedation. The mean age of patients was 29.59 ± 11.59. The average satisfaction of the surgeon was 8.82 ± 1.13 and the satisfaction of patients with anesthesia was 8.89 ± 1.16. There was one serious complication (laryngospasm) in one patient.
Conclusions
The upper airway nerve block method is a suitable anesthesia technique for patients with tracheal stenosis who are candidates for the tracheal dilatation with rigid bronoscopy, especially when the patient has respiratory distress and has not been evaluated before surgery.
Keywords: Tracheal Stenosis, Rigid Bronchoscopy, Nerve Block, Anesthesia
1. Background
Tracheal stenosis, when combined with respiratory distress, is often a life-threatening condition that requires serious intervention. It is a serious challenge between the thoracic surgeon and the anesthesiologist. To treat the resection of the tracheal stenosis, rigid bronchoscopy is often used which is a selective procedure for dilatation of tracheal stenosis, especially when accompanied by respiratory distress (1-5).
There are several methods to manage anesthesia for rigid bronchoscopy in the tracheal stenosis (6-12):
1- Apneic oxygenation: In this method, the patient is given 100% oxygen before the induction of anesthesia with intravenous anesthetic drugs. And the anesthesiologist has to stop the ventilation completely. The surgeon is allowed to work for 3 minutes or a little longer. In this method, there is a risk of hypoxia and hypercarbia.
2- Positive pressure ventilation through the bronchoscope: In this method, after complete anesthesia of the patient with intravenous drugs and rigid bronchoscopy, positive pressure ventilation is performed through the bronchoscope circuit. It causes low ventilation and contamination of the operating room due to the risk of high air leakage.
3- Jet ventilation method: In this method, after the induction of anesthesia and placing the catheter inside the airway with a manual injector, ventilation is performed at high speed but with a low respiratory rate. In this method, the risk of hypoventilation and barotrauma is high.
4- The method of maintaining spontaneous ventilation during bronchoscopy includes induction of anesthesia with inhaled anesthetics, and the method of nerve blocks of the upper airway.
To manage anesthesia for tracheal stenosis, it is important to maintain the spontaneous respiration during rigid bronchoscopy. There are several methods for the management of anesthesia to these patients. One of the common anesthetic methods is the induction of anesthesia using inhalation anesthetics, such as high concentrations of sevoflurane with or without low dose of intravenous drugs, such as propofol and fentanyl with spontaneous respiration. This method is not suitable for the elderly and cardiovascular patients due to the negative effects of high-dose inhaled anesthetics. In addition, general inhalation anesthesia with spontaneous breathing does not provide sufficient depth for rigid bronchoscopy (1, 2, 6-12). Another method of anesthesia for tracheal stenosis are upper airway nerve block. Typically, the three major nerves are blocked by local anesthetic drugs, as follows (1, 11-16).
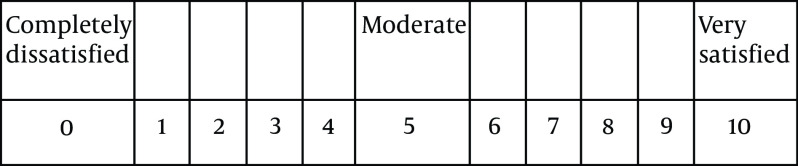
1- Bilateral glossopharyngeal block for oropharyngeal anesthesia and removal of gag reflex: Glossopharyngeal nerve provides sensory innervation to the posterior third of the tongue, anterior surface of the epiglottis, vallecular, wall of the pharynx and the tonsils. This nerve block requires the patient’s cooperation to open the mouth completely to inject the local anesthetics at the base of the posterior tonsillar pillar (Figure 1).
Figure 1. Shows the method of the glossopharyngeal nerve blocking with an open mouth (Taken from Narouze S.N. (2014) Glossopharyngeal Nerve Block. In: N. Narouze S. (eds) Interventional Management of Head and Face Pain. Springer, New York, NY).
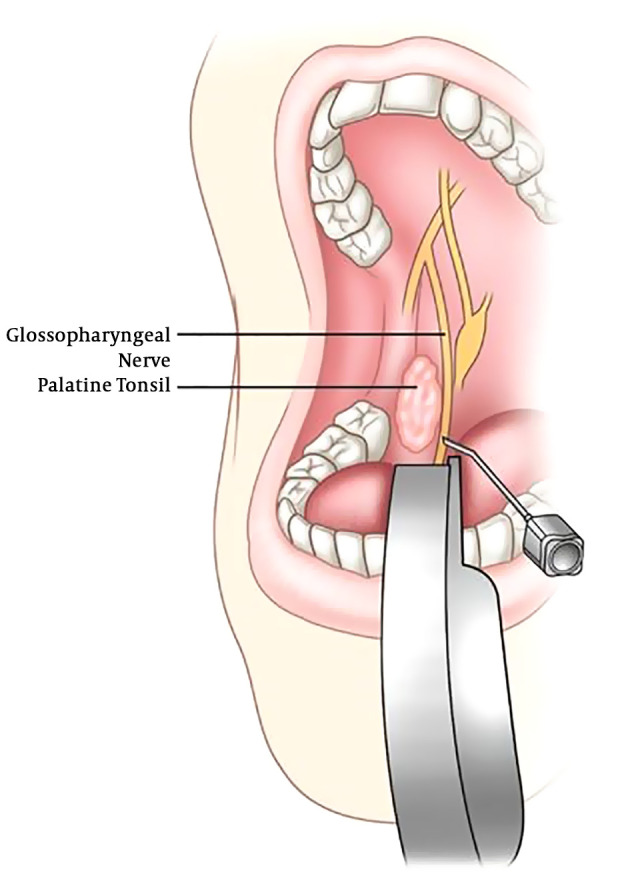
2- Bilateral superior laryngeal nerve blocks provide anesthesia to larynx above the vocal cords (the epiglottis, aryepiglottic folds, and laryngeal structures to the false cords) to remove cough response. For this nerve block, the local anesthetics are infiltrated to thyrohyoid membrane between thyroid and hyoid cartilage (Figure 2).
Figure 2. Shows the superior laryngeal nerve block. (Taken from Artime CA, Sanchez A: Preparation of the patient for awake intubation. In Hagberg CA, editor: Benumof and Hagberg’s airway management, 3‘*ed_ Philadelphia. 2013, Saunders. p. 259.
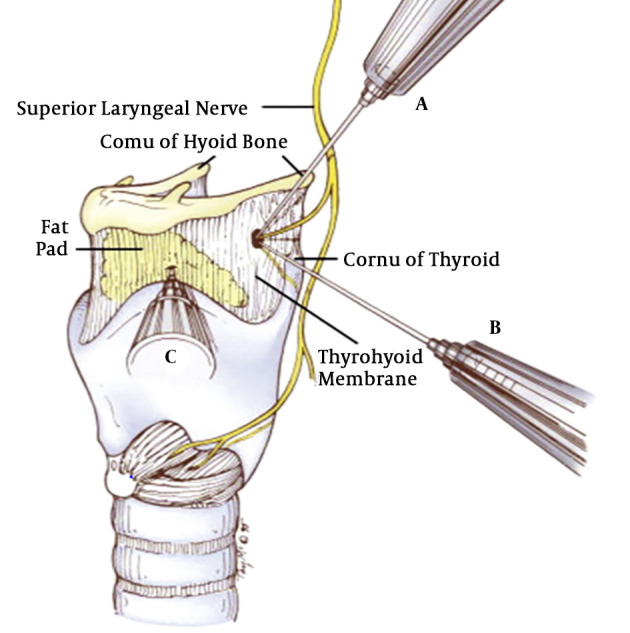
3- Recurrent laryngeal nerve (Trans laryngeal block) provides anesthesia to larynx and trachea below the cords for removal of bronchospasm (Figure 3). Trans laryngeal injection (cricoid membrane) causes coughing and rapid dissemination of local anesthetics. The administration of blouse narcotics prevents severe cough before nerve block.
Figure 3. shows how the recurrent laryngeal nerve (translargeal) is blocked. After entering the needle into the trachea, make an air aspiration before the injection of drugs. (Taken from Artime CA, Sanchez A: Preparation of the patient for awake intubation. In Hagberg CA, editor. Benumof and Hagberg's airway management, 3* ed, Philadelphia, 2013, Saunders, p. 259.).
Short-acting intravenous drugs such as fentanyl and propofol can be used simultaneously to relieve the patient and relieve the cough (16-16) before performing the upper airway block operation.
The advantage of the upper airway block, in addition to maintaining spontaneous respiration, is that the surgeon allows the chin stenosis (as opposed to the apnea oxygenation method) to be accurately assessed for the exact location and extent of the stenosis. Moreover, there is no risk of air pollution in the operating room (Unlike the ventilation during the bronchoscopy) with inhalation anesthetics and unlike jet ventilation, there is no risk of barotrauma (6-13) (Figure 4).
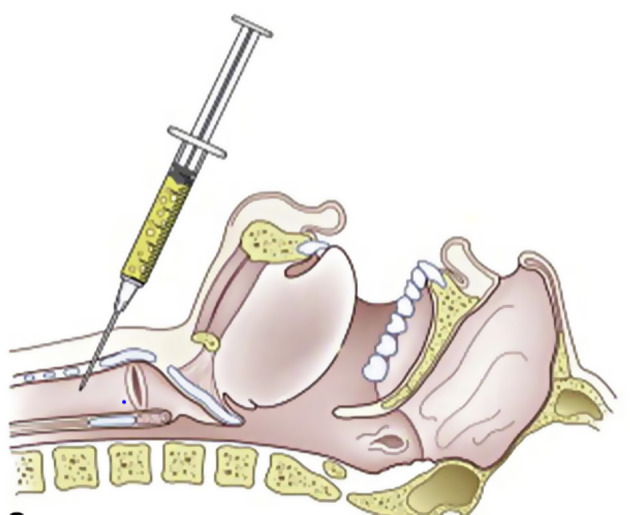
Figure 4. Patient and thoracic surgeon consent.
2. Objectives
There have been few studies on the upper airway nerve block for rigid bronchoscopy in Iran. In this study, we decided to introduce patients diagnosed with tracheal stenosis from 2002 to 2017, and candidate for rigid bronchoscopy dilatation by the upper airway nerve blocks.
3. Methods
A prospective observational study was conducted from 2002 to 2017 on all patients with tracheal stenosis scheduled for rigid bronchoscopy at Shahid Behshti and Rouhani Hospital of Babol University of Medical Sciences. In all the patients, the diagnosis of tracheal stenosis was established by CT-scan. Patients with the following conditions were excluded: Not accepting the method of nerve block by the patient, coagulopathy, full stomach, allergy to local anesthesia and local pathology. Prior to starting the Nerve blocks, the Thoracic surgeon was prepared for a rigid bronchoscopy the patient’s bedside and 0.25 intravenous Atropine was administrated, 30 minutes before the nerve block.
The airway nerve block was performed after explaining the block method to the patient and obtaining the informed consent. Airway nerve blocks include bilateral glossopharyngeal block for oropharynx, bilateral superior laryngeal block for larynx above the cords, and translaryngeal block for larynx and trachea below the cords. This research has been approved in the Ethics Committee of Babol University of Medical Sciences as registration code IR.MUBABOL.HRI.REC.1398.232.
The procedure was done in the operation room. Basic monitoring included electrocardiography, heart rate, pulseoximetry, and Noninvasive blood pressure. Oxygen was administered by face mask.
Before starting the block, intravenous fentanyl was administered 50 to 150 micrograms for the patient’s comfort and 0.25 mg intravenous atropine was prescribed to reduce oral and airway secretion. Patient comfort and sedation score were determined based on the Ramsay Sedation Scale. The procedure was performed when the patients’ sedation score based on Ramsey’s score was 2 (Patient is cooperative, oriented, and tranquil) or 3 (Patient responds only to commands).
Bilateral superior laryngeal nerve blocks were performed with 3 mL of 2% lidocaine. This block was injected percutaneously into thyrohyoid membrane midway between the lateral aspect of the hyoid and superior cornea of the thyroid cartilage. Glossopharyngeal nerve blocks: one milliliter 1% lidocaine is injected just to posterior tonsillar pillar (aspirate first, avoid carotid artery injection).
Translaryngeal block was performed with 3 mL of 2% lidocaine into tracheal lumen through the cricothyroid membrane.
Bronchoscopy started after a successful block test (removal of swallowing and coughing reflux). To evaluate the quality of the airway nerve block, the intubation score was used when entering the bronchoscope into the trachea (Table 1).
Table 1. Intubation Score During the Passage of Rigid Bronchoscope into the Trachea (11).
| Variable | Intubation Score | ||
|---|---|---|---|
| Excellent | Good | Poor | |
| Vocal cord movement | Open | Moving | Closing |
| Coughing | None | Slight | Sustained |
| Limb movement | None | Slight | Vigorous |
Intubation condition excellent = all scores are excellent; good = all scores are excellent or good; clinically acceptable intubation = excellent and good condition
Patient and thoracic surgeon’s satisfaction were determined on a Likert scale from 0 (completely dissatisfied) to 10 (very satisfied). We evaluated the demographic data, cause of tracheal stenosis, the quality of the airway nerve block (Intubation score), patients’ satisfaction from bronchoscopy and thoracic surgeons’ satisfaction. The complications of nerve blocks were recorded.
4. Results
From 2002 to 2017, 17 patients with tracheal stenosis who were candidates for dilatation with bronchoscopy and accepted the upper nerve block were included.
Block quality was acceptable in 16 patients (94%) and one patient was not acceptable, but the surgeon performed a rigid bronchoscopy immediately due to bronchospasm and then continued using intravenous anesthetics.
Table 3 shows background information and the cause of tracheal stenosis.
Table 3. Demographic Data of 17 Tracheal Stenosis Patients.
| Characteristic | Value |
|---|---|
| Gender (male/female) | 14/3 |
| Age (year), Mean | 29.59 ± 11.59 |
| Patients’ consent | 8.89 ± 1.16 |
| Surgeons’ consent | 8.82 ± 1.13 |
| Post-intubation tracheal stenosis, No. (%) | 9 (52.94) |
| Post-tracheostomy tracheal stenosis, No. (%) | 5 (29.41) |
| Post-anastomotic stenosis, No. (%) | 1 (5.88) |
| Endotracheal tumor, No. (%) | 2 (11.76) |
Fifteen patients received fentanyl and only two patients did not need the intravenous sedation. Of the 17 patients, 14 were male and 3 were female. The mean age of patients was 29.59 ± 11.59. The average satisfaction of the surgeon was 8.82 ± 1.13 and the satisfaction of patients with anesthesia was 8.89 ± 1.16. There was one serious complication (laryngospasm) in one patient (Tables 2 and 3).
Table 2. Characteristics, Quality of Block, Patient and Surgeon Consent and Complication of 17 Tracheal Stenosis Patients.
| Variable | Sex | Age (year) | Quality of Block | Surgeon Satisfaction | Patient Satisfaction | Complication |
|---|---|---|---|---|---|---|
| 1 | M | 26 | Good | 8 | 9 | - |
| 2 | F | 21 | Excellent | 8 | 10 | Hypertension |
| 3 | M | 26 | Poor | 6 | 7 | Laryngospasm Severe hypoxemia |
| 4 | M | 24 | Good | 9 | 8 | - |
| 5 | M | 26 | Excellent | 10 | 9 | - |
| 6 | F | 29 | Excellent | 10 | 10 | - |
| 7 | M | 28 | Good | 8 | 8 | Tachycardia |
| 8 | M | 31 | Excellent | 10 | 10 | - |
| 9 | M | 24 | Good | 7 | 7 | Cough, Mild hypoxemia |
| 10 | M | 70 | Excellent | 9 | 9 | - |
| 11 | M | 18 | Good | 9 | 8 | - |
| 12 | M | 26 | Good | 9 | 7 | - |
| 13 | M | 26 | Good | 9 | 9 | - |
| 14 | M | 40 | Excellent | 10 | 9 | - |
| 15 | M | 34 | Excellent | 10 | 10 | - |
| 16 | M | 28 | Excellent | 10 | 10 | - |
| 17 | M | 26 | Good | 9 | 10 | - |
5. Discussion
From 2002 to 2017, 17 patients were enrolled in this study with a diagnosis of tracheal stenosis that was candidates for dilatation with rigid bronchoscopy and accepted nerve block method.
In 16 patients, block quality was acceptable for rigid bronchoscopy (94%). Serious complications were observed in one patient (laryngospasm).
Chatrath et al. conducted an observational study on 50 ASA I-II patients who were candidates for fiberoptic bronchoscopy intubation. In the method, glycopyrolate as an anticholinergic and low dose of sedative agents were administered; the bilateral blocks of SLN, bilateral glossopharyngeal and RLN (transtracheal) with lidocaine 2% were performed. They concluded that the upper airway nerve block for tracheal intubation with fiberoptic bronchoscopy provides better patient comfort and hemodynamic stability. In our study, the glossopharyngeal block was performed intraorally, but in Chatrath’s study, this block was performed extraorally (perihyoid approach). Similar to our study the quality of intubation was acceptable in more than 90% of patients (11).
Ramaswamy et al. reported a patient with rigid bronchoscopy and dilatation due to respiratory distress after long-term intubation with a diagnosis of tracheal stenosis by combining Nerve block and intravenous drugs. They concluded that the combination of upper airway nerve block and intravenous drugs was appropriate for patients with respiratory distress and poor medical evaluation (16). The patient’s symptoms and anesthesia management were similar to our patient.
Ito et al. introduced a 65-year-old woman with a history of tracheal stenosis who candidate for dilatation of trachea. The patient was sedated with midazolam and doxmedetomedine. Under the guide of bronchoscopy, tracheal tube number 5 was placed above the site of the stenosis. Then, the trachea dilated by ablation with argon laser and balloon. Eventually, the tube number 7 was passed from the stenosis, and the patient was extubated after spontaneous respiration (8).
The block and procedure approach was similar to our study. The method of sedation was Midazolam and Dexmedetomidine. These combination does not increase the risk of respiratory depression.
In most studies, anticholinergic drugs such as glycopyrillate were prescribed before the block to reduce respiratory secretion, but in our study, low-dose atropine (0.25) was prescribed because glycopyrrolate was not available (8, 16).
Chumpathong et al. studied the incidence and risk factors of hypoxia during anesthesia in 126 tracheal stenosis patients undergoing intravenous anesthesia with spontaneous breathing for dilatation and stent insertion. The main cause of tracheal stenosis was tuberculosis (41.3%) and malignancy (35.7%). The incidence of hypoxia was 25.5% during anesthesia (17). In our study, the rigid bronchoscopy was performed with nerve block with spontaneous respiration, and the incidence of hypoxemia was 2 patients (11.76%).
The present study encountered some limitations. For instance, the glossopharyngeal nerve block was performed by the intraoral method. Although an anesthesiologist was experienced in this work, this approach requires patient cooperation and is now less acceptable.
5.1. Conclusion
The upper airway nerve block method is a suitable anesthesia technique for patients with tracheal stenosis who are candidates for the tracheal dilatation with rigid bronoscopy, especially when the patient has respiratory distress and has not been evaluated before surgery.
Acknowledgments
The staff of the operating room and the anesthetic technicians at Ayatollah Rouhani Hospital and Beheshti Hospital are honored and thanked for cooperation in the treatment of the patient. We thank Rouhani Clinical Research Development Unit for typing, data preparation, and manuscript submission
Footnotes
Authors' Contribution: P.A. carried out the experiment. P.A and N.N. wrote the manuscript with support from P.A, N.N, R.M. supervised the project. R.N. performed the analytic calculations. R.N. helped supervise the project.
Conflict of Interests: Authors declared no conflict of interest.
Ethical Approval: This article does not contain any studies with Human participants or animals performed by any of the authors.
Funding/Support: None.
Informed Consent: After explaining the block method to the patient informed consent was obtained.
Contributor Information
Parviz Amri, Email: pamrimaleh@gmail.com.
Novin Nikbakhsh, Email: n.nikbakhsh@mubabol.ac.ir.
Seyed Reza Modaress, Email: r.modarres@mubabol.ac.ir.
Ramin Nosrati, Email: nosrati.r@mubabol.ac.ir.
References
- 1.de Lima A, Kheir F, Majid A, Pawlowski J. Anesthesia for interventional pulmonology procedures: a review of advanced diagnostic and therapeutic bronchoscopy. Can J Anaesth. 2018;65(7):822–36. doi: 10.1007/s12630-018-1121-3. [DOI] [PubMed] [Google Scholar]
- 2.Kumar A, Asaf BB, Puri HV, Lingaraju VC, Siddiqui S, Venkatesh PM, et al. Video-assisted thoracoscopic surgery for pulmonary aspergilloma. Lung India. 2017;34(4):318–23. doi: 10.4103/0970-2113.209232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Esakov YS, Pechetov AA, Khlan TN, Solodinina EN, Slepenkova KV, Bessonova SA, et al. [Circular tracheal resection for acquired tracheal stenosis: evaluation of early and long-term outcomes]. Khirurgiia (Mosk). 2019;(2):19–25. doi: 10.17116/hirurgia201902119. [DOI] [PubMed] [Google Scholar]
- 4.Ezemba N, Echieh CP, Chime EN, Okorie CO, Okonna FG, Idoko FL, et al. Postintubation tracheal stenosis: surgical management. Nigerian Journal of Clinical Practice. 2019;22(1) doi: 10.4103/njcp.njcp_288_18. [DOI] [PubMed] [Google Scholar]
- 5.Pournajafian AR, Ghodraty MR, Faiz SH, Rahimzadeh P, Goodarzynejad H, Dogmehchi E. Comparing GlideScope Video Laryngoscope and Macintosh Laryngoscope Regarding Hemodynamic Responses During Orotracheal Intubation: A Randomized Controlled Trial. Iran Red Crescent Med J. 2014;16(4):e12334. doi: 10.5812/ircmj.12334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramkumar V. Preparation of the patient and the airway for awake intubation. Indian J Anaesth. 2011;55(5):442–7. doi: 10.4103/0019-5049.89863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mathur PR, Jain N, Kumar A, Thada B, Mathur V, Garg D. Comparison between lignocaine nebulization and airway nerve block for awake fiberoptic bronchoscopy-guided nasotracheal intubation: a single-blind randomized prospective study. Korean J Anesthesiol. 2018;71(2):120–6. doi: 10.4097/kjae.2018.71.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ito K, Yamazaki K, Kan T, Tetsu S, Saito K, Kohno M, et al. Anesthetic Management in Tracheal Dilatation for Severe Tracheal Stenosis. The Tokai journal of experimental and clinical medicine. 2018;43(2):50–3. [PubMed] [Google Scholar]
- 9.Derakhshan P, Reza Faiz SH, Mohseni M, Yazdi A. Comparison of intravenous and transtracheal lidocaine on hemodynamic changes in patients with hypertension following tracheal intubation: A double blind clinical trial. Trends in Anaesthesia and Critical Care. 2019;29:35–9. doi: 10.1016/j.tacc.2019.09.002. [DOI] [Google Scholar]
- 10.Li N, Zhu L, Sun J, Pan Y, Gao M. Difficulty in tracheal extubation followed by tracheal collapse after balloon dilatation for tracheal stenosis therapy: A case report. Medicine (Baltimore). 2018;97(22):e10907. doi: 10.1097/MD.0000000000010907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chatrath V, Sharan R, Jain P, Bala A, Ranjana. Sudha The efficacy of combined regional nerve blocks in awake orotracheal fiberoptic intubation. Anesth Essays Res. 2016;10(2):255–61. doi: 10.4103/0259-1162.171443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mononyane R. Regional anaesthesia for awake intubation. Southern African Journal of Anaesthesia and Analgesia. 2018;24(3) [Google Scholar]
- 13.Daumerie G, Su S, Ochroch EA. Anesthesia for the patient with tracheal stenosis. Anesthesiol Clin. 2010;28(1):157–74. doi: 10.1016/j.anclin.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 14.Juvekar NM, Neema PK, Manikandan S, Rathod RC. Anesthetic management for tracheal dilatation and stenting. Indian J Anaesth. 2003;47(4):307–10. [Google Scholar]
- 15.Cho AR, Kim HK, Lee EA, Lee DH. Airway management in a patient with severe tracheal stenosis: bilateral superficial cervical plexus block with dexmedetomidine sedation. J Anesth. 2015;29(2):292–4. doi: 10.1007/s00540-014-1912-9. [DOI] [PubMed] [Google Scholar]
- 16.Ramaswamy AH, Kurdi MS, Shaikh SI, Deva RS, Raza SU. Awake rigid bronchoscopy for post intubation tracheal stenosis. Anaesthesia, Pain & Intensive Care. 2019:299–301. [Google Scholar]
- 17.Chumpathong S, Tscheikuna J, Boonsombat T, Muangman S, Luansritisakul C. Incidence and Risk Factors of Hypoxemia During Interventional Rigid Bronchoscopy Under Spontaneous-assisted Ventilation. J Bronchology Interv Pulmonol. 2017;24(4):268–74. doi: 10.1097/LBR.0000000000000387. [DOI] [PubMed] [Google Scholar]